Abstract
Background and Aims:
Patients with trigeminal neuralgia (TN) can be overwhelmed with information they are given when first seen in a specialist secondary care clinic. The purpose of this study is to evaluate the extent to which a telephone service provided by the clinical nurse specialist (CNS) with independent prescribing rights improves patient management and satisfaction and reduces costs.
Methods:
All patients with a diagnosis of TN who used the CNS telephone service in 2015 were contacted by two medical students (independent observers) using a semi-structured questionnaire. Patients who could not be contacted were sent the same questionnaire and asked to return it by post.
Results:
Fifty-two patients were identified and 34 replied to a telephone call and 10 to a questionnaire, response rate 85%. Overall, 61% of patients rated their care outstanding or excellent. Four patients could not remember their consultation, others had used it on multiple occasions. Reasons for the consultation were pain management 50%, changeover of drugs 25%, advice about drug schedules 17%, and dealing with side effects 8%. The number of general practitioner (GP) consultations decreased as a result of this service. Patients suggested that the service should be available more than once a week.
Conclusion:
The CNS telephone service cut down on the number of outpatient appointments needed and reduced travel costs. Patients were appreciative that the CNS was in contact with GPs and this ensured prescriptions were filled in a timely manner and strengthen links with practices.
Keywords: Trigeminal neuralgia, clinical nurse specialist
Introduction
Trigeminal neuralgia (TN) is a condition described as a brief, stabbing, severe, unilateral facial pain brought on by light touch activities. The episode can last from a few seconds to minutes and recur multiple times a day but can also go into remission for months.1 Some attacks are relatively mild but others are so severe that eating, talking and washing the face becomes impossible. Its unpredictability results in added psychological burden of not knowing if and when the next pain paroxysm may strike and how severe it may be. TN has been associated with depression, anxiety and poor sleep.2 It is a rare condition and it is estimated that an average GP practice may have three to five patients in their practice and may not always be using the correct medications.3,4
TN can be managed pharmaceutically or surgically. The mainstays of medical treatment are anticonvulsants: carbamazepine and oxcarbazepine. Second-line treatments include lamotrigine, pregabalin and gabapentin; however, their efficacy is variable.5 Patients with episodic neuralgic pain may find it difficult to manage their medication. Given the nature of the condition, many continue taking medication even when they are symptom-free in case of a relapse, increasing the likelihood of experiencing adverse effects, whereas other patients believe they can take their medications like analgesics to treat their pain when it occurs. The dosages used, therefore, vary and many GPs do not appreciate the need for flexible dosage schemes. Patients referred to a specialist centre have often been to several other providers and not all have used the standard drugs,4 for example, carbamazepine as recommended by NICE and European guidelines.6,7
Patients report significant side effects from their medications which are often dose dependent.8,9 It is important that patients increase their medications slowly and use the minimum dosage required to achieve good pain control.
The challenge of long-term management of TN as well as the acute onset of severe pain paroxysms could be addressed through the introduction of a clinical nurse specialist (CNS). A CNS could provide additional support and thereby reduce the burden on medical outpatient clinics and GP visits. CNSs specialise in a particular field and become competent both in diagnostics and prescribing.10 Courtenay et al. found that CNS could be instrumental in managing pain when utilising clinical guidelines. CNS play a crucial role in patient education and so enabling patients to manage their condition more effectively but a review of their role in 2008 showed there were few rigorous studies and no literature on the role of nurse prescribers in chronic pain.11 A more recent UK national survey of nurses prescribing in the pain field showed that up to 24% prescribe anti-epileptic drugs but there are currently no studies reporting on the role of a CNS in the TN field.12 The primary aim of this study was to determine the role of a CNS with independent prescriber rights in the management of patients with TN through a survey of users of the CNS-led telephone service. Secondary aims included evaluating the extent to which a telephone service provided by the CNS impacted on overall patient satisfaction and its costs.
