Abstract
BACKGROUND
Reprogramming of host metabolism supports viral pathogenesis by fueling viral proliferation, by providing, for example, free amino acids and fatty acids as building blocks.
METHODS
To investigate metabolic effects of SARS-CoV-2 infection, we evaluated serum metabolites of patients with COVID-19 (n = 33; diagnosed by nucleic acid testing), as compared with COVID-19–negative controls (n = 16).
RESULTS
Targeted and untargeted metabolomics analyses identified altered tryptophan metabolism into the kynurenine pathway, which regulates inflammation and immunity. Indeed, these changes in tryptophan metabolism correlated with interleukin-6 (IL-6) levels. Widespread dysregulation of nitrogen metabolism was also seen in infected patients, with altered levels of most amino acids, along with increased markers of oxidant stress (e.g., methionine sulfoxide, cystine), proteolysis, and renal dysfunction (e.g., creatine, creatinine, polyamines). Increased circulating levels of glucose and free fatty acids were also observed, consistent with altered carbon homeostasis. Interestingly, metabolite levels in these pathways correlated with clinical laboratory markers of inflammation (i.e., IL-6 and C-reactive protein) and renal function (i.e., blood urea nitrogen).
CONCLUSION
In conclusion, this initial observational study identified amino acid and fatty acid metabolism as correlates of COVID-19, providing mechanistic insights, potential markers of clinical severity, and potential therapeutic targets.
FUNDING
Boettcher Foundation Webb-Waring Biomedical Research Award; National Institute of General and Medical Sciences, NIH; and National Heart, Lung, and Blood Institute, NIH.
Keywords: COVID-19, Metabolism
Keywords: Amino acid metabolism, Intermediary metabolism
COVID-19 infection dysregulates nitrogen and carbon metabolism, and increases serum levels of free fatty acids and glucose, thereby increasing tryptophan metabolism into the kynurenine pathway.
Introduction
On December 12, 2019, the first patient presented in Wuhan, Hubei province, China, with symptoms consistent with severe acute respiratory syndrome (SARS). Investigators soon realized that these symptoms were caused by a newly identified RNA virus strain belonging to the Coronaviridae family and referred to it as “2019-nCoV” (1). Phylogenetic analyses of the genome (29,903 nucleotides) demonstrated its similarity (89.1%) to a group of SARS-like coronaviruses (genus Betacoronavirus, subgenus Sarbecovirus) previously isolated in bats in China (1). The virus has since spread worldwide, resulting in 10,185,374 confirmed cases and 503,862 confirmed deaths as of June 30, 2020, according to data from WHO (2).
To face the global pandemic, nations initiated lockdowns, social distancing, and mandatory regulations regarding wearing personal protective equipment. A worldwide mobilization of scientists also occurred, in an effort to slow viral spread, identify suitable therapies, and expedite vaccine development and testing (3). This rapidly generated new information and a concomitant concern for the quality of the resulting evidence (4).
COVID-19 initiates multiple symptoms, including fever, persistent dry cough, shortness of breath, chills, muscle pain, headache, loss of taste or smell, and gastrointestinal symptoms. However, some subjects are more susceptible, by unknown mechanisms, to develop severe disease, especially older males with various comorbidities, including obesity, diabetes, cardiovascular disease, or immunosuppression (e.g., in cancer patients or transplant patients). In contrast, children, younger adults, and women tend to be either asymptomatic or present with mild disease, while remaining contagious and contributing to viral transmission. As such, widespread testing, even of asymptomatic subjects, has been recommended for monitoring and preventing disease dissemination. Testing of nasopharyngeal swabs with molecular assays was introduced worldwide to diagnose disease and monitor recovery; for example, Italy enforces quarantine of any positive subjects until they are symptom free for at least 14 days and test negative twice within 24 hours. However, logistical issues have limited generalized testing in most countries, including the United States (<12,000 tests/million people) (5). Nonetheless, serological testing for antibodies against SARS-CoV-2 proteins suggests that a significantly larger fraction of the total population was infected than identified by molecular testing (e.g., up to 85-fold higher) (6). These findings provoked ongoing debate, especially regarding test sensitivity and specificity and the distinction between case fatality rates (mortality among those testing positive by molecular assays) and infection fatality rates (extrapolated from serological results), resulting in estimates of approximately 75-fold and approximately 7-fold higher mortality than seasonal influenza, respectively. Large international initiatives (e.g., Solidarity II) proposed to tackle this issue through homogeneous serological testing in 12 countries (7). In addition, serological testing detects antibodies against SARS-CoV-2 proteins in patients who recovered from infection; they are being actively enrolled as “convalescent” plasma donors to determine whether their antibodies can stop spread of the virus and provide therapeutic benefit in actively infected patients (8).
Recombinant expression of SARS-CoV-2 proteins, along with structural and protein-protein interaction (9) studies, confirm that, like other coronaviruses (10), the SARS-CoV-2 spike protein S interacts with the angiotensin converting enzyme receptor 2 (ACE2) to penetrate host cells, especially lung epithelium (11). Disrupting this interaction may provide a therapeutic target (12, 13) and is the strategy of vaccine candidates aiming to elicit humoral responses to capsid proteins (3, 14). Still, it is unclear whether, and for how long, recovered patients are immune to this virus; therefore, the scientific community is invested in defining interventions to treat the most severe symptoms of COVID-19. For example, in March 2020, preliminary evidence seemed to suggest a beneficial role for antimalarial drugs (e.g., hydroxychloroquine), especially in combination with azithromycin (15); however, a larger clinical trial showed a deleterious effect (e.g., a ~2-fold increase in mortality) for patients on hydroxychloroquine (with or without azithromycin) (16). Other treatments, while effective in sanitizing inert surfaces (e.g., UV light or bleach) (17), are clearly incompatible with the primum non nocere principle of medical practice. Although using antiretroviral drugs to treat SARS coronaviruses was proposed in vitro (18), no clinical evidence in vivo has yet been provided; nonetheless, ongoing trials with remdesivir show promise, with approximately 30% faster recovery and reduced mortality (ClinicalTrials.gov identifier NCT04280705).
Given the difficulties in preventing infection or decreasing viral load, multiple approaches are being used to identify key pathways involved in SARS-CoV-2 infection. For example, the most severe cases exhibit “cytokine storm,” driven by sustained increases in circulating interleukin-6 (IL-6) levels (19). Antibody-based approaches (e.g., tocilizumab) are currently being tested as a strategy to mitigate the clinical complications of COVID-19–induced cytokines (19). Notably, this extreme inflammation often requires ventilator support or, even, extracorporeal membrane oxygenation (20). However, in approximately 80% of cases, the latter did not prevent mortality, owing to insufficient lung perfusion, which could be explained by developing thromboembolic complications (21). In this context, clinical trials are underway to determine whether anticoagulants (e.g., heparin) or profibrinolytic drugs (e.g., tissue plasminogen activator) ameliorate severe infection with thromboembolic complications (22). Interestingly, platelets from older subjects are hypercoagulable in the presence of proinflammatory stimuli (23), which may help explain the increased mortality in older patients with COVID-19. Of note, small-molecule metabolites are used to treat coagulopathies (e.g., tranexamic acid for hyperfibrinolysis in active hemorrhage) (24). However, to date, nothing is known about the serum metabolome of patients with COVID-19.
Small-molecule metabolites are essential for viral infection because they provide building blocks that a rapidly proliferating virus requires to assemble its nucleic acids, proteins (including capsid proteins), and membrane. Indeed, viral infections mobilize free fatty acids to support capsid-associated membrane formation, which was described for other coronaviruses and is explained, in part, by activating phospholipase A2, a target amenable to pharmacological intervention (25–27). The current study likely provides the first comprehensive targeted and untargeted metabolomics analysis of sera from patients with COVID-19, stratified by circulating levels of IL-6, and correlated to inflammatory markers and renal function. Though observational, this study identifies substantial alterations in fatty acid metabolism in infected patients and unanticipated alterations of glucose homeostasis and amino acid metabolism; specifically, dysregulated tryptophan, arginine, and sulfur metabolism are potential therapeutic targets.
