Abstract
Background:
Anterior cruciate ligament reconstruction (ACLR) with hamstring autograft has gained popularity. However, an unpredictably small graft diameter has been a drawback of this technique. Smaller graft diameter has been associated with increased risk of revision, and increasing the number of strands has been reported as a successful technique to increase the graft diameter.
Purpose:
To compare failure rates of 5-strand (5HS) and 6-strand (6HS) hamstring autograft compared with conventional 4-strand (4HS) hamstring autograft. We describe the technique in detail, supplemented by photographs and illustrations, to provide a reproducible technique to avoid the variable and often insufficient 4HS graft diameter reported in the literature.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We retrospectively reviewed prospectively collected data of all primary hamstring autograft ACLRs performed at our institution with a minimum 2-year follow-up and 8.0-mm graft diameter. A total of 413 consecutive knees met the study inclusion and exclusion criteria. The study population was divided into 5HS and 6HS groups as well as a 4HS control group. The primary outcome was failure of ACLR, defined as persistent or recurrent instability and/or revision ACLR.
Results:
The analysis included 224, 156, and 33 knees in the 5HS, 6HS, and 4HS groups, respectively. The overall ACLR failure rate in this study was 11 cases (8%): 5 cases for 5HS, 3 cases for 6HS, and 3 cases for 4HS. No statistically significant differences were found among groups (P = .06). The mean graft diameter was 9 mm, and the mean follow-up was 44.27 months.
Conclusion:
The 5HS and 6HS constructs have similar failure rates to the conventional 4HS construct of 8.0-mm diameter and are therefore safe and reliable to increase the diameter of relatively smaller hamstring autografts. We strongly recommend using this technique when the length of the tendons permits to avoid failures reportedly associated with inadequate graft size.
Keywords: ACL, hamstring autograft, 5-strand, 6-strand, 4-strand
Quadrupled hamstring tendon autografts (4HS) are commonly used in anterior cruciate ligament reconstruction (ACLR) surgery with equivalent outcomes and fewer complications in comparison to patellar tendon autografts.3,8,19 Despite the popularity of this technique, a notable disadvantage is the variability of the graft size. To date, anthropometric studies have not been consistently successful at predicting the graft diameter preoperatively,6,12,13,24 and nearly half of the grafts do not meet the sufficient 8.0-mm diameter.18 Biomechanical studies have shown a positive correlation between load-to-failure rate and an increasing graft diameter,2 and clinical studies have shown a lower risk of revision21,23 as well as better functional outcomes with a larger graft size.11,14,15
Several techniques have been described that produce a larger hamstring graft diameter when relatively undersized tendons are used. One of these is the 5-strand hamstring autograft (5HS), in which the longer semitendinosus tendon is tripled and the gracilis tendon is doubled. This technique has been reported to increase the final graft diameter by 1 to 2 mm.11,22 A 6-strand configuration (6HS) has also been described. In a series published by Tutkus et al,25 the 5- and 6-strand configurations had a probability of almost 100% of producing grafts of more than 8.0 mm in diameter.
The current study aimed to compare the failure rates of 5HS and 6HS autograft reconstructions compared with the conventional 4HS autograft of adequate diameter of 8.0 mm and larger and to provide a detailed yet simplified description of the technique. Previous studies had significantly smaller numbers and shorter follow-up. We hypothesized that 5HS and 6HS constructs would have an ACLR failure rate similar to that of the 4HS provided that all graft diameters were above the 8.0-mm threshold.
Methods
This retrospective comparative review of prospectively collected data was approved by the institutional review board of Hamad Medical Corporation (HMC) and was conducted in concordance with the Declaration of Helsinki. We retrospectively reviewed all of the prospectively collected data in the electronic medical records (EMRs) of patients who underwent ACLR at HMC between January 2011 and November 2017. Patients were examined clinically for signs of instability via Lachman and anterior drawer tests in the office and by pivot-shift test under anesthesia at the beginning of the procedure, and all patients underwent confirmatory magnetic resonance imaging (MRI) to diagnose ACL rupture and other knee pathologies. The surgical technique, follow-up, and rehabilitation protocol were standardized. Isolated ACLR with or without partial meniscectomy was followed by an accelerated ACL rehabilitation protocol with immediate weightbearing, closed chain quadriceps strengthening, and return to sport at 9 months after surgery. Concomitant meniscal tear repairs and chondromalacia were rehabilitated on a case-by-case basis. Patients’ medical histories, mechanism of injury, demographics, surgical technique, complications, and concomitant knee pathologies, if any, were recorded.
