Abstract
Background
An effective vaccine against Bordetella pertussis was introduced into the Expanded Programme on Immunisation (EPI) by WHO in 1974, leading to a substantial global reduction in pertussis morbidity and mortality. In low- and middle-income countries (LMICs), however, the epidemiology of pertussis remains largely unknown. This impacts negatively on pertussis control strategies in these countries. This study aimed to systematically and comprehensively review published literature on the burden of laboratory-confirmed pertussis in LMICs over the 45 years of EPI.
Methods
Electronic databases were searched for relevant literature (1974 to December 2018) using common and MeSH terms for pertussis. Studies using PCR, culture or paired serology to confirm Bordetella pertussis and parapertussis in symptomatic individuals were included if they had clearly defined numerators and denominators to determine prevalence and mortality rates.
Results
Eighty-two studies (49,167 participants) made the inclusion criteria. All six WHO regions were represented with most of the studies published after 2010 and involving mainly upper middle-income countries (n = 63; 77%). PCR was the main diagnostic test after the year 2000.
The overall median point prevalence of PCR-confirmed Bordetella pertussis was 11% (interquartile range (IQR), 5–27%), while culture-confirmed was 3% (IQR 1–9%) and paired serology a median of 17% (IQR 3–23%) over the period. On average, culture underestimated prevalence by 85% (RR = 0.15, 95% CI, 0.10–0.22) compared to PCR in the same studies.
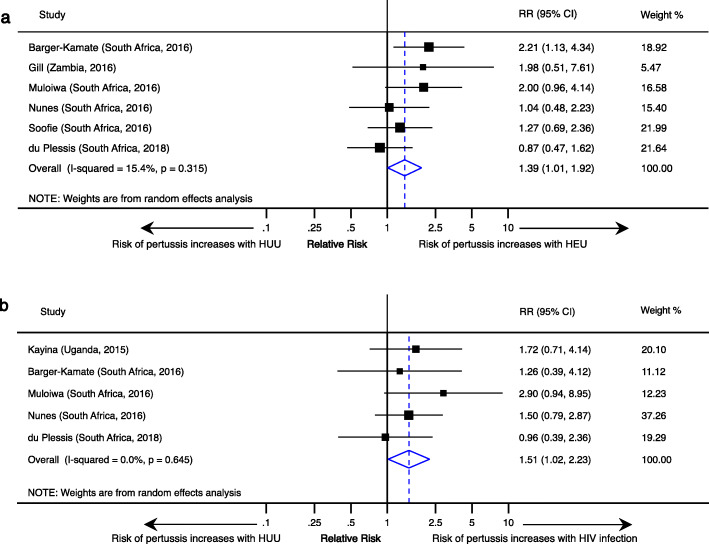
Risk of pertussis increased with HIV exposure [RR, 1.4 (95% CI, 1.0–2.0)] and infection [RR, 2.4 (95% CI, 1.1–5.1)]. HIV infection and exposure were also related to higher pertussis incidences, higher rates of hospitalisation and pertussis-related deaths.
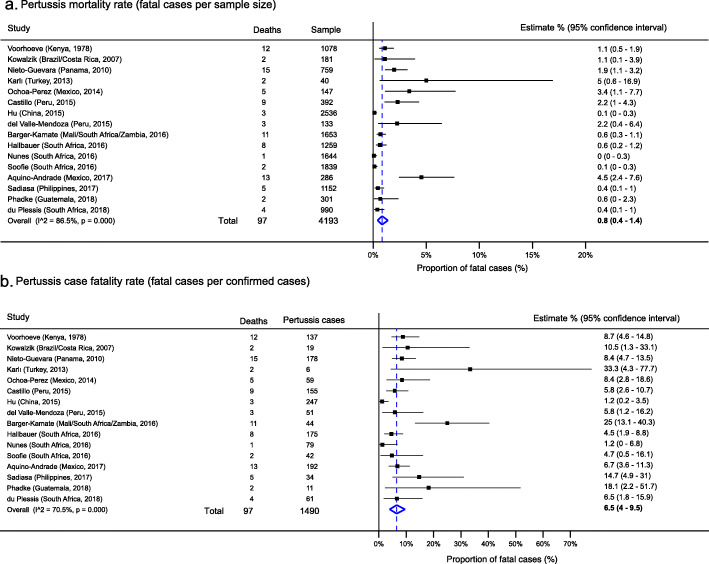
Pertussis mortality and case fatality rates were 0.8% (95% CI, 0.4–1.4%) and 6.5% (95% CI, 4.0–9.5%), respectively. Most deaths occurred in infants less than 6 months of age.
Conclusions
Despite the widespread use of pertussis vaccines, the prevalence of pertussis remains high in LMIC over the last three decades. There is a need to increase access to PCR-based diagnostic confirmation in order to improve surveillance. Disease control measures in LMICs must take into account the persistent significant infant mortality and increased disease burden associated with HIV infection and exposure.
Keywords: Pertussis, Burden, Prevalence, Incidence, Mortality, Case fatality, HIV, Low- and middle-income countries (LMIC)
Background
Pertussis is a highly infectious respiratory illness caused by Bordetella pertussis or Bordetella parapertussis. Using a model developed in 2003, the World Health Organization (WHO) estimated that in 2008 there were 20 to 40 million annual cases of pertussis. They further estimated that 90% of the cases and their 300,000 associated deaths occurred in low- and middle-income countries (LMICs) [1, 2]. An updated model by WHO estimated that 24.1 million cases of pertussis occurred in 2014 with 160,700 associated deaths in children under 5 years of age; a majority of these (58%) were estimated to have occurred in the African region and largely involved infants (53%) [3].
While there are good surveillance data to support the re-emergence of pertussis in high-income countries (HICs), the disease trends are unknown in LMICs due to the paucity of epidemiological data in these settings [4, 5]. A non-systematic review of available data for the African continent was published recently by the Global Pertussis Initiative (GPI) [6].
The high HIV prevalence estimates in LMICs coupled with suboptimal vaccine uptake are modifiable risk factors that can fuel high pertussis burdens [7, 8]. The pertussis resurgence reported lately in HICs has resulted in the review of disease control strategies in these countries [4, 9]. A review of existing pertussis control programmes in LMICs is yet to be undertaken.
The availability of an effective vaccine against Bordetella pertussis since the 1940s has led to a substantial global reduction in the morbidity and mortality caused by pertussis [10]. In 1974, WHO included the whole cell vaccine (wP) in the Expanded Programme on Immunisation (EPI) adopted in several countries. Although wP is still widely used in many LMICs, many HICs have replaced wP with various formulations of the acellular vaccine (aP) [11]. Epidemiological data from HICs show that despite high vaccine coverage with aP, the pertussis burden has increased in non-immunised and partially immunised infants, as well as in previously immunised adolescents and adults [4, 9, 12–14]. The reported pertussis resurgence has been linked to several factors such as reduced efficacy of aP vaccines and genetic evolution of the pertussis bacteria as well as improved diagnosis and reporting of the disease [5].
A sound understanding of trends in the burden of pertussis is required to assess the impact of current pertussis control strategies as well as to decide on future policy. We conducted a comprehensive systematic review to address the knowledge gap in the longitudinal epidemiology of pertussis in LMICs for the 45 years starting in 1974 to 2018, inclusive. Primarily, our systematic review aimed to review available published literature on the prevalence and/or incidence of laboratory-confirmed pertussis in LMICs since the inception of the EPI and to determine the trend in the burden of pertussis in LMICs from 1974. For secondary objectives, we sought to determine the mortality and case fatality rates ascribed to pertussis in LMICs, as well as to investigate the impact of vaccine choice, and HIV infection and in utero exposure on the burden of pertussis in LMICs over the review period.
Methods
Search strategy and criteria for selecting studies
The protocol for the systematic review was registered with PROSPERO International Prospective Register of systematic reviews (http://www.crd.york.ac.uk/PROSPERO), with registration CRD42015015159. The methods employed in conducting this review have been previously published [15]. The following electronic databases were searched for qualifying literature: MEDLINE, Scopus, Africa-Wide, PDQ-Evidence, WHOLIS, CINAHL, CENTRAL and Web of Science. Search terms used included “pertussis,” “Bordetella pertussis”, “Bordetella parapertussis” and “whooping cough” combined with “burden”, “epidemiology”, “incidence”, “prevalence” and “case”. These were used together with the specific names of all LMICs as classified by the World Bank [16, 17]. The search strategy as used in MEDLINE via PubMed is shown in Additional file 1. The reported search was carried out in April 2019. The World Bank groupings reflect the country status at this period.
The search was limited to studies published from 1974, the year that the EPI was introduced, until December 2018. Titles and abstracts of the search outputs and references were screened, and the full texts of potentially relevant articles were independently assessed by two reviewers (RM and BK) using a standardised score sheet. Disagreements on final inclusions were resolved by consensus following discussions involving a third reviewer (GH). Authors and publishers were contacted for full texts not available online or via our collaborative networks.
Studies were included if the study populations were from LMICs. While the diagnosis of pertussis is largely made on the basis of clinical parameters, it is well-known that clinical presentation may be modified by age, previous immunisation or infection, antibiotic exposure and concurrent infection with other pathogens [10]. This makes the presentation of pertussis frequently atypical, thus requiring laboratory confirmation of cases by serology, culture or polymerase chain reaction (PCR). Therefore, laboratory confirmation by either PCR, culture or paired serological assays was also an inclusion criterion.
Studies that failed to provide a numerator (number of participants testing positive) or denominator (number of participants tested for pertussis), as well as those that failed to specify the laboratory diagnostic method utilised, were excluded. Studies on sero-epidemiological and laboratory diagnostic methods in the absence of clinical disease were also excluded.
The systematic review included published randomised controlled trials, cross-sectional, cohort and surveillance studies. Case series and review articles were excluded as they failed to provide the required denominator.
Data extraction
The denominator and numerator were extracted from each study to determine the prevalence for each diagnostic method. We defined prevalence as proportions with confirmed laboratory diagnosis from all participants suspected and tested for pertussis. Bordetella pertussis prevalence data were stratified by WHO region, diagnostic method (culture, paired serology or PCR), clinical setting (hospital or population based) and age category of the study participants. Prevalence was further stratified by HIV status, that is HIV infected (HIV+), HIV-exposed uninfected (HEU) and HIV-unexposed uninfected (HUU). Incidence data were extracted as reported by the authors.
The epidemiology of Bordetella parapertussis was separately assessed. Data on the type of pertussis vaccine (wP or aP) used, clinical diagnostic criteria (e.g. WHO, Centers for Disease Control and Prevention (CDC), etc.) and the study design were captured.
Foreign language articles were reviewed, and data extracted with the assistance of online translation programmes and native speakers [18, 19].
Data analysis and reporting
Percentage point estimates together with their 95% confidence intervals (CIs) were calculated to represent the prevalence of laboratory-confirmed pertussis for all outcomes. The Mantel-Haenszel method was used to pool together prevalence data from individual studies using random-effects meta-analysis. Heterogeneity was evaluated both visually by assessing forest plots and formally using the χ2-based Q and I2 statistics [20]. Where a meta-analysis was not feasible, either because data were too heterogeneous or insufficient to allow for meaningful pooling, narrative reporting was used.