Results
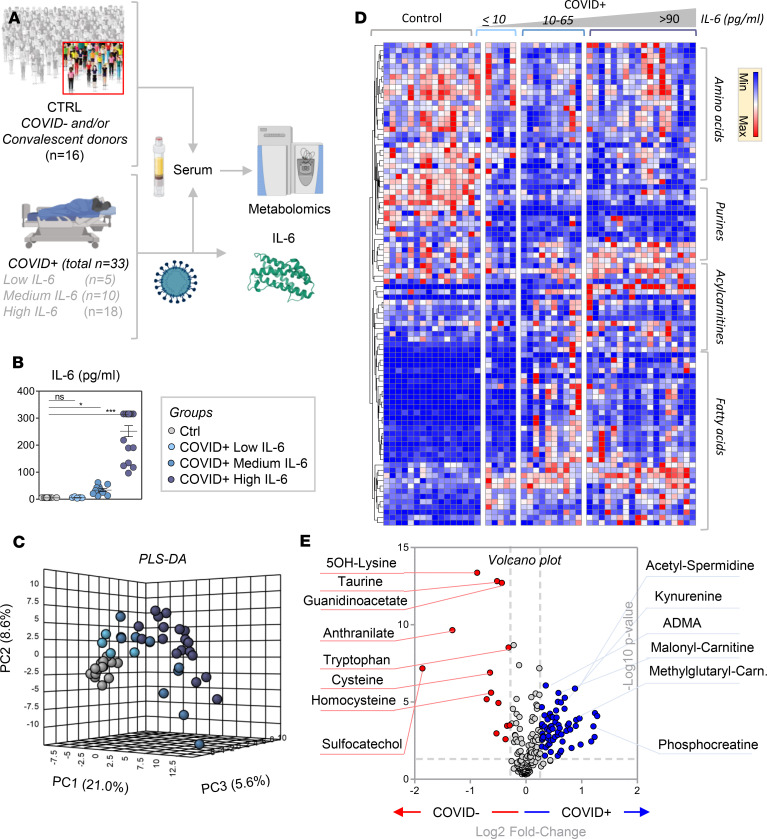
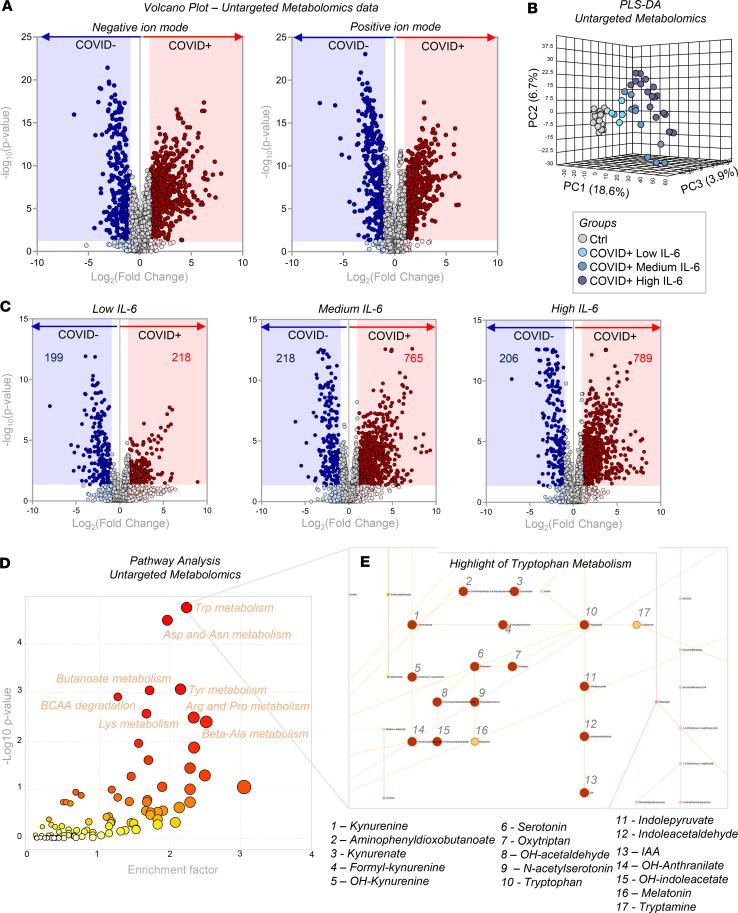
Forty-nine subjects were enrolled in this observational study: 33 COVID-19–positive subjects and 16 COVID-19–negative subjects; the latter included “never positive” subjects and convalescent plasma donors (Figure 1A). Owing to the skewed demographics of the COVID-19–positive patients (prevalence and mortality being ~2-fold higher in men) (28), 76% of the subjects in this group were male, 56.5 ± 18.1 years old (mean ± standard deviation) versus 38% male, 37.8 ± 11.6 years old for the control group. Of the COVID-19–positive patients, 5 subjects had IL-6 levels of less than 10 pg/mL; 10 subjects had IL-6 levels of 10–65 pg/mL, and 18 subjects had IL-6 levels of more than 90 pg/mL. Subjects in these 3 subgroups had no significant differences in age or sex. Reference ranges for IL-6 levels in healthy controls are less than 5 pg/mL (Figure 1B). Of all the COVID-19–positive subjects, only 6 had renal function parameters within the reference range (blood urea nitrogen [BUN] of 7–26 mg/dL and creatinine of 0.5–0.95 mg/dL), of which 3 were in the low and 2 in the medium IL-6 group (Supplemental Table 1 and Supplemental Figure 1A; supplemental material available online with this article; https://doi.org/10.1172/jci.insight.140327DS1). Targeted metabolomics analyses were performed on sera using ultra-high-pressure liquid chromatography-mass spectrometry (UHPLC-MS), and the results are reported extensively in Supplemental Table 1. The metabolic phenotypes of sera from COVID-19–positive patients differed substantially from controls, when examined by partial least squares discriminant analysis (PLS-DA; Figure 1C). Hierarchical clustering analysis (Figure 1D) highlighted significant associations of COVID-19 and IL-6 levels with amino acid metabolism, purines, acylcarnitines, and fatty acids; a vectorial version of this figure is provided in Supplemental Figure 2. Volcano plots (Figure 1E) from targeted metabolomics analyses highlighted the top metabolites that increased (blue) or decreased (red) in the sera of COVID-19–positive patients, as compared with controls. To expand on these observations, untargeted metabolomics analyses were performed based on high-resolution, accurate intact mass, isotopic patterns, and MS2 fragmentation patterns, as described previously (29); the “top” correlates with clinical laboratory parameters are reported in Supplemental Table 2. In Figure 2A, volcano plot analyses highlighted 3034 and 2484 differential metabolites for negative and positive ion modes between COVID-19–positive and –negative subjects, respectively. PLS-DA analysis based on untargeted metabolomics data supported the targeted results and further separated COVID-19–positive and COVID-19–negative subjects (Figure 2B), the former group separating from the latter across principal component 1 (18.7% of the total variance) as a function of IL-6 levels. Interestingly, volcano plot analyses comparing COVID-19–positive subjects with low, medium, and high serum IL-6 levels, as compared with controls, showed that the low IL-6 group was most comparable to controls (199 and 218 metabolites significantly decreasing and increasing), whereas the medium (218 and 765) and high IL-6 (206 and 789) groups differed the most (Figure 2C). Metabolite Set Enrichment Analysis (30) of merged targeted and untargeted metabolomics data revealed a significant impact of COVID-19 on amino acid metabolism, especially the pathways involving tryptophan, aspartate, arginine, tyrosine, and lysine (Figure 2D). Top hits from these pathways were mapped against Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway map hsa01100 in Supplemental Figure 3, and tryptophan metabolism is highlighted in Figure 2E. Targeted absolute quantitative measurements, as determined by stable isotope–labeled internal standards, are provided in Supplemental Table 1 for a subset of metabolites from the most significantly affected pathways.
Figure 1. Metabolomics analysis of patients with COVID-19.
(A) Forty-nine subjects were studied, of which 16 were COVID-19–negative and 33 were COVID-19–positive patients, as determined by nucleic acid testing of nasopharyngeal swabs. IL-6 levels were determined during routine clinical care using a clinically validated ELISA (B), and the results were used to divide COVID-19–positive patients into groups with low (≤10 pg/mL), medium (10–65 pg/mL) and high (>90 pg/mL) IL-6 levels (although IL-6 levels were treated as a continuous variable, no patients had a result of >65 but ≤90 pg/mL). Sera were obtained from these subjects for metabolomics analyses. Asterisks indicate significance by ANOVA (1-way ANOVA with Tukey’s multiple comparisons, *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). (C) The serum metabolic phenotypes of COVID-19–positive patients substantially differed from controls by PLS-DA. (D) Hierarchical clustering analysis highlighted a significant impact of COVID-19 and IL-6 levels on amino acid metabolism, purines, acylcarnitines, and fatty acids. A vectorial version of this figure is provided in Supplemental Figure 2. (E) The volcano plot derived from a targeted metabolomics analysis highlights the top serum metabolites that increased (shown in blue) or decreased (shown in red) in COVID-19–positive patients, as compared with controls.
Figure 2. Untargeted metabolomics analyses.