The inclusion criteria were as follows:
Gracilis and semitendinosus hamstring autograft
Femoral fixation through use of suspensory fixation with Endobutton (Smith & Nephew Endoscopy) and tibial fixation with an interference absorbable screw
A minimum of 24 months of follow-up
Sufficient final graft diameter, defined as 8 mm and larger
Operative notes, follow-up notes, and images available for review on the EMR
Femoral tunnel position at 10 o’clock for the right knee and 2 o’clock for the left knee
Primary ACLR
The exclusion criteria were as follows:
Intraoperative complications associated with failure of the graft, such as femoral tunnel blow-out or malposition
High-energy trauma, fracture, or knee dislocation leading to graft failure
ACLR performed as part of a multiligamentous repair
The primary outcome was graft failure. Failure was defined as having a revision ACLR of the index knee, persistent or recurrent instability, and/or MRI evidence of rupture of the graft. The study population was divided into 3 groups: those who had a 5HS, those who had a 6HS, and a control group who had conventional quadruple graft reconstruction (4HS). We screened 542 records against inclusion and exclusion criteria, and 413 knees were included. The majority of excluded cases entailed either bone-tendon-bone grafts or hamstring autografts less than 8 mm in diameter. All ACLR cases excluded due to insufficient graft size entailed quadruple strands. All of the 5-strand and 6-strand grafts were larger than 8.0 mm. Table 1 shows the characteristics of the study patients.
Table 1.
Patient Characteristicsa
| Overall (N = 413 Knees) |
4HS (Control) (n = 33 Knees) |
5HS (n = 224 Knees) |
6HS (n = 156 Knees) |
P Valueb | |
|---|---|---|---|---|---|
| Age, y, mean (95% CI) | 31.54 (30.86-32.23) |
32.12 (29.58-34.65) |
30.89 (29.88-31.90) |
32.37 (31.39-33.34) |
.122 |
| Sex, % | |||||
| Male | 93.9 | 98.2 | 97.4 | ||
| Female | 6.1 | 1.8 | 2.6 | ||
| Laterality, % | |||||
| Right | 54.7 | 42.4 | 57.1 | 54.8 | |
| Left | 45.3 | 57.6 | 42.9 | 46.2 | |
| Body mass index, kg/m2, mean (95% CI) | 27.34 (26.90-27.78) |
28.39 (26.86-29.93) |
27.01 (26.41-27.60) |
27.67 (26.97-28.38) |
.189 |
| Follow-up, mo, mean (95% CI) | 44.27 (42.99-45.56) |
28.46 (24.78-32.15) |
44.14 (42.35-45.93) |
47.81 (46.11-49.50) |
<.001 |
a4HS, 4-strand hamstring tendon autograft; 5HS, 5-strand hamstring tendon autograft; 6HS, 6-strand hamstring tendon autograft.
bComparison between the 3 graft types.
Surgical Technique
The technique has been described in recent articles by investigators using aperture femoral fixation.10 The following describes our technique for using suspensory fixation with an Endobutton. This technique has been used at our institution for well over 7 years.
Standard anterior medial and lateral arthroscopic portals were used. A diagnostic arthroscopy was performed to examine the ACL tear and presence of injuries to other knee structures. A longitudinal skin incision of approximately 5 cm was then made on the anteromedial tibial surface, starting 2 cm distal and 2 cm medial to the tibial tubercle, and was extended distally. The gracilis and semitendinosus tendons were harvested using a closed tendon stripper. Tendons were cleared from residual muscle tissue, and the length and thickness were measured in a conventional 4-strand arrangement. Our technique was performed consistently, and apart from the number of strands, all variables were similar among the 3 groups (Table 2).
Table 2.
Intraoperative Detailsa
| 4HS | 5HS | 6HS | |
|---|---|---|---|
| Endobutton loop length, mm, mean | 14.7 | 16.4 | 15.1 |
| Femoral tunnel length, mm, mean | 35.0 | 38.2 | 37.4 |
| Concomitant injury, n (%) | |||
| Medial meniscus | 11 (33.3) | 64 (28.5) | 39 (25) |
| Lateral meniscus | 5 (15.2) | 23 (10.3) | 8 (5.1) |
| Medial and lateral meniscal tears | 1 (3) | 9 (4) | 4 (3) |
a4HS, 4-strand hamstring tendon autograft; 5HS, 5-strand hamstring tendon autograft; 6HS, 6-strand hamstring tendon autograft.
