Abstract
Introduction
Patients with stroke-like symptoms may be underutilising emergency medical services and avoiding hospitalisation during the COVID-19 pandemic. We investigated a decline in admissions for stroke and transient ischaemic attack (TIA) and emergency department (ED) stroke alert activations.
Methods
We retrospectively compiled total weekly hospital admissions for stroke and TIA between 31 December 2018 and 21 April 2019 versus 30 December 2019 and 19 April 2020 at five US tertiary academic comprehensive stroke centres in cities with early COVID-19 outbreaks in Boston, New York City, Providence and Seattle. We collected available data on ED stroke alerts, stroke severity using the National Institutes of Health Stroke Scale (NIHSS) and time from symptom onset to hospital arrival.
Results
Compared with 31 December 2018 to 21 April 2019, a decline in stroke/TIA admissions and ED stroke alerts occurred during 30 December 2019 to 19 April 2020 (p trend <0.001 for each). The declines coincided with state stay-at-home recommendations in late March. The greatest decline in hospital admissions was observed between 23 March and 19 April 2020, with a 31% decline compared with the corresponding weeks in 2019. Three of the five centres with 2019 and 2020 stroke alert data had a 46% decline in ED stroke alerts in late March and April 2020, compared with 2019. Median baseline NIHSS during these 4 weeks was 10 in 2020 and 7 in 2019. There was no difference in time from symptom onset to hospital arrival.
Conclusion
At these five large academic US hospitals, admissions for stroke and TIA declined during the COVID-19 pandemic. There was a trend for fewer ED stroke alerts at three of the five centres with available 2019 and 2020 data. Acute stroke therapies are time-sensitive, so decreased healthcare access or utilisation may lead to more disabling or fatal strokes, or more severe non-neurological complications related to stroke. Our findings underscore the indirect effects of this pandemic. Public health officials, hospital systems and healthcare providers must continue to encourage patients with stroke to seek acute care during this crisis.
Keywords: stroke, infection
Introduction
The WHO declared COVID-19 a pandemic on 11 March 2020 and the USA declared a national emergency over COVID-19 on 13 March. Reports examining the effect of the pandemic on healthcare delivery for non-COVID conditions are emerging,1–5 including observations of fewer mechanical thrombectomy procedures being performed for acute ischaemic stroke and on delays in stroke care. We hypothesised a decline in admissions for stroke and transient ischaemic attack (TIA) and emergency department (ED) stroke alert activations.
Methods
We retrospectively compiled total weekly hospital admissions for stroke and TIA and ED stroke alert activations between 31 December 2018 and 21 April 2019 versus 30 December 2019 and 19 April 2020. Hospital admission data were collected at five US tertiary academic comprehensive stroke centres in cities with early COVID-19 outbreaks in Boston, New York City, Providence and Seattle. Hospital capacities ranged from 413 to 719 beds with a combined catchment population of 3–4 million. Data for ED stroke alerts were available from three of the stroke centres in New York City, Providence and Seattle.
Hospital admissions included ischaemic stroke, intracerebral haemorrhage, subarachnoid haemorrhage or TIA, including transfers. Stroke alert was defined as stroke team notification of an ED patient with stroke-like symptoms within 24 hours of presentation. We collected data on baseline stroke severity using the National Institutes of Health Stroke Scale (NIHSS) and data on time from symptom onset to hospital arrival for patients with ischaemic and haemorrhagic stroke, excluding patients with TIA and those presenting over 24 hours after symptom onset.
Hospital admissions for stroke and TIA, ED stroke alerts, baseline NIHSS and time from symptom onset to hospital arrival were compared using t-test, Fisher’s exact test or Wilcoxon rank-sum test, where appropriate. Univariate analyses were restricted to the weeks after a national emergency was declared (after 13 March). In our primary analysis, over the total 16-week period, time series regression models (autoregressive integrated moving average) and time series forecasting systems were used to assess the inter-relationship of weekly stroke/TIA admissions and ED stroke alerts, separately. The standard variation of weekly stroke alerts and admissions were compared with the same measures in 2019.