Narratively reported frequencies were summarised using medians and interquartile ranges (IQR) of prevalence point estimates and graphically represented using forest-like plots that omitted pooled data. Instead, dotted lines were used to indicate where group averages would lie without emphasising their meaning. The Kruskal-Wallis test was used to compare point prevalence between groups.
Mortality was defined as the proportion of deaths attributable to pertussis in the study sample while case fatality was defined as mortality attributable to the disease among confirmed cases of pertussis.
The incidence of pertussis could not be independently estimated as the requisite data was not available. Incidence was narratively reported per 100,000 as reported by the authors themselves.
All statistical analyses were done on STATA software version 14 (STATA Corporation, College Station, TX). The command metaprop_one was used to generate pooled prevalence forest plots after Freeman-Tukey transformation and metan, for comparative effect forest plots showing relative risks (RR) and their 95% CI, respectively.
The study utilised the guidelines for reporting systematic reviews as set down by the revised 2009 PRISMA Statement [21].
Quality of included studies
An adaptation of the tool developed by Wasserman et al. was used to assess the risk of bias as well as the quality of the included studies [22]. The quality assessment criteria examined specific variables to make judgement on the studies, taking into account methodological aspects discussed by Hoy et al. pertaining to internal and external validity of prevalence studies [23].
Results
Characteristics of the included studies
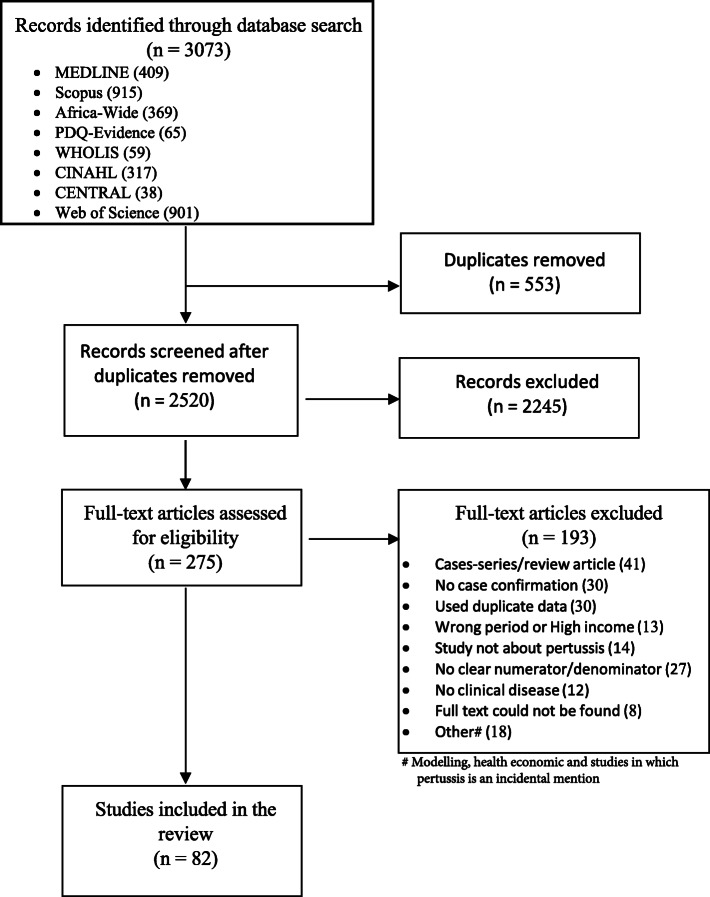
The search strategy returned 3186 studies which reduced to 2633 after excluding duplicates. Following screening of abstracts and titles, 275 articles were deemed potentially relevant and subjected to full-text evaluation. Eighty-two studies (n = 49,167) met the final criteria for inclusion into the systematic review (Fig. 1). Studies were excluded if they did not report clinical cases such as in laboratory studies, animal studies, economic evaluation and modelling studies. Other reasons for exclusions are shown in Fig. 1. The included studies involved symptomatic individuals meeting WHO and CDC (n = 52 and n = 8 respectively) clinical criteria. The remaining studies (n = 22) used clinical definitions derived from modifications of the criteria set by WHO or CDC. Two studies were multinational (two and seven countries in each) so that in the end the final 82 studies included, represented 88 unique populations [24, 25].
Fig. 1.
Studies included in the systematic review
Table 1 shows the characteristics of the included studies by WHO region. A large proportion of the studies (n = 63; 77%) was published between 2010 and 2018. Sixty-eight studies (83%) involved hospital-based participants. Forty-seven studies (57%) used one laboratory diagnostic confirmatory test while 32 (39%) and three (4%) studies used two and three methods for pertussis diagnosis, respectively.
Table 1.
Characteristics of studies included in the systematic review
| Region and study | Design | Setting | Diagnosis | Country | Vaccine | Period | Sample (cases) |
|---|---|---|---|---|---|---|---|
| Africa | |||||||
| Voorhoeve# (1978) [26] | Surveillance | Population | C, S | Kenya | wP | 1974–19077 | 1078 (138) |
| Ramkissoon (1991) [27] | Clinical trial | Population | S | South Africa | wP | 1988 | 112 (3) |
| Strebel (1991) [28] | Surveillance | Hospital | C, S | South Africa | wP | 1989 | 34 (3) |
| Simondon (1997) [29] | Clinical trial | Population | C, P, S | Senegal | wP and aP | 1990–1995 | 3619 (193) |
| Anukam# (2004) [30] | Cross-sectional | Hospital | C | Nigeria | wP | 1997–2000 | 296 (22) |
| Lassmann (2008) [31] | Cross-sectional | Hospital | P | Gabon | wP | 2003–2004 | 99 (6) |
| Jusot# (2014) [32] | Cross-sectional | Hospital | C, P | Niger | wP | 2010–2011 | 305 (34) |
| Kayina (2016) [33] | Cross-sectional | Hospital | P | Uganda | wP | 2013 | 449 (67) |
| Barger-Kamate (2016) [24] | Cross-sectional | Hospital | P | Multinational | wP and aP | 2011–2014 | 3451 (52) |
| Gill (2016) [34] | Cohort | Population | P | Zambia | wP | 2015 | 775 (10) |
| Hallbauer# (2016) [35] | Cross-sectional | Hospital | P | South Africa | aP | 2008–2015 | 1259 (183) |
| Muloiwa# (2016) [36] | Cross-sectional | Hospital | C, P | South Africa | aP | 2011–2012 | 460 (41) |
| Nunes (2016) [37] | Clinical trial | Population | P | South Africa | aP | 2011–2012 | 1644 (79) |
| Soofie (2016) [38] | Cross-sectional | Hospital | P | South Africa | aP | 2015 | 1839 (42) |
| Zar (2016) [39] | Cohort | Population | P | South Africa | aP | 2012–2014 | 284 (16) |
| du Plessis# (2018) [40] | Surveillance | Hospital | C, P | South Africa | aP | 2013–2015 | 990 (76) |
| Eastern Mediterranean | |||||||
| Al-Bargish# (1999) [41] | Cross-sectional | Hospital | C | Iran | wP | 1996 | 133 (67) |
| Kakar (2009) [42] | Surveillance | Hospital | C | Afghanistan | wP | 2006–2007 | 203 (7) |
| Ghanaie# (2010) [43] | Cross-sectional | Population | C, P | Iran | wP | 2007–2008 | 328 (27) |
| Bokhari# (2011) [44] | Cross-sectional | Hospital | C, P | Pakistan | wP | 2005–2009 | 802 (64) |
| Hajia (2012) [45] | Cross-sectional | Hospital | P | Iran | wP | 2008–2011 | 138 (12) |
| Mughal (2012) [46] | Cross-sectional | Hospital | C | Pakistan | wP | 2004–2006 | 700 (22) |
| Zouari# (2012) [47] | Cross-sectional | Hospital | C, P | Tunisia | wP | 2007–2011 | 599 (120) |
| Bahari (2013) [48] | Cross-sectional | Hospital | C | Iran | wP | 2008–2012 | 156 (7) |
| Nikbin (2013) [49] | Cross-sectional | Hospital | C, P | Iran | wP | 2009–2010 | 779 (100) |
| Saffar (2014) [50] | Cross-sectional | Hospital | P | Iran | wP | 2008–2012 | 518 (43) |
| Sedaghat# (2014) [51] | Cross-sectional | Hospital | C, P | Iran | wP | 2004–2008 | 347 (30) |
| Benamrouche (2016) [52] | Surveillance | Hospital | C, P | Algeria | wP | 2012–2013 | 246 (123) |
| Ghorbani (2016) [53] | Surveillance | Hospital | P | Iran | wP | 2011–2013 | 3629 (239) |
| Omer (2016) [54] | Surveillance | Hospital | P | Pakistan | wP | 2015–2016 | 2021 (8) |
| Katfy# (2017) [55] | Cross-sectional | Hospital | C, P | Morocco | wP | 2013–2015 | 156 (88) |
| Ben Fraji# (2018) [56] | Cross-sectional | Hospital | C, P | Tunisia | wP | 2007–2017 | 1844 (306) |
| Dumaidi (2018) [57] | Cross-sectional | Hospital | P | West Bank | wP | 2004–2008 | 267 (130) |
| Mohammadzadeh (2018) [58] | Cross-sectional | Hospital | C, P | Iran | wP | 2015–2016 | 184 (43) |
| Europe | |||||||
| Lukić-Grlić# (1999) [59] | Cross-sectional | Hospital | C, S | Croatia | wP | 1988–1994 | 201 (2) |
| Daǧla (2004) [60] | Cross-sectional | Hospital | C | Turkey | wP | 2001–2003 | 66 (2) |
| Aksakal (2007) [61] | Cross-sectional | Population | S | Turkey | wP | 2004 | 307 (51) |
| Yıldırım (2008) [62] | Cross-sectional | Hospital | P, S | Turkey | wP | 2005–2006 | 148 (16) |