Untargeted metabolomics analyses were performed using sera obtained from COVID-19–positive and –negative subjects. (A) Volcano plots highlight 3034 and 2484 differential metabolites (unique molecular formulas were determined by high-resolution, accurate intact mass, isotopic patterns, and MS/MS analyses) for negative and positive ion modes (left and right), respectively. (B) PLS-DA based on the untargeted metabolomics data further separates COVID-19–negative and –positive subjects, the latter separating from the former across principal component 1 (18.7% of the total variance) as a function of IL-6 levels. (C) Volcano plots highlight differences between COVID-19–positive subjects with low, medium, and high serum IL-6 levels, as compared with controls. (D) Pathway analysis of untargeted metabolomics data identified significant effects of COVID-19 on amino acids, especially regarding tryptophan, aspartate, arginine, tyrosine, and lysine metabolism. (E) Tryptophan metabolism, one of the top hits from pathway analysis, is mapped against KEGG pathway map hsa01100.
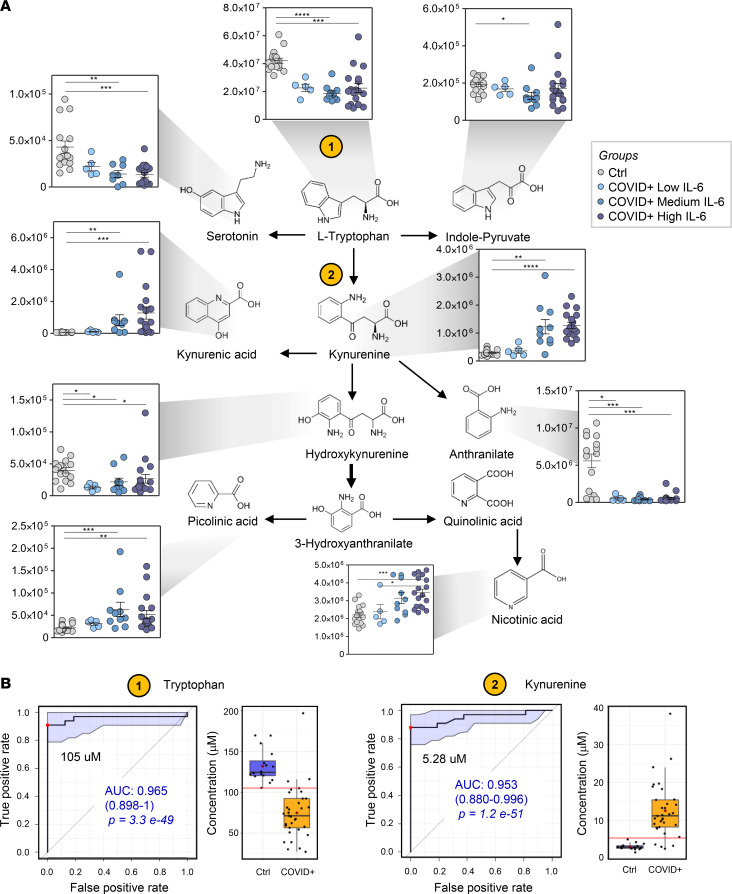
Alteration of tryptophan metabolism in sera of COVID-19–positive patients.
Tryptophan metabolism was the top pathway affected by COVID-19 in the analysis of targeted and untargeted metabolomics data (Figure 2E). As such, focused analysis of this pathway highlighted significant decreases (inversely proportional to IL-6 concentration) in tryptophan, serotonin, and indolepyruvate levels (Figure 3A). In contrast, increases in kynurenine, kynurenic acid, picolinic acid, and nicotinic acid, but not anthranilate, suggested hyperactivation of the kynurenine pathway (Figure 3A). Although it is beyond the scope of this work to identify diagnostic metabolic markers of COVID-19 positivity, receiver operating characteristic (ROC) curves were calculated for the absolute quantitative measurements of serum tryptophan and kynurenine in these sera (Figure 3B); interestingly, tryptophan levels lower than 105 μM and kynurenine levels higher than 5.3 μM had areas under the curves more than 95% in distinguishing between the 2 groups (positive vs. negative). The potential relevance of this observation will require additional study in the future.
Figure 3. Alterations of tryptophan metabolism in COVID-19–positive subjects.
(A) Tryptophan metabolism was identified in targeted and untargeted metabolomics data as the top pathway affected by COVID-19. Asterisks indicate significance by ANOVA (1-way ANOVA with Tukey’s multiple comparisons, *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). The y axis in the dot plots indicates arbitrary units (AU). In particular, decreases in tryptophan and increases in kynurenine were proportional to disease severity, as inferred by IL-6 levels, and predicted COVID-19 infection with good sensitivity and specificity, as shown by the ROC curves (B). The box plots depict the minimum and maximum values (whiskers), the upper and lower quartiles, and the median. The length of the box represents the interquartile range. The red horizontal lines represent the respective metabolite concentration thresholds used in the statistical model to differentiate COVID-19 and control subjects.
Dysregulation of amino acid metabolism in patients with COVID-19 as a function of IL-6 levels.
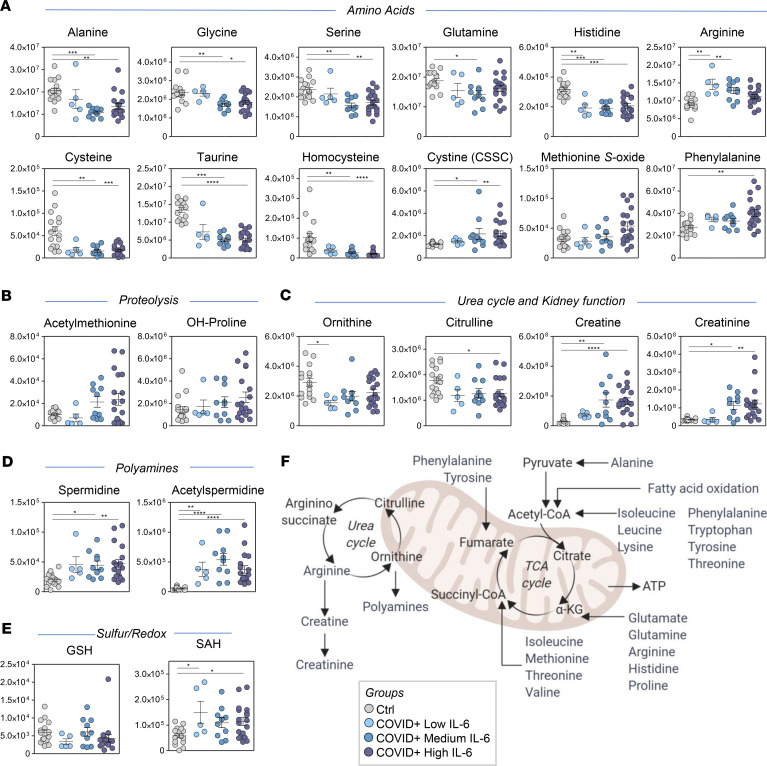
Beyond tryptophan, metabolomics analyses revealed a significant impact of SARS-CoV-2 infection on serum amino acid levels (Figure 4). Specifically, gluconeogenic (e.g., alanine, glycine, serine, glutamine, and histidine) and sulfur-containing amino acids (e.g., cysteine, taurine) tended to decrease, especially in the moderate-high IL-6 group (Figure 4A). In contrast, oxidized forms of sulfur-containing amino acids (e.g., methionine sulfoxide, cystine), as well as of arginine, increased (Figure 4A). Although no significant changes were noted in methionine levels, increases in acetyl-methionine and hydroxyproline, by-products of proteolysis and collagen catabolism, respectively, were observed, particularly in patients with COVID-19 with the highest IL-6 levels (Figure 4B). Despite increases in arginine, the urea cycle metabolic intermediates ornithine and citrulline decreased in patients with COVID-19 (Figure 4C). In addition, creatine and creatinine, as well as the polyamines spermidine and acetyl-spermidine, increased significantly, particularly in patients with medium and high IL-6 levels (Figure 4, C and D); this is suggestive of renal dysfunction in these groups, which was confirmed by clinical laboratory measurements of creatinine and BUN (Supplemental Table 1).
Figure 4. Amino acid levels and metabolism in sera of COVID-19–positive patients.
Serum levels of amino acids (A), proteolysis markers (B), urea cycle and renal function metabolites (C), polyamines (D), and sulfur-redox metabolism (E) showed significant differences between COVID-19–positive patients and controls. GSH, reduced glutathione; SAH, S-Adenosylhomocysteine. (F) An overview of the pathways related to these metabolites. Asterisks indicate significance by ANOVA (1-way ANOVA with Tukey’s multiple comparisons, *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). The y axis in the dot plots indicates AU.
Evidence of hyperglycemia, hemolysis, and lipid abnormalities in sera of patients with COVID-19.
