Abstract
Background
In response to the COVID-19 pandemic, many centers altered stroke triage protocols for the protection of their providers. However, the effect of workflow changes on stroke patients receiving mechanical thrombectomy (MT) has not been systematically studied.
Methods
A prospective international study was launched at the initiation of the COVID-19 pandemic. All included centers participated in the Stroke Thrombectomy and Aneurysm Registry (STAR) and Endovascular Neurosurgery Research Group (ENRG). Data was collected during the peak months of the COVID-19 surge at each site. Collected data included patient and disease characteristics. A generalized linear model with logit link function was used to estimate the effect of general anesthesia (GA) on in-hospital mortality and discharge outcome controlling for confounders.
Results
458 patients and 28 centers were included from North America, South America, and Europe. Five centers were in high-COVID burden counties (HCC) in which 9/104 (8.7%) of patients were positive for COVID-19 compared with 4/354 (1.1%) in low-COVID burden counties (LCC) (P<0.001). 241 patients underwent pre-procedure GA. Compared with patients treated awake, GA patients had longer door to reperfusion time (138 vs 100 min, P=<0.001). On multivariate analysis, GA was associated with higher probability of in-hospital mortality (RR 1.871, P=0.029) and lower probability of functional independence at discharge (RR 0.53, P=0.015).
Conclusion
We observed a low rate of COVID-19 infection among stroke patients undergoing MT in LCC. Overall, more than half of the patients underwent intubation prior to MT, leading to prolonged door to reperfusion time, higher in-hospital mortality, and lower likelihood of functional independence at discharge.
Keywords: stroke, thrombectomy, complication
Introduction
The coronavirus disease 2019 (COVID-19) outbreak, which originated in Wuhan, China, has now spread to more than 200 countries worldwide and led to more than 300 000 deaths.1 The hallmark of infection with COVID-19 is a severe respiratory syndrome with symptoms ranging from mild infection with fever, cough, shortness of breath, and fatigue to severe pneumonia requiring hospitalization and assisted ventilation.2–4 Recent studies have reported neurologic manifestations in approximately 37% of patients with confirmed COVID-19 infection.5 6 A study from China reported ischemic stroke in about 5% of patients with COVID-19 infection, and most recently, a case series from New York reported five cases of large-vessel occlusion (LVO) in young patients, raising the concern for a possible association between COVID-19 infection and LVO in young patients.7 8 Additional studies have linked COVID-19 with a hypercoagulable state, including systemic venous and arterial thromboses.9–11 However, it is unclear whether there is a causal relationship between COVID-19 and LVO in younger patients.
Given the high contagiousness and rapid spread of COVID-19, along with reports of high rates of infection among healthcare workers, multiple national and international societies set forth guidelines based on expert recommendations to help guide stroke providers during the COVID-19 pandemic, in order to mitigate provider illness. Some of the recommendations included modifying the triage workflow and lowering intubation thresholds.12–17 As such, healthcare systems worldwide, in areas with high as well as low burden of COVID-19, adjusted protocols related to mechanical thrombectomy (MT), not necessarily adjusted to the actual local burden of COVID-19. The impact of such changes on MT time metrics and outcomes is unknown, and whether such changes should be implemented in all centers regardless of the COVID-19 burden is also unclear. It is possible that new protocol implementations,5 while aimed at protecting healthcare providers and patients, might not achieve this goal and possibly result in harmful delays and unnecessary use of resources. Furthermore, the prevalence of COVID-19 among patients undergoing MT remains unknown. In this study, we sought to determine the rate of COVID-19 infection among patients undergoing MT in a prospective, multicenter, international observational study. We also aimed to evaluate baseline features among patients undergoing MT during the pandemic and determining the impact of protocol changes on outcomes.
