Abstract
Background
Cerebral ischemia-reperfusion injury is a form of serious nervous system injury. Activation of the PI3K/Akt pathway can effectively relieve cerebral ischemia-reperfusion injury. miR-214 can target and inhibit the expression of PTEN, thereby alleviating its inhibitory effect on the PI3K/Akt pathway. Moreover, lncRNA NEAT1 was reported to affect proliferation and metastasis of tumor cells by targeting and suppressing the expression of miR-214. However, whether lncRNA NEAT1 affects the cerebral ischemia-reperfusion-induced damage by regulating the miR-214/PTEN/PI3K/Akt pathway is unclear.
Material/Methods
The miR-214 agomir and miR-214 antagomir were designed and injected into the encephalocele of MCAO rats. Next, the production of oxidative stress kinase and apoptosis of brain cells were detected using commercial kits. The levels of PTEN, PI3K, Akt, p-Akt, and VEGF in brain tissues were determined. Next, the targeting effect of lncRNA NEAT1 and miR-214 was determined with luciferase reporter assay.
Results
Overexpression of miR-214 relieved the apoptosis and oxidative stress of brain tissues. Overexpression of miR-214 promoted the expression of PI3K, Akt, p-Akt, and VEGF by inhibiting the production of PTEN. However, overexpression of lncRNA NEAT1 repressed the remission effect of miR-214 on cerebral ischemia-reperfusion-induced damage and inhibited the production of PI3K, Akt, p-Akt, and VEGF by rescuing the levels of PTEN.
Conclusions
lncRNA NEAT1 aggravates cerebral ischemia-reperfusion injury by abolishing the activation effect of miR-214 on the PI3K/Akt pathway.
MeSH Keywords: Hypoxia-Ischemia, Brain; MicroRNAs; RNA, Long Noncoding
Background
Decreasing of blood supply in brain tissues can lead to lack of glucose and cause hypoxia of nerve cells. Moreover, the recovery of blood supply further aggravates the damage of brain tissues, which is called cerebral ischemia-reperfusion injury [1]. Cerebral ischemia-reperfusion injury causes serious nervous system damage, which can further induce the occurrence and development of ischemic stroke and other diseases [2,3]. It is well known that ischemic stroke is a common cerebrovascular disorder with high morbidity and it is recognized as one of the leading causes of severe disability and death worldwide. Additionally, cerebral ischemia-reperfusion can lead to oxidative stress, inflammatory responses, and dysfunction of the brain by promoting the production of reactive oxygen species (ROS) [4,5]. Although recent studies have revealed some molecular mechanisms of cerebral tissue injury induced by cerebral ischemia-reperfusion, current clinical therapies for cerebral ischemia-reperfusion injury have various limitations. Therefore, there is a need to find novel and effective therapeutic strategies for cerebral ischemia-reperfusion injury.
Previous research revealed that the PI3K/Akt pathway plays a critical role during the development of cerebral ischemia-reperfusion-induced damage, and activation of the PI3K/Akt pathway can relieve the symptoms of ischemia-reperfusion injury [6,7]. However, higher levels of PTEN are associated with the development of cerebral ischemia-reperfusion injury [8], and PTEN can also aggravate cerebral ischemia-reperfusion-induced damage by repressing the PI3K/Akt pathway [9]. There is also research showing that miR-214 can relieve the inhibitory effect of PTEN on the PI3K/Akt pathway by suppressing the production of PTEN [10]. However, whether miR-214 can affect cerebral ischemia-reperfusion injury by regulating the PTEN/PI3K/Akt pathway is unclear.
Long non-coding RNA (lncRNA) is a type of non-coding RNA more than 200 nucleotides in length. Some studies have revealed that such non-coding RNAs play an essential role during the processes of cell differentiation, transcription, and apoptosis [11,12]. Moreover, lncRNA is also expressed in the central nervous system and regulates dysfunction of the nervous system and brain function [13,14], and there is research suggesting that the lncRNA NEAT1 affects progression of thyroid carcinoma [15]. However, whether lncRNA NEAT1 impedes the regulating effect of miR-214 on cerebral ischemia-reperfusion injury is unclear.
We injected the miR-214 inhibitor into the encephalocele of middle cerebral artery occlusion (MCAO) model rats. Next, we assessed oxidative stress, inflammatory responses, and apoptosis of brain tissue, and measured the levels of lncRNA NEAT1, PI3K, PTEN, and Akt in brain tissue with Western blotting and RT-PCR. The results revealed the effect of lncRNA NEAT1/miR-214/PTEN/PI3K/Akt on cerebral ischemia-reperfusion injury.