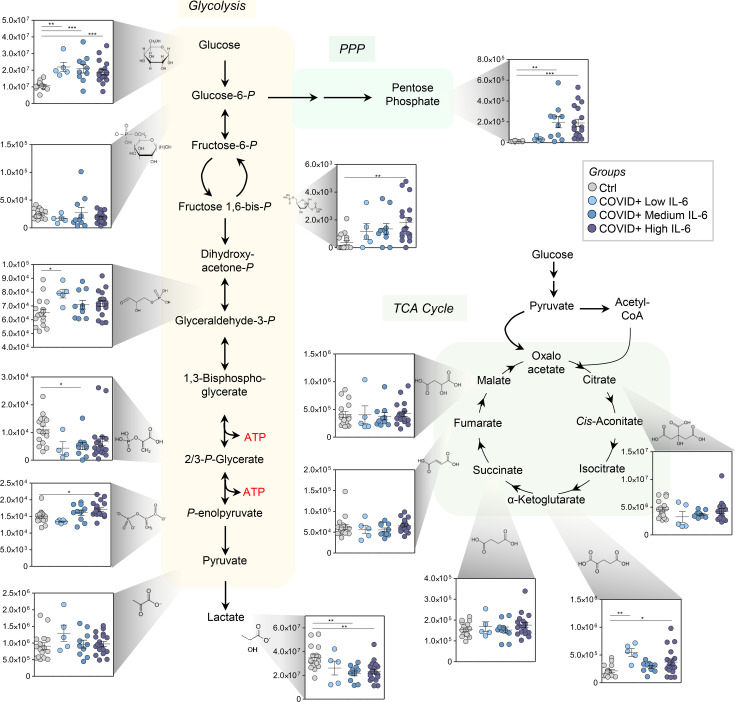
Because altered amino acid metabolism suggested dysregulated nitrogen metabolism, we determined whether this was also accompanied by significant alterations in carbon metabolism. Notably, all patients with COVID-19 in this cohort, independent of IL-6 levels, exhibited hyperglycemia (Figure 5 — also confirmed by clinical laboratory measurements — Supplemental Table 1). Some metabolic intermediates of the glycolysis and pentose phosphate pathways were increased in subjects with the highest IL-6 levels; this was suggestive of potential hemolysis (e.g., ribose phosphate; Figure 5), although no significant increases in lactate dehydrogenase (LDH) were noted across the 3 groups of patients with COVID-19 (Supplemental Figure 1A). However, unexpected decreases in lactate levels were noted in the same subjects, in the absence of differences in the levels of all carboxylic acids except α-ketoglutarate (Figure 5); this suggested altered transamination homeostasis consistent with an altered nitrogen balance.
Figure 5. Circulating levels of glucose and its catabolites in sera of COVID-19–positive patients.
Serum levels of glucose were significantly different when comparing COVID-19–positive patients and controls. Similarly, significant increases were seen in the levels of some intermediates of the glycolytic and pentose phosphate pathways in sera of COVID-19–positive patients. No significant changes were noted in serum levels of carboxylic acids across the groups. Asterisks indicate significance by ANOVA (1-way ANOVA with Tukey’s multiple comparisons, *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). The y axis in the dot plots indicates AU. PPP, pentose phosphate pathway.
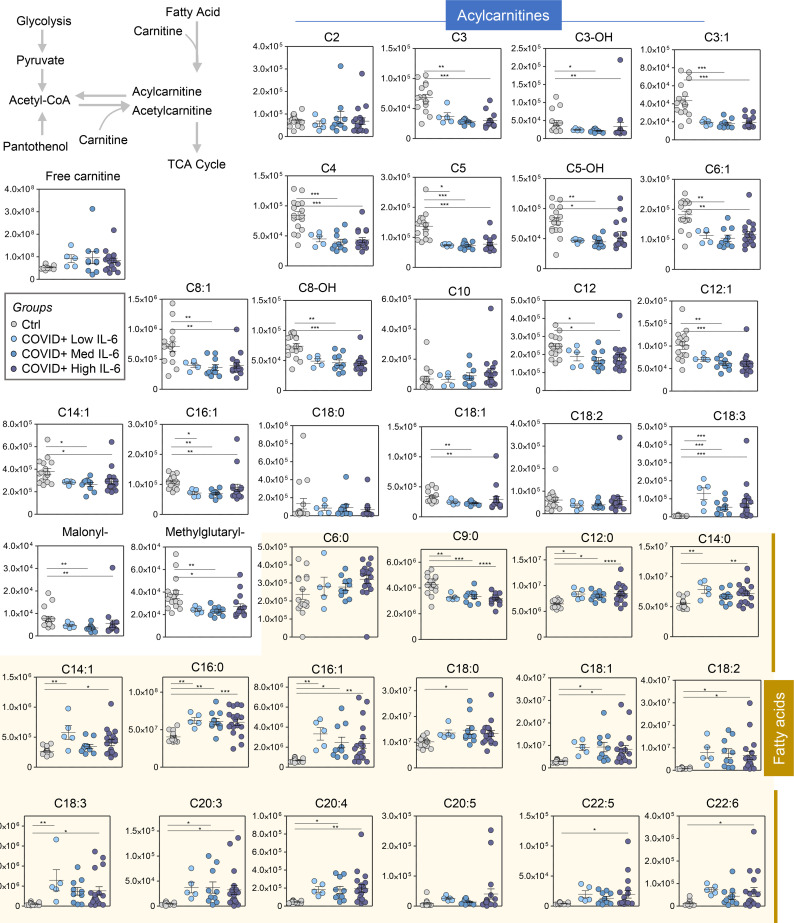
In addition, sera from patients with COVID-19 demonstrated significant changes in levels of acylcarnitines and free fatty acids (Figure 6). Specifically, all short- and medium-chain acylcarnitines, but not acyl-C18:3, were significantly decreased in all patients with COVID-19, independent of IL-6 levels. Finally, all fatty acids, except for nonanoic acid, were increased in all patients with COVID-19, independent of IL-6 levels (Figure 6).
Figure 6. Circulating levels of free fatty acids and acylcarnitines in sera of COVID-19–positive patients.
Serum levels of free fatty acids and acylcarnitines were significantly different when comparing COVID-19–positive patients and controls. Asterisks indicated significance by ANOVA (1-way ANOVA with Tukey’s multiple comparisons, *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). The y axis in the dot plots indicates AU.
Metabolic correlates of laboratory markers of inflammation and renal function.
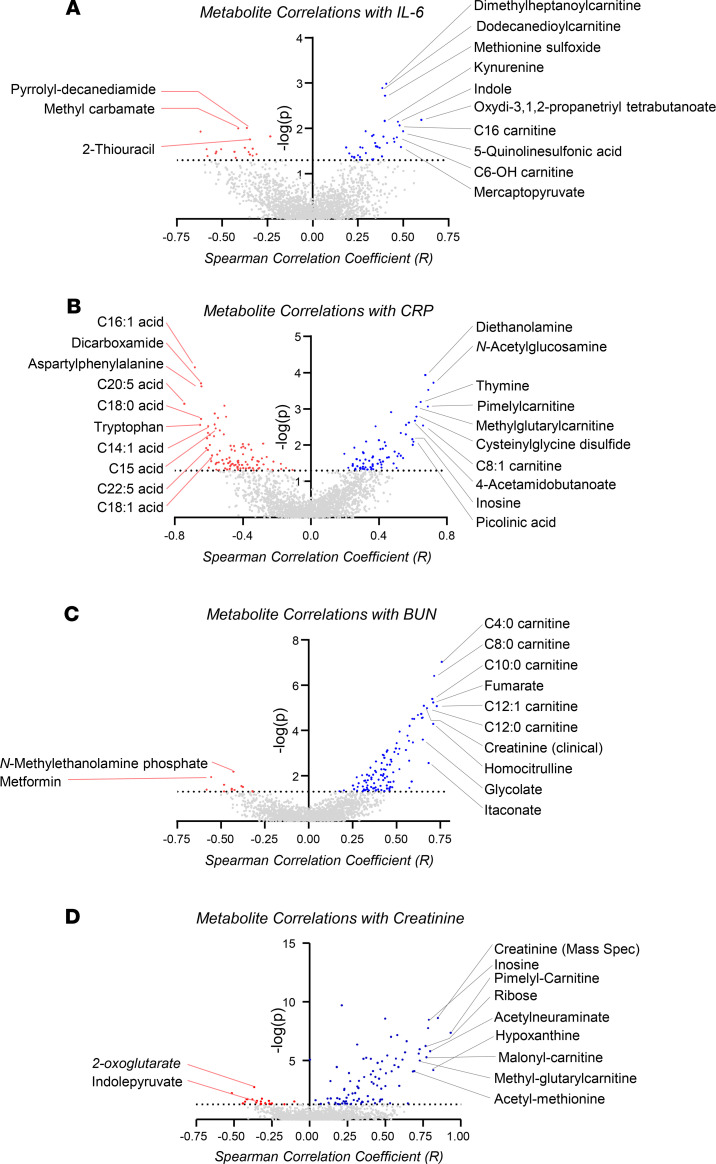
To determine the potential clinical relevance of these metabolic findings, metabolite levels were correlated to clinical laboratory markers of inflammation (i.e., IL-6 and C-reactive protein [CRP], Figure 7, A and B) and renal function (i.e., BUN and creatinine, Figure 7, C and D). Notably, several acylcarnitines, kynurenine, and methionine sulfoxide were among the top correlates to IL-6 (Figure 7A). Free fatty acid and tryptophan levels were among the top negative correlates to CRP levels, which were also directly proportional to levels of picolinic acid, inosine, and short-chain acylcarnitines (Figure 7B). Interestingly, acylcarnitines, but not free carnitine, ranked among the top positive correlates to BUN levels, along with creatinine (as expected), carboxylic acids (e.g., fumarate, itaconate), and oxidized purines (e.g., inosine; Figure 7C). As a supportive internal validation, creatinine, as measured by mass spectrometry, had a significant positive correlation (Spearman’s r = 0.93) with clinical laboratory measurements of creatinine (Figure 7D). In addition, purine deamination products (inosine and hypoxanthine) and several acylcarnitines ranked among the top correlates to creatinine (Figure 7D).