| Medkova (2010) [63] | Cross-sectional | Unclear | C, P | Russian Fed. | wP | Unknown | 172 (81) |
| Gürsel (2012) [64] | Cross-sectional | Hospital | C, P, S | Turkey | aP | 2009–2010 | 51 (6) |
| Karlı (2013) [65] | Cross-sectional | Hospital | C, P | Turkey | aP | 2008–2012 | 40 (6) |
| Uslu (2013) [66] | Cross-sectional | Hospital | P | Turkey | aP | 2012 | 173 (48) |
| Dinu (2014) [67] | Cross-sectional | Hospital | C, P, S | Romania | aP | 2012–2013 | 51 (14) |
| Karagül (2014) [68] | Cross-sectional | Hospital | C, P | Turkey | aP | 2010–2011 | 214 (26) |
| Öksüz# (2014) [69] | Cross-sectional | Hospital | C, P | Turkey | aP | 2010–2013 | 410 (106) |
| Aslan (2016) [70] | Cross-sectional | Hospital | P | Turkey | aP | 2013–2014 | 101 (20) |
| Goktas (2016) [71] | Cross-sectional | Hospital | P | Turkey | aP | 2014–2015 | 845 (15) |
| Gökçe (2018) [72] | Cross-sectional | Hospital | P | Turkey | aP | 2013–2016 | 172 (44) |
| South-East Asia | |||||||
| Singh (1987) [73] | Cross-sectional | Hospital | C | India | wP | c.1986 | 560 (20) |
| Dahiya (2009) [74] | Cross-sectional | Hospital | C, P | India | wP | 2007–2007 | 21 (2) |
| Barger-Kamate (2016) [24] | Cross-sectional | Hospital | P | Multinational | wP | 2011–2014 | 749 (1) |
| Das (2016) [75] | Cross-sectional | Hospital | P | India | wP | 2013–2014 | 180 (7) |
| Siriyakorn (2016) [76] | Cross-sectional | Hospital | P | Thailand | wP | 2010–2011 | 76 (14) |
| Hughes# (2017) [77] | Cohort | Population | P | Nepal | wP | 2011–2014 | 2026 (17) |
| Chinthate (2018) [78] | Cross-sectional | Hospital | P | Thailand | wP | 2016–2017 | 70 (7) |
| The Americas | |||||||
| Cooper (1983) [79] | Surveillance | Hospital | C, S | St Lucia | wP | 1981 | 10 (2) |
| Baptista (2006) [80] | Cross-sectional | Hospital | C | Brazil | wP | 2003 | 287 (51) |
| Kowalzik (2007) [25] | Cross-sectional | Hospital | P | Multinational | wP and aP | 2001–2004 | 181 (19) |
| Sandoval (2008) [81] | Cross-sectional | Population | P | Mexico | wP | 2002–2003 | 61 (20) |
| Nieto Guevara (2010) [82] | Surveillance | Hospital | C, P | Panama | wP and aP | 2001–2008 | 759 (178) |
| Astudillo (2011) [83] | Cross-sectional | Hospital | C, P | Colombia | wP | 2006–2007 | 133 (45) |
| Leite (2012) [84] | Surveillance | Hospital | C | Brazil | wP | 2006–2008 | 652 (132) |
| Ferronato (2013) [85] | Cohort | Hospital | C, P | Brazil | wP | 2009–2012 | 57 (25) |
| Ochoa-Perez (2014) [86] | Surveillance | Hospital | C, P | Mexico | aP | 2011–2012 | 147 (59) |
| Vaz-de-Lima (2014) [87] | Surveillance | Hospital | P | Brazil | wP | 2009–2012 | 503 (66) |
| Castillo (2015) [88] | Cross-sectional | Hospital | P | Peru | wP | 2010–2012 | 392 (155) |
| Pavic-Espinoza (2015) [89] | Cross-sectional | Hospital | P | Peru | wP | 2009–2010 | 596 (114) |
| Pimentel (2015) [90] | Cross-sectional | Hospital | C, P | Brazil | wP | 2010–2011 | 192 (10) |
| del Valle-Mendoza (2015) [91] | Cross-sectional | Hospital | P | Peru | wP | 2010–2013 | 133 (51) |
| Bailon# (2016) [92] | Cross-sectional | Hospital | C, P | Peru | wP | 2012 | 840 (191) |
| Aquino-Andrade# (2017) [93] | Cross-sectional | Hospital | P | Mexico | aP | 2011–2014 | 286 (192) |
| Phadke (2018)# [94] | Cross-sectional | Hospital | P | Guatemala | wP | 2009–2012 | 301 (11) |
| del Valle-Mendoza (2018) [95] | Cross-sectional | Hospital | P | Peru | wP | 2016–2017 | 88 (18) |
| Western Pacific | |||||||
| Ong (1978) [96] | Cross-sectional | Hospital | C | Malaysia | wP | 1974 | 65 (1) |
| Lin (2010) [97] | Cross-sectional | Hospital | C, P | China | wP | 2008–2009 | 1001 (99) |
| Mi (2013) [98] | Cross-sectional | Hospital | P | China | wP | 2011–2012 | 176 (51) |
| Ting (2013) [99] | Cross-sectional | Hospital | C, P | Malaysia | wP | 2011 | 707 (275) |
| Huang (2014) [100] | Surveillance | Population | P | China | wP and aP | 2010–2012 | 1022 (113) |
| Liu (2014) [101] | Cross-sectional | Hospital | C, P | China | wP | 2013 | 148 (101) |
| Wang (2014) [102] | Cross-sectional | Hospital | C, P | China | wP and aP | 2012–2013 | 313 (122) |
| Hu (2015) [103] | Cross-sectional | Hospital | P | China | aP | 2013–2014 | 2536 (247) |
| Moriuchi (2017) [104] | Cross-sectional | Unclear | P | Cambodia | wP | 2008–2016 | 651 (82) |
| Sadiasa (2017) [105] | Cross-sectional | Hospital | P | Philippines | wP | 2012–2015 | 1152 (34) |
C culture, P polymerase chain reaction, S paired serology, wP whole cell vaccine, aP acellular vaccine
#Includes Bordetella parapertussis. NB. Cooper, Strebel and Al-Bargish conducted in outbreak settings
Study designs included three clinical trials, four cohorts, 62 cross-sectional and 13 surveillance studies. There were 71 studies published in English, four in Mandarin, three each in Spanish and Turkish and one in Persian. Three studies by Cooper and Fitch, Strebel et al. and Al-Bargish et al. were conducted in outbreak settings [28, 41, 79].
In total, the studies originated from 37 countries, representing all six WHO regions (Additional file 2). Nineteen (51%) of the countries represented were upper middle-income, while 11 (30%) and seven (19%) were lower middle- and low-income countries, respectively. Five countries contributed 28 (49%) of the studies (Turkey = 11, Iran = 9, South Africa = 8, China = 6 and Brazil = 6). Sixty-four (78%) studies had epidemiological data for Bordetella pertussis only while 18 (22%) studies investigated for both Bordetella pertussis and Bordetella parapertussis. The most frequently used vaccine over the period the included studies were conducted was wP in 72/88 (82%) settings either on its own (n = 66) or in combination with aP (n = 6). In 16 (18%) settings, aP was the only vaccine in use.
Data from a study by Zouari et al. was considered only for the purpose of estimating mortality but not for estimation of disease burden as its data overlapped with that of Ben Fraj et al. who reported cases over a longer period but did not report on mortality [47, 56].
Prevalence of pertussis
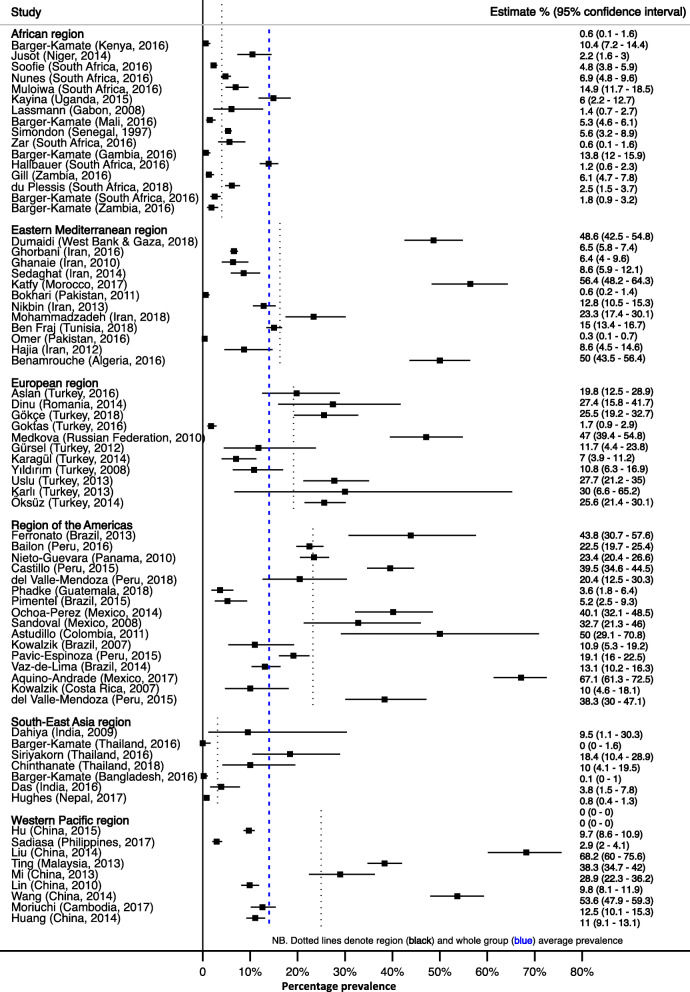
The median prevalence of PCR-confirmed disease due to Bordetella pertussis was 11% (IQR, 5–27%; n = 43,696, 64 studies) (Fig. 2 and Additional file 3). PCR prevalence differed across WHO regions ranging from a median of 4% (IQR 4–10%) in South-East Asia to a median of 22% (IQR 12–40%) in the Region of the Americas, P = 0.001. In one multinational study, conducted in countries in the Africa and South-East Asia regions, Barger-Kamate et al. found an increased risk for pertussis in African countries with an adjusted odds ratio of 8.8 (P = 0.03) [24].
Fig. 2.
Prevalence of polymerase chain reaction-confirmed Bordetella pertussis. Dotted lines show subgroup and whole group average estimates
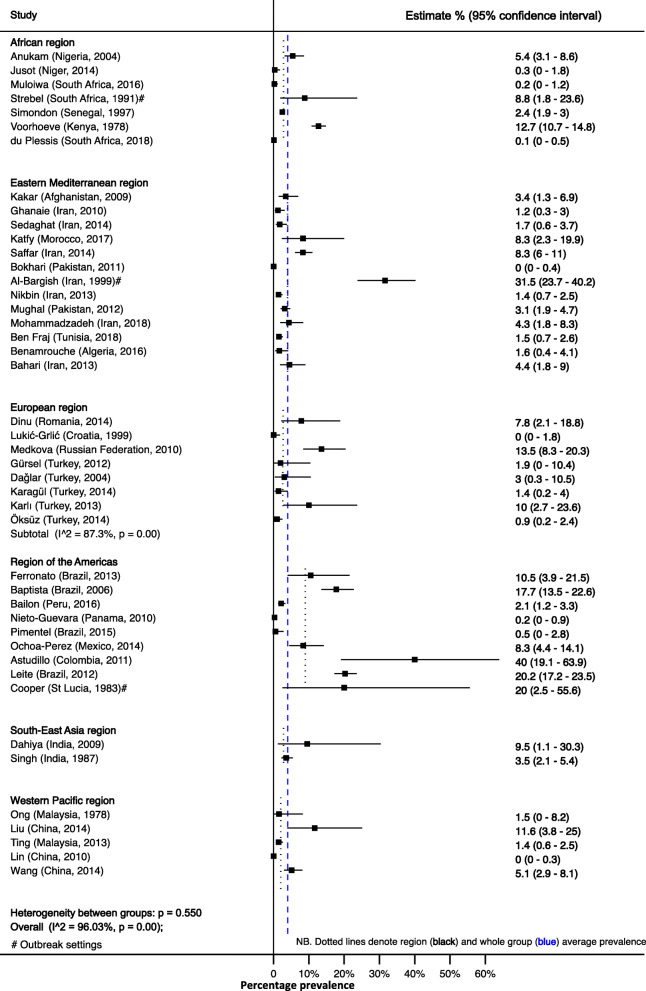
The median prevalence of culture-confirmed Bordetella pertussis was 3% (IQR 1–9%) (n = 18,868, 44 studies). The point prevalence was similar across WHO regions, P = 0.1380 (Fig. 3 and Additional file 2).