We determined the final strand arrangements after considering the following:
The graft was a minimum of 8.0-mm diameter.
A minimum of 20 mm of the graft was in the femoral tunnel. The femoral tunnel length was measured, and the length of the Endobutton was subtracted.
30 mm of the graft was inside the joint.
A minimum of 30 mm of the graft was in the tibial tunnel.
Thus, to achieve an adequate graft, a minimum size of 80 mm long and 8 mm wide was required. When the length permitted, the surgeon would increase the strand numbers to achieve the largest diameter possible (Table 3).
Table 3.
Minimum Required Tendon Length for Each Technique
| Technique | Semitendinosus, mm | Gracilis, mm |
|---|---|---|
| 4-strand graft | 160 | 160 |
| 5-strand graft | 240 | 160 |
| 6-strand graft | 240 | 240 |
Four-Strand Graft
A whipstitch was placed at each end of both the gracilis and semitendinosus tendons with Ti-Cron (Coviden) nonabsorbable braided coated sutures. The proximal free ends of both tendons were passed through the loop of the Endobutton and pulled until both ends of each tendon were at the same level distally.
Five-Strand Graft
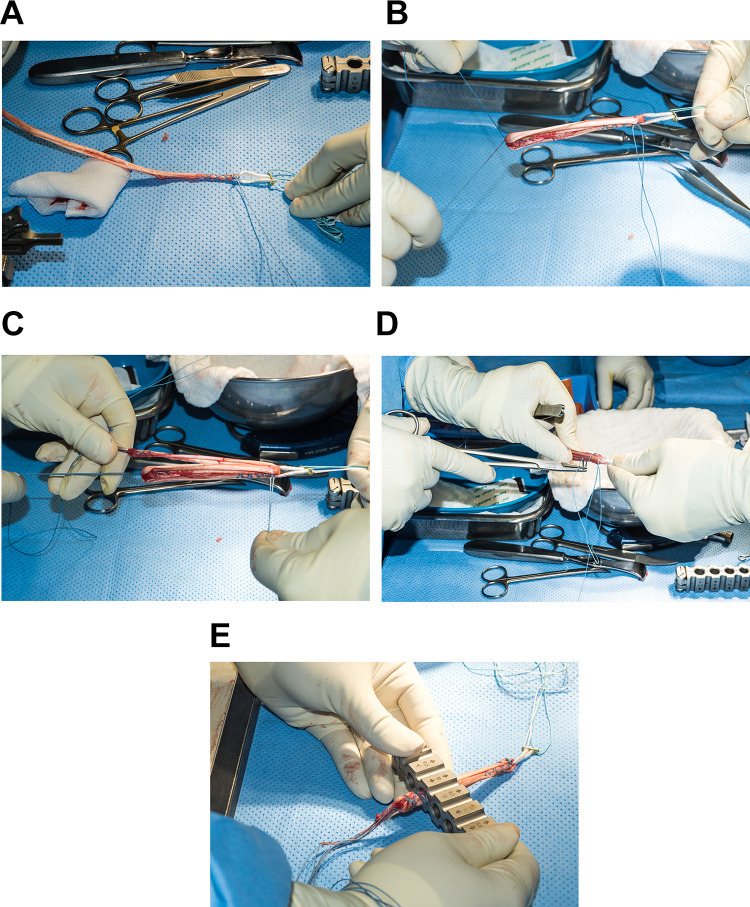
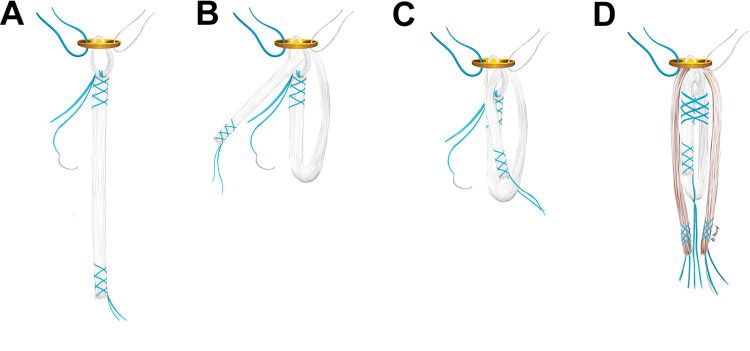
A whipstitch was placed at each end of the gracilis tendon with Ti-Cron nonabsorbable braided coated sutures. In the semitendinosus tendon, a whipstitch was placed on either end through use of nonabsorbable braided coated sutures. With the same stitch thread, the distal free end was then tied to both ends of the Endobutton and secured. The needle was left to be used later to reinforce the proximal part of the graft (Figure 1, A and B). The graft was then folded and the distal free end was passed through the Endobutton (Figure 2B) and pulled until it reached the folded end of the graft (Figure 1B). One limb of the whipstitch of the distal end was passed through the loop (Figure 2C) and tied to the other limb securely (Figure 1B). Next, the gracilis tendon was passed through the loop of the Endobutton and pulled until both proximal and distal ends were at the same level (Figure 1C). Finally, the proximal end of the graft, now having the 3 strands of the semitendinosus and 2 strands of gracilis, was sutured by use of the needle that was left at the proximal end of the semitendinosus graft, and the needle was cut (Figures 1D and 2D).