Material and Methods
Animal experiments
We obtained 65 healthy male Sprague-Dawley (SD) rats from the Experimental Animal Center of the Chinese Academy of Sciences (Shanghai, China). All animal care and experimental procedures were conducted in accordance with the guidelines approved by the Animal Ethics Committee of the Third People’s Hospital of Nantong City (EK2019008). MCAO rat modeling was conducted as previously described [16,17]. In brief, rats were anesthetized with 4% isoflurane in medical oxygen, and then isoflurane was reduced to 2% for maintenance. The right common carotid artery, external carotid artery, and internal carotid artery were dissected from the surrounding tissues. After ligation of the common carotid artery and external carotid artery, a 4–0 nylon suture with silicon was gently introduced into the internal carotid artery for approximately 20 mm. After 2 h of ischemia, the line plug was withdrawn to allow for reperfusion. Sham group rats underwent the same procedure but without blocking the origin of the MCA. miR-214 agomir and miR-214 antagomir were designed by GeneChem (Shanghai, China) and injected into the encephalocele to change the expression of miR-214 in the brain. Fifteen rats were injected with miR-214 agomir, miR-214 antagomir, and the corresponding negative control to confirm the effect of overexpression and inhibition. Twenty-five SD rats were grouped into 5 groups (5 rats per group): a control group, an MCAO group, MCAO+PBS group (containing the negative control of miR-214 agomir and miR-214 antagomir), an MCAO+miR-214 agomir group, and an MCAO+miR-214 antagomir group. Twenty-five SD rats were divided into 4 groups: a control group, an MCAO group, an MACO+miR-214 agomir group, an MACO+miR-214 agomir+vector group, and an MACO+miR-214 agomir+lnc NEAT1 group. lncRNA NEAT1 (overexpression lentivirus) was obtained from GeneChem (Shanghai, China) and injected into the tail vein. All these rats were humanely euthanized according to ethics guidelines 48 h after the injection. After euthanasia, the brain tissues and blood of these rats were collected for the next assessment.
Staining of 2, 3, 5-triphenyltetrazolium chloride (TTC)
TTC staining was performed to distinguish between viable and infarcted brain tissue after stroke. The brain tissues were washed with PBS and then maintained at −20°C for 10 min. The brain tissues were cut along the coronal shape, and then were incubated with TTC solution for 30 min. These sections were fixed with 4% paraformaldehyde (Wako Pure Chemical Industries, Osaka, Japan) after staining. Next, the sections were photographed and analyzed with ImageJ software (NIH, USA). White areas were infarcted brain tissues and the other areas were the normal tissues. Cerebral infarction rate (%)=infarct area/total area×100%.
Detection of SOD, MDA, and CAT
MDA was measured with an MDA assay kit (Nanjing Jiancheng company, China; A003-1-2). Briefly, brain samples were incubated with RIPA buffer for 30 min on ice. After centrifugation at 13 000 rpm, 0.1 ml supernatant of each sample and 3 mL of mixed reagent were mixed and cultured for 40 min at 95°C, and then centrifuged at 3500 rpm for 10 min. Finally, the absorbance of each sample was determined at 532 nm wavelength by a microplate reader (Thermo Scientific, Boston, USA). SOD was quantified with a SOD assay kit (Nanjing Jiancheng company, China; A001-3-2). Briefly, 20 μl of sample and 0.22 mL of mixed reagent were added and mixed evenly. After culturing for 20 min at 37°C, the absorbance of each sample was determined at 450 nm wavelength by a microplate reader (Thermo Scientific, Boston, USA). CAT was determined with a CAT assay kit (Nanjing Jiancheng company, China; A007-2-1). Briefly, 0.05 ml of sample and 1 mL of mixed reagent were added and mixed evenly. After culturing for 1 min at 37°C, the absorbance of each sample was determined at 240 nm wavelength by a microplate reader (Thermo Scientific, Boston, USA).
TUNEL staining
Rat brain tissues were cut into sections and deparaffinized, then hydrolyzed with proteinase K working solution for 30 min. Then, the sections were washed with PBS 3 times. Next, terminal deoxynucleotide transferase (TdT) buffer was added and incubated with the sections for 10 min. After that, TUNEL reaction mixture (Roche, Switzerland) was added to the sections and maintained at room temperature for 1 h. Next, the sections were washed 3 times with cold PBS. Diaminobenzidine chromogen (DAB) was added and incubated with the sections for color development. All images were captured with a light microscope (OLYMPUS, Japan) at 400× magnification.
Luciferase reporter assays
PC12 cells were obtained from ATCC (Manassas, VA, USA) and used for the luciferase reporter assay. These cells were cultured with Dulbecco’s modified Eagle’s medium (DMEM, USA) with 10% fetal bovine serum (Gibco, USA). By searching on the LncBase v.2 database, we found that PTEN was the potential target gene of miR-214-3b and miR-214-3b was a target of lncRNA NEAT1. To confirm these results, luciferase reporter assay was carried out, and commercial kits (Promega, USA; E1910) were used for detection of fluorescence. The intensity of fluorescence was measured with a spectrophotometer (Thermo Fisher Scientific, USA). All procedures were performed according to the manufacturer’s instructions.