Methods
The service
All patients with TN are fully assessed at their first visit to a facial pain unit. All are then given a treatment plan which includes general information about TN, (booklet from the Brain and Spine Foundation – https://www.brainandspine.org.uk/our-publications/booklets/face-pain/). Medications are discussed and patients are given a medication schedule and a pain diary if necessary. The GPs are sent a standardised but individualised letter, asking them to continue medications as detailed on the included medication schedule; the patient receives a copy of all of this too. The patients are re-appointed for a follow-up and also a review in a joint neurosurgical clinical as per Trust guidelines. Since the appointment of a CNS, patients are also provided with details on how to contact the CNS if they were not coping or needed further advice. The CNS telephone appointments are booked by the unit’s secretary at 30-minute intervals for one afternoon a week. The CNS provides a service for the whole facial pain unit. The CNS files all details in the medical records and electronic records are also made. If necessary, the CNS will ring or write to GPs or arrange a follow-up appointment in outpatients. If necessary, she will also discuss the patient at a multidisciplinary team meeting (MDT) or with one of the consultants.
Evaluation of the service
The study was completed between March and September 2016. From a database containing 240 telephone consultations for 2015, 52 patients were selected who met the eligibility criteria of having a diagnosis of TN and who had at least one telephone consultation with the CNS in 2015. This was done by two medical students (M.H., T.M.) independent of the unit. All authors then agreed on a semi-structured interview which could be carried out by telephone or by post if necessary. All telephone interviews were initially conducted on a weekday evening and lasted approximately 15 minutes each, but were rescheduled to a time more convenient to the patient if necessary. The answers to the questions were immediately entered on to an anonymised excel spreadsheet in the form of free text and dropdown categories for each question. Where appropriate these categories were coded to facilitate quantitative analysis.
Patients
All patients were registered at the facial pain clinic in a London teaching hospital and had undergone a full assessment, been given a treatment plan and subsequently requested a telephone consultation with the CNS in 2015. The list of patients was standardised according to age/gender and the number of CNS telephone consultations they had (single or multiple); each patient on the list was assigned a study number to maintain anonymity and from which the medical students chose either odd or even numbered patients to call. The majority of this cohort were from London. The number of telephone consultations and medical outpatient appointments they had in 2015 was determined from the electronic clinical records as the codes used for the two services are different. A control group was chosen from all patients who had attended in 2010, prior to introduction of the CNS; the number of outpatient appointments they had attended, as recorded on the electronic clinical records, was documented. All patients attending the teaching hospital provide written generic consent but additionally they provided verbal consent on being contacted by TM and MH.
Interviews
The questionnaire was designed to measure the patients’ experience and perception of the CNS-led telephone service. Questions broadly focused on the following three areas: pain and medication management (e.g. whether CNS clarified medication use and gave patients better control of pain-related symptoms); the need for other services (e.g. did the patients require further medical attention after the telephone call and how quickly did the CNS arrange referrals for the patients when required) and finally patients’ overall satisfaction with the quality of service rendered. The exact content of the interview/questionnaire was reviewed by experts in the field so as to determine its construct validity. Consent was obtained prior to each telephone interview, which were carried out by two medical students closely following a predetermined script. The students belonged to AcaMedics, a group of students interested in doing research and had no affiliations to the facial pain unit. All telephone interviews took place from the facial pain office at the hospital. Those patients who could not be contacted by telephone were sent a questionnaire comprising the same questions with a cover letter and pre-addressed stamped envelope.
Data analysis
Data analysis consisted of comparing demographic statistics and determining the outcome measures using descriptive statistics. The sample size was based on the number of calls made in 1 year.