Figure 1.
Intraoperative clinical photographs showing the steps of the 5-strand hamstring graft preparation. (A) The whipstitch end of the harvested semi-T tendon is securely tied to the loop of the Endobutton. (B) The free end of the semi-T tendon is passed through the loop and the suture ends are tied to form the 3-strand semi-T graft part. (C) The gracilis is passed through the loop and folded on itself to from a double-strand graft. (D) The now 5 strand graft is secured by suturing all the 5 strands together. (E) The 5 strand graft is now ready to be measured.
Figure 2.
Illustration of the 5-strand hamstring graft preparation. (A) The whipstitch end of the harvested semi-T tendon (white) is securely tied to the loop of the Endobutton. The needle of the proximal whipstitch is left in place. (B) The free end of the semi-T tendon is passed through the loop. (C) The suture ends are tied on either sides of the distal end to form a triple-strand configuration. (D) The final 5-strand configuration.
Six-Strand Graft
Both semitendinosus and gracilis tendons were treated in a manner similar to the semitendinosus preparation in the 5-strand technique, and both ends were sutured and secured.
Graft Sizing
Sizing of the graft was done in the same fashion regardless of the selected graft technique by passing it through a diameter sizing block. Graft diameter was defined as the smallest diameter lumen through which the graft would pass smoothly. The sizing was made by use of standard graft measurement block in 0.5-mm increments (Figure 1E).
Femoral Tunnel Drilling
Femoral tunnel drilling was conducted freehand by means of the anteromedial portal technique.
Graft Fixation and Tensioning
The hamstring graft was passed through the femoral and tibial tunnels, and the Endobutton was flipped. The graft was conditioned by moving the knee through 0° to 130° of flexion for 30 cycles followed by tibial fixation at 30° of flexion while maintaining tension at 40 N/m through use of the tensioning device.
Statistical Analysis
Statistical analysis was performed by an independent statistician. Descriptive statistics for variables such as age, sex, body mass index, concomitant knee pathologies, failure rate, and graft size were generated as they related to study groups. Data were reported as means and 95% CIs and compared via analysis of variance (statistical significance set at P < .05) by use of SPSS software (Version 21; SPSS Inc).
Results
The overall rate of failure for all the study participants was 11 of 413 knees (2.7%). The failure rate in the 4HS group was higher than that in the 5HS and 6HS groups: 9.1% vs 2.3% and 2.7%, respectively. However, given the number of cases available for analysis, this difference in failure rate did not reach statistical significance (Table 4).
Table 4.
Graft Failure Ratesa
| 4HS | 5HS | 6HS | P Value | |
|---|---|---|---|---|
| Graft failure, n (%) | 3 (9.1) | 5 (2.3) | 3 (2.7) | .06 |
| Graft diameter, mm, mean (95% CI) | 8.25 (8.05-8.45) | 9.14 (9.04-9.24) | 8.95 (8.85-9.05) | <.001 |
a4HS, 4-strand hamstring tendon autograft; 5HS, 5-strand hamstring tendon autograft; 6HS, 6-strand hamstring tendon autograft.