Western blotting
Total protein was collected with RIPA buffer (Beyotime, China). Next, the concentration of these protein samples was determined with BCA method (Beyotime, China). After that, proteins were separated with 10% SDS-PAGE gel (Beyotime, China) and transferred to PVDF membranes (Millipore, USA). Membranes were blocked with the 5% skim milk powder (Cell Signaling Technology, USA). Next, the membranes were incubated with the primary antibodies at 4°C overnight. The primary antibodies used in this research were Bax (Abcam, ab32503), Bcl-2 (Abcam, ab32124), Cleaved caspase3 (Abcam, ab2302), pro-caspase3 (Abcam, ab32150), PTEN (Abcam, ab32199), PI3K (Abcam, ab32089), p-PI3K (CST, 17366S), Akt (Abcam, ab8805), p-Akt (Abcam, ab38449), and VEGF (Abcam, ab32152). On the second day, membranes were incubated with secondary antibody. Bands were observed with enhanced chemiluminescence reagents (Pierce, Rockford, IL, USA). The relative intensity of target proteins was analyzed by Image J software and normalized to GAPDH expression level.
RT-PCR
Total RNA was extracted with the Trizol method (Thermo Fisher Scientific, USA). Next, the mRNA was reverse-transcribed into cDNA using a commercial kit (Roche, Switzerland; 11483188001). SYBR Green Realtime PCR Master Mix (TaKaRa, Japan) was used for the determination of fluorescence signals. The amplification of cDNA was performed with the ABI 7500 system (Thermo Fisher Scientific, USA), and the 2−ΔΔCt method was used for analysis of relative expression of target genes. The following primers were used in this study: miR-214 forward primer 5′-CACTCTATATAGTGTATCTTTC-3′, Reverse primer 5′-GGCTTTTAGTGTACGTCGTAATG-3′.
Statistical analysis
Data were analyzed with Graphpad Prism 7.0 (GraphPad Software Inc., USA). The t test was performed to compare differences between groups, with statistical significance set at P less than 0.05. Data are expressed as mean±SD. All experiments were repeated 3 times independently.
Results
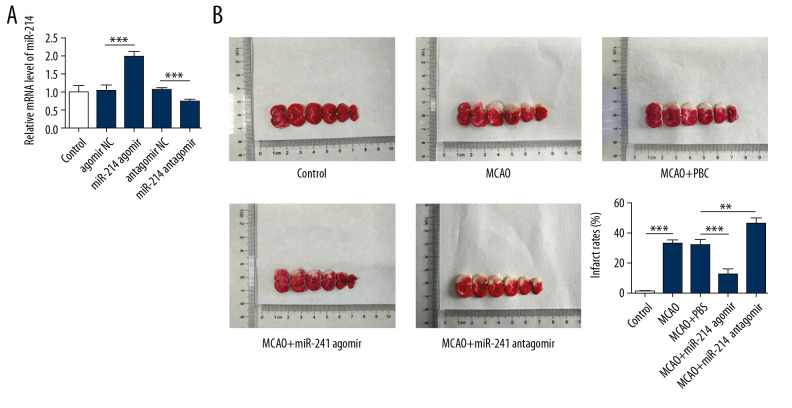
miR-214 relieved the cerebral infarction induced by cerebral ischemia-reperfusion
miR-214 agomir, miR-214 antagomir, and the corresponding negative control were designed and injected into the encephalocele of SD rats. Next, the levels of miR-214 in brain tissues of rats were determined with RT-PCR. The results (Figure 1A) showed that the levels of miR-214 were upregulated after the injection of miR-214 agomir, and the expression of miR-214 was decreased after the injection of miR-214 antagomir. After that, we established the MCAO rat model to further study the effect of miR-214 on cerebral ischemia-reperfusion injury. TTC staining assay results showed that the cerebral infarction rate decreased after injection of miR-214 agomir and was increased after injection of miR-214 antagomir (Figure 1B, 1C).
Figure 1.
miR-214 relieved the cerebral ischemia-reperfusion-induced cerebral infarction. (A) The efficacy of miR-214 agomir and miR-214 antagomir was detected with RT-PCR. (B) 2,3,5-triphenyltetrazolium chloride staining sections of brain tissues. (C) Proportions of cerebral infarction were determined with the formula: Cerebral infarction rate (%)=infarct area/total area×100%. ** p<0.01; ***p<0.001.