Figure 7. Metabolic correlates to IL-6, renal function (BUN), and CRP.
Metabolite levels were correlated (Spearman’s, x axis) to measurements of inflammatory markers IL-6 (A) and CRP (B) or renal function (BUN in C and creatinine in D). In each panel, the x axis indicates Spearman’s correlation coefficients, and the y axis indicates the significance of the correlation (–log10 of P values for each correlate).
Discussion
The present study provides what is likely the first observational metabolic characterization of sera from COVID-19–positive patients. The results show marked alterations in nitrogen metabolism (especially amino acid homeostasis, catabolism, and transamination) and carbon metabolism (especially affecting levels of glucose and free fatty acids). Metabolites in these pathways significantly correlated with circulating levels of inflammatory markers (i.e., IL-6 and CRP) and renal function (i.e., BUN and creatinine). Interestingly, the major effects of COVID-19 were on tryptophan metabolism and the kynurenine pathway. The rate-limiting step in this pathway is indole 2,3-dioxygenase (IDO1), a pleiotropic enzyme with complex effects, including immunoregulation, typically as a negative regulator of inflammation and immunization (31, 32). The kynurenine/tryptophan ratio is a general measure of IDO activity, although its meaning alters depending upon metabolic activity and its effects on kynurenine and tryptophan half-lives. Of particular relevance to our study, IDO helps limit lung inflammation in the context of IL-6, and IDO deletion severely exacerbates inflammatory lung pathology in mice (33). IDO regulates immune responses by depleting tryptophan and by generating tryptophan metabolites that activate the aryl hydrocarbon receptor; these metabolic alterations were observed in the current report. Moreover, IDO activity (inferred from metabolite levels) inversely correlated with IL-6 levels. Although causes and effects cannot be inferred by our results, it is reasonable to hypothesize that IDO activity is mechanistically involved in COVID-19 inflammation. Consistent with this, IDO is expressed by the lung mucosa, including antigen-presenting and epithelial cells (34).
IDO1 is downstream of interferon signaling (involving STAT6 and NF-κB) (31), which is activated by viral infection (35). Intriguingly, however, type I interferon production is suppressed in SARS-CoV-2 infection; in addition, interferon-γ production correlates with disease severity (36–39). In one predicted mechanism, interferon induces ACE2 receptor expression (40), which also binds SARS-CoV-2 spike protein S to mediate infection of host cells (11–13). Thus, interferon and its signaling partners can have complex and potentially opposing effects in SARS-CoV-2 pathology and the ensuing inflammation. Importantly, IDO activity is also regulated by oxidative stress, being enhanced by superoxide and NO. In summary, multiple factors may affect how IDO limits inflammation and affects adaptive immunity. Therefore, IDO activity may increase survival from COVID-19 by limiting pulmonary inflammation while simultaneously decreasing development of protective adaptive immunity to SARS-CoV-2.
Recently, we identified IDO pathway activation in individuals with trisomy 21 (Down syndrome) (31). Indeed, 4 of the 6 receptors for interferon-α and -γ are encoded by genes on chromosome 21. In addition, individuals with Down syndrome have respiratory comorbidities (e.g., pulmonary hypertension, chronic obstructive pulmonary disease), gastrointestinal disorders, diabetes, and accelerated aging (31), all risk factors for, or manifestations of, severe COVID-19 illness. In the Down syndrome population, therapies targeting IDO1 or its upstream pathways (i.e., Janus-activated kinase [JAK]), were proposed to ameliorate some of the accompanying comorbidities (41). Thus, the current findings suggest the possible relevance of JAK inhibitors in COVID-19 (42). Epidemiological studies of COVID-19 in the Down syndrome population could also provide clues regarding interferon signaling in SARS-CoV-2 infection.
Nonetheless, blunted interferon type I and III responses were reported in COVID-19 (43), which could, in part, be explained by SARS-CoV-2 proteins ORF3B, ORF6, and nsp nuclease; these were implicated in antagonizing interferon and cleaving host mRNA to prevent ribosomal loading and causing host shutoff, respectively (44, 45). Similarly, impaired type I interferon activity and exacerbated inflammatory responses were also described in patients with severe COVID-19 (46), although progressive increases in disease severity correlated with transcript levels of JAK1, STAT1 and STAT2, interferon-α2, interferon-α receptors 1 and 2, and interferon regulatory factors 1, 4, 5, and 7. Thus, strategies were designed to supplement interferon-α/β to treat COVID-19 (47), which significantly reduce persistence of virus in the upper respiratory tract and reduce the duration of elevated blood levels of IL-6 and CRP. Although speculative, metabolites in the kynurenine pathway are critical immunomodulators, which contribute, along with arginine (one of the most affected pathways identified herein), to immunosuppressive activity of dendritic cells (48) and to CD8+ T cell suppression in breast cancer (49, 50). Therefore, activating this pathway may allow SARS-CoV-2 to evade immunity. Moreover, dysregulated tryptophan metabolism is seen in inflammation (51) and aging, resulting in decreased NAD synthesis in older animals (52) and humans, an observation suggesting nicotinamide riboside as a dietary supplement (53); this provides a potential metabolic explanation for the severity of COVID-19 in older subjects. It is worth noting that proinflammatory signaling favors proteolysis and amino acid catabolism (represented herein by increased acetyl-methionine and hydroxyproline and altered levels of free amino acids), which can be antagonized, in part, by antiinflammatory cytokines (e.g., IL-37) (54) or inflammasome inhibitors (55). These antiinflammatory cytokines show promise in regulating glycemia in aging mice (56), which is relevant to finding increased glycemia in our patients with COVID-19; this may also help explain why diabetes is a risk factor for severe COVID-19 illness (57) and outcomes (58). Interestingly, similar increases in circulating glucose levels are found in critically ill patients with diabetes (59–61). Similarly, in trauma, extreme lipolysis is seen minutes to hours after trauma/shock, producing increased circulating free fatty acids (59), which we also identified in patients with COVID-19 (e.g., long-chain free fatty acids), especially those with high IL-6 levels. Phospholipase A2 (PLA2), which cleaves fatty acids in the sn-2 position of phospholipids, is required for replication of other coronaviruses, such as Middle Eastern Respiratory Syndrome–CoV (MERS-CoV) and human coronavirus 229E (26). Elevated levels of long-chain polyunsaturated fatty acids (PUFAs), which are highly enriched in the sn-2 position of phospholipids, in the absence of elevated long-chain acylcarnitines, which could reflect impaired mitochondrial fatty acid oxidation, suggest that this pathway may be upregulated in COVID-19. Increased PLA2 activity is associated with increased production of bioactive lipids by metabolism of omega-6 PUFAs and lysophosphatidylcholine. Some resulting metabolites (e.g., eicosanoids, oxylipins) may help propagate infection and thromboinflammatory complications (62), by directly supporting viral capsid membrane synthesis (25–27), by targeting proinflammatory immune cells, or by activating platelets (63). Thus, inhibiting PLA2 activity or increasing omega-3 PUFA levels, which are metabolized to bioactive lipids with antiinflammatory activity, might reduce disease severity.
Inflammatory stimuli promote platelet hyperreactivity in older individuals (23). Notably, polyamine by-products of nitrogen metabolism (e.g., spermidine, acetyl-spermidine) were greatly increased in COVID-19 patient sera. Primary amines, such as tranexamic acid, prevent hyperfibrinolysis in actively bleeding patients by interacting with tissue plasminogen activator (64). One can speculate that inflammation-induced alterations in nitrogen metabolism may participate in dysregulated coagulation leading to thrombus formation in severe COVID-19. In contrast, other metabolites associated with hypercoagulability, such as homocysteine (65) (which increases in Down syndrome, ref. 66), were decreased in patients with COVID-19. The latter may be explained by increased oxidant stress in patients with COVID-19, suggested by increased serum levels of methionine sulfoxide and cystine, along with decreased antioxidants, such as cysteine and taurine (67) (but, interestingly, not reduced glutathione). Conversely, decreased serum acylcarnitine levels, which may have an anticoagulant function (68), are consistent with a potential hypercoagulable phenotype.