Results
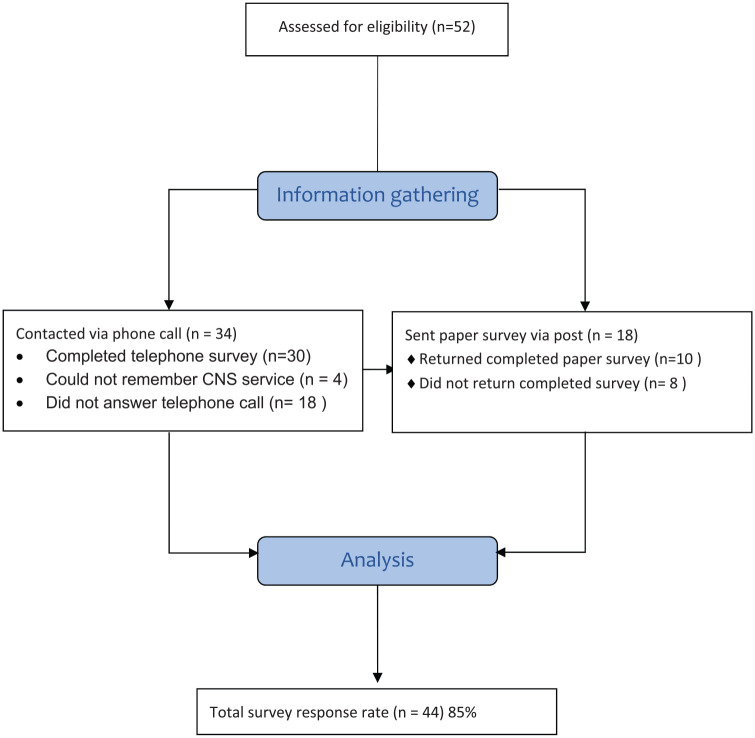
A total of 52 patients were identified from the telephone consultations database. Figure 1 shows the results of the calls and postal replies. There was an overall response of 85% with 40 (77%) usable replies. The patients who could not recall a telephone consultation were three females aged 63, 73 and 87 and one male aged 76. Of the eight who did not respond to the survey, five were females aged 43, 47, 55, 57 and 61 and three were males aged 59, 73 and 76.
Figure 1.
Flow chart of CNS survey collection.
Prior to commencing the CNS telephone service, patients had an average of 2.3 face-to-face consultations with a TN specialist per year. Once the CNS service was started in 2011, the number of appointments with the consultant were reduced, although the telephone service overall increased the number of times the patients were in contact with the unit as shown in Table 1. The mean age of patients using the TN service in 2015 remains similar to those using the service in 2010, with comparable male:female ratios.
Table 1.
Demographics of group and control cohorts.
| 2015 responders n = 44 |
Non-responders n = 8 |
2010 (control) cohort n = 49 |
|
|---|---|---|---|
| Mean age (youngest, oldest) | 63.0 (17–87) | 65.1 (43–76) | 62.2 (39–84) |
| No. of males: | 13 | 3 | 17 |
| No. of females: | 31 | 5 | 32 |
| Mean no. of consultant appointments in 1 year | 1.6 | 0.9 | 2.3 |
| Mean no. of telephone consultations | 2.6 | 1.5 | Not applicable |
For a 30-minute review appointment, the current telephone service tariff is £29.85 and the face-to-face consultation tariff is £96.73. The cost of a band 7 CNS for 1 session a week is £140, in which there are six telephone consultations (allowing time for administrative work at the end of the session), resulting in the cost to the hospital of £23.33 per telephone consult. For a consultant, the cost is £49.83 for a 30-minute consultation, in addition to £13.00 for a nurse to assist. Therefore, both the CNS-led telephone service and face-to-face review appointments result in a profit for the service overall; however, the CNS service does not require clinic space; therefore, the clinic room can be used by other clinicians, increasing the capacity and therefore revenue of the service.
The CNS-led telephone service may reduce the overall costs to the health service as 63% of patients reported that they would have sought an appointment with their GP or other health care professional. The cost of a GP appointment is currently £30 (https://www.england.nhs.uk/2019/01/missed-gp-appointments-costing-nhs-millions/). Furthermore, GP appointments are often approximately 10 minutes; the CNS consultations are for 30 minutes, and for patients on complex medication regimes, it is probable that a 10-minute consultation with a GP would be insufficient to resolve the patients’ queries. In addition, the qualitative analysis shows that some patients do not feel their GPs have sufficient experience in managing TN, as it is a rare pain disorder.
Figure 2 shows that the reasons for using the CNS-led telephone service had most commonly been for pain management, followed by changeover of drugs, discussing side effects of medications and discussing the drug schedule.
Figure 2.