Results
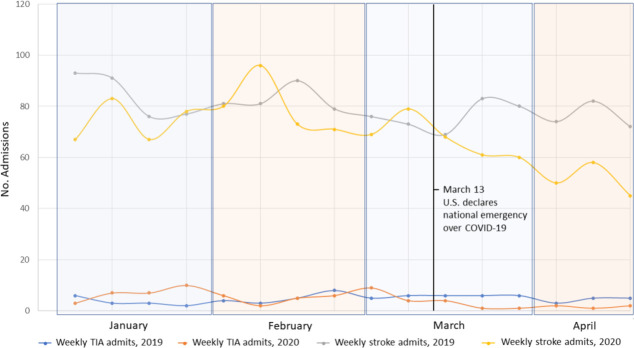
Trends in weekly stroke and TIA admissions are displayed in figure 1. Compared with the 31 December 2018 to 21 April 2019 time period, there was a decline in admissions observed between 30 December 2019 and 19 April 2020 (p trend <0.001). The decline coincided with the declaration of a US national emergency over the COVID-19 pandemic on 13 March, and with state stay-at-home recommendations in New York, Washington, Massachusetts and Rhode Islands (22, 23, 24 and 28 March, respectively). The greatest decline in stroke and TIA admissions was seen between 23 March and 19 April 2020, with a total of 281 admissions, compared with 410 in the corresponding time period in 2019, representing 31% fewer admissions (table 1).
Figure 1.
Weekly admissions for stroke and transient ischaemic attack (TIA) in the first 16 weeks of 2019 and 2020. Data from five medical centres in Boston, New York City, Providence and Seattle.
Table 1.
Stroke and TIA admissions, emergency department stroke alerts, stroke severity and delay to hospital presentation during the COVID-19 pandemic at US medical centres
| 2019 25 March to 21 April |
2020 23 March to 19 April* |
|
| Stroke/TIA admissions, n | 410 | 281 |
| Stroke only† | 391 | 274 |
| TIA only | 19 | 7 |
| ED stroke alerts, n‡ | 561 | 301 |
| Baseline NIHSS, median score (range) | 7 (7–10) | 10 (8–11) |
| Stroke symptom onset to hospital arrival, median hours (range) | 6.9 (5.4–8.0) | 7.6 (4.9–12.5) |
*Univariate analyses comparing 2020 with 2019 measures were statistically significant (p<0.01), except for median time from stroke symptom onset to hospital arrival (p=0.14).
†Includes admissions for ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage.
‡Including three medical centres in New York City, Providence and Seattle with available data.
ED, emergency department; NIHSS, National Institutes of Health Stroke Scale; TIA, transient ischaemic attack.
At three of the five centres with data on ED stroke alert activations from both 2019 and 2020 (figure 2), we observed a decline in the first 16 weeks of 2020, compared with 2019 (p trend <0.001). There was a 46% decline in stroke alerts in late March and April, compared with 2019 (table 1).
Figure 2.
Weekly emergency department (ED) stroke alert activations in the first 16 weeks of 2019 and 2020. Data from three medical centres in New York City, Providence and Seattle.
The median NIHSS for all centres between 23 March and 19 April 2020 was 10, compared with a median score of 7 for the corresponding weeks in 2019. The median time from symptom onset to hospital arrival did not appear to differ between 23 March and 19 April 2020 and 25 March and 21 April 2019 (6.9 and 7.6 hours, respectively).
Discussion
In this multicentre study, admissions for stroke and TIA and ED stroke alerts declined during the COVID-19 pandemic. Patients with stroke may be reluctant to activate emergency services or present to hospitals for fear of exposure to COVID-19. They may be underestimating their risk of death or disability due to stroke and avoiding hospital and emergency systems which they assume are under stress. Citing fear of in-hospital infection and disrupted functioning at stroke centres in China and France, separate groups have described a decline, between 21% and 50%, in the number of mechanical thrombectomy cases performed during the first weeks of the outbreak.3 6 In a recent report, individuals undergoing acute stroke imaging, as a surrogate for stroke evaluation, declined by 39% in late March.2 This was observed across all age and sex subgroups.
Additional factors may be contributing. Patients with milder stroke symptoms may be avoiding medical care.7 We noted an increase in median NIHSS scores, from 7 to 10, in late March of 2019 and 2020, suggesting an increase in the severity of stroke cases. Another contributing factor may be that because family members or bystanders usually activate emergency services,8 stay-at-home and social distancing practices may lead to a lack of contact with others and under-reporting of symptoms. However, we did not find a noticeable delay in stroke symptom onset to hospital presentation among patients presenting within 24 hours of symptoms. Additionally, outpatient clinics have also cancelled in-person visits, which could result in suboptimal recognition of stroke in the community. Finally, urban flight in the hardest hit cities may have resulted in fewer strokes in metropolitan areas. A limitation is that our findings may not be representative of smaller community or rural hospitals.