Methods
Centers and patient variables
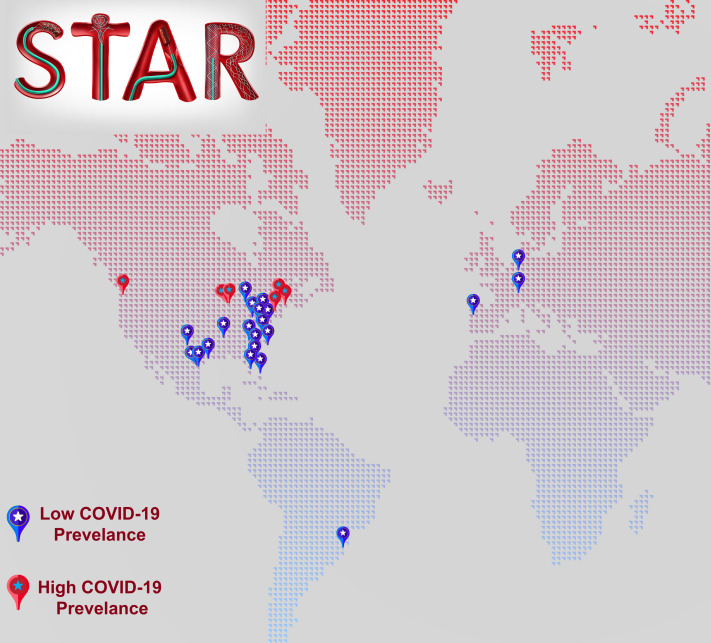
We prospectively collected data from 28 thrombectomy-capable stroke centers from two working collaborations: Stroke Thrombectomy and Aneurysm Registry (STAR) and Endovascular Neurosurgery Research Group (ENRG), including centers in North America, South America, and Europe (figure 1). Consecutive patients who underwent MT for LVO during the peak 2 months of the COVID-19 surge (February–March or March–April 2020, depending on the individual site). We evaluated the rate of COVID-19 in MT patients during the COVID-19 surge period. Testing was performed for symptomatic patients only using real-time reverse transcriptase-polymerase chain reaction of nasopharyngeal swabs.18 Collected data included baseline demographics, admission National Institute Health Stroke Scale (NIHSS), whether or not patients received intravenous alteplase (tPA), time from last known normal (LKN) to hospital arrival, Alberta Stroke Program Early CT score (ASPECTS) for patients with anterior circulation strokes, location of occlusion, door to groin puncture time, thrombectomy procedure duration, number of attempts, complication rate, and rate of symptomatic intracranial hemorrhage. Using data from Johns Hopkins University Center for Systems Science and Engineering COVID-19 tracking project,19 we determined that centers that are located in counties with COVID-19 rate of ≥500 cases per 100 000 people (as of May 1 2020) were considered high COVID-19 burden counties (HCC), and centers with <500 cases per 100 000 people were considered low COVID-19 counties (LCC). Successful revascularization was defined as modified thrombolysis in cerebral infarction 2B-3. Symptomatic intracranial hemorrhage (sICH) was as worsening of 4 or more points in NIHSS attributed to hemorrhagic transformation,20 and favorable discharge outcome was defined as modified Rankin scale (mRS) of 0–2 on discharge. Procedural data was adjudicated by the investigators in each of the included centers.
Figure 1.
Locations of the included centers in this study.
Statistical analysis
We used descriptive statistics to report patient demographic and clinical characteristics using median and IQR for continuous variables and percentages for categorical variables. Characteristics of groups were compared using the Wilcoxon rank-sum (Mann–Whitney U) test, Fisher’s exact test, and chi-square as appropriate. To evaluate the effect of COVID-19 infection on the discharge outcomes of MT patients, we used inverse probability of treatment weight (IPTW) using propensity scores to estimate a generalized linear model with a logit link function. The propensity scores were calculated using a binary logistic regression model for COVID-19 status using age, NIHSS, LKN to groin puncture, and location of LVO as predictors. Covariates in the propensity score model that had a less than 0.20 standardized difference before and after weighting were considered well-matched. Finally, to assess the relationship between intubation prior to MT and favorable discharge outcome (mRS 0–2), we estimated a generalized linear model with logit link to control for confounders including age, door to reperfusion time, tPA status, admission NIHSS, and location of LVO. All final models were tested for collinearity. An alpha level of 0.05 was used as the level of statistical significance. The analysis was conducted using SPSS v25 (IBM Corporation, New York, NY).
Results
Patient population
During the COVID-19 surge period (February–April 2020), 458 patients underwent MT in 28 centers from five countries (USA, Germany, Switzerland, Portugal, and Uruguay) (figure 1). The median age was 71 (IQR 60–80) years' old, admission NIHSS 16 (10-21), LKN to hospital door duration 260 (IQR 119–506), and ASPECTS 8 (IQR 7–10). Our cohort included 210 (45.9%) females, 310 (67.7%) white patients, 46 (10%) patients with posterior circulation occlusion, and 184 (40.2%) patients who received IV tPA (table 1). Thirteen (2.8%) patients were confirmed COVID-19 positive out of 242 MT patients who were tested; two were confirmed positive on admission and 11 during the same hospitalization. Of the 242 patients that were tested, 50 were in HCC, of which nine (18%) were positive, and 192 were LCC of which 4 (2.1%) were positive (P<0.001).