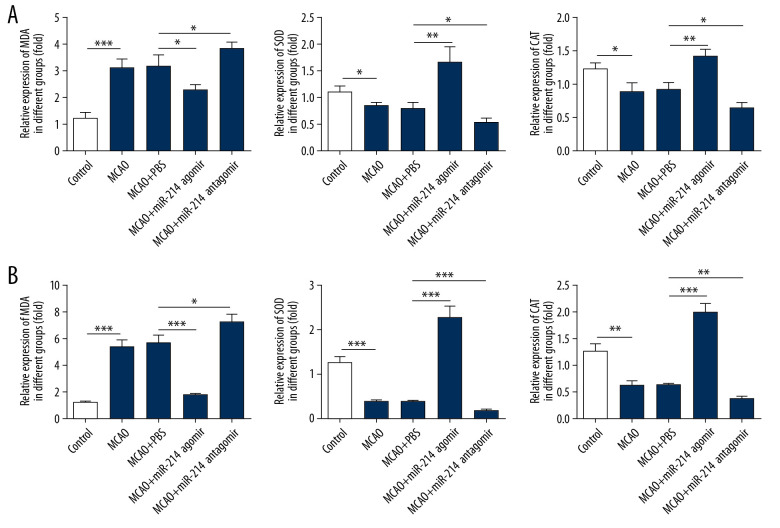
miR-214 alleviated the oxidative stress of brain tissues caused by cerebral ischemia-reperfusion
Brain tissues and peripheral blood were collected for the next experiment. The levels of oxidative stress-related enzymes in brain tissues and peripheral blood were detected with kits. SOD and CAT are antioxidant enzymes, while MDA is a product of peroxidation. As shown in Figure 2A, the expression of SOD and CAT was enhanced but the levels of MDA were decreased in brain tissues after injection of miR-214 agomir. Moreover, the levels of SPD and CAT declined while the expression of MDA was promoted after injection of miR-214 antagomir. Changes in levels of these factors reflected the same trend in peripheral blood (Figure 2B).
Figure 2.
miR-214 alleviated the oxidative stress of brain tissues. (A) The levels of MDA, SOD, and CAT in brain tissues were determined using commercial kits. (B) The levels of MDA, SOD, and CAT in peripheral blood were measured with commercial kits. * p<0.05; **p<0.01; ***p<0.001.
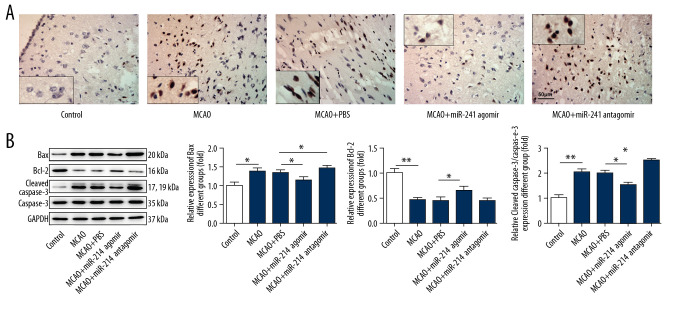
miR-214 relieved cerebral ischemia-reperfusion-induced brain cells apoptosis
TUNEL staining was performed to determine the apoptosis rate of brain cells, showing that apoptosis of brain cells was relieved after injection of miR-214 agomir (Figure 3A), and the injection of miR-214 antagomir aggravated the apoptosis of brain cells. The expression of apoptosis-related proteins (Bax, Bcl-2, and Cleaved caspase3) was detected with Western blotting, showing that the levels of Bax and Cleaved caspase3, and apoptotic proteins were reduced, while the level of Bcl-2, an anti-apoptotic protein, was increased in brain tissues of the miR-214 agomir group rats. After injection of miR-214 antagomir, the expression levels of Bax and Cleaved caspase3 were enhanced, while Bcl-2 expression was decreased in brain tissues (Figure 3B).
Figure 3.
miR-214 relieved the apoptosis of brain cells. (A) TUNEL staining of brain tissues (400×). (B) The expression of apoptosis-related proteins in brain tissues was detected with Western blotting. * p<0.05; ** p<0.01.
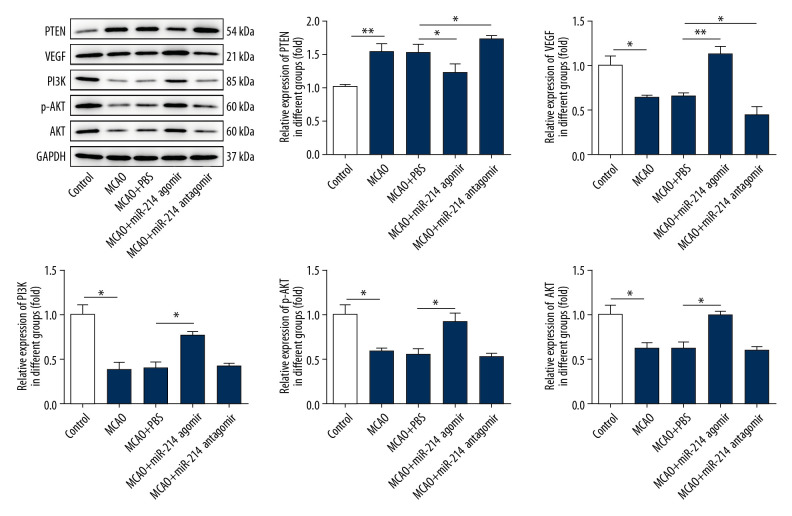
miR-214 alleviated cerebral ischemia-reperfusion injury by interfering in the PTEN/PI3K/Akt pathway
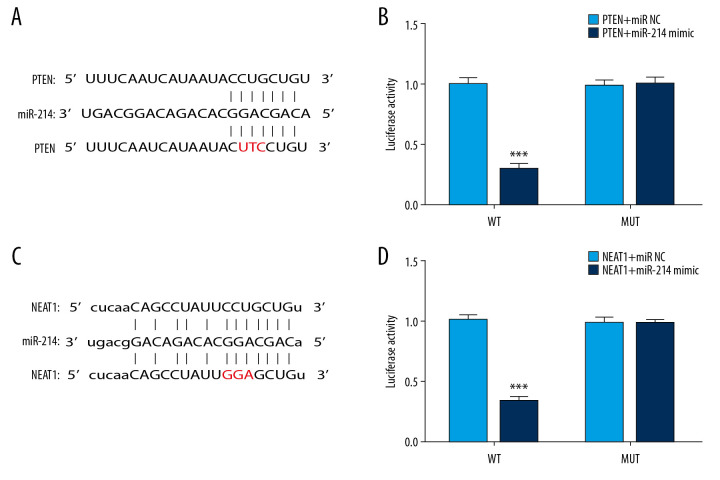
Some studies revealed that miR-214 overexpression relieved the suppressive influence of PTEN on the PI3K/Akt pathway and thus alleviated the apoptosis of multiple types of cells [10,18], and activation of the PI3K/Akt pathway was associated with the remission of cerebral ischemia-reperfusion injury [6,19]. Thus, we determined the expression of PTEN, PI3K, Akt, p-Akt, and VEGF in brain tissues after changing the expression of miR-214. We found that the expression of PI3K, Akt, p-Akt, and VEGF was enhanced and the expression of PTEN was inhibited after the injection of miR-214 agomir (Figure 4). After the injection of miR-214 antagomir, the expression of PI3K, Akt, p-Akt, and VEGF was suppressed, while the level of PTEN was upregulated in the brain tissues