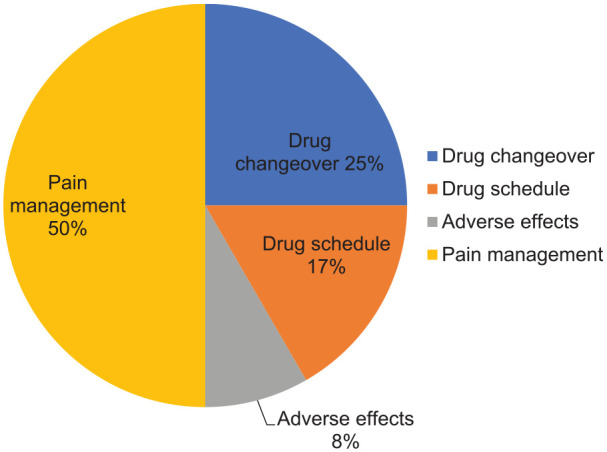
Main reasons for CNS telephone consultation.
The majority of patients were satisfied with the service, with 83% rating it as good to outstanding. The CNS helped the patients by making changes to their medication/prescriptions for at least 11 out of the 40 patients surveyed and had been able to arrange medical/neurosurgical appointments for seven patients out of the 18 patients who had experienced severe pain at the time of their consultation. All patients are offered an annual face-to-face review with the consultant but not all required it. Of the 16 patients who visited their GP after the CNS consultation, it was for a repeat prescription in 50% of cases. Acute severe flare-ups resulted in three patients attending Accident and Emergency departments.
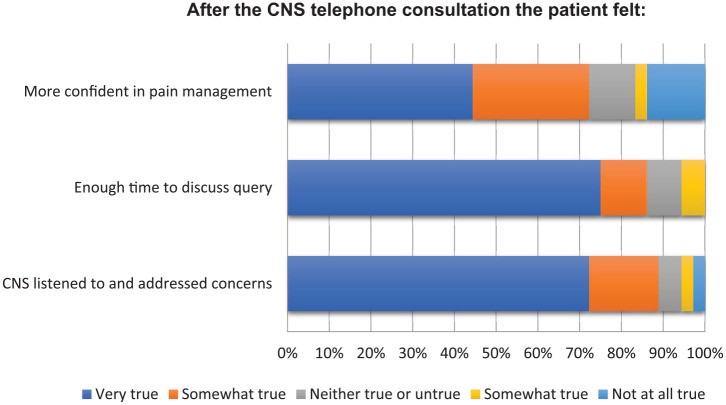
Overall, 72% of patients felt more confident in their pain management after talking to the CNS, whereas 16% felt this was ‘somewhat untrue’ or ‘very untrue’ as illustrated in Figure 3. When asked to rate the care they received during the telephone consultation, 36% reported it as ‘outstanding’, 25% ‘excellent’, 6% as poor. The majority of patients suggested that more telephone clinics should be made available.
Figure 3.
The patient impact after the CNS telephone consultation.
Overall, the patients commented that it was a very useful service especially if they lived some distance away but a more frequent service would be helpful as shown in Table 2. Some suggested that this could be extended to email as talking could be very difficult when in pain.
Table 2.
Summary of patient responses to CNS survey.
| Question | Response category | Percentage of patients |
|---|---|---|
| Satisfaction with the CNS service itself? | ||
| How easy did you find it to make an appointment with the CNS? | Somewhat easy–very easy | 56 |
| How long did you have to wait before being contacted by the CNS after making the request? | Less than 6 days | 74 |
| Did the CNS answer your question in a way you could understand? | Somewhat true–very true | 78 |
| Did you feel you had enough time to discuss your query with the CNS? | Somewhat true–very true | 86 |
| Use of other health care services | ||
| Would you have made arrangements to see your GP/other health care professional if you had not been able to speak to the CNS? | True to very true | 67 |
| Since your telephone appointment have you visited | Yes | |
| 1. GP | 19 | |
| 2. TN specialist | 33 | |
| 3. Emergency medicine | 8 | |
| Did the CNS change your medications/prescription? | Yes | 24 |
| Patient suggestion re CNS service | ||
| This clinic only runs on Wed pm. Do you feel it would have been helpful if you could speak to the CNS at another time? | Somewhat helpful to very helpful | 61 |
| If the pain is stable, would a 6 month review with the doctor and a 3 month review telephone consultation be better? | Yes No |
Yes = 57 No = 22 |
CNS: clinical nurse specialist; GP: general practitioner; TN: trigeminal neuralgia.