Fig. 3.
Prevalence of culture-confirmed Bordetella pertussis. Dotted lines show subgroup and whole group average estimates
Confirmation of Bordetella pertussis using paired serology showed a median of 17% (IQR 3–23%; n = 4912, 9 studies). Only three WHO regions were represented, and the median prevalence was 3% (IQR 3–13%) in the African region and 17% (95% CI, 13–26%) in the European region, while the one country, St Lucia, representing the Region of the Americas had a prevalence of 44% (95% CI, 14–79%), P = 0.1309 (Additional file 3 and Additional file 4).
The prevalence of confirmed Bordetella parapertussis infection using any of the three confirmatory methods was 1% (IQR, 0–2%; n = 12,062, 18 studies). The Eastern Mediterranean region was noted to have the highest prevalence with a median 2% (IQR 0–7%) with one study from the same region having a prevalence of 19% (95% CI 13–26%) [41] (Additional file 5).
The prevalence of Bordetella pertussis differed in the same population depending on the method of laboratory confirmation used. On average, culture underestimated prevalence by 85% (RR = 0.15, 95% CI, 0.10–0.22) compared to PCR in the 29 (n = 14,315) studies that used both methods (Additional file 6).
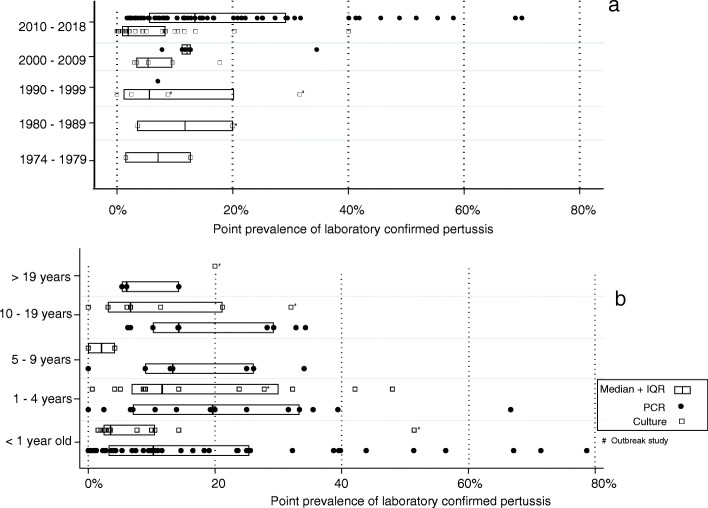
Pertussis prevalence declined in the 1990s from the levels seen in the 1970s and 1980s. A slight increase was noted since the period after 2000 (Fig. 4a). Huang et al. reported a 26-fold increase in confirmed adult pertussis between 2010 and 2014 in China [100]. There was sufficient information in 48 studies to estimate age prevalence by age group. The lowest prevalence was noted in individuals older than 19 years with a median prevalence of 6% (IQR 5–14%). After the high prevalence noted below 5 years of age, the risk declined in late childhood (6 to 10 years) but increased again in adolescents who showed the highest prevalence of all groups with a median prevalence of 20% (IQR 14–32%) (Fig. 4b).
Fig. 4.
Distribution of point prevalence of polymerase chain reaction- and culture-confirmed pertussis by period (a) and age group (b)
Pertussis prevalence was also stratified by the study setting (hospital versus population based) as well as by the type of vaccine used in settings where the included studies were conducted. The prevalence of pertussis in hospital-based studies had a median of 10% (IQR 4–25%) compared to population-based studies which reported a median prevalence of 6% (IQR 3–13%). There was an overlap in the distribution of prevalence of confirmed pertussis in populations using aP only [median 10% (IQR 6–28%)] compared to populations using some wP [median 10% (IQR 3–20%)]. The overlap remained even when prevalence was stratified by the diagnostic method. In the only included clinical trial comparing the two vaccine types, Simondon et al. found aP vaccine efficacy against all confirmed pertussis to be 85% (95% CI, 66–93%) and that of wP to be 96% (95% CI, 86–99%) [29].
Incidence of pertussis
Population-level incidence rates of pertussis and hospitalisation were reported by some of the authors, but these could not be independently verified as the requisite population data were not available (Table 2). In addition, a majority of the authors reported point estimate incidences with no confidence intervals. Where data was available for different age groups (Voorhoeve et al., Nieto Guevara et al., Saffar et al. and Ochoa-Perez et al.), the incidence was always highest in infancy [26, 50, 82, 86]. The highest incidence of 15,900/100000 was reported in Kenyan infants between 1974 and 1977 [26]. In addition to Bordetella pertussis incidence, Ghanaie et al. reported a separate incidence of 2 per 100,000 for Bordetella parapertussis [43]. Contacts were reported to have an incidence of 0.69/100000 in Benamrouche et al.’s study [52].
Table 2.
Population and hospitalisation incidence rates of Bordetella pertussis
| Study (year) | Incidence | Age ranges | Country |
|---|---|---|---|
| Voorhoeve (1978) [26] | 3800/100000 | All ages | Kenya |
| Strebel# (1991) [28] | 187/100000 | 6 months to 5 years | South Africa |
| Simondon (1997) [29] | 119/100000 | 2 months to 15 years | Senegal |
| Sandoval (2008) [81] | 500/100000 | 12 to 15 years | Mexico |
| Ghanaie (2010) [43] | 318/100000 | 6 to 14 years | Iran |
| Nieto Guevara# (2010) [82] | 144/100000 | All ages | Panama |
| Uslu (2013) [66] | 0.9/100000 | < 5 years | Turkey |
| Huang (2014) [100] | 23.52/100000 | All ages | China |
| Jusot (2014) [32] | 820/100000 | < 5 years | Niger |
| Ochoa-Perez (2014) [86] | 2.3/100000 | 0 to > 18 years | Mexico |
| Saffar (2014) [50] | 4.92/100000 | 0 month to 25 years | Iran |
| Benamrouche (2016) [52] | 1.04/100000 | All ages | Algeria |
| Gill (2016) [34] | 520/100000 | < 1 year | Zambia |
| Muloiwa# (2016) [36] | 526/100000 | < 13 years | South Africa |
| Omer (2016) [54] | 247/100000 | < 1 year | Pakistan |
| Soofie (2016) [38] | 220/100000 | < 1 year | South Africa |
| Giayetto (2017) [106] | 4.53/100000 | All ages | Argentina |
| Ben Fraj (2018) [56] | 134/100000 | < 5 years | Tunisia |
#Incidence represents hospitalisation rates for pertussis
Time-denominated rates were recorded for three studies. Gill et al. reported a rate of 2.4 (95% CI, 1.2–4.2) cases per 1000 infant-months with the highest rate of 3.5 cases/1000 infant-months noted between birth and 6 weeks, while Hughes et al. reported a rate of 13.3 (95% CI, 7.7–21.3) cases per 1000 infant-years [34, 77]. Nunes et al.’s data gave an overall rate of 4.9 per 1000 person-months, which differed between infants (5.7/1000) and mothers (4.3/1000) as well as by HIV status as reported below [37].
Risk of pertussis in HIV exposed and infected
Ten studies, all from the Africa region, investigated the impact of HIV status on the risk of pertussis. The incidence rate of pertussis was 7.4/1000 infant-months in HEU infants and 5.5/1000 in HUU infants in the study by Nunes et al., while the rates in HIV+ and HIV uninfected mothers were 6.8 and 3.9/1000, respectively [37]. Gill et al. reported RR 1.8 (95% CI, 95% CI 0.5–6.9) in HEU infants compared to HUU. The incidence of Bordetella pertussis-associated hospitalisation was 2.9 (95% CI, 1.8–4.5) and 1.9 (95% CI, 1.3–2.6) per 1000 in HIV-exposed and HIV-unexposed infants, respectively, in a study by Soofie et al. The reported 4.8% case fatality rate in Soofie et al. was only due to deaths in HIV-exposed infants [38]. In the study by Hallbauer et al., there was insufficient data to estimate stratum-specific rates, but HIV+ cases, who made 14% of the study sample, accounted for 22 (19%) of the 113 pertussis cases with known HIV status [35]. A gradual increase in risk of pertussis was reported in a study by Muloiwa et al. in which the risk of pertussis was 5.4% in HUU, 10.9% in HEU and 15.8% in HIV+ [36].
There was sufficient data to do a meta-analysis comparing risk of pertussis in HUU with HEU and HIV+ in six and five studies, respectively. Compared to HUU, HIV+ and HEU individuals had a RR 1.51 (95% CI, 1.02–2.23) and RR 1.4 (95% CI, 1.01–1.92) for confirmed pertussis, respectively (Fig. 5). The highest risk of pertussis was reported by Anukam et al., in a cohort of wP-vaccinated HIV-infected adolescents who were not on antiretroviral therapy with RR 22.8 (95% CI, 6.9–75.1) [30]. This study was not included in the HIV meta-analysis as it was an obvious outlier composed of individuals not on treatment which seemed to show excessive risk for pertussis. All other studies involved HIV+ individuals on antiretroviral therapy.
Fig. 5.
Meta-analysis of the relative risk of pertussis comparing HIV-unexposed uninfected (HUU) to HIV-exposed uninfected (HEU) (a) and HIV infected (b)
Mortality rate and case fatality rate of pertussis
A total of 97 pertussis-related deaths out of 1490 confirmed cases were reported in 16 studies (n = 14,390) representing 13 countries. All deaths were associated with Bordetella pertussis with none attributed to Bordetella parapertussis. From the 16 studies, the overall mortality rate was 0.8% (95% CI, 0.4–1.5%) with a pertussis case fatality rate of 5.5% (95% CI, 3.3–6.1%) (Fig. 6). When only infants were considered (13 studies), the case fatality rate was 7.2% (95% CI, 3.6–11.8%) in the studies reporting deaths.
Fig. 6.
Mortality and case fatality rate of confirmed pertussis
All children who died were younger than 5 years and the majority were younger than 6 months of age. Almost all deaths occurred under 1 year of age with only one study (Voorhoeve et al.) reporting pertussis deaths after the second year of life (n = 5) [26].
Quality of the included studies
Using the modified tool published with the protocol for this systematic review, we found all the included studies to be of high quality [15]. This is because components of the quality index score, such as laboratory confirmation and availability of raw denominator and numerator data formed part of the inclusion criteria, which automatically excluded poor-quality studies. Similarly, studies had moderate to low risk of attrition and selection bias.