of rats. Next, the targeting effect of miR-214 on PTEN was verified with luciferase reporter assay in PC12 cells, showing that the fluorescence intensity was decreased in the wild-type PTEN and miR-214 mimic system (Figure 5A, 5B). There is also research showing that lncRNA NEAT1 can target and inhibit the expression of miR-214 in endometrial carcinoma cells [20]. Therefore, the targeting effect of lncRNA NEAT1 on miR-214 was also detected with the luciferase reporter assay in PC12 cells. As shown in Figure 5C and 5D, the fluorescence intensity was lower in the wild-type lncRNA NEAT1 and miR-214 mimic system. These results suggest that lncRNA NEAT1 targets and suppresses the expression of miR-214, and miR-214 also targets and inhibits the expression of PTEN.
Figure 4.
miR-214 alleviated cerebral ischemia-reperfusion injury by inhibiting the expression of PTEN and activating the PI3K/Akt pathway. The expression of PTEN, VEGF, PI3K, Akt, and p-Akt in brain tissues was determined by Western blotting. * p<0.05; ** p<0.01.
Figure 5.
lncRNA NEAT1 targeted and inhibited the expression of miR-214 while miR-214 targeted and suppressed the expression of PTEN. (A) The sequences of mature miR-214 and putative target sites of wild-type PTEN. (B) Luciferase activity was determined in the miR-214 mimic and negative control groups. (C) The sequences of mature miR-214 and putative target sites of wild-type lncRNA NEAT1. (D) Luciferase activity was assessed in the miR-214 mimic and negative control groups. *** p<0.001.
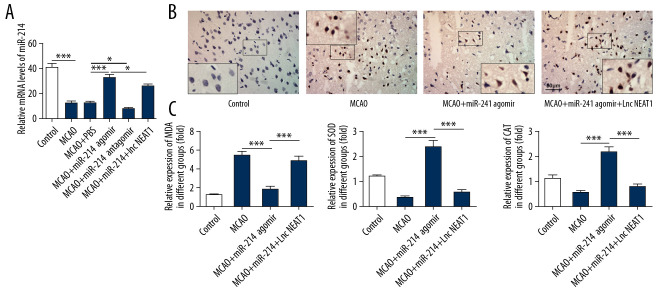
lncRNA NEAT1 attenuated the remission effect of miR-214 on cerebral ischemia-reperfusion injury by regulating the PTEN/PI3K/Akt pathway
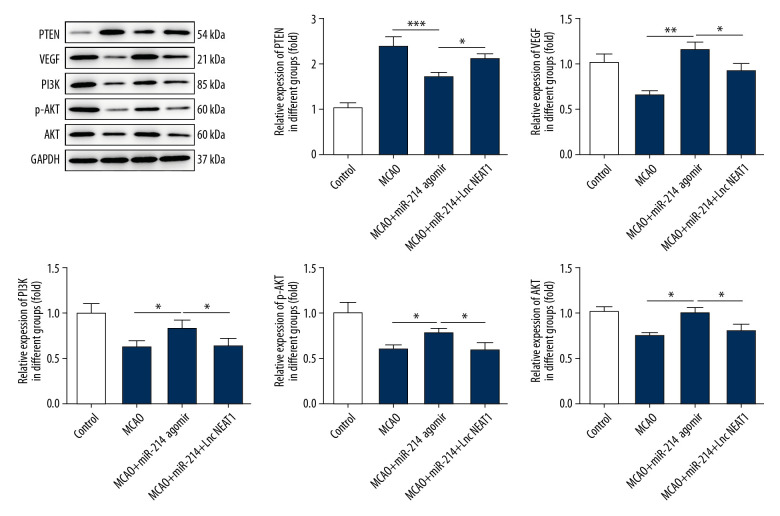
To further explore the role of lncRNA NEAT1 in cerebral ischemia-reperfusion-induced damage, the lncRNA NEAT1 (overexpression lentivirus) and the corresponding vector were administered to rats by tail vein injection. Then, the levels of miR-214 in the brain were determined with RT-PCR. We found that the expression of miR-214 was lower than in the vector group after the overexpression of lncRNA NEAT1 (Figure 6A). Next, the apoptosis of brain cells was determined with TUNEL staining. As shown in Figure 6B, the overexpression of lncRNA NEAT1 aggravated the apoptosis of brain cells. Then, the production of SOD, CAT, and MDA in brain tissues was detected with kits. The results (Figure 6C) showed that miR-214 overexpression inhibited the production of MDA and promoted the expressions of CAT and SOD in brain tissues of MCAO rats, and the overexpression of lncRNA NEAT1 rescued the expression of MDA and inhibited the production of CAT and SOD. Furthermore, we detected the expression of PTEN, PI3K, Akt, p-Akt, and VEGF in brain tissues after the overexpression of lncRNA NEAT1 (Figure 7). We found that overexpression of lncRNA NEAT1 suppressed the expression of PI3K, Akt, p-Akt, and VEGF, which was promoted with the higher levels of miR-214. However, the levels of PTEN were enhanced after the overexpression of lncRNA NEAT1.
Figure 6.