Table 1.
Patient, procedural, and outcome metrics of stroke patients treated with mechanical thrombectomy at the 28 international sites and divided by COVID-19 status
| All patients (n=458) | COVID-19 positive patents (n=13) | Non-COVID-19 patients (n=445) | P-value* | |
| Age, median (IQR) | 71 (60–80) | 58 (50–71) | 72 (60–80) | 0.04 |
| Females, n (%) | 210 (45.9%) | 5 (38.5%) | 205 (46.1%) | 0.779 |
| White, n (%) | 310 (67.7%) | 6 (46.2%) | 304 (68.3%) | 0.129 |
| LKN to hospital door, median (IQR) | 260 (119–506) | 202 (92–606) | 260 (119–506) | 0.557 |
| Admission NIHSS, median (IQR) | 16 (10–21) | 19 (16–24) | 15 (10–20) | 0.047 |
| IV-tPA, n (%) | 184 (40.2%) | 4 (30.8%) | 180 (40.4%) | 0.576 |
| ASPECTS, median (IQR)† | 8 (7–10) | 9 (8–10) | 8 (7–10) | 0.249 |
| Posterior circulation, n (%) | 46 (10%) | 0 | 46 (10.3%) | 0.38 |
| Intubation, n (%) | 241 (52.6%) | 5 (38.5%) | 236 (53%) | 0.4 |
| Door to groin, median (IQR) | 81 (50–127) | 56 (37–150) | 82 (50–127) | 0.315 |
| LKN to groin, median (IQR) | 351 (200–654) | 259 (181–343) | 355 (200–659) | 0.118 |
| Number of passes during thrombectomy, median (IQR) | 2 (1–3) | 2 (1–4) | 2 (1–3) | 0.189 |
| Successful recanalization (mTICI ≥2 b), n (%) | 381 (83.2%) | 13 (100%) | 368 (82.7%) | 0.138 |
| Procedure duration, median (IQR) | 40 (24–66) | 45 (29–76) | 40 (24–66) | 0.455 |
| Door to reperfusion, median (IQR) | 120 (75–178) | 86 (35–154) | 122 (76–178) | 0.064 |
| Length of stay, median (IQR) | 5 (3–10) | 8 (4–15) | 5 (3–10) | 0.231 |
| sICH, n (%) | 28 (6.1%) | 2 (15.4%) | 26 (5.8%) | 0.185 |
| In-hospital mortality, n (%)‡ | 80 (24.4) | 4 (33.3%) | 76 (24.1%) | 0.496 |
| DC mRS, median (IQR)‡ | 4 (2–5) | 4 (3–6) | 4 (2–5) | 0.443 |
| Functional independence on discharge (mRS 0–2), n (%)‡ | 96 (29.2%) | 2 (16.7%) | 94 (29.7%) | 0.52 |
*Calculated using Fisher's exact test for categorical variables and Wilcoxon test for the continuous variables.
†Only for patients with anterior circulation occlusion.
‡Missing for 130 patients.
ASPECTS, Alberta Stroke Program Early CT score; COVID-19, coronavirus disease of 2019; IV-tPA, intravenous tissue plasminogen activator; LKN, last known normal; mRS, modified Rankin Scale; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institute of Health Stroke Scale; sICH, symptomatic intracerebral hematoma.
COVID-19 positive vs non-COVID-19 patients
In COVID-19 positive patients, the median age was 58 (IQR 50–71) with a range of 35–98, and three patients were younger than 50 years of age. COVID-19 patients had a higher NIHSS on admission (19 (IQR 16–24) vs 15 (IQR 10–20), P=0.047), otherwise there was no difference in the percentage of female patients (38.5% vs 46.1%, P=0.779), percentage of white patients (46.2% vs 68.3%, P=0.129), or LKN to hospital door duration (202 (IQR 92–606) vs 260 (IQR 119–506), P=0.557), in-hospital mortality rate (33.3% vs 24.1%, P=0.496), length of stay (8 (IQR 4–15) vs 5 (IQR 3–10), discharge mRS (4 (IQR 3–6) vs 4 (IQR 2–5), P=0.443), or rate of functional independence (mRS 0–2) at discharge (2 (16.7%) vs 94 (29.7%), P=0.52) between COVID-19 and non-COVID-19 patients. The full characteristics of MT patients with confirmed COVID-19 are summarized in table 1. On multivariate analysis using logistic regression model with IPTW and propensity score, COVID-19 status was not associated with in-hospital mortality (RR 2.19, 95% CI 0.585 to 8.199, P=0.244) or functional independence (mRS 0–2) on discharge (RR 0.493, 95% CI 0.101 to 2.412, P=0.383).