Note: Not all patients answered all the questions.
Discussion
This is the first formal independent evaluation of a CNS-led telephone service for patients with TN and demonstrates it to be a novel and valuable service. It shows that the role of the CNS is multifaceted, and as well as providing advice on prescriptions, it helps in monitoring and education of both patients and GPs. The response rate is very high compared with previous studies and the cohort is well characterised.11
The service could reduce the number of doctors’ appointments required per patient in primary care and accident and emergency. It also shows a reduction in the mean number of specialist facial pain consultant appointments when patients have access to a CNS service. The study design did not determine the exact reduction in primary care or other doctor appointments; however, 67% said that they would have made arrangements to see another healthcare professional if the CNS service was not available, which would suggest that the presence of the CNS clinic reduced their demand on other health care services.
Improving quality of care while reducing costs remains a priority for many healthcare services, and the CNS service achieves this; the telephone service appointments cost less than consultant-led pain clinic appointments or psychologist appointments, and a reduction in the number of appointments further reduces costs. Furthermore, the service may improve interdisciplinary collaboration and communication, for the benefit of patient care, as the CNS is part of a wider MDT and also liaises directly with the patients’ primary care providers as required. This means GPs are educated about management of this rare but debilitating condition.
The service facilitates medicines management as the CNS can prescribe and advise GPs regarding prescriptions, thereby acting as patient’s advocates to GPs. Indeed, medication-related queries were a common reason for using the service, with 50% of users identifying medication scheduling, side effects or changing medications as the primary reason for the consultation. It is hoped that this service has helped to strengthen links with GP practices.
Patients often feel comfortable discussing psychosocial impacts of their condition with a CNS who is knowledgeable about their condition. Courtenay and Carey’s11 review shows that education is a major role of CNS alongside the ability to prescribe. Four of the patients in this cohort who also attended psychological group sessions highlighted the value of a holistic multidisciplinary approach where all the staff have specialist knowledge about this rare condition. A recent report from the Danish Headache service also highlights that TN patients often consult the CNSs in the department but no further details about their specific role is provided.13
As well as highlighting the benefits of the service, the study also draws attention to areas for improvement; the responses received show that there is a desire for a more frequent service, which may be due to the nature of TN as it can become acute and severe very quickly. We have now been able to increase the number of CNS sessions which means regular reviews can also be a carried out rather than only dealing with patients requesting further help.
The survey suggested that although all patients were given written information about their drug use at their first consultation, it appears that this needs to be further supplemented by further instructions and more individualised regimes. Some patients still need to learn that anti-epileptic drugs are not taken as analgesics and equally GPs need to understand that patients need to have a flexible dosage scheme dependent on pain severity and side effects. A dosage escalation may be required very rapidly.
Limitations
One potential methodological flaw with this study was not being able to contact all the patients via telephone. Although, in such cases, patients were additionally sent questionnaires through the post, resulting in an 85% response rate, this may not be representative of the entire sample population. Moreover, discrepancies may have arisen in patient responses to the spoken versus written format of the questions; patients completing the questionnaire may have been at a disadvantage in terms of understanding certain questions, when compared with the interview patients, who were able to seek immediate clarification from the interviewer. However, patients who completed the written questionnaire may have been able to consult with other members of the household and reflected on their experience before providing answers. The study was carried out almost a year following the CNS-led telephone consultations and therefore the results may have been affected by the patient’s memory of the phone call, as well as their degree of honesty due to the self-reported nature of the questionnaire. Four patients had even forgotten that they had consulted the CNS.
To the wider society, a telephone clinic saves the patient money, such as transportation or child-care costs, and allows the patient to work on the day of the appointment, with only a pause required for a pre-arranged telephone consultation. Therefore, the CNS telephone service is both economically viable within the NHS, and for the wider society but it has not been possible to provide a monetary value for the current service.
Conclusion
The CNS service appears to decrease costly healthcare utilisation as patients report they would have used other services if the telephone clinic was not available; furthermore, patients required fewer face-to-face consultations with a TN specialist.
The service reduces costs for patients as they do not have to travel to attend appointments.