lncRNA NEAT1 attenuated the remission effect of miR-214 on cerebral ischemia-reperfusion injury. (A) The levels of miR-214 in brain tissues were determined by RT-PCR after overexpression of lncRNA NEAT1. (B) TUNEL staining was performed to detect apoptosis in brain tissues after the overexpression of lncRNA NEAT1. (C) The levels of MDA, SOD, and CAT in brain tissues were determined after the overexpression of lncRNA NEAT1. * p<0.05; *** p<0.001.
Figure 7.
Overexpression of lncRNA NEAT1 rescued the expression of PTEN and suppressed the expression of VEGF, PI3K, Akt, and p-Akt in brain tissues. The expression of PTEN, VEGF, PI3K, Akt, and p-Akt in brain tissues was determined with Western blotting after the overexpression of lncRNA NEAT1. * p<0.05; ** p<0.01; ***p<0.001.
Discussion
Cerebral ischemia-reperfusion injury is a serious nervous system injury. Without effective therapy, it can induce symptoms such as cerebral infarction and hemorrhagic stroke [2,3]. Some studies have revealed that cerebral ischemia-reperfusion-induced damage of cerebral cortex and inflammatory responses are crucial causes of severe neurological injury [21–23]. In addition, research suggests activation of the PI3K/Akt pathway relieves the symptoms of cerebral ischemia-reperfusion injury [24]. Another study suggested that urolithin A alleviates myocardial ischemia-reperfusion-induced damage by upregulating the expression of PI3K and Akt [25]. The neuroinflammation and oxidative stress caused by cerebral ischemia-reperfusion can also be alleviated after activation of the PI3K/Akt/Nrf2 pathway [19]. However, a study suggested that higher levels of PTEN can target and suppress activation of the PI3K/Akt pathway and thus aggravate hepatic ischemia/reperfusion injury [26]. Furthermore, the decreasing expression of PTEN was also reported to be associated with remission of ischemia/reperfusion injury of the myocardium [27].
It is well known that microRNA non-coding RNA molecules play critical roles in multiple physiological activities of cells, and miR-214 can relieve the symptoms of acute kidney injury and regulate the proliferation and metastasis of diverse malignant cells [28–30]. miR-214 was reported to target and repress PTEN expression and thus activate the PI3K/Akt pathway, and activation of the PI3K/Akt pathway alleviated the apoptosis of ovarian cancer cells [10]. In our research, the results showed that the injection of miR-214 agomir promoted the expression of SOD and relieved the apoptosis of brain cells. Furthermore, miR-214 agomir also promoted the expression of PI3K, Akt, and p-Akt, and the levels of PTEN declined after injection miR-214 agomir. However, the remission effect of miR-214 on cerebral ischemia-reperfusion injury was suppressed after the injection of miR-214 antagomir. The results of luciferase reporter gene assay also showed that miR-214 targets and inhibits the expression of PTEN. These results reveal that the miR-214 upregulation relieved the cerebral ischemia-reperfusion injury through suppressing PTEN expression and activating the PI3K/Akt pathway.