High vs low prevalence COVID-19 counties
Five centers with 104 patients treated with MT met the criteria for HCC, and the remaining 354 patients in 23 centers were considered LCC. There was a higher number of patients who tested positive for COVID-19 infection in HCC (9 (8.6%) vs 4 (1.1%), P≤0.001). Six of those positive COVID-19 cases inHCC came from a single institution where the incidence was 6/30 (20%). Of the nine patients from HCC, two were positive on admission and the remaining tested positive during admission. All four patients in LCC tested positive during admission. Table 2 summarizes baseline features and outcomes between HCC and LCC groups. Notably, there was a trend toward longer door to groin time in the LCC group (85 (45-127) min vs 68 (36-123) min, P=0.054). In addition, more patients received tPA in the LCC group (29 (27.9%) vs 155 (43.8%), P=0.004). There was no significant difference in any other variables between the two groups.
Table 2.
Clinical characteristics and outcomes of patients in high and low COVID-19 counties
| Thrombectomy patients in high COVID-19 burden counties (n=104) | Thrombectomy patients in low COVID-19 counties (n=354) | P-value* | |
| Age, median (IQR) | 70 (58–78) | 72 (60–80) | 0.219 |
| Females, n (%) | 46 (44.2%) | 164 (46.3%) | 0.706 |
| White, n (%) | 71 (68.3%) | 239 (67.5%) | 0.885 |
| LKN to hospital door, median (IQR) | 286 (144–639) | 255 (105–490) | 0.262 |
| Admission NIHSS, median (IQR) | 15 (11–20) | 16 (10–21) | 0.491 |
| IV-tPA, n (%) | 29 (27.9%) | 155 (43.8%) | 0.004 |
| ASPECTS, median (IQR)† | 9 (8–10) | 8 (7–10) | 0.063 |
| Posterior circulation, n (%) | 8 (7.7%) | 38 (10.7%) | 0.364 |
| Intubation, n (%) | 38 (36.5%) | 203 (57.3%) | <0.001 |
| Door to groin, median (IQR) | 68 (36–123) | 85 (54–127) | 0.054 |
| LKN to groin, median (IQR) | 350 (195–686) | 352 (200–651) | 0.529 |
| Number of passes, median (IQR) | 2 (1–3) | 2 (1–3) | 0.395 |
| mTICI ≥2 b, n (%) | 83 (79.8%) | 298 (84.2%) | 0.294 |
| Procedure duration, median (IQR) | 35 (23–62) | 41 (25–69) | 0.177 |
| Door to reperfusion, median (IQR) | 111 (60–188) | 127 (79–176) | 0.221 |
| Length of stay, median (IQR) | 5 (3–10) | 6 (3–10) | 0.387 |
| DC mRS, median (IQR)‡ | 4 (2–6) | 4 (2–5) | 0.713 |
| Functional independence at discharge (mRS 0–2), n (%)‡ | 23 (30.7%) | 73 (28.7%) | 0.747 |
| sICH, n (%) | 9 (8.7%) | 19 (5.4%) | 0.219 |
*Calculated using chi-square test for categorical variables and Wilcoxon test for the continuous variables.
†Only for patients with anterior circulation occlusion.
‡Missing for 130 patients.
ASPECTS, Alberta Stroke Program Early CT score; COVID-19, coronavirus disease of 2019; DC, discharge; IV-tPA, intravenous tissue plasminogen activator; LKN, last known normal; mRS, modified Rankin Scale; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institute of Health Stroke Scale; sICH, symptomatic intracerebral hematoma.