Discussion
This study comprehensively reports on the burden of confirmed pertussis over a 45-year period (1974–2018) in LMICs. This period starts in 1974 with the inception of EPI. The prevalence of confirmed pertussis disease differed in the same study depending on the method of laboratory confirmation with PCR showing the greatest diagnostic sensitivity as expected [5]. Most cases were due to Bordetella pertussis. Bordetella parapertussis was less common and did not have any reported fatalities associated with it. The study indicates that pertussis deaths are significantly high in LMICs with a disproportionate case fatality rate in young infants. Secondly, the meta-analysis shows that HIV has a significant impact in the burden of pertussis in settings where the burden of HIV is high.
Not surprisingly, the findings from our study agree with those from some HICs: the highest incidence of pertussis was in infants and the greatest pertussis-specific mortality in children younger than 6 months [107–109]. Moreover, we also noted the increase in the prevalence of pertussis in adolescents similarly described in highly vaccinated cohorts from HICs [110–112]. The noted decline in adulthood may indicate protection following the natural boosting in adolescence. Worryingly, the pooled case fatality rate of nearly 6% exceeds the less than 4% estimated by WHO for developing countries [2]. As noted, this is even higher when only infants are considered.
The prevalence data presented in this systematic review suggests that LMICs may also be experiencing a resurgence of pertussis as noted in HICs. Both the GPI and WHO advocate for the strengthening of surveillance systems as a key component in the control of pertussis [110, 113]. Currently, surveillance of pertussis in LMICs is suboptimal. As a result, there are many gaps in accurate pertussis epidemiological data which we observed in this study. The review indicates that the choice of laboratory case confirmation influences the quantification of pertussis disease burden within the same setting. This is an important finding that suggests that the use of PCR to confirm pertussis should be prioritised in LMICs. The higher sensitivity of PCR is more likely to capture the true burden of pertussis and give a better understanding of the global epidemiological pattern of the disease across different settings than any other method. In contrast, culture, recognised as the diagnostic gold standard, missed on average 85% of cases identified by PCR in the studies that used both methods in this systematic review. Higher culture prevalence estimates than in other studies in a similar WHO group were noted when the studies were conducted before a vaccination programme was fully established (Voorhoeve et al.), during an outbreak (Cooper and Fitch [79]; Strebel et al.; and Al-Bargish) and when the study included secondary attack data of close contacts (Astudillo et al.) [26, 28, 41, 83].
A number of authors reported incidences although population denominators could not be independently verified as these went largely unreported. The rates were quite high compared to HICs and showed no pattern of decline over the period in which the incidences were reported.
An unexpected finding was the significant overlap in the prevalence of pertussis noted with different vaccines in use. Most LMICs use wP vaccines in contrast with the predominant use of aP vaccines in HICs. In general, wP vaccines are regarded as offering better protection against pertussis [114]. Despite the predominant use of wP in the reviewed studies, we noted a steady increase in confirmed pertussis in studies reporting after 2000. This suggests that the observed resurgence of pertussis noted in HIC may only be partly explained by the change of vaccine from wP to aP in these countries. Another possible explanation for the increase may be the increase in the use of PCR for case confirmation—all the included studies conducted after 2010 used PCR as the primary method of confirming cases. The increase in the observed prevalence coincides with the use of these molecular techniques.
Although data are limited by the number of countries reporting HIV status, there is strong evidence from the meta-analysis showing that the risk of pertussis is increased in HIV+ and HEU individuals. The risk of pertussis was increased by 50% and 40% respectively in the two groups compared to HUU. With the exception of the study by du Plessis et al., all studies showed an increased risk of pertussis incidence or prevalence associated with HIV infection or exposure [40]. In addition, there was a higher risk of hospitalisation and deaths related to pertussis in HIV-exposed or HIV-infected infants [34, 37, 38]. In considering their pertussis control strategies, LMICs, which have the biggest burden of HIV, need to take into account this increased risk associated with HIV exposure and infection [8].
Our study is largely limited by paucity of data, especially longitudinal data for each included country as well as vaccine coverage and number of vaccine doses received in the specific population studied. The available data was disproportionately provided by only a few upper middle-income countries. A further limitation is the case detection that may have been affected by the variability of PCR assays used. In particular, this is noted with respect to our inability to assess the sensitivity and specificity of each assay. Regardless, our results will encourage generation of more epidemiological studies on pertussis in LMICs, while in the meantime, assisting policy makers in disease control planning.
Conclusions
Immunisation remains suboptimal with vaccine coverage with the three infant doses (DPT3) remaining low in LMIC in general and in low-income countries, in particular [115]. Even where vaccine coverage with DPT3 is acceptable, the doses are not often received in a timely manner, undermining the protective effect of the vaccine on young infants [116, 117]. Unlike in HIC countries in which re-emergence of pertussis may be related to low and delayed vaccine coverage secondary to vaccine hesitancy, in LMIC, this usually reflects the lack of administrative capacity [118]. This study indicates an urgent need to review and strengthen the existing pertussis control programmes in LMICs to target children, adolescents and HIV-exposed and HIV-infected groups. In addition, the study highlights the need to urgently consider measures to reduce the high infant mortality rate, with specific consideration for maternal vaccination. There is now strong evidence to showing that immunisation of pregnant women, even when given as early as the second trimester, is safe for both the mother and the foetus and induces sufficient transplacental antibodies to protect the young infant still too young to complete primary immunisation schedule for pertussis [119, 120]. In their recommendation, the GPI in addition to prioritising surveillance and increasing overall vaccine coverage made this an urgent area of action for LMICs [6]. Encouragingly, we noted a substantial increase in the number of studies published in the last 8 years of the period under review (2010–2018), possibly reflecting recent increase in interest and funding for pertussis research in LMICs.
Supplementary information
Additional file 1: Table: Strategy used to search for literature in MEDLINE (Via Pubmed).
Additional file 2. Country and year of included studies with confirmed pertussis shown by World Health Organisation region.
Additional file 3. Distribution of point prevalence of confirmed pertussis by World Health Organisation region and confirmation method [PCR = polymerase chain reaction].
Additional file 4 Prevalence of paired serology confirmed Bordetella pertussis. Dotted lines show subgroup and whole group average estimates.
Additional file 5 Prevalence of polymerase chain reaction and culture confirmed Bordetella parapertussis. Dotted line shows group average estimate [# Culture confirmed].
Additional file 6. Meta-analysis of relative detection rates of polymerase chain reaction (PCR) and culture in confirming Bordetella pertussis infection.
Acknowledgements
The authors wish to thank Drs Tunc Numanoglu and Nei-yuan Hsiao for assisting with translation of non-English full texts.
Abbreviations
- aP
Acellular vaccine
- CDC
Centers for Disease Control and Prevention
- CIs
Confidence intervals
- EPI
Expanded Programme on Immunisation
- GPI
Global Pertussis Initiative
- HEU
HIV-exposed uninfected
- HICs
High-income countries
- HIV+
HIV infected
- HUU
HIV-unexposed uninfected
- IQR
Interquartile range
- LMICs
Low- and middle-income countries
- PCR
Polymerase chain reaction
- RR
Relative risks
- WHO
World Health Organization
- wP
Whole cell vaccine
Authors’ contributions
RM conceived the research project, extracted the data, designed and executed the analyses, interpreted the findings, wrote the first draft and revised drafts of the manuscript. BK contributed to the search strategy, study selection and revision of manuscript. ME revised drafts of the report and contributed to the interpretation of the findings. GH contributed to the interpretation of the findings and supervised the research project. The authors read and approved the final manuscript.
Funding
No funding was received for the submitted work.
Availability of data and materials
All data generated or analysed during this study are included in this published article and in the reference list provided, all of which are in the public domain.
Ethics approval and consent to participate
The study did not recruit participants. As the study employed a secondary analysis of data already in the public domain, no Institutional Review Board or Ethics Committee was approached to give approval for this study.
Consent for publication
No consent for publication was required. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12916-020-01699-3.
References
- 1.Crowcroft NS, Stein C, Duclos P, Birmingham M. How best to estimate the global burden of pertussis? Lancet Infect Dis. 2003;3(7):413–418. doi: 10.1016/s1473-3099(03)00669-8. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Managing pertussis outbreaks during humanitarian emergencies : WHO technical note, February 2008. Geneva: World Health Organization; 2008. [Google Scholar]
- 3.Yeung KHT, Duclos P, Nelson EAS, Hutubessy RCW. An update of the global burden of pertussis in children younger than 5 years: a modelling study. Lancet Infect Dis. 2017;17(9):974–980. doi: 10.1016/S1473-3099(17)30390-0. [DOI] [PubMed] [Google Scholar]
- 4.Cherry JD. Pertussis: challenges today and for the future. PLoS Pathog. 2013;9(7):e1003418. doi: 10.1371/journal.ppat.1003418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood N, McIntyre P. Pertussis: review of epidemiology, diagnosis, management and prevention. Paediatr Respir Rev. 2008;9(3):201–211. doi: 10.1016/j.prrv.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Muloiwa R, Wolter N, Mupere E, Tan T, Chitkara AJ, Forsyth KD, von Konig CW, Hussey G. Pertussis in Africa: findings and recommendations of the Global Pertussis Initiative (GPI) Vaccine. 2018;36(18):2385–2393. doi: 10.1016/j.vaccine.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Machingaidze S, Wiysonge CS, Hussey GD. Strengthening the expanded programme on immunization in Africa: looking beyond 2015. PLoS Med. 2013;10(3):e1001405. doi: 10.1371/journal.pmed.1001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UNAIDS Data; 2017. https://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf. Accessed 3 July 2020.
- 9.Clark TA. Changing pertussis epidemiology: everything old is new again. J Infect Dis. 2014;209(7):978–981. doi: 10.1093/infdis/jiu001. [DOI] [PubMed] [Google Scholar]
- 10.Cherry JD, Tan T, Wirsing von Konig CH, Forsyth KD, Thisyakorn U, Greenberg D, Johnson D, Marchant C, Plotkin S. Clinical definitions of pertussis: summary of a Global Pertussis Initiative roundtable meeting, February 2011. Clin Infect Dis. 2012;54(12):1756–1764. doi: 10.1093/cid/cis302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L, Prietsch SO, Axelsson I, Halperin SA. Acellular vaccines for preventing whooping cough in children. Cochrane Database Syst Rev. 2014;9:Cd001478. doi: 10.1002/14651858.CD001478.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wendelboe AM, Njamkepo E, Bourillon A, Floret DD, Gaudelus J, Gerber M, Grimprel E, Greenberg D, Halperin S, Liese J, et al. Transmission of Bordetella pertussis to young infants. Pediatr Infect Dis J. 2007;26(4):293–299. doi: 10.1097/01.inf.0000258699.64164.6d. [DOI] [PubMed] [Google Scholar]
- 13.Jardine A, Conaty SJ, Lowbridge C, Staff M, Vally H. Who gives pertussis to infants? Source of infection for laboratory confirmed cases less than 12 months of age during an epidemic, Sydney, 2009. Commun Dis Intell Q Rep. 2010;34(2):116–121. [PubMed] [Google Scholar]
- 14.von Konig CH, Halperin S, Riffelmann M, Guiso N. Pertussis of adults and infants. Lancet Infect Dis. 2002;2(12):744–750. doi: 10.1016/s1473-3099(02)00452-8. [DOI] [PubMed] [Google Scholar]
- 15.Muloiwa R, Kagina BM, Engel ME, Hussey GD. The burden of pertussis in low- and middle-income countries since the inception of the Expanded Programme on Immunization (EPI) in 1974: a systematic review protocol. Syst Rev. 2015;4:62. doi: 10.1186/s13643-015-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Country and Lending Groups. http://data.worldbank.org/about/country-and-lending-groups. Accessed 3 July 2020.