Of the 11 failed ACLRs, 7 cases were related to soccer 12 to 14 months after surgery, and the patients underwent revision ACLR. Two patients had persistent subjective and clinical instability and elected not to undergo revision. In 2 patients, the mode of failure was documented as trauma to the knee with no further details, but MRI revealed a ruptured graft without concomitant fractures. Of the latter 2 patients, only 1 patient received an ACLR revision with an anterolateral ligament reconstruction.
Although all grafts included in this study were 8.0 mm or larger in diameter, the 4HS technique produced a mean graft diameter of 8.25 mm compared with 9.14 mm and 8.95 mm in 5HS and 6HS groups, respectively. The mean difference in graft diameter was statistically significant when we compared the 5HS versus the 4HS control group as well as the 6HS versus the 4HS control group. No statistically significant difference was seen in graft diameter between the 5HS and 6HS groups.
Discussion
We have demonstrated that in hamstring autografts with sufficient diameter of 8.0 mm, the 5HS and 6HS techniques have not shown any statistically significant increase in failure rate. In theory, the 5HS and 6HS constructs have a possible weak point at the proximal end where the graft is tied to the Endobutton in comparison with being looped through the Endobutton in the conventional 4HS preparation technique. This assumption, however, proved unfounded, and there was a trend toward lower failure rates. A recently published systematic review of the relatively scant comparative studies of 4HS and 5HS techniques showed that no significant differences exist in ultimate load, stiffness, displacement, and stress relaxation.20 That review also showed no clinically or statistically significant differences between both techniques in failure rates, but it entailed a significantly smaller number of total patients. Our study had a 300% larger sample size, and despite excluding undersized 4HS grafts, we arrived at the same conclusion of no significant difference in failure rate while controlling for graft size. Another point worth highlighting in the current study is that we included only those procedures that used suspensory cortical fixation. This is the only comparative clinical study of 5HS and 6HS versus 4HS constructs reporting on this technique to date. We have standardized the graft preparation technique, fixation of femoral and tibial ends of the graft, and rehabilitation and follow-up protocols since 2013, and all of our 5- and 6-strand ACLR procedures have been performed by the 2 senior authors (F.A., K.A.), which limits the variability in technique. It is worth mentioning, however, that use of a femoral fixation device in conventional 4HS ACLR has shown no effect on mechanical stability, revision rate, or functional outcomes, as reported in a meta-analysis published by Hurley et al.9
Hamstring autograft ACLR has gained popularity due to the higher tensile strength it provides and lower risk of complications such as anterior knee pain and donor site morbidity compared with bone–patellar tendon–bone (BPTB) autografts. A meta-analysis published by Mohtadi et al16 of almost 1600 patients in 19 comparative clinical trials showed a statistically significant increase in anterior knee pain, a loss of extension range of motion, and a trend toward loss of extension strength with BPTB grafts. Despite the popularity and potential benefits of hamstring autografts, many reports have highlighted the unpredictable graft diameter compared with BPTB.
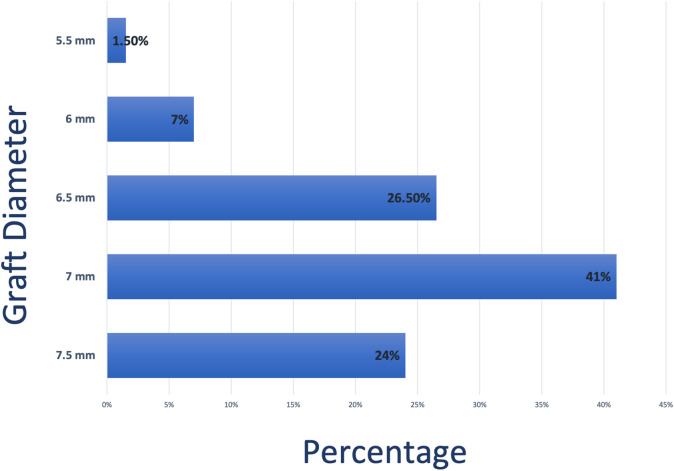
The variability of hamstring autograft diameter is a serious drawback, and ACL autograft diameter has received much attention over the past decade. Biomechanical and clinical studies have supported the superiority of larger diameter grafts. A biomechanical study by Boniello et al2 showed increasing load to failure with increasing graft diameter. This was confirmed by many authors who reported that lower functional outcomes such as Knee injury and Osteoarthritis Outcome Score15 and higher failure rates14,15,21,23 were associated with smaller graft diameter. The widely acceptable minimum graft diameter among many authors and experts is 8.0 to 8.5 mm in adults. It was reported that the likelihood of a patient requiring revision was 0.82 times lower for every 0.5-mm increase in graft diameter from 7.0 to 9.0 mm.23 Grawe et al7 also found a higher failure rate with grafts smaller than 8.0 mm in diameter. An analysis of all 4HS procedures conducted at our institute revealed a significantly smaller diameter. The mean graft size was 7 mm with significant variability, with grafts as small as 5.5 mm (Figure 3).
