Abstract
A strategy of complete revascularization (CR) versus infarct-related artery revascularization (IRA) in patients with ST-elevation myocardial infarction (STEMI) continues to be a subject of debate. We performed an updated meta-analysis to compare the 2 strategies. Outcomes of interest included major adverse cardiovascular events (MACE), cardiovascular mortality, all-cause mortality, stroke, repeat revascularization, myocardial infarction, and contrast-induced nephropathy. Ten randomized trials including 7,423 patients (CR = 3,574 and IRA = 3,849), with a follow-up of 2.0 ± 0.8 years were included. There was a significant reduction in MACE with CR versus IRA (10.7% vs 18.6%, relative risk [RR] 0.64, 95% confidence interval [CI] 0.51 to 0.81, p = 0.002, I2 = 66%), with higher risk reduction with immediate versus stages revascularization (RR 0.40, 95% CI 0.32 to 0.5 vs RR 0.69, 95% CI 0.54 to 0.89, P-interaction = 0.002). Complete revascularization was associated with lower rates of repeat revascularization (4.0% vs 11.7%, RR 0.44, 95% CI 0.28 to 0.70, p <0.0001, I2 = 81%), and a nonsignificant trend toward lower cardiovascular mortality (2.8% vs 3.7%, RR 0.78, 95% CI 0.60 to 1.03, p = 0.08, I2 = 0%). However, there was no difference between the 2 strategies in all-cause mortality (4.6% vs 4.8%, RR 0.90, 95% CI 0.73 to 1.12, p = 0.36, I2 = 0%), myocardial infarction (5.2% vs 6.5%, RR 0.73, 95% CI, 0.58 to 1.08, p = 0.08, I2 = 30%), stroke (1.5% vs 1.2%, RR 1.14, 95% CI 0.56 to 2.29, p = 0.33, I2 = 14%), or contrast-induced nephropathy (1.6% vs 1.2%, RR 1.35, 95% CI 0.85 to 2.15, p = 0.78, I2 = 0%). In conclusion, CR in patients with STEMI is associated with significant reduction in MACE compared with IRA. This reduction is derived mainly by the low rates of repeat revascularization in the CR group. © 2019 Elsevier Inc. All rights reserved.
More than 60% of patients who underwent primary percutaneous coronary intervention (PCI) for an ST-elevation myocardial infarction (STEMI) have multivessel coronary artery disease.1,2 American College of Cardiology (ACC)—American Heart Association (AHA) guidelines yield a gray area updating from a Class III: Harm recommendation against complete revascularization (CR) to a Class IIb recommendation.3 Multiple randomized controlled trials (RCTs) showed complete revascularization either immediate, at the time of primary PCI, or as a planned, staged procedure reduces risk of major adverse cardiac events (MACE).4−8 The objective of the present study was to assemble and analyze the most recent RCTs with adequate sample size and follow-up with an emphasis on hard clinical outcomes.
Methods
We conducted a literature search of PubMed, Embase, and Cochrane library from inception through September 10, 2019. We used the following terms for the database search: “coronary angioplasty” or “coronary intervention” or “completer revascularization” or “staged revascularization” and “myocardial infarction” or “St-segment elevation myocardial infarction” and “multivessel” (or “multivessel”). We utilized the “related articles” function in PubMed to find relevant articles which were missed by the initial search. Our search and meta-analysis were conducted and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement. Titles and abstracts of studies retrieved by the initial search were screened by 2 authors (CN and BK). Consequently, the full texts of the potentially relevant articles were reviewed to determine if the study fulfill the inclusions criteria. Any discrepancies or disagreements were resolved by a third author (MO).
The priori inclusion criteria were: (1) RCTs comparing complete revascularization (CR) versus infarct related artery (IRA) revascularization in patients with ST-elevation myocardial infarction (STEMI) and multivessel disease (MVD), (2) sample size ≥100 patients and follow-up duration of at least 1 year, and (3) reporting on cardiovascular outcomes of interest. We selected particular sample size and follow-up duration to avoid small study effects, and since longer follow-up durations are most likely to generate clinical differences in hard outcomes.9−11 Single-arm trials or those not assessing IRA group were excluded.
We assessed the methodological quality of the studies and risk of bias independently by 2 authors (BK and SK) using the Cochrane Collaboration tool for assessing the quality of RCTs.
The primary outcome of interest was major adverse cardiovascular events (MACE). The secondary end points were cardiovascular mortality, myocardial infarction (MI), all-cause mortality, repeat revascularization, stroke, and contrast-induced nephropathy (CIN). The MACE was defined in (eTable 1).
Outcomes were pooled using Mantel-Hansel random effects model. DerSimonian and Laird method was used for estimation of t2.12 We preferred random effects model to account for potential statistical heterogeneity. Summary estimates were calculated as relative risk (RR) with 95% confidence intervals (CI). We performed a subgroup analysis by dividing the CR group into 2 subgroups, immediate revascularization group defined as: trials in which >50% CR was performed during index procedure and staged revascularization group defined as trials in which >50% CR performed 1 to 30 days after the index procedure. Subgroup differences were assessed by formal P-interaction testing. Heterogeneity was evaluated via Q statistics with I2 >75% being consistent with a high degree of heterogeneity.13 Sensitivity analysis was performed on primary outcomes by exclusion of one trial at a time. Publication bias assessment was done using funnel plots. We did not perform meta-regression analyses due to low number of studies.14 Statistical significance was set at 5%. All analyses were conducted using RevMan version 5.3 Windows (Cochrane Collaboration, Oxford, UK).