Interestingly, increased serum sphingosine 1-phosphate levels were observed in patients with COVID-19. Circulating levels of this metabolite are significantly influenced by red blood cell (RBC) sphingosine kinase 1 activity in response to hypoxia (69), whereas alterations to this pathway mediate responses to angiotensin II–induced stimulation in the hypoxic kidney in chronic kidney disease (70); the latter may be relevant in light of renal dysfunction in some patients with COVID-19 in our study. In contrast, one would have predicted significantly increased serum levels of lactate and carboxylic acid markers of hypoxia (e.g., succinate) in patients with COVID-19, similar to that seen in patients following ischemic (71) or hemorrhagic shock (72). Surprisingly, no significant increases in serum lactate or succinate levels were observed, which may be because our patients were either normoxic or receiving intense respiratory therapy at the time of blood draw. Although unrelated to IL-6, fumarate and itaconate positively correlated with BUN and inosine, suggesting potential crosstalk between deaminated purine salvage reactions and carboxylic acid metabolism in renal dysfunction in COVID-19, similar to acute kidney ischemia (73). In addition, hemolysis markers (e.g., metabolic intermediates of the glycolytic and pentose phosphate pathways) correlated with IL-6 levels, suggesting interactions between inflammation, disease severity (e.g., correlation between LDH and BUN; Supplemental Figure 1B), and, ultimately, the effect of therapeutic interventions and mechanical/oxidant stress on circulating RBCs. As such, future studies will assess COVID-19 effects on RBCs.
The present study has several limitations. First, analyses were performed on a small set of sera obtained as a by-product of routine clinical laboratory testing. Although immediately refrigerated and stored for less than 24 hours, technical bias may have been introduced owing to collection procedures. Protocols are being implemented to prospectively collect and bank fresh samples of serum and plasma, RBCs, and buffy coats. In addition, males were disproportionally represented (75% of patients with COVID-19). As such, no sex-specific analysis was performed, and future investigations on larger, prospectively enrolled cohorts are underway to address this issue. Similarly, the mean age of COVID-19–positive patients was 56, whereas the control population was generally younger (mean: 33 years old). Nonetheless, although aging is associated with increased systemic inflammation, comparisons to prior studies on the effect of aging on the plasma/whole-blood metabolome in humans (74, 75) and animal models (52, 54, 56) does not suggest that the observations reported here are due to aging alone. In addition, the patients with COVID-19 in this study had significant disease, by definition, because they were all inpatients; future studies will investigate patients with milder disease and asymptomatic infected patients. Conversely, the control group did not include patients requiring hospitalization for respiratory infections distinct from SARS-CoV-2. As such, some of the biosignatures reported herein (e.g., fatty acids, refs. 25, 26) may be explained by the effects of responses to viral infection, in general, rather than being specifically associated with SARS-CoV-2. In addition, all patients with COVID-19 in this study exhibited some degree of renal dysfunction, which may affect serum metabolism by compromising metabolite filtration capacity. Nonetheless, it is worth noting that the present study did not identify an effect of the inflammatory state (e.g., IL-6 levels) on the characteristic increases in purine breakdown and deamination/oxidation products seen in the context of chronic kidney disease (70) or acute kidney ischemia (73, 76). However, accumulation of metabolites in this pathway did correlate with BUN and creatinine, consistent with a role of renal dysfunction in regulating circulating levels of oxidized purines. In addition, the patients in this study with more severe disease were most likely simultaneously receiving multiple therapeutic interventions, which may have confounded some of the findings in this group. Finally, it will be important to study serial samples from patients throughout their clinical course to evaluate the serum metabolome as a function of clinical status (e.g., stage of infection, on or off a ventilator, receiving hemodialysis or not) and in response to various therapies (e.g., treatment with IL-6 receptor inhibitors).
In conclusion, we provide the first observational report of the comprehensive serum metabolome in patients with COVID-19 as a function of IL-6 level, the latter as a proxy for disease severity and as a promising therapeutic target. These results suggest potential therapeutic targets in systems metabolism, including (a) IDO1 or its upstream modulators (e.g., JAK, STAT, and/or interferon signaling); (b) amino acid catabolism as a function of oxidant stress (e.g., taurine) or inflammation-induced proteolysis (through dietary supplementation with taurine/N-acetylcysteine, using antibodies against proinflammatory cytokines or antagonists to their receptors, such as, anakinra, or using antiinflammatory cytokines or inflammasome inhibitors) (54–56); and (c) free fatty acid levels and unsaturation, which are amenable to dietary or pharmacological intervention (e.g., fish oil in the diet or fatty acid desaturase inhibitors).
Methods
Blood collection and processing.
Subjects seen at NewYork-Presbyterian/Columbia University Irving Medical Center included 33 COVID-19–positive patients, as determined by SARS-CoV-2 nucleic acid testing of nasopharyngeal swabs; in this group, the severity of the disease was inferred from serum IL-6 levels, which were determined by a CLIA-certified ELISA-based assay. The control group included 16 subjects, all of whom were SARS-CoV-2 negative by nasopharyngeal swab at the time of the blood draw. Some patients in this group were “never positive” subjects, and some were COVID-19 convalescent patients who were previously positive but currently negative, as determined by testing nasopharyngeal swabs, and at least 14 days postresolution of symptoms. Serum was obtained from freshly drawn blood after an overnight hold at 4°C and all samples were then deidentified. Sera were extracted via a modified Folch method (chloroform/methanol/water 8:4:3), which completely inactivates other coronaviruses, such as MERS-CoV (77). Briefly, 20 μL of serum was diluted in 130 μL of LC-MS–grade water, 600 μL of ice-cold chloroform/methanol (2:1) was added, and the samples were vortexed for 10 seconds. Samples were then incubated at 4°C for 5 minutes, quickly vortexed (5 seconds), and centrifuged at 14,000 g for 10 minutes at 4°C. The top (i.e., aqueous) phase was transferred to a new tube for metabolomics analysis.
UHPLC-MS metabolomics.
Metabolomics analyses were performed using a Vanquish UHPLC coupled online to a Q Exactive mass spectrometer (Thermo Fisher Scientific, Bremen, Germany). Samples were analyzed using 5-, 15-, and 17-minute gradients, as described (78, 79). For targeted quantitative experiments, extraction solutions were supplemented with stable isotope–labeled standards, and endogenous metabolite concentrations were quantified against the areas calculated for heavy isotopologs for each internal standard (78, 79). Data were analyzed using Maven (Princeton University, Princeton, New Jersey, USA) and Compound Discoverer 2.1 (Thermo Fisher Scientific).
Statistics.
Graphs and statistical analyses were prepared with GraphPad Prism 8.0 (GraphPad Software, Inc, La Jolla, California, USA), GENE E (Broad Institute, Cambridge, Massachusetts, USA), and MetaboAnalyst 4.0 (80). Spearman’s correlations and related P values were calculated with RStudio (Boston, Massachusetts, USA). One-way ANOVA with Tukey’s multiple comparisons follow-up test was used for comparing metabolite concentrations across different groups. P < 0.05 was considered statistically significant. Data are shown as mean ± SD unless indicated.
Study approval.
This observational study was conducted according to the Declaration of Helsinki, in accordance with good clinical practice guidelines, and approved by the Columbia University Institutional Review Board. Residual samples were obtained following the completion of routine clinical laboratory testing for each subject and deidentified before evaluation for research purposes.
Additional approval was obtained from the University of Colorado – Anschutz Medical Campus Institutional Review Board as part of the COVID Omics project (protocol 1300v3).
Author contributions
TT, ROF, SLS, and EAH designed the study. TT, ROF, and EAH collected and processed the samples. DS, LB, JAR, TN, and ADA performed metabolomics analyses and prepared the figures. JAR, TN, and ADA performed data analysis and prepared figures and tables. ADA wrote the first draft of the manuscript, which was significantly revised by SLS, TT, JCZ, and KEH and finally approved by DS, LB, JAR, TN, TT, JCZ, KEH, ROF, EAH, KCH, ADA, and SLS.
Supplementary Material
Acknowledgments
This research was supported by funds from the Boettcher Foundation Webb-Waring Biomedical Research Award (to ADA); RM1GM131968 (to ADA, KCH) from the National Institute of General and Medical Sciences, NIH; and R01HL146442 (to ADA), R01HL149714 (to ADA), R01HL148151 (to ADA, JCZ, SLS), R21HL150032 (to ADA), and T32HL007171 (to TN) from the National Heart, Lung, and Blood Institute, NIH.