Figure 3.
Details of excluded knees with quadrupled hamstring tendon autografts (4HS).
The drawback of the conventional quadruple hamstring autograft was reported by Mariscalco et al,15 who concluded that 55.1% of grafts were less than 8.0 mm. We have noted that Asian and Arab patients have more often than not produced smaller diameter grafts. The overwhelming consensus on the importance of graft size and the lack of a reliable and simple method to quantify expected hamstring graft before harvesting it as well as local observation of our population has been the driving force to use our 5HS and 6HS techniques to maximize the graft diameter. As a result, all of the patients who underwent 5HS or 6HS procedures received a graft of 8.0-mm diameter or larger. This is in accordance with Tutkus et al,25 who measured the graft diameter of ACL grafts using the 5HS and 6HS technique. They found that this technique had almost 100% probability of obtaining grafts with a diameter of 8 mm or larger.
Although multiple studies have attempted to establish a method to reliably predict graft diameter preoperatively, it is unclear whether a graft diameter of 8.0 mm can be guaranteed. Authors of 2 studies suggested that patient height, weight, and thigh circumference were correlated with hamstring graft diameter.1,5 In other words, a taller, heavier patient may have a thicker hamstring graft compared with a lighter, shorter patient, but grafts of both patients may still be smaller than 8.0 mm when the conventional 4HS technique is used. Moreover, those 2 studies relied on MRI measurements and/or equations that we had difficulty applying in our high-volume setting. Another study reported a correlation between the cross-sectional area of the semitendinosus muscle on MRI and the diameter of the ACL graft using its tendon in a 4-strand configuration. We are not certain whether this correlation applies to combined semitendinosus and gracilis tendons grafts.4 The remainder of articles published state that adequate graft diameter cannot be predicted.6,12,13,24
Finally, increasing the graft diameter by adding 1 or 2 strands using the same autograft avoids the use of added allograft in a hybrid configuration. The latter technique has been reported to increase the risk of graft failure.17 Although allografts can have a predictable diameter preoperatively, they are costly and not available in every center.
Limitations
Despite the authors' best efforts, this study is not without limitations. One of the definitions of ACL graft failure used in this study is revision ACLR of the index knee, which is limited to those revisions performed at our institution and does not account for those done elsewhere. However, Hamad Medical Corporation is the sole provider of nationwide public health care with a centralized EMR accessible to the researchers that includes all its hospitals and primary care centers across the country.
Another limitation is the large number of 4HS grafts that were excluded due to inadequate graft size. We elected to exclude those because of inherent failure risk with undersized grafts and resulting confounding of the results. However, this study has the largest number of 5- and 6-strand grafts reported in the literature. Moreover, the drawback of inadequate 4HS graft size is the reason we conducted this study.
Finally, the study’s retrospective nature renders it impossible to make any conclusions about functional outcomes, given the inadequate documentation of validated outcome scores. We believe it would be unethical to conduct this study in a randomized controlled fashion, as this would entail using grafts of inadequate diameter with known higher risks of failure reported in the literature.14,15,21,23
Conclusion
ACLR techniques entailing 5HS and 6HS grafts have similar failure rates to the conventional 4HS of 8.0 mm in diameter and are therefore safe and reliable to increase the diameter of relatively smaller hamstring autografts. We strongly recommend using this technique when the length of the tendons permits to avoid failures reportedly associated with inadequate graft size.
Acknowledgment
The authors thank Dr. Prem Chandra at the HMC medical research center for his outstanding help with the statistical analysis.
Footnotes
Final revision submitted March 27, 2020; accepted April 14, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto. IRB approval was granted from Hamad Medical Corporation (protocol No. MRC-01-18-419).