- 17.What is the World Bank Atlas method? https://datahelpdesk.worldbank.org/knowledgebase/articles/378832-what-is-the-world-bank-atlas-method. Accessed 3 July 2020.
- 18.Google Translate. https://translate.google.com. Accessed 3 July 2020.
- 19.DocTranslator. https://www.onlinedoctranslator.com/translationform. Accessed 3 July 2020.
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wasserman S, Engel ME, Mendelson M. Burden of pneumocystis pneumonia in HIV-infected adults in sub-Saharan Africa: protocol for a systematic review. Syst Rev. 2013;2:112. doi: 10.1186/2046-4053-2-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 24.Barger-Kamate B, Deloria Knoll M, Kagucia EW, Prosperi C, Baggett HC, Brooks WA, Feikin DR, Hammitt LL, Howie SR, Levine OS, et al. Pertussis-associated pneumonia in infants and children from low- and middle-income countries participating in the PERCH study. Clin Infect Dis. 2016;63(suppl 4):S187–s196. doi: 10.1093/cid/ciw546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kowalzik F, Barbosa AP, Fernandes VR, Carvalho PR, Avila-Aguero ML, Goh DY, Goh A, de Miguel JG, Moraga F, Roca J, et al. Prospective multinational study of pertussis infection in hospitalized infants and their household contacts. Pediatr Infect Dis J. 2007;26(3):238–242. doi: 10.1097/01.inf.0000256750.07118.ee. [DOI] [PubMed] [Google Scholar]
- 26.Voorhoeve AM, Muller AS, Schulpen TWJ, t’ Mannetje W, van Rens M. Machakos project studies. Agents affecting health of mother and child in a rural area of Kenya. IV: the epidemiology of pertussis. Trop Geogr Med. 1978;30(1):125–139. [PubMed] [Google Scholar]
- 27.Ramkissoon A, Coovadia HM, Loening WEK, Ndlovana M. Does whole-cell pertussis vaccine protect black South African infants? Assessment of post-vaccination events and antibody responses to pertussis toxin, filamentous haemagglutinin and agglutinogens 2 and 3. S Afr Med J. 1991;79(11):645–649. [PubMed] [Google Scholar]
- 28.Strebel P, Hussey G, Metcalf C, Smith D, Hanslo D, Simpson J. An outbreak of whooping cough in a highly vaccinated urban community. J Trop Pediatr. 1991;37(2):71–76. doi: 10.1093/tropej/37.2.71. [DOI] [PubMed] [Google Scholar]
- 29.Simondon F, Preziosi MP, Yam A, Kane CT, Chabirand L, Iteman I, Sanden G, Mboup S, Hoffenbach A, Knudsen K, et al. A randomized dowble-blind trial comparing a two-component acellular to a whole-cell pertussis vaaccine in Senegal. Vaccine. 1997;15(15):1606–1612. doi: 10.1016/s0264-410x(97)00100-x. [DOI] [PubMed] [Google Scholar]
- 30.Anukam KC, Osazuwa EE, Mbata TI, Ahonkhai IN. Increased incidence of pertussis and parapertussis in HIV-1-positive adolescents vaccinated previously with whole-cell pertussis vaccine. World J Microbiol Biotechnol. 2004;20(3):231–234. [Google Scholar]
- 31.Lassmann B, Poetschke M, Ninteretse B, Issifou S, Winkler S, Kremsner PG, Graninger W, Apfalter P. Community-acquired pneumonia in children in Lambarene, Gabon. Am J Trop Med Hyg. 2008;79(1):109–114. [PubMed] [Google Scholar]
- 32.Jusot V, Aberrane S, Ale F, Laouali B, Moussa I, Alio SA, Adehossi E, Collard JM, Grais RF. Prevalence of Bordetella infection in a hospital setting in Niamey, Niger. J Trop Pediatr. 2014;60(3):223–230. doi: 10.1093/tropej/fmu001. [DOI] [PubMed] [Google Scholar]
- 33.Kayina V, Kyobe S, Katabazi FA, Kigozi E, Okee M, Odongkara B, Babikako HM, Whalen CC, Joloba ML, Musoke PM, et al. Pertussis prevalence and its determinants among children with persistent cough in urban Uganda. PLoS One. 2015;10(4):e0123240. doi: 10.1371/journal.pone.0123240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gill CJ, Mwananyanda L, MacLeod W, Kwenda G, Mwale M, Williams AL, Siazeele K, Yang Z, Mwansa J, Thea DM. Incidence of severe and nonsevere pertussis among HIV-exposed and -unexposed Zambian infants through 14 weeks of age: results from the Southern Africa Mother Infant Pertussis Study (SAMIPS), a longitudinal birth cohort study. Clin Infect Dis. 2016;63(suppl 4):S154–s164. doi: 10.1093/cid/ciw526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hallbauer UM, Joubert G, Goosen Y. Pertussis in children in Bloemfontein, South Africa: a 7-year retrospective review. South Afr Med J. 2016;106(10):1042–1046. doi: 10.7196/SAMJ.2016.v106i10.10401. [DOI] [PubMed] [Google Scholar]
- 36.Muloiwa R, Dube FS, Nicol MP, Zar HJ, Hussey GD. Incidence and diagnosis of pertussis in South African children hospitalized with lower respiratory tract infection. Pediatr Infect Dis J. 2016;35(6):611–616. doi: 10.1097/INF.0000000000001132. [DOI] [PubMed] [Google Scholar]
- 37.Nunes MC, Downs S, Jones S, van Niekerk N, Cutland CL, Madhi SA. Bordetella pertussis infection in South African HIV-infected and HIV-uninfected mother-infant dyads: a longitudinal cohort study. Clin Infect Dis. 2016;63(suppl 4):S174–s180. doi: 10.1093/cid/ciw527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soofie N, Nunes MC, Kgagudi P, van Niekerk N, Makgobo T, Agosti Y, Hwinya C, Pathirana J, Madhi SA. The burden of pertussis hospitalization in HIV-exposed and HIV-unexposed South African infants. Clin Infect Dis. 2016;63(suppl 4):S165–s173. doi: 10.1093/cid/ciw545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zar HJ, Barnett W, Stadler A, Gardner-Lubbe S, Myer L, Nicol MP. Aetiology of childhood pneumonia in a well vaccinated South African birth cohort: a nested case-control study of the Drakenstein Child Health Study. Lancet Respir Med. 2016;4(6):463–472. doi: 10.1016/S2213-2600(16)00096-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.du Plessis NM, Ntshoe G, Reubenson G, Kularatne R, Blumberg L, Thomas J, Avenant T. Risk factors for pertussis among hospitalized children in a high HIV prevalence setting, South Africa. Int J Infect Dis. 2018;68:54–60. doi: 10.1016/j.ijid.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 41.Al-Bargish KA. Outbreak of pertussis in Basra, Iraq. East Mediterr Health J. 1999;5(3):540–548. [PubMed] [Google Scholar]
- 42.Kakar RM, Mojadidi MK, Mofleh J. Pertussis in Afghanistan, 2007-2008. Emerg Infect Dis. 2009;15(3):501. doi: 10.3201/eid1503.080982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ghanaie RM, Karimi A, Sadeghi H, Esteghamti A, Falah F, Armin S, Fahimzad A, Shamshiri A, Kahbazi M, Shiva F. Sensitivity and specificity of the World Health Organization pertussis clinical case definition. Int J Infect Dis. 2010;14(12):e1072–e1075. doi: 10.1016/j.ijid.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Bokhari H, Said F, Syed MA, Mughal A, Kazi YF, Heuvelman K, Mooi FR. Whooping cough in Pakistan: Bordetella pertussis vs Bordetella parapertussis in 2005-2009. Scand J Infect Dis. 2011;43(10):818–820. doi: 10.3109/00365548.2011.577804. [DOI] [PubMed] [Google Scholar]
- 45.Hajia M, Rahbar M, Fallah F, Safadel N. Detection of Bordetella pertussis in infants suspected to have whooping cough. Open Respir Med J. 2012;6:34–36. doi: 10.2174/1874306401206010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mughal A, Kazi YF, Bukhari HA, Ali M. Pertussis resurgence among vaccinated children in Khairpur, Sindh, Pakistan. Public Health. 2012;126(6):518–522. doi: 10.1016/j.puhe.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 47.Zouari A, Smaoui H, Brun D, Njamkepo E, Sghaier S, Zouari E, Fé, lix R, Menif K, Ben Jaballah N et al: Prevalence of Bordetella pertussis and Bordetella parapertussis infections in Tunisian hospitalized infants: results of a 4-year prospective study. Diagn Microbiol Infect Dis 2012, 72(4):303–317. [DOI] [PubMed]
- 48.Bahari M, Sadeghian I, Rezai M, Ghorbani G. Clinical manifestations of pertussis in pediatrics admitted to Sari Boalisina hospital, 2008-2012. J Mazandaran Univ Med Sci. 2013;23(101):2–9. [Google Scholar]
- 49.Nikbin VS, Shahcheraghi F, Lotfi MN, Zahraei SM, Parzadeh M. Comparison of culture and real-time PCR for detection of Bordetella pertussis isolated from patients in Iran. Iran J Microbiol. 2013;5(3):209–214. [PMC free article] [PubMed] [Google Scholar]
- 50.Saffar MJ, Ghorbani G, Hashemi A, Rezai MS. Pertussis resurgence in a highly vaccinated population, Mazandaran, North of Iran 2008-2011: an epidemiological analysis. Indian J Pediatr. 2014;81(12):1332–1336. doi: 10.1007/s12098-014-1445-0. [DOI] [PubMed] [Google Scholar]
- 51.Sedaghat M, Lotfi MN, Talebi M, Saifi M, Pourshafie MR. Status of pertussis in iran. Jundishapur J Microbiol. 2014;7(11):e12421. [DOI] [PMC free article] [PubMed]
- 52.Benamrouche N, Tali Maamar H, Lazri M, Hasnaoui S, Radoui A, Lafer O, Boukari R, Kaddache C, Arrada Z, Rahal K. Pertussis in north-central and northwestern regions of Algeria. J Infect Dev Ctries. 2016;10(11):1191–1199. doi: 10.3855/jidc.7262. [DOI] [PubMed] [Google Scholar]