Conclusions
Acute stroke therapies are time-sensitive,9 so decreased healthcare access or utilisation may lead to more disabling or fatal strokes, or more severe non-neurological complications related to stroke. Our findings underscore the indirect effects of this pandemic. Public health officials, hospital systems and healthcare providers must continue to encourage patients with stroke to seek acute care during this crisis. Future investigations using stroke registries, national admissions data and stroke mortality estimates will help elucidate where all the missing strokes have gone.
Footnotes
Contributors: Study conception and design of work: Malveeka Sharma, MD, MPH; Vasileios Lioutas, MD; Tracy Madsen, MD, ScM; Tina M. Burton, MD; Amelia Boehme, PhD; Hugo J. Aparicio, MD, MPH. Data acquisition: Malveeka Sharma, MD, MPH; Vasileios Lioutas, MD; Tracy Madsen, MD, ScM; Judith Clark, Jillian O’Sullivan, Mitchell S. V. Elkind, MD, MS; Joshua Z. Willey, MD; Randolph S. Marshall, MD, Magdy H. Selim, MD, PhD; David Greer, MD, MA; David L. Tirschwell, MD, MSc; Tina M. Burton, MD; Amelia Boehme, PhD; Hugo J. Aparicio, MD, MPH. Data analysis and interpretation: Malveeka Sharma, MD, MPH; Vasileios Lioutas, MD; Tracy Madsen, MD, ScM; Tina M. Burton, MD; Amelia Boehme, PhD; Hugo J. Aparicio, MD, MPH. Statistical analysis: Amelia Boehme, PhD. Manuscript preparation: Malveeka Sharma, MD, MPH; Vasileios Lioutas, MD; Tracy Madsen, MD, ScM; Judith Clark, Jillian O’Sullivan, Tina M. Burton, MD; Amelia Boehme, PhD; Hugo J. Aparicio, MD, MPH. Manuscript editing: Malveeka Sharma, MD, MPH; Vasileios Lioutas, MD; Tracy Madsen, MD, ScM; Judith Clark, Jillian O’Sullivan, Mitchell S. V. Elkind, MD, MS; Joshua Z. Willey, MD; Randolph S. Marshall, MD; Magdy H. Selim, MD, PhD; David Greer, MD, MA; David L. Tirschwell, MD, MSc; Tina M. Burton, MD; Amelia Boehme, PhD; Hugo J. Aparicio, MD, MPH.
Funding: This research is supported by the National Institutes of Health (NIH 1UL1TR001430). Dr. Aparicio is supported by the Boston University Aram V. Chobanian Assistant Professorship.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The institutional review boards at each centre approved the study and received approval from the ethical standards committee to conduct this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Garcia S, Albaghdadi MS, Meraj PM, et al. . Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:S0735109720349135. 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kansagra AP, Goyal MS, Hamilton S, et al. . Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med 2020;383:400–1. 10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kerleroux B, Fabacher T, Bricout N, et al. . Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke 2020;51:1–3. 10.1161/STROKEAHA.120.030373 [DOI] [PubMed] [Google Scholar]
- 4. Teo K-C, Leung WCY, Wong Y-K, et al. . Delays in stroke onset to hospital arrival time during COVID-19. Stroke 2020;51:2228–31. 10.1161/STROKEAHA.120.030105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uchino K, Kolikonda MK, Brown D, et al. . Decline in stroke presentations during COVID-19 surge. Stroke 2020;51:2544–7. 10.1161/STROKEAHA.120.030331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhao J, Rudd A, Liu R. Challenges and potential solutions of stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke 2020;51:1356–7. 10.1161/STROKEAHA.120.029701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diegoli H, Magalhães PSC, Martins SCO, et al. . Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 2020;51:2315–21. 10.1161/STROKEAHA.120.030481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehosp Emerg Care 1999;3:211–6. 10.1080/10903129908958939 [DOI] [PubMed] [Google Scholar]
- 9. Saver JL, Fonarow GC, Smith EE, et al. . Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013;309:2480–8. 10.1001/jama.2013.6959 [DOI] [PubMed] [Google Scholar]