A CNS well-versed in TN can provide medical advice, education and support, so that patients report feeling more confident in pain management after the consultation.
Medicine management is facilitated as a nurse prescribing CNS can manage prescriptions, medication queries comprising of 42% of referrals. This is an important area for patient management.
The CNS acts as patient’s advocates to GPs and can ensure that prescriptions are issued in a timely and correct manner.
Overall, the surveyed patients found this service very helpful and suggested that it should be available more than once a week.
Acknowledgments
The authors are grateful to the reviewers for their helpful comments. JMZ undertook the work at UCL/UCLHT who received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centre funding scheme. AcaMedics UCL linked the two medical students T-YM and MH to the project.
Footnotes
Contributorship: The two medical students T-YM and MH phoned all the patients, AG provided the list of patients and the methodology and EH assessed the costs. JMZ oversaw the whole project and all contributed to the preparation and writing of the article.
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: This was part of an audit and all patients when registering at the Eastman Dental Hospital sign a general consent form to agree for their data to be used for teaching and research.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: JMZ is the guarantor of this study.
Informed consent: Patient were asked by telephone to give verbal consent.
ORCID iD: Joanna M Zakrzewska  https://orcid.org/0000-0001-7805-5851
https://orcid.org/0000-0001-7805-5851
References
- 1. Cruccu G, Finnerup NB, Jensen TS, et al. Trigeminal neuralgia: new classification and diagnostic grading for practice and research. Neurology 2016; 87(2): 220–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu TH, Hu LY, Lu T, et al. Risk of psychiatric disorders following trigeminal neuralgia: a nationwide population-based retrospective cohort study. J Headache Pain 2015; 16: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hall GC, Carroll D, Parry D, et al. Epidemiology and treatment of neuropathic pain: the UK primary care perspective. Pain 2006; 122(1–2): 156–162. [DOI] [PubMed] [Google Scholar]
- 4. Zakrzewska JM, Wu J, Mon-Williams M, et al. Evaluating the impact of trigeminal neuralgia. Pain 2017; 158(6): 1166–1174. [DOI] [PubMed] [Google Scholar]
- 5. Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ Clin Evid 2014; 348: g474. [DOI] [PubMed] [Google Scholar]
- 6. NICE. Neuropathic pain – pharmacological management (NICE Guideline 173). Report no. 2, November 2013, https://www.nice.org.uk/guidance/cg173/evidence/full-guideline-pdf-4840898221
- 7. Bendtsen L, Zakrzewska JM, Abbott J, et al. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol 2019; 26: 831–849. [DOI] [PubMed] [Google Scholar]
- 8. Besi E, Boniface DR, Cregg R, et al. Comparison of tolerability and adverse symptoms in oxcarbazepine and carbamazepine in the treatment of trigeminal neuralgia and neuralgiform headaches using the Liverpool Adverse Events Profile (AEP). J Headache Pain 2015; 16: 563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tentolouris-Piperas V, Lee G, Reading J, et al. Adverse effects of anti-epileptics in trigeminal neuralgiform pain. Acta Neurol Scand 2018; 137: 566–574. [DOI] [PubMed] [Google Scholar]
- 10. Kaasalainen S, Ploeg J, Donald F, et al. Positioning clinical nurse specialists and nurse practitioners as change champions to implement a pain protocol in long-term care. Pain Manag Nurs 2015; 16(2): 78–88. [DOI] [PubMed] [Google Scholar]
- 11. Courtenay M, Carey N. The impact and effectiveness of nurse-led care in the management of acute and chronic pain: a review of the literature. J Clin Nurs 2008; 17(15): 2001–2013. [DOI] [PubMed] [Google Scholar]
- 12. Stenner K, Carey N, Courtenay M. Prescribing for pain – how do nurses contribute? A national questionnaire survey. J Clin Nurs 2012; 21: 3335–3345. [DOI] [PubMed] [Google Scholar]
- 13. Heinskou TB, Maarbjerg S, Wolfram F, et al. Favourable prognosis of trigeminal neuralgia when enrolled in a multidisciplinary management program – a two-year prospective real-life study. J Headache Pain 2019; 20(1): 23. [DOI] [PMC free article] [PubMed] [Google Scholar]