- 53.Ghorbani GR, Zahraei SM, Moosazadeh M, Afshari M, Doosti F. Comparing seasonal pattern of laboratory confirmed cases of pertussis with clinically suspected cases. Osong Public Health Res Perspect. 2016;7(2):131–137. doi: 10.1016/j.phrp.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Omer SB, Kazi AM, Bednarczyk RA, Allen KE, Quinn CP, Aziz F, Sial K, Phadke VK, Tondella ML, Williams MM, et al. Epidemiology of pertussis among young Pakistani infants: a community-based prospective surveillance study. Clin Infect Dis. 2016;63(suppl 4):S148–s153. doi: 10.1093/cid/ciw561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katfy K, Guiso N, Diawara I, Zerouali K, Slaoui B, Jouhadi Z, Zineddine A, Belabbes H, Elmdaghri N. Epidemiology of pertussis in Casablanca (Morocco): contribution of conventional and molecular diagnosis tools. BMC Infect Dis. 2017;17(1):348. doi: 10.1186/s12879-017-2452-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ben Fraj I, Kechrid A, Guillot S, Bouchez V, Brisse S, Guiso N, Smaoui H. Pertussis epidemiology in Tunisian infants and children and characterization of Bordetella pertussis isolates: results of a 9-year surveillance study, 2007 to 2016. J Med Microbiol. 2019;68(2):241–247. doi: 10.1099/jmm.0.000892. [DOI] [PubMed] [Google Scholar]
- 57.Dumaidi K, Al-Jawabreh A. The prevalence of PCR-confirmed pertussis cases in Palestine from archived nasopharyngeal samples. Arch Iran Med. 2018;21(5):208–212. [PubMed] [Google Scholar]
- 58.Mohammadzadeh Asl Y, Akhi MT, Soroush MH, Sefidan FY, Mousapour J, Hejazi ME, Sabbaghi BG, Sharifi A, Jabari Y, Ghotaslou R. Clinical manifestations and seasonality of pertussis in Azerbaijan, Iran. Infect Dis Clin Pract. 2018;26(3):145–149. [Google Scholar]
- 59.Lukić-Grlić A, Baće A, Lokar-Kolbas R, Loffler-Badžek D, Draženović V, Božikov J, Mlinarić-Galinović G. Clinical and epidemiological aspects of respiratory syncytial virus lower respiratory tract infections. Eur J Epidemiol. 1999;15(4):361–365. doi: 10.1023/a:1007503302742. [DOI] [PubMed] [Google Scholar]
- 60.Daǧlar E, Nar S, Tanir G, Akbaş E, Zorlu P, Esen B. Approach to the diagnosis of pertussis infection: evaluation of cases suffering from prolonged cough symptoms. Mikrobiyoloji Bulteni. 2004;38(4):393–408. [PubMed] [Google Scholar]
- 61.Aksakal FN, Çöplü N, Ceyhan MN, Sönmez C, Özkan S, Esen B, Ilhan MN, Aygün R. High incidence of pertussis among schoolchildren with prolonged cough in Turkey. Tohoku J Exp Med. 2007;211(4):353–358. doi: 10.1620/tjem.211.353. [DOI] [PubMed] [Google Scholar]
- 62.Yıldırım I, Ceyhan M, Kalayci O, Cengiz AB, Secmeer G, Gur D, Pelton S. Frequency of pertussis in children with prolonged cough. Scand J Infect Dis. 2008;40(4):314–319. doi: 10.1080/00365540701689659. [DOI] [PubMed] [Google Scholar]
- 63.Medkova AY, Alyapkina YS, Sinyashina LN, Amelina IP, Alekseev YI, Bokovoi AG, Karataev GI. Detection of avirulent insertional Bordetella pertussis bvg(−) mutants in patients with pertussis and with upper respiratory tract infection and in seemingly healthy people. Mol Genet Microbiol Virol. 2010;25(4):167–171. [Google Scholar]
- 64.Gürsel D, Asian A, Sönmez C, Koturoǧlu G, Çöplü N, Kurugöl Z, Aydemlr S. Detection of Bordetella pertussis infection by culture, real-time polymerase chain reaction and serologic tests among children with prolonged cough. Mikrobiyoloji Bulteni. 2012;46(2):211–224. [PubMed] [Google Scholar]
- 65.Karlı A, Şensoy G, Belet N, Yener N, Akgün M, Paksu MŞ. Clinical features and prognosis of infants hospitalized with pertussis. Cocuk Enfeksiyon Dergisi. 2013;7(2):47–52. [Google Scholar]
- 66.Uslu ZDT, Ceyhan M, Dinleyici EC, Kurugol Z, Alpman BN, Oncel EK, Gurbuz V, Aycan E, Tezer H, Gulhan B. Detection of the presence of Bordetella pertussis by real-time polymerase chain reaction in children diagnosed with pertussis and among their household contacts. J Vaccines Vaccin. 2013;4:199. [Google Scholar]
- 67.Dinu S, Guillot S, Dragomirescu CC, Brun D, Lazar S, Vancea G, Ionescu BM, Gherman MF, Bjerkestrand AFD, Ungureanu V, et al. Whooping cough in South-East Romania: a 1-year study. Diagn Microbiol Infect Dis. 2014;78(3):302–306. doi: 10.1016/j.diagmicrobio.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 68.Karagul A, Ogunc D, Midilli K, Ongut G, Ozhak Baysan B, Donmez L, Daglar D, Kuskucu MA, Bingol A, Ozbudak O, et al. Epidemiology of pertussis in adolescents and adults in Turkey. Epidemiol Infect. 2015;143(12):2613–2618. [DOI] [PMC free article] [PubMed]
- 69.Öksüz L, Hançerli S, Somer A, Salman N, Gürler N. Pertussis in children in the İstanbul Faculty Of Medicine: results for four years. Turk J Pediatr. 2014;56(6):632–637. [PubMed] [Google Scholar]
- 70.Aslan A, Kurugol Z, Aydemir S, Gursel D, Koturoglu G. High frequency of pertussis in older children and adolescents with prolonged cough in Turkey. Turk J Pediatr. 2016;58(1):41–46. doi: 10.24953/turkjped.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 71.Goktas S, Sirin MC. Prevalence and seasonal distribution of respiratory viruses during the 2014–2015 season in Istanbul. Jundishapur J Microbiol. 2016;9(9):e39132. doi: 10.5812/jjm.39132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gökçe S, Kurugöl Z, Şöhret Aydemir S, Çiçek C, Aslan A, Koturoğlu G. Bordetella pertussis infection in hospitalized infants with acute bronchiolitis. Indian J Pediatr. 2018;85(3):189–193. doi: 10.1007/s12098-017-2480-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Singh MP, Srivastava VK, Agarwal SK. Pertussis in rural children. Indian Pediatr. 1987;24(7):553–556. [PubMed] [Google Scholar]
- 74.Dahiya S, Kapil A, Kabra SK, Mathur P, Sood S, Lodha R, Das BK. Pertussis in India. J Med Microbiol. 2009;58(Pt 5):688–689. doi: 10.1099/jmm.0.47847-0. [DOI] [PubMed] [Google Scholar]
- 75.Das A, Patgiri SJ, Saikia L, Dowerah P, Nath R. Bacterial pathogens associated with community-acquired pneumonia in children aged below five years. Indian Pediatr. 2016;53(3):225–227. doi: 10.1007/s13312-016-0825-0. [DOI] [PubMed] [Google Scholar]
- 76.Siriyakorn N, Leethong P, Tantawichien T, Sripakdee S, Kerdsin A, Dejsirilert S, Paitoonpong L. Adult pertussis is unrecognized public health problem in Thailand. BMC Infect Dis. 2016;16:25. doi: 10.1186/s12879-016-1357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hughes MM, Englund JA, Kuypers J, Tielsch JM, Khatry SK, Shrestha L, LeClerq SC, Steinhoff M, Katz J. Population-based pertussis incidence and risk factors in infants less than 6 months in Nepal. J Pediatr Infect Dis Soc. 2017;6(1):33–39. doi: 10.1093/jpids/piw079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chinthanate S, Wanlapakorn N, Puenpa J, Wongthong D, Poovorawan Y. Pertussis in Thai adult and pediatric patients presenting with prolonged acute cough. Southeast Asian J Trop Med Public Health. 2018;49(3):447–455. [Google Scholar]
- 79.Cooper E, Fitch L. Pertussis: herd immunity and vaccination coverage in St Lucia. Lancet. 1983;2(8359):1129–1132. doi: 10.1016/s0140-6736(83)90637-2. [DOI] [PubMed] [Google Scholar]
- 80.Baptista PN, Magalhães V, Rodrigues LC, Rocha MW, Pimentel AM. Pertussis vaccine effectiveness in reducing clinical disease, transmissibility and proportion of cases with a positive culture after household exposure in Brazil. Pediatr Infect Dis J. 2006;25(9):844–846. doi: 10.1097/01.inf.0000232642.25495.95. [DOI] [PubMed] [Google Scholar]
- 81.Sandoval PT, Arreola LDT, Quechol GR, Gallardo HG. Bordetella pertussis in adolescents students in Mexico City. Rev De Saude Publica. 2008;42(4):679–683. doi: 10.1590/s0034-89102008000400014. [DOI] [PubMed] [Google Scholar]
- 82.Nieto Guevara J, Luciani K, Montesdeoca Melián A, Mateos Durán M, Estripeaut D. Hospital admissions due to whooping cough: experience of the del niño Hospital in Panama. Period 2001–2008. An Pediatr. 2010;72(3):165–171. doi: 10.1016/j.anpedi.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 83.Astudillo M, Estrada VE, de Soto MF, Moreno LA. Bordetella pertussis infection in household contacts of cases of pertussis in the southeast zone of the city of Cali, Colombia, 2006–2007. Colomb Med. 2011;42(2):184–190. [Google Scholar]
- 84.Leite D, Cassiday PK, Tatti KM, Vaz TMI, Tondella ML. Serotypes and genetic profiles of Bordetella pertussis strains isolated in the city of São Paulo, 2006-2008. J Pediatr. 2012;88(4):357–360. doi: 10.2223/JPED.2186. [DOI] [PubMed] [Google Scholar]
- 85.Ferronato AE, Gilio AE, Vieira SE. Respiratory viral infections in infants with clinically suspected pertussis. J Pediatr. 2013;89(6):549–553. doi: 10.1016/j.jped.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 86.Ochoa-Perez UR, Hernández-Sierra JF, Escalante-Padrón FJ, Contreras-Vidales S, Berman-Puente AM, Hernandez-Maldonado F, Noyola DE. Epidemiology of Bordetella pertussis in San Luis Potosí, Mexico. Pediatr Infect Dis J. 2014;33(5):540–542. doi: 10.1097/INF.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 87.Vaz-de-Lima LRA, Martin MD, Pawloski LC, Leite D, Rocha KCP, De Brito CA, Vaz TMI, Martins LM, Alvarenga DP, Ribeiro AF, et al. Serodiagnosis as adjunct assay for pertussis infection in São Paulo, Brazil. Clin Vaccine Immunol. 2014;21(5):636–640. doi: 10.1128/CVI.00760-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Castillo ME, Bada C, Del Aguila O, Petrozzi-Helasvuo V, Casabona-Ore V, Reyes I, Del Valle-Mendoza J. Detection of Bordetella pertussis using a PCR test in infants younger than one year old hospitalized with whooping cough in five Peruvian hospitals. Int J Infect Dis. 2015;41:36–41. doi: 10.1016/j.ijid.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 89.Pavic-Espinoza I, Bendezú-Medina S, Herrera-Alzamora A, Weilg P, Pons MJ, Aguilar-Luis MA, Petrozzi-Helasvuo V, del Valle MJ. High prevalence of Bordetella pertussis in children under 5 years old hospitalized with acute respiratory infections in Lima, Peru. BMC Infect Dis. 2015;15:554. doi: 10.1186/s12879-015-1287-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pimentel AM, Baptista PN, Ximenes RA, Rodrigues LC, Magalhães V, Silva AR, Souza NF, Matos DG, Pessoa AK. Pertussis may be the cause of prolonged cough in adolescents and adults in the interepidemic period. Braz J Infect Dis. 2015;19(1):43–46. doi: 10.1016/j.bjid.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Del Valle-Mendoza J, Casabona-Oré V, Petrozzi-Helasvuo V, Cornejo-Tapia A, Weilg P, Pons MJ, Cieza-Mora E, Bazán-Mayra J, Cornejo-Pacherres H, Ruiz J. Bordetella pertussis diagnosis in children under five years of age in the Regional Hospital of Cajamarca, Northern Peru. J Infect Dev Ctries. 2015;9(11):1180–1185. doi: 10.3855/jidc.6803. [DOI] [PubMed] [Google Scholar]