General anesthesia vs monitored anesthesia care
A total of 243 (53.1%) were intubated and underwent MT under general anesthesia (GA) (241 patients were intubated prior to the procedure and two patients required intubation during the procedure). The remaining 215 patients underwent MT with monitored anesthesia care (MAC) (n=215). Table 3 summarizes baseline demographics and outcomes in the GA and MAC groups. Compared with the MAC group, GA patients were younger (70 (IQR 58–79) vs 73 (IQR 63–82) years' old, P=0.02), more likely to have received tPA (110 (45.6%) vs 73 (34%), P=0.011), had higher rate of posterior circulation LVOs (31 (12.9%) vs 15 (7%), P=0.037), longer door to groin puncture time (92 (IQR 62–136) vs 67 (35-112) minutes, P<0.001), longer procedure duration (47 (IQR 92–188) vs 32 (19-56) minutes, P<0.001), and longer overall door to reperfusion time (138 (IQR 92–188) vs 100 (IQR 64–156) min, P≤0.001). Less patients in the GA group were functionally independent (mRS 0–2) at discharge compared with the MAC group (45 (24.5%) vs 51 (35.4%), P=0.03). There was no difference in any other variable between the two groups.
Table 3.
Clinical characteristics and outcomes of patients who underwent mechanical thrombectomy under general anesthesia vs monitored anesthesia care
| General anesthesia (n=241)* | Monitored anesthesia care (n=215) | P-value† | |
| Age, median (IQR) | 70 (58–79) | 73 (63–82) | 0.02 |
| Females, n (%) | 104 (43.2%) | 105 (48.8%) | 0.224 |
| White, n (%) | 160 (66.4%) | 149 (69.3%) | 0.507 |
| LKN to hospital door, median (IQR) | 283 (100–485) | 255 (120–517) | 0.791 |
| Admission NIHSS, median (IQR) | 16 (10–22) | 15 (10–20) | 0.226 |
| IV-tPA, n (%) | 110 (45.6%) | 73 (34%) | 0.011 |
| ASPECTS, median (IQR)‡ | 8 (7–10) | 9 (7–10) | 0.305 |
| Posterior circulation, n (%) | 31 (12.9%) | 15 (7%) | 0.037 |
| Door to groin, median (IQR) | 92 (62–136) | 67 (35–112) | <0.001 |
| LKN to groin, median (IQR) | 355 (213–620) | 335 (191–687) | 0.564 |
| Number of passes, median (IQR) | 2 (1–3) | 2 (1–3) | 0.138 |
| Achieved successful reperfusion, n (%) | 198 (82.2%) | 181 (84.2%) | 0.564 |
| Procedure duration, median (IQR) | 47 (27–76) | 32 (19–56) | <0.001 |
| Door to reperfusion, median (IQR) | 138 (92–188) | 100 (64–156) | <0.001 |
| Length of stay, median (IQR) | 6 (3–11) | 5 (3–9) | 0.111 |
| DC mRS, median (IQR)§ | 4 (3–6) | 4 (2–5) | 0.008 |
| Functional independence on discharge (mRS 0–2), n (%)§ | 45 (24.5%) | 51 (35.4%) | 0.03 |
| sICH, n (%) | 17 (7.1%) | 11 (5.1%) | 0.39 |
*Excluded two patients who required intra-procedural intubation.
†Calculated using chi-suare test for categorical variables and Wilcoxon test for the continuous variables.
‡Only for patients with anterior circulation occlusion.
§Missing for 128 patients (57 in the intubated group and 71 in the un intubated group).
ASPECTS, Alberta Stroke Program Early CT score; COVID, coronavirus disease of 2019; DC, discharge; IV-tPA, intravenous tissue plasminogen activator; LKN, last known normal; mRS, modified Rankin Scale; mTICI, modified Thrombolysis in Cerebral Infarction; NIHSS, National Institute of Health Stroke Scale; sICH, symptomatic intracerebral hematoma.
On multivariate analysis, intubation status was associated with higher probability of in-hospital mortality (RR 1.871, 95% CI 1.066 to 3.284, P=0.029) and lower probability of functional independence on discharge (0.53, 95% CI 0.318 to 0.884, P=0.015) after controlling for age, door to reperfusion duration, tPA status, admission NIHSS, and location of occlusion. Of note, discharge mRS was missing for 57 (23.6%) patients in the intubated group and 71 (33%) in the non-intubated group.