Version 1. 06/19/2020
In-Press Preview
Version 2. 07/23/2020
Electronic publication
Funding Statement
To Angelo D’Alessandro
To Angelo D’Alessandro
To Angelo D’Alessandro
To Angelo D’Alessandro, Steven L. Spitalnik, James C. Zimring
To Angelo D’Alessandro
To Travis Nemkove
To Angelo D’Alessandro and Kirk Hansen
Footnotes
Conflict of interest: ADA, KCH, and TN are founders of Omix Technologies Inc and Altis Biosciences LLC. AD and SLS are consultants for Hemanext Inc. SLS is also a consultant for Tioma Therapeutics Inc. JCZ is a consultant for Rubius Therapeutics.
Copyright: © 2020, American Society for Clinical Investigation.
Reference information: JCI Insight. 2020;5(14):e140327.https://doi.org/10.1172/jci.insight.140327.
Contributor Information
Tiffany Thomas, Email: tt2254@cumc.columbia.edu.
Davide Stefanoni, Email: DAVIDE.STEFANONI@CUANSCHUTZ.EDU.
Julie A. Reisz, Email: JULIE.HAINES@CUANSCHUTZ.EDU.
Travis Nemkov, Email: TRAVIS.NEMKOV@UCDENVER.EDU.
Lorenzo Bertolone, Email: lorenzo.bertolone@univr.it.
Richard O. Francis, Email: rof3@cumc.columbia.edu.
Krystalyn E. Hudson, Email: keh2197@cumc.columbia.edu.
James C. Zimring, Email: jcz2k@virginia.edu.
Kirk C. Hansen, Email: Kirk.Hansen@UCDenver.edu.
Eldad A. Hod, Email: eh2217@cumc.columbia.edu.
Steven L. Spitalnik, Email: ss2479@cumc.columbia.edu.
Angelo D’Alessandro, Email: ANGELO.DALESSANDRO@UCDENVER.EDU.
References
- 1.Wu F, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO. Coronavirus disease 2019 (COVID-19) situation report – 162. https://www.who.int/docs/default-source/coronaviruse/20200630-covid-19-sitrep-162.pdf?sfvrsn=e00a5466_2 Updated June 30, 2020. Accessed June 30, 2020.
- 3.Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580(7805):576–577. doi: 10.1038/d41586-020-01221-y. [DOI] [PubMed] [Google Scholar]
- 4.London AJ, Kimmelman J. Against pandemic research exceptionalism. Science. 2020;368(6490):476–477. doi: 10.1126/science.abc1731. [DOI] [PubMed] [Google Scholar]
- 5. Woodward A, Gal S. One chart shows how many coronavirus tests per capita have been completed in 6 countries. The US has finally caught up. Business Insider. https://www.businessinsider.com/coronavirus-testing-per-capita-us-italy-south-korea-2020-4 Published April 20, 2020. Accessed June 25, 2020.
- 6. doi: 10.1101/2020.04.14.20062463. Bendavid E, et al. COVID-19 antibody seroprevalence in Santa Clara County, California. Posted on medRxiv April 30, 2020. [DOI]
- 7. Vogel G. ‘These are answers we need.’ WHO plans global study to discover true extent of coronavirus infections. Science. https://www.sciencemag.org/news/2020/04/these-are-answers-we-need-who-plans-global-study-discover-true-extent-coronavirus Published April 2, 2020. Accessed June 25, 2020.
- 8.Bloch EM, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest. 2020;130(6):2757–2765. doi: 10.1172/JCI138745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. doi: 10.1038/s41586-020-2286-9. Gordon DE, et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing [published online April 30, 2020]. Nature . [DOI] [PMC free article] [PubMed]
- 10.Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lan J, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581(7807):215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 12.Lei C, et al. Neutralization of SARS-CoV-2 spike pseudotyped virus by recombinant ACE2-Ig. Nat Commun. 2020;11(1):2070. doi: 10.1038/s41467-020-16048-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shang J, et al. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020;581(7807):221–224. doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanmugaraj B, Siriwattananon K, Wangkanont K, Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19) Asian Pac J Allergy Immunol. 2020;38(1):10–18. doi: 10.12932/AP-200220-0773. [DOI] [PubMed] [Google Scholar]
- 15. doi: 10.1016/j.ijantimicag.2020.105949. Gautret P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial [published online March 20, 2020]. Int J Antimicrob Agents . [DOI] [PMC free article] [PubMed]
- 16. doi: 10.1016/j.medj.2020.06.001. Magagnoli J, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19 [published online June 5, 2020]. Med . [DOI] [PMC free article] [PubMed]
- 17.Lim HW, Feldman SR, Van Voorhees AS, Gelfand JM. Recommendations for phototherapy during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(1):287–288. doi: 10.1016/j.jaad.2020.04.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan EL, et al. Inhibition of SARS coronavirus infection in vitro with clinically approved antiviral drugs. Emerging Infect Dis. 2004;10(4):581–586. doi: 10.3201/eid1004.030458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu B, Li M, Zhou Z, Guan X, Xiang Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J Autoimmun. 2020;111:102452. doi: 10.1016/j.jaut.2020.102452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang X, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scialpi M, Scialpi S, Piscioli I, Battista Scalera G, Longo F. Pulmonary thromboembolism in critical ill patients with COVID-19. Int J Infect Dis. 2020;95:361–362. doi: 10.1016/j.ijid.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. doi: 10.1111/jth.14828. Wang J, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series [published online April 8, 2020]. J Thromb Haemost . [DOI] [PMC free article] [PubMed]
- 23.Davizon-Castillo P, et al. TNF-α-driven inflammation and mitochondrial dysfunction define the platelet hyperreactivity of aging. Blood. 2019;134(9):727–740. doi: 10.1182/blood.2019000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pabinger I, Fries D, Schöchl H, Streif W, Toller W. Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis. Wien Klin Wochenschr. 2017;129(9-10):303–316. doi: 10.1007/s00508-017-1194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greseth MD, Traktman P. De novo fatty acid biosynthesis contributes significantly to establishment of a bioenergetically favorable environment for vaccinia virus infection. PLoS Pathog. 2014;10(3):e1004021. doi: 10.1371/journal.ppat.1004021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Müller C, Hardt M, Schwudke D, Neuman BW, Pleschka S, Ziebuhr J. Inhibition of cytosolic phospholipase A2α impairs an early step of coronavirus replication in cell culture. J Virol. 2018;92(4):e01463-17. doi: 10.1128/JVI.01463-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan B, et al. Characterization of the lipidomic profile of human coronavirus-infected cells: implications for lipid metabolism remodeling upon coronavirus replication. Viruses. 2019;11(1):E73. doi: 10.3390/v11010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wenham C, Smith J, Morgan R, Gender COVID-19 Working Group COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. doi: 10.3324/haematol.2019.229930. Stefanoni D, et al. Red blood cell metabolism in Rhesus macaques and humans: comparative biology of blood storage [published online November 7, 2019]. Haematologica . [DOI] [PMC free article] [PubMed]
- 30.Chong J, et al. MetaboAnalyst 4.0: towards more transparent and integrative metabolomics analysis. Nucleic Acids Res. 2018;46(W1):W486–W494. doi: 10.1093/nar/gky310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powers RK, et al. Trisomy 21 activates the kynurenine pathway via increased dosage of interferon receptors. Nat Commun. 2019;10(1):4766. doi: 10.1038/s41467-019-12739-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu H, Gong J, Liu Y. Indoleamine 2, 3-dioxygenase regulation of immune response (Review) Mol Med Rep. 2018;17(4):4867–4873. doi: 10.3892/mmr.2018.8537. [DOI] [PubMed] [Google Scholar]
- 33.Lee SM, et al. Inhibition of acute lethal pulmonary inflammation by the IDO-AhR pathway. Proc Natl Acad Sci U S A. 2017;114(29):E5881–E5890. doi: 10.1073/pnas.1615280114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aldajani WA, Salazar F, Sewell HF, Knox A, Ghaemmaghami AM. Expression and regulation of immune-modulatory enzyme indoleamine 2,3-dioxygenase (IDO) by human airway epithelial cells and its effect on T cell activation. Oncotarget. 2016;7(36):57606–57617. doi: 10.18632/oncotarget.11586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nguyen KB, et al. Critical role for STAT4 activation by type 1 interferons in the interferon-gamma response to viral infection. Science. 2002;297(5589):2063–2066. doi: 10.1126/science.1074900. [DOI] [PubMed] [Google Scholar]
- 36.Zheng HY, et al. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in patients with COVID-19. Cell Mol Immunol. 2020;17(5):541–543. doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. doi: 10.1101/2020.03.12.20034736. Shi Y, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China [preprint]. Posted on medRxiv March 16, 2020. [DOI] [PMC free article] [PubMed]