References
- 1. Asif N, Ranjan R, Ahmed S, Sabir AB, Jilani LZ, Qureshi OA. Prediction of quadruple hamstring graft diameter for anterior cruciate ligament reconstruction by anthropometric measurements. Indian J Orthop. 2016;50(1):49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boniello MR, Schwingler PM, Bonner JM, Robinson SP, Cotter A, Bonner KF. Impact of hamstring graft diameter on tendon strength: a biomechanical study. Arthroscopy. 2015;31(6):1084–1090. [DOI] [PubMed] [Google Scholar]
- 3. Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33(2):450–463. [DOI] [PubMed] [Google Scholar]
- 4. Cobanoglu M, Ozgezmez FT, Omurlu IK, Ozkan I, Savk SO, Cullu E. Preoperative magnetic resonance imaging evaluation of semitendinosus tendon in anterior cruciate ligament reconstruction: does this have an effect on graft choice? Indian J Orthop. 2016;50(5):499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Corey S, Mueller T, Hartness C, Prasad B. Correlation of intra-operative hamstring autograft size with pre-operative anthropometric and MRI measurements. J Orthop. 2018;15(4):988–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goyal S, Matias N, Pandey V, Acharya K. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop. 2016;40(1):173–181. [DOI] [PubMed] [Google Scholar]
- 7. Grawe BM, Williams PN, Burge A, et al. Anterior cruciate ligament reconstruction with autologous hamstring: can preoperative magnetic resonance imaging accurately predict graft diameter? Orthop J Sports Med. 2016;4(5):2325967116646360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81(4):549–557. [DOI] [PubMed] [Google Scholar]
- 9. Hurley ET, Gianakos AL, Anil U, Strauss EJ, Gonzalez-Lomas G. No difference in outcomes between femoral fixation methods with hamstring autograft in anterior cruciate ligament reconstruction—a network meta-analysis. Knee. 2019;26(2):292–301. [DOI] [PubMed] [Google Scholar]
- 10. Krishna L, Tan XY, Wong FKL, Toh SJ. A 5-strand hamstring autograft achieves outcomes comparable to those of a 4-strand hamstring autograft with a graft diameter of 8 mm or more in anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;6(3):2325967118760815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lavery KP, Rasmussen JF, Dhawan A. Five-strand hamstring autograft for anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3(4):e423–e426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Loo W, Liu B, Lee Y, Soon Y. Can we predict ACL hamstring graft sizes in the Asian male? A clinical relationship study of anthropometric features and 4-strand hamstring graft sizes. Malays Orthop J. 2010;4:9–12. [Google Scholar]
- 13. Ma CB, Keifa E, Dunn W, Fu FH, Harner CD. Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17(1):81–83. [DOI] [PubMed] [Google Scholar]
- 14. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 15. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29(12):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pennock AT, Ho B, Parvanta K, et al. Does allograft augmentation of small-diameter hamstring autograft ACL grafts reduce the incidence of graft retear? Am J Sports Med. 2017;45(2):334–338. [DOI] [PubMed] [Google Scholar]
- 18. Ramkumar PN, Hadley MD, Jones MH, Farrow LD. Hamstring autograft in ACL reconstruction: a 13-year predictive analysis of anthropometric factors and surgeon trends relating to graft size. Orthop J Sports Med. 2018;6(6):2325967118779788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39(10):2161–2169. [DOI] [PubMed] [Google Scholar]
- 20. Smith JH, Houck DA, Hart JA, et al. Five-strand hamstring autografts for anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2019;7(2):2325967119826094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Snaebjornsson T, Hamrin Senorski E, Ayeni OR, et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med. 2017;45(9):2092–2097. [DOI] [PubMed] [Google Scholar]
- 22. Snow M, Cheung W, Mahmud J, et al. Mechanical assessment of two different methods of tripling hamstring tendons when using suspensory fixation. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):262–267. [DOI] [PubMed] [Google Scholar]
- 23. Spragg L, Chen J, Mirzayan R, Love R, Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(6):1475–1481. [DOI] [PubMed] [Google Scholar]
- 24. Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(11):1945–1949. [DOI] [PubMed] [Google Scholar]
- 25. Tutkus V, Kluonaitis K, Silove S, et al. ACL reconstruction using 5- or 6-strand hamstring autograft provides graft’s diameter bigger than 8 mm. Knee Surg Sports Traumatol Arthrosc. 2018;26:1349. [DOI] [PubMed] [Google Scholar]