Discussion
Several studies have evaluated the incidence of neurologic symptoms in patients with COVID-19. A study by Mao et al evaluated 214 patients with confirmed COVID-19 infection at three centers in China.5 In this study, 78 (36.4%) patients had neurologic manifestations. Acute cerebrovascular diseases were observed in five patients. Another Chinese study reported a similar incidence of acute cerebrovascular disease of 5.8% (13/221).21 Of these, 11 were arterial ischemic stroke, one was venous sinus thrombosis, and one was intracerebral hemorrhage. However, to date there are no reports regarding the incidence or prevalence of COVID-19 among patients presenting with emergent LVO. In this prospective, observational, multicenter international study we evaluated the rate of COVID-19 infection among patients undergoing MT: we also evaluated the impact of the COVID-19 pandemic on MT-related time metrics and clinical outcomes. We found that 2.8% of patients undergoing MT tested positive for COVID-19. In HCC, approximately 8.6% of patients undergoing MT tested positive for COVID-19 compared with 1.1% in LCC.
Cerebrovascular complications are reported in approximately 5% of patients admitted with COVID-19.7 Ischemic stroke in the setting of COVID-19 might occur concurrently either from common stroke risk factors such as hypertension, diabetes mellitus, hyperlipidemia, and atrial fibrillation, as a hypercoaguability- related complication due to COVID-19, a proinflammatory state, or due to decompensation in patients with underlying cerebrovascular disease such as extracranial or intra-cranial stenosis.7 8 22 23 As such, a recent report from New York raised the concern of a possible association between COVID-19 and LVO in young patients.8 Among the five reported patients however, three had vascular risk factors.8 In our study, while COVID-19 patients were relatively younger than non-COVID patients undergoing MT (58 vs 72), only 3/13 patients with confirmed COVID-19 infection were younger than 50 and the youngest was 35. While it is possible that COVID-19 could be associated with acute ischemic stroke in young, previously healthy patients, there is no evidence that this is a widespread phenomenon.
With the goal of protecting healthcare providers and optimizing neurologic outcomes among patients undergoing MT, and in light of potential and severe personal protective equipment shortages, various neuro-interventional societies have published recommendations based on expert consensus to guide interventionists performing MT. Some of the recommendations, especially related to the type of anesthetic use (MAC vs GA), required drastic changes in local protocols. The Society of Neurointerventional Surgery recommended a lower threshold for intubation prior to MT in patients who are either positive for COVID-19 or possibly could be positive (unknown or unconfirmed negative status).12 Similarly, the Society of Neuroscience in Anesthesiology & Critical Care recommended lower threshold for intubating patients with unknown COVID-19 status.16 While the intubation itself places the providers performing the intubation procedure at risk, the rationale for lowering thresholds for intubation involved protecting against unplanned aerosol generation, for example, a patient who decompensates during the MT procedure and requires intubation. On the other hand, the Society for Vascular and Interventional Neurology recommended considering MAC if possible to protect anesthesiologists from exposure and to reduce unnecessary intubation as well as conserve mechanical ventilator resources.13 Thus, there remains considerable uncertainty regarding ‘best practices’ as the pandemic progresses across the world.
Somewhat paradoxically, significantly higher number of patients were intubated in LCC prior to MT, which was associated with longer door to reperfusion times. Evidence from clinical trials indicates that GA is non-inferior to MAC in patients undergoing MT24–26 and in clinical practice there is considerable variability. In this study, 241/458 (52.6%) of the patients underwent planned pre-procedure GA, and only 2/194 (1%) required emergent, unplanned intra-procedural intubation. We found an approximately 25 min delay in door to groin times in patients undergoing GA compared with MAC. Similarly, door to reperfusion time was approximately 38 min longer in GA patients. In this study, despite relatively younger age for GA patients and higher rate of intravenous thrombolysis, independence at discharge was significantly lower in GA patients (24.5% vs 35.4%). By contrast, The Anesthesia During Stroke (AnStroke) and the General Or Local Anesthesia in Intra Arterial Therapy (GOLIATH) trials both showed no difference in long-term outcomes between patients undergoing MT with GA compared with MAC.27 28 However, in both trials there was no difference in door to groin puncture time or symptom onset to reperfusion duration between the GA and MAC groups. Similarly, there was no difference in time from symptom onset to reperfusion. A post hoc analysis of data collected in the MR CLEAN trial demonstrated an approximately 32 min delay with GA which was associated with worse outcome.29
In our study the majority of sites were not intubating most patients for MT prior to the pandemic, but rather did so following scientific society recommendations. It is therefore possible that the worsened outcomes in the GA group were as a direct result of the delay in door to reperfusion times compared with MAC patients. Changes in local protocols take time to become streamlined and when first implemented are often not optimized into the patient workflow. This consideration was likely exacerbated by other pandemic-related protocols affecting supporting services. Unlike centers that routinely perform MT under GA, centers that primarily perform MT under MAC are likely to encounter longer times to intubate and therefore delayed door to groin puncture times, as identified in this study. Beyond the actual intubation procedure itself, local protocols commonly dictated transporting patients to designated negative pressure rooms and mandated wait times prior to transporting up to the angiography suite. It is important to note that all these changes in patient care workflow likely contributed to the observed effect.