- 38.Pedersen SF, Ho YC. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;130(5):2202–2205. doi: 10.1172/JCI137647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ziegler CGK, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rachubinski AL, Estrada BE, Norris D, Dunnick CA, Boldrick JC, Espinosa JM. Janus kinase inhibition in Down syndrome: 2 cases of therapeutic benefit for alopecia areata. JAAD Case Rep. 2019;5(4):365–367. doi: 10.1016/j.jdcr.2019.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Napolitano M, Fabbrocini G, Patruno C. Reply: Potential role of Janus kinase inhibitors in COVID-19. J Am Acad Dermatol. 2020;83(1):e65. doi: 10.1016/j.jaad.2020.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blanco-Melo D, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181(5):1036–1045.e9. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frieman M, Baric R. Mechanisms of severe acute respiratory syndrome pathogenesis and innate immunomodulation. Microbiol Mol Biol Rev. 2008;72(4):672–685. doi: 10.1128/MMBR.00015-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kopecky-Bromberg SA, Martínez-Sobrido L, Frieman M, Baric RA, Palese P. Severe acute respiratory syndrome coronavirus open reading frame (ORF) 3b, ORF 6, and nucleocapsid proteins function as interferon antagonists. J Virol. 2007;81(2):548–557. doi: 10.1128/JVI.01782-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. doi: 10.1101/2020.04.19.20068015. Hadjadj J, et al. Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid-19 patients [preprint]. Posted on medRxiv April 23, 2020. [DOI] [PMC free article] [PubMed]
- 47. doi: 10.1101/2020.04.06.20042580. Zhou Q, et al. Interferon-a2b treatment for COVID-19 [preprint]. Posted on medRxiv April 10, 2020. [DOI]
- 48.Mondanelli G, et al. A relay pathway between arginine and tryptophan metabolism confers immunosuppressive properties on dendritic cells. Immunity. 2017;46(2):233–244. doi: 10.1016/j.immuni.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.D’Amato NC, et al. A TDO2-AhR signaling axis facilitates anoikis resistance and metastasis in triple-negative breast cancer. Cancer Res. 2015;75(21):4651–4664. doi: 10.1158/0008-5472.CAN-15-2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Greene LI, et al. A role for tryptophan-2,3-dioxygenase in CD8 T-cell suppression and evidence of tryptophan catabolism in breast cancer patient plasma. Mol Cancer Res. 2019;17(1):131–139. doi: 10.1158/1541-7786.MCR-18-0362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baumgartner R, Forteza MJ, Ketelhuth DFJ. The interplay between cytokines and the Kynurenine pathway in inflammation and atherosclerosis. Cytokine. 2019;122:154148. doi: 10.1016/j.cyto.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 52.Morrison EJ, et al. Parabiosis incompletely reverses aging-induced metabolic changes and oxidant stress in mouse red blood cells. Nutrients. 2019;11(6):E1337. doi: 10.3390/nu11061337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson S, Imai SI. NAD + biosynthesis, aging, and disease. F1000Res. 2018;7:132. doi: 10.12688/f1000research.12120.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cavalli G, et al. Interleukin 37 reverses the metabolic cost of inflammation, increases oxidative respiration, and improves exercise tolerance. Proc Natl Acad Sci U S A. 2017;114(9):2313–2318. doi: 10.1073/pnas.1619011114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marchetti C, et al. OLT1177, a β-sulfonyl nitrile compound, safe in humans, inhibits the NLRP3 inflammasome and reverses the metabolic cost of inflammation. Proc Natl Acad Sci U S A. 2018;115(7):E1530–E1539. doi: 10.1073/pnas.1716095115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ballak DB, et al. Short-term interleukin-37 treatment improves vascular endothelial function, endurance exercise capacity, and whole-body glucose metabolism in old mice. Aging Cell. 2020;19(1):e13074. doi: 10.1111/acel.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. doi: 10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu L, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31(6):1068–1077.e3. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peltz ED, et al. Pathologic metabolism: an exploratory study of the plasma metabolome of critical injury. J Trauma Acute Care Surg. 2015;78(4):742–751. doi: 10.1097/TA.0000000000000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.D’Alessandro A, et al. Trauma/hemorrhagic shock instigates aberrant metabolic flux through glycolytic pathways, as revealed by preliminary (13)C-glucose labeling metabolomics. J Transl Med. 2015;13:253. doi: 10.1186/s12967-015-0612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.D’Alessandro A, et al. Early hemorrhage triggers metabolic responses that build up during prolonged shock. Am J Physiol Regul Integr Comp Physiol. 2015;308(12):R1034–R1044. doi: 10.1152/ajpregu.00030.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dennis EA, Norris PC. Eicosanoid storm in infection and inflammation. Nat Rev Immunol. 2015;15(8):511–523. doi: 10.1038/nri3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yeung J, Hawley M, Holinstat M. The expansive role of oxylipins on platelet biology. J Mol Med. 2017;95(6):575–588. doi: 10.1007/s00109-017-1542-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Urano T, Castellino FJ, Suzuki Y. Regulation of plasminogen activation on cell surfaces and fibrin. J Thromb Haemost. 2018;16(8):1487–1497. doi: 10.1111/jth.14157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coppola A, Davi G, De Stefano V, Mancini FP, Cerbone AM, Di Minno G. Homocysteine, coagulation, platelet function, and thrombosis. Semin Thromb Hemost. 2000;26(3):243–254. doi: 10.1055/s-2000-8469. [DOI] [PubMed] [Google Scholar]
- 66.Culp-Hill R, et al. Red blood cell metabolism in Down syndrome: hints on metabolic derangements in aging. Blood Adv. 2017;1(27):2776–2780. doi: 10.1182/bloodadvances.2017011957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.et al. Impact of taurine on red blood cell metabolism and implications for blood storage. Transfusion. 2020;60(6):1212–1226. doi: 10.1111/trf.15810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Deguchi H, et al. Acylcarnitines are anticoagulants that inhibit factor Xa and are reduced in venous thrombosis, based on metabolomics data. Blood. 2015;126(13):1595–1600. doi: 10.1182/blood-2015-03-636761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sun K, et al. Sphingosine-1-phosphate promotes erythrocyte glycolysis and oxygen release for adaptation to high-altitude hypoxia. Nat Commun. 2016;7:12086. doi: 10.1038/ncomms12086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. doi: 10.1161/CIRCRESAHA.119.316298. Xie T, et al. Erythrocyte metabolic reprogramming by sphingosine 1-phosphate in chronic kidney disease and therapies [published online April 14, 2020]. Circ Res . [DOI] [PubMed]
- 71.Chouchani ET, et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature. 2014;515(7527):431–435. doi: 10.1038/nature13909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.D’Alessandro A, et al. Plasma succinate is a predictor of mortality in critically injured patients. J Trauma Acute Care Surg. 2017;83(3):491–495. doi: 10.1097/TA.0000000000001565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fox BM, et al. Metabolomics assessment reveals oxidative stress and altered energy production in the heart after ischemic acute kidney injury in mice. Kidney Int. 2019;95(3):590–610. doi: 10.1016/j.kint.2018.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Johnson LC, et al. The plasma metabolome as a predictor of biological aging in humans. Geroscience. 2019;41(6):895–906. doi: 10.1007/s11357-019-00123-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chaleckis R, Murakami I, Takada J, Kondoh H, Yanagida M. Individual variability in human blood metabolites identifies age-related differences. Proc Natl Acad Sci U S A. 2016;113(16):4252–4259. doi: 10.1073/pnas.1603023113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Clendenen N, et al. Selective organ ischaemia/reperfusion identifies liver as the key driver of the post-injury plasma metabolome derangements. Blood Transfus. 2019;17(5):347–356. doi: 10.2450/2018.0188-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Burnum-Johnson KE, et al. MPLEx: a method for simultaneous pathogen inactivation and extraction of samples for multi-omics profiling. Analyst. 2017;142(3):442–448. doi: 10.1039/C6AN02486F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nemkov T, Reisz JA, Gehrke S, Hansen KC, D’Alessandro A. High-throughput metabolomics: isocratic and gradient mass spectrometry-based methods. Methods Mol Biol. 2019;1978:13–26. doi: 10.1007/978-1-4939-9236-2_2. [DOI] [PubMed] [Google Scholar]
- 79.Reisz JA, Zheng C, D’Alessandro A, Nemkov T. Untargeted and semi-targeted lipid analysis of biological samples using mass spectrometry-based metabolomics. Methods Mol Biol. 2019;1978:121–135. doi: 10.1007/978-1-4939-9236-2_8. [DOI] [PubMed] [Google Scholar]
- 80.Chong J, Wishart DS, Xia J. Using MetaboAnalyst 4.0 for comprehensive and integrative metabolomics data analysis. Curr Protoc Bioinformatics. 2019;68(1):e86. doi: 10.1002/cpbi.86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.