- 92.Bailon H, León-Janampa N, Padilla C, Hozbor D. Increase in pertussis cases along with high prevalence of two emerging genotypes of Bordetella pertussis in Perú, 2012. BMC Infect Dis. 2016;16:422. doi: 10.1186/s12879-016-1700-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Aquino-Andrade A, Martínez-Leyva G, Mérida-Vieyra J, Saltigeral P, Lara A, Domínguez W, García de la Puente S, De Colsa A. Real-time polymerase chain reaction-based detection of Bordetella pertussis in Mexican infants and their contacts: a 3-year multicenter study. J Pediatr. 2017;188:217–223.e211. doi: 10.1016/j.jpeds.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 94.Phadke VK, McCracken JP, Kriss JL, Lopez MR, Lindblade KA, Bryan JP, Garcia ME, Funes CE, Omer SB. Clinical characteristics of hospitalized infants with laboratory-confirmed pertussis in Guatemala. J Pediatric Infect Dis Soc. 2018;7(4):310–316. doi: 10.1093/jpids/pix081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Del Valle-Mendoza J, Silva-Caso W, Aguilar-Luis MA, Del Valle-Vargas C, Cieza-Mora E, Martins-Luna J, Aquino-Ortega R, Silva-Vásquez A, Bazán-Mayra J, Weilg P. Bordetella pertussis in children hospitalized with a respiratory infection: Clinical characteristics and pathogen detection in household contacts. BMC Res Notes. 2018;11(1):318. doi: 10.1186/s13104-018-3405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ong SB, Thong ML, Tay LK. Viruses and bacteria associated with acute respiratory illnesses in young children in general practice. Southeast Asian J Trop Med Public Health. 1978;9(1):98–102. [PubMed] [Google Scholar]
- 97.Lin LPK, Lim TK. Multicenter clinical investigation of pertussis in children and adolescents with persistent cough. Zhonghua Er Ke Za Zhi. 2010;48(10):748–752. [PubMed] [Google Scholar]
- 98.Mi R, Fu J, Wang XY, Kang LM, Li L, Xu FS, Cui XD. Clinical research of Bordetella pertussis infection in infants with prolonged cough. Zhonghua Yi Xue Za Zhi. 2013;93(22):1721–1725. [PubMed] [Google Scholar]
- 99.Ting TX, Hashim R, Ahmad N, Abdullah KH. Detection of Bordetella pertussis from clinical samples by culture and end-point PCR in Malaysian patients. Int J Bacteriol. 2013;2013:324136. doi: 10.1155/2013/324136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Huang H, Liu Y, Gao Z, Liu P, Li Y, Zhang Y, Cao W. A sero-epidemiological study on pertussis among the community-based populations in Tianjin during 2010-2012. Zhonghua liu xing bing xue za zhi. 2014;35(12):1354–1357. [PubMed] [Google Scholar]
- 101.Liu Y, Huang H, Liu P, Su X, Gao Z, Guo L, Zhang Y. The status of pertussis infection and molecular epidemiological characteristics of pertussis in Tianjin, 2013. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35(12):1358–1361. [PubMed] [Google Scholar]
- 102.Wang Z, Cui Z, Li Y, Hou T, Liu X, Xi Y, Liu Y, Li H, He Q. High prevalence of erythromycin-resistant Bordetella pertussis in Xi’an, China. Clin Microbiol Infect. 2014;20(11):O825–O830. doi: 10.1111/1469-0691.12671. [DOI] [PubMed] [Google Scholar]
- 103.Hu Y, Liu Q. Clinical analysis of 247 children with whooping cough and the risk factors of severe cases. Zhonghua er ke za zhi. 2015;53(9):684–689. [PubMed] [Google Scholar]
- 104.Moriuchi T, Vichit O, Vutthikol Y, Hossain MS, Samnang C, Toda K, Grabovac V, Hiramatsu Y, Otsuka N, Shibayama K, et al. Molecular epidemiology of Bordetella pertussis in Cambodia determined by direct genotyping of clinical specimens. Int J Infect Dis. 2017;62:56–58. doi: 10.1016/j.ijid.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 105.Sadiasa A, Saito-Obata M, Dapat C, Saito M, Frederick Quicho R, Perez M, Joy Almonia D, De Leon-Asi L, Tamaki R, Sombrero L, et al. Bordetella pertussis infection in children with severe pneumonia, Philippines, 2012–2015. Vaccine. 2017;35(7):993–996. doi: 10.1016/j.vaccine.2016.11.087. [DOI] [PubMed] [Google Scholar]
- 106.Giayetto VO, Blanco S, Mangeaud A, Barbás MG, Cudolá A, Gallego SV. Features of Bordetella pertussis, Bordetella spp. infection and whopping cough in Córdoba province, Argentina. Rev Chil Infectol. 2017;34(2):108–115. doi: 10.4067/S0716-10182017000200002. [DOI] [PubMed] [Google Scholar]
- 107.Heininger U, Weibel D, Richard JL. Prospective nationwide surveillance of hospitalizations due to pertussis in children, 2006-2010. Pediatr Infect Dis J. 2014;33(2):147–151. doi: 10.1097/01.inf.0000435503.44620.74. [DOI] [PubMed] [Google Scholar]
- 108.Chow MY, Khandaker G, McIntyre P. Global childhood deaths from pertussis: a historical review. Clin Infect Dis. 2016;63(suppl 4):S134–S141. doi: 10.1093/cid/ciw529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Macdonald-Laurs E, Ganeshalingham A, Lillie J, McSharry B, Segedin ER, Best E, Pillai A, Harnden A, Gilchrist CA, Grant CC. Increasing incidence of life-threatening pertussis: a retrospective cohort study in New Zealand. Pediatr Infect Dis J. 2017;36(3):282–289. doi: 10.1097/INF.0000000000001441. [DOI] [PubMed] [Google Scholar]
- 110.Tan T, Dalby T, Forsyth K, Halperin SA, Heininger U, Hozbor D, Plotkin S, Ulloa-Gutierrez R, von Konig CH. Pertussis across the globe: recent epidemiologic trends from 2000–2013. Pediatr Infect Dis J. 2015;34(9):e222–232. doi: 10.1097/INF.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 111.Quinn HE, McIntyre PB. Pertussis epidemiology in Australia over the decade 1995-2005--trends by region and age group. Commun Dis Intell Q Rep. 2007;31(2):205–215. [PubMed] [Google Scholar]
- 112.Wylks CE, Ewald B, Guest C. The epidemiology of pertussis in the Australian Capital Territory, 1999 to 2005--epidemics of testing, disease or false positives? Commun Dis Intell Q Rep. 2007;31(4):383–391. [PubMed] [Google Scholar]
- 113.WHO Vaccine-Preventable Diseases Surveillance Standards. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/WHO_SurveillanceVaccinePreventable_16_Pertussis_R2.pdf?ua=1. Accessed 14 July 2020.
- 114.Mills KH. Immunity to Bordetella pertussis. Microbes and infection / Institut Pasteur. 2001;3(8):655–677. doi: 10.1016/s1286-4579(01)01421-6. [DOI] [PubMed] [Google Scholar]
- 115.Diphtheria tetanus toxoid and pertussis (DTP3) Immunization coverage estimates by World Bank Income Group. https://apps.who.int/gho/data/view.main.81200WB?lang=en. Accessed 3 July 2020.
- 116.Clark A, Sanderson C. Timing of children’s vaccinations in 45 low-income and middle-income countries: an analysis of survey data. Lancet. 2009;373(9674):1543–1549. doi: 10.1016/S0140-6736(09)60317-2. [DOI] [PubMed] [Google Scholar]
- 117.Odutola A, Afolabi MO, Ogundare EO, Lowe-Jallow YN, Worwui A, Okebe J, Ota MO. Risk factors for delay in age-appropriate vaccinations among Gambian children. BMC Health Serv Res. 2015;15:346. doi: 10.1186/s12913-015-1015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016;315(11):1149–1158. doi: 10.1001/jama.2016.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gkentzi D, Katsakiori P, Marangos M, Hsia Y, Amirthalingam G, Heath PT, Ladhani S. Maternal vaccination against pertussis: a systematic review of the recent literature. Arch Dis Child Fetal Neonatal Ed. 2017;102(5):F456–F463. doi: 10.1136/archdischild-2016-312341. [DOI] [PubMed] [Google Scholar]
- 120.Switzer C, D'Heilly C, Macina D. Immunological and clinical benefits of maternal immunization against pertussis: a systematic review. Infect Dis Ther. 2019;8(4):499–541. doi: 10.1007/s40121-019-00264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table: Strategy used to search for literature in MEDLINE (Via Pubmed).
Additional file 2. Country and year of included studies with confirmed pertussis shown by World Health Organisation region.
Additional file 3. Distribution of point prevalence of confirmed pertussis by World Health Organisation region and confirmation method [PCR = polymerase chain reaction].
Additional file 4 Prevalence of paired serology confirmed Bordetella pertussis. Dotted lines show subgroup and whole group average estimates.
Additional file 5 Prevalence of polymerase chain reaction and culture confirmed Bordetella parapertussis. Dotted line shows group average estimate [# Culture confirmed].
Additional file 6. Meta-analysis of relative detection rates of polymerase chain reaction (PCR) and culture in confirming Bordetella pertussis infection.
Data Availability Statement
All data generated or analysed during this study are included in this published article and in the reference list provided, all of which are in the public domain.