Strengths and limitations
This study’s strengths include the relatively large volume of patients and the prospective, multicenter nature of the data. The main limitations of the study include lack of long-term functional outcomes and missing discharge mRS for a considerable number of patients given that the study was undertaken between the months of January and April of this year and many of the included patients were still admitted when the analysis was conducted. Another limitation is that not all MT patients in our study were tested for COVID-19 which may have resulted in missing some of asymptomatic COVID-19 patients. Also, we cannot rule out false negativity in symptomatic patients either. In addition, this study cannot provide data related to whether COVID-19 is associated with LVO, particularly in the young especially given that HCC patients were under-represented in this cohort. This multicenter experience, however, provides preliminary demographic data on patients undergoing MT.
Conclusions
In this prospective, multicenter, international study, we found a low number of confirmed COVID-19 infections among stroke patients with LVO undergoing MT in LCC. Intubation prior to MT during the early stages adjustment to COVID-19 pandemic was associated with a higher in-hospital mortality rate and lower rate of functional independence on discharge.
Footnotes
Twitter: @DrMichaelLevitt, @PascalJabbourMD, @AhmadSweidMD, @Starke_neurosurgery, @AdamArthurMD, @abhipandhi, @BrianHoward_MD, @brainvesseldoc, @SantiagoGP92, @alex_spiotta
Collaborators: Dileep R Yavagal MD, Eric C Peterson MD, Daniel Raper MBBS, Patrick A Brown MD, M. Reid Gooch MD, Nabeel Herial MD, Ajith Thomas MD, Justin Moore MD, Felipe Albuquerque MD, Louis J. Kim MD, Melanie Walker MD, Michael Chen MD, Stephan Munich MD, Daniel Alan Hoit MD MPH, Violiza Inoa-Acosta MD, Christopher Nickele MD, Lucas Elijovich MD, Fernanda Rodriguez-Erazú PD Dr. med. Jan Liman, Michael Cawley, MD, Gustavo Pradilla MD, Brian Walcot, MD, Zeguang Re, MD PhD, Ryan Hebert MD, João Rei, MD, Jaime Pamplon, Rui Carvalho MD, Mariana Baptist, MD, Ana Nunes MD, Russell Cerejo MD, Ashis Tayal MD, Parita Bhuv, MD, Paul Hansen MD, Norman Ajiboye MD, Alex Brehm, MD
Contributors: All authors have: provided a substantial contribution to the conception and design of the studies and/or the acquisition and/or the analysis of the data and/or the interpretation of the data. They have drafted the work or revised it for significant intellectual content and approved the final version of the manuscript. They agree to be accountable for all aspects of the work, including its accuracy and integrity.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction, or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Additional data from this project can be acquired by contacting the corresponding author.