lncRNA NEAT1 can regulate the polarization of M2 macrophages by sponging miR-214 [31]. In addition, lncRNA NEAT1 can promote the proliferative ability and metastasis of endometrial carcinoma cells through restricting the biological effect of miR-214 [20]. The above studies indicate that lncRNA NEAT1 exerts its biological function through sponging miR-214, suggesting it may be an effective therapeutic strategy for cerebral ischemia-reperfusion injury treatment. However, whether lncRNA NEAT1 affects the cerebral ischemia-reperfusion-induced damage by regulating the miR-214/PTEN/PI3K/Akt pathway has been unclear. Results of the present study suggest that lncRNA NEAT1 targets and inhibits the expression of miR-214, which is consistent with previous studies. In addition, the overexpression of lncRNA NEAT1 abolished the remission effect of miR-214 on oxidative stress and apoptosis of brain cells of rats. Overexpression of lncRNA NEAT1 also led to upregulation of the levels of PTEN and inhibition of expression of PI3K, Akt, and p-Akt. These results indicate that lncRNA NEAT1 aggravates the cerebral ischemia-reperfusion-induced nervous system injury by abolishing the inhibitory effect of miR-214 on PTEN and inactivating the PI3K/Akt pathway. Taken together, the evidence presented above indicates that lncRNA NEAT1 blocking and miR-214 upregulation may be a novel and effective therapeutic strategy for cerebral ischemia-reperfusion injury treatment.
Conclusions
We demonstrated the effect of the lncRNA NEAT1/miR-214/PTEN/PI3K/Akt pathway on cerebral ischemia-reperfusion-induced damage. Our results revealed that lncRNA NEAT1 aggravated the cerebral ischemia-reperfusion-induced damage by repressing the inhibitory effect of miR-214 on PTEN and thus inactivating the PI3K/Akt pathway. Our study also provides new strategies and targets for clinical treatment of cerebral ischemia-reperfusion patients.
Footnotes
Conflict of interest
None.
Source of support: This study was supported by the Nantong Health Commission (MA2019009)
References
- 1.Xie G, Yang S, Chen A, et al. Electroacupuncture at Quchi and Zusanli treats cerebral ischemia-reperfusion injury through activation of ERK signaling. Exp Ther Med. 2013;5:1593–97. doi: 10.3892/etm.2013.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics – 2016 update: A report from the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 3.Xu Q, Deng F, Xing Z, et al. Long non-coding RNA C2dat1 regulates CaMKIIδ expression to promote neuronal survival through the NF-κB signaling pathway following cerebral ischemia. Cell Death Dis. 2016;7:e2173. doi: 10.1038/cddis.2016.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lei C, Denh J, Wang B, et al. Reactive oxygen species scavenger inhibits STAT3 activation after transient focal cerebral ischemia-reperfusion injury in rats. Anesth Analg. 2011;113:153–59. doi: 10.1213/ANE.0b013e31821a9fbe. [DOI] [PubMed] [Google Scholar]
- 5.Zhang B, Gao M, Shen J, He D. Inhaled methane protects rats against neurological dysfunction induced by cerebral ischemia and reperfusion injury: PI3K/Akt/HO-1 pathway involved. Arch Med Res. 2017;48:520–25. doi: 10.1016/j.arcmed.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Yan H, Li S, Zhang M. Berberine ameliorates MCAO induced cerebral ischemia/reperfusion injury via activation of the BDNF-TrkB-PI3K/Akt signaling pathway. Neurochem Res. 2018;43:702–10. doi: 10.1007/s11064-018-2472-4. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J, Du T, Li B, et al. Crosstalk between MAPK/ERK and PI3K/AKT signal pathways during brain ischemia/reperfusion. ASN Neuro. 2015;7 doi: 10.1177/1759091415602463. 1759091415602463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo XL, Liang H, Sun Y, Wang C-B, et al. MicroRNA-26a regulates cerebral ischemia injury through targeting PTEN. Eur Rev Med Pharmacol Sci. 2019;23:7033–41. doi: 10.26355/eurrev_201908_18745. [DOI] [PubMed] [Google Scholar]
- 9.Xue X, Wang H, Su J, et al. Inhibition of MiR-122 decreases cerebral ischemia-reperfusion injury by upregulating DJ-1-phosphatase and tensin homologue deleted on chromosome 10 (PTEN)/phosphonosinol-3 kinase (PI3K)/AKT. Med Sci Monit. 2020;26:e915825. doi: 10.12659/MSM.915825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu J, Chen W, Zhang H, et al. miR-214 targets the PTEN-mediated PI3K/Akt signaling pathway and regulates cell proliferation and apoptosis in ovarian cancer. Oncol Lett. 2017;14:5711–18. doi: 10.3892/ol.2017.6953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fatica A, Bozzoni I. Long non-coding RNAs: New players in cell differentiation and development. Nat Rev Genet. 2014;15:7–21. doi: 10.1038/nrg3606. [DOI] [PubMed] [Google Scholar]
- 12.Guttman M, Rinn JL. Modular regulatory principles of large non-coding RNAs. Nature. 2012;482:339–46. doi: 10.1038/nature10887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen R, Liu L, Xiao M, Lin X. Microarray expression profile analysis of long noncoding RNAs in premature brain injury: A novel point of view. Neuroscience. 2016;319:123–33. doi: 10.1016/j.neuroscience.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 14.Knauss JL, Sun T. Regulatory mechanisms of long noncoding RNAs in vertebrate central nervous system development and function. Neuroscience. 2013;235:200–14. doi: 10.1016/j.neuroscience.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li JH, Zhang SQ, Qiu XG, et al. Long non-coding RNA NEAT1 promotes malignant progression of thyroid carcinoma by regulating miRNA-214. Int J Oncol. 2017;50:708–16. doi: 10.3892/ijo.2016.3803. [DOI] [PubMed] [Google Scholar]
- 16.You D, You H. Repression of long non-coding RNA MEG3 restores nerve growth and alleviates neurological impairment after cerebral ischemia-reperfusion injury in a rat model. Biomed Pharmacother. 2019;111:1447–57. doi: 10.1016/j.biopha.2018.12.067. [DOI] [PubMed] [Google Scholar]
- 17.Popp A, Jaenisch N, Witte OW, Frahm C, et al. Identification of ischemic regions in a rat model of stroke. PLoS One. 2009;4:e4764. doi: 10.1371/journal.pone.0004764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao C, Sun W, Zhang P, et al. miR-214 promotes osteoclastogenesis by targeting Pten/PI3k/Akt pathway. RNA Biol. 2015;12:343–53. doi: 10.1080/15476286.2015.1017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wen Z, Hou W, Wu W, et al. 6′-O-galloylpaeoniflorin attenuates cerebral ischemia reperfusion-induced neuroinflammation and oxidative stress via PI3K/Akt/Nrf2 activation. Oxid Med Cell Longev. 2018;2018 doi: 10.1155/2018/8678267. 8678267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang J, Zhao X, Guo Z, et al. Regulation of NEAT1/miR-214-3p on the growth, migration and invasion of endometrial carcinoma cells. Arch Gynecol Obstet. 2017;295:1469–75. doi: 10.1007/s00404-017-4365-1. [DOI] [PubMed] [Google Scholar]
- 21.del Zoppo GJ, Hallenbeck JM. Advances in the vascular pathophysiology of ischemic stroke. Thromb Res. 2000;98:73–81. doi: 10.1016/s0049-3848(00)00218-8. [DOI] [PubMed] [Google Scholar]
- 22.Ishikawa M, Zhang JH, Nanad A, Granger DN. Inflammatory responses to ischemia and reperfusion in the cerebral microcirculation. Front Biosci. 2004;9:1339–47. doi: 10.2741/1330. [DOI] [PubMed] [Google Scholar]
- 23.Mehta SL, Manhas N, Raghubir R. Molecular targets in cerebral ischemia for developing novel therapeutics. Brain Res Rev. 2007;54:34–66. doi: 10.1016/j.brainresrev.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Li Z, Zhao F, Cao Y, et al. DHA attenuates hepatic ischemia reperfusion injury by inhibiting pyroptosis and activating PI3K/Akt pathway. Eur J Pharmacol. 2018;835:1–10. doi: 10.1016/j.ejphar.2018.07.054. [DOI] [PubMed] [Google Scholar]
- 25.Tang L, Mo Y, Li Y, et al. Urolithin A alleviates myocardial ischemia/reperfusion injury via PI3K/Akt pathway. Biochem Biophys Res Commun. 2017;486:774–80. doi: 10.1016/j.bbrc.2017.03.119. [DOI] [PubMed] [Google Scholar]
- 26.Su S, Luo D, Liu X, et al. miR-494 up-regulates the PI3K/Akt pathway via targetting PTEN and attenuates hepatic ischemia/reperfusion injury in a rat model. Biosci Rep. 2017;37:BSR20170798. doi: 10.1042/BSR20170798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheng Y, Sun T, Yin C, et al. Downregulation of PTEN by sodium orthovanadate protects the myocardium against ischemia/reperfusion injury after chronic atorvastatin treatment. J Cell Biochem. 2019;120:3709–15. doi: 10.1002/jcb.27651. [DOI] [PubMed] [Google Scholar]
- 28.Cao TH, Ling X, Chen C, et al. Role of miR-214-5p in the migration and invasion of pancreatic cancer cells. Eur Rev Med Pharmacol Sci. 2018;22:7214–21. doi: 10.26355/eurrev_201811_16255. [DOI] [PubMed] [Google Scholar]
- 29.Zhu X, Li W, Li H, et al. miR-214 ameliorates acute kidney injury via targeting DKK3 and activating of Wnt/β-catenin signaling pathway. Biol Res. 2018;51:31. doi: 10.1186/s40659-018-0179-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cai H, Miao M, Wang Z, et al. miR-214-3p promotes the proliferation, migration and invasion of osteosarcoma cells by targeting CADM1. Oncol Lett. 2018;16:2620–28. doi: 10.3892/ol.2018.8927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao Y, Feng P, Li WJ, et al. LncRNA NEAT1 sponges miR-214 to regulate M2 macrophage polarization by regulation of B7-H3 in multiple myeloma. Mol Immunol. 2020;117:20–28. doi: 10.1016/j.molimm.2019.10.026. [DOI] [PubMed] [Google Scholar]