References
- 1. Organization WH Coronavirus disease 2019 (COVID-19): situation report, 117, 2020. [Google Scholar]
- 2. Li Q, Guan X, Wu P, et al. . Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liu W, Tao Z-W, Wang L, et al. . Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J 2020;133:1032–8. 10.1097/CM9.0000000000000775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang C, Wang Y, Li X, et al. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mao L, Jin H, Wang M, et al. . Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020;77:683–90. 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Poyiadji N, Shahin G, Noujaim D, et al. . COVID-19–associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology 2020;296:E119–20. 10.1148/radiol.2020201187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li Y, Li M, Wang M, et al. . Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol 2020. doi: 10.1136/svn-2020-000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Oxley TJ, Mocco J, Majidi S, et al. . Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med 2020;382:e60. 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Helms J, Tacquard C, Severac F, et al. . High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020;46:1–10. 10.1007/s00134-020-06062-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Klok FA, Kruip MJHA, van der Meer NJM, et al. . Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–7. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Levi M, Thachil J, Iba T, et al. . Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol 2020;S2352-3026:30145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fraser JF, Arthur AS, Chen M, et al. . Society of NeuroInterventional Surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19. J Neurointerv Surg 2020;12:539–41. 10.1136/neurintsurg-2020-016098 [DOI] [PubMed] [Google Scholar]
- 13. Nguyen TN, Abdalkader M, Jovin TG, et al. . Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the Society of vascular and Interventional Neurology. Stroke 2020;51:1896–901. 10.1161/STROKEAHA.120.030100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aggour M, White P, Kulcsar Z, et al. . European Society of Minimally Invasive Neurological Therapy (ESMINT) recommendations for optimal interventional neurovascular management in the COVID-19 era. J Neurointerv Surg 2020;12:542–4. 10.1136/neurintsurg-2020-016137 [DOI] [PubMed] [Google Scholar]
- 15. Smith MS, Bonomo J, Knight WA, et al. . Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke 2020;51:1902–9. 10.1161/STROKEAHA.120.029863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sharma D, Rasmussen M, Han R, et al. . Anesthetic Management of Endovascular Treatment of Acute Ischemic Stroke During COVID-19 Pandemic: Consensus Statement From Society for Neuroscience in Anesthesiology & Critical Care (SNACC): endorsed by Society of Vascular & Interventional Neurology (SVIN), Society of NeuroInterventional Surgery (SNIS), Neurocritical Care Society (NCS), European Society of Minimally Invasive Neurological Therapy (ESMINT) and American Association of Neurological Surgeons (AANS) and Congress of Neurological Surgeons (CNS) Cerebrovascular Section. J Neurosurg Anesthesiol 2020;32:193–201. 10.1097/ANA.0000000000000688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fiorella D, Fargen KM, Leslie-Mazwi TM, et al. . Neurointervention for emergent large vessel occlusion during the COVID-19 pandemic. J Neurointerv Surg 2020;12:537–8. 10.1136/neurintsurg-2020-016117 [DOI] [PubMed] [Google Scholar]
- 18. Wang W, Xu Y, Gao R, et al. . Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hacke W, Kaste M, Bluhmki E, et al. . Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–29. 10.1056/NEJMoa0804656 [DOI] [PubMed] [Google Scholar]
- 21. Filatov A, Sharma P, Hindi F, et al. . Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus 2020;12:e7352. 10.7759/cureus.7352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mei H, Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19. Zhonghua Xue Ye Xue Za Zhi 2020;41:185–91. 10.3760/cma.j.issn.0253-2727.2020.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thachil J. The versatile heparin in COVID-19. J Thromb Haemost 2020;18:1020–2. 10.1111/jth.14821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schönenberger S, Hendén PL, Simonsen CZ, et al. . Association of General Anesthesia vs procedural sedation with functional outcome among patients with acute ischemic stroke undergoing thrombectomy: a systematic review and meta-analysis. JAMA 2019;322:1283–93. 10.1001/jama.2019.11455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Campbell D, Diprose WK, Deng C, et al. . General anesthesia versus conscious sedation in endovascular thrombectomy for stroke: a meta-analysis of 4 randomized controlled trials. J Neurosurg Anesthesiol 2019. doi: 10.1097/ANA.0000000000000646 [DOI] [PubMed] [Google Scholar]
- 26. Zhang Y, Jia L, Fang F, et al. . General anesthesia versus conscious sedation for intracranial mechanical thrombectomy: a systematic review and meta-analysis of randomized clinical trials. J Am Heart Assoc 2019;8:e011754. 10.1161/JAHA.118.011754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Löwhagen Hendén P, Rentzos A, Karlsson J-E, et al. . General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke: the AnStroke Trial (anesthesia during stroke). Stroke 2017;48:1601–7. 10.1161/STROKEAHA.117.016554 [DOI] [PubMed] [Google Scholar]
- 28. Simonsen CZ, Yoo AJ, Sørensen LH, et al. . Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke: a randomized clinical trial. JAMA Neurol 2018;75:470–7. 10.1001/jamaneurol.2017.4474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berkhemer OA, van den Berg LA, Fransen PSS, et al. . The effect of anesthetic management during intra-arterial therapy for acute stroke in MR CLEAN. Neurology 2016;87:656–64. 10.1212/WNL.0000000000002976 [DOI] [PubMed] [Google Scholar]