Results
The initial database search retrieved 1,528 articles. After excluding duplicates, a total of 1,313 were screened for eligibility by reading the title and abstract of the study. A total of 24 articles were then screened using the predetermined inclusions criteria to assess eligibility. Funnel plots for the outcomes were examined for asymmetry; corresponding Egger’s regression test did not show any significance publication bias (eFigure 1). Details of the study selection process are reported following the PRISMA-P guidelines (Figure 1). A total of 10 RCTs, with 7,423 patients (CR = 3,574 and IRA = 3,849), 21% female, mean follow-up 2.0 ± 0.8 years, mean age of 63 ± 1.8 years, were included in the current meta-analysis. Detailed baseline characteristics of the included studies and definition of the MACE are shown in (eTables 1 and 2).
Figure 1.
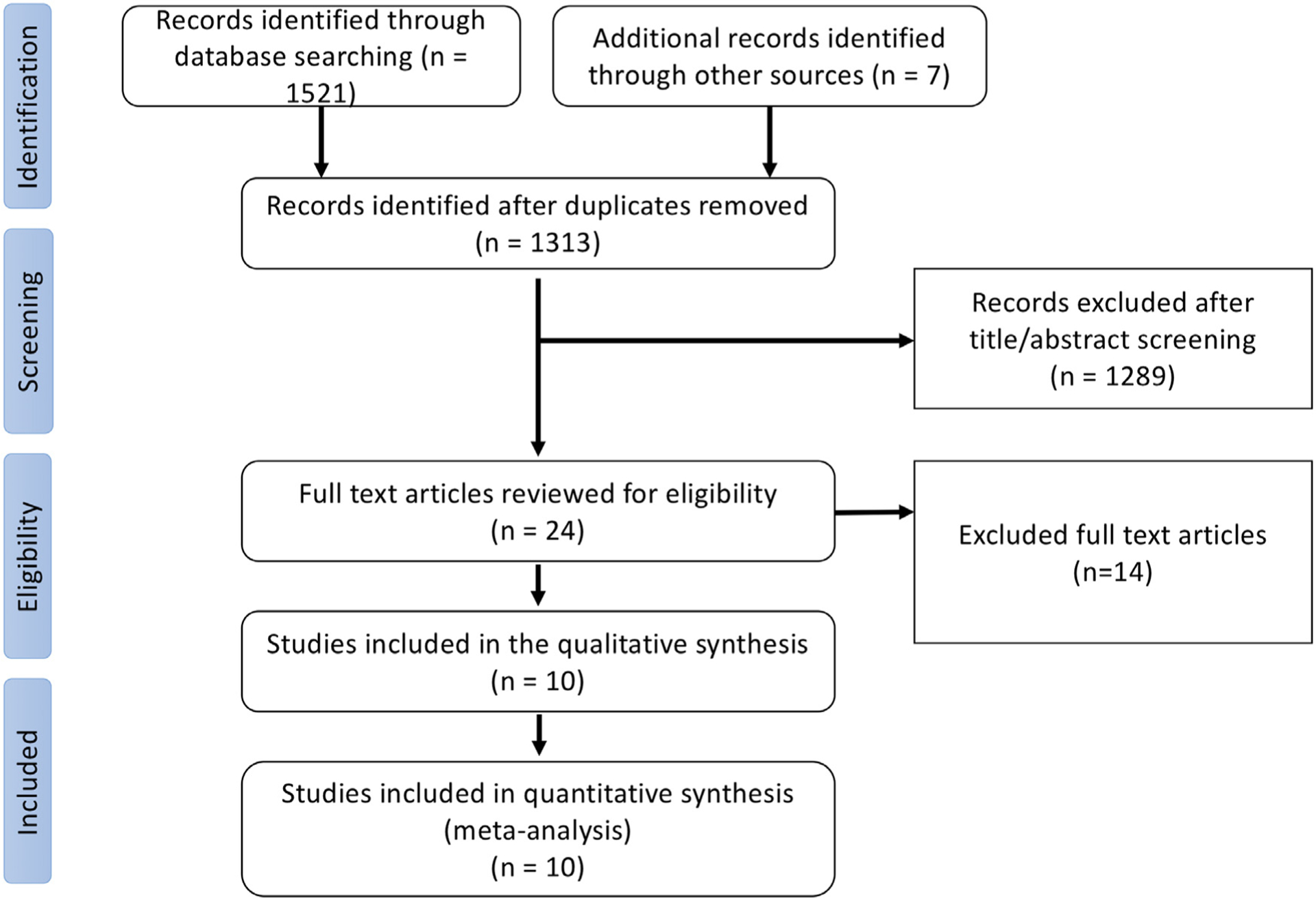
Flow chart for the systematic review and meta-analysis as per the Preferred Reporting System for Systematic Review and Meta-Analysis (PRISMA).
Complete revascularization reduced the risk of MACE compared with IRA (10.7% vs 18.6%, RR 0.64, 95% CI 0.51 to 0.81, p = 0.002, I2 = 66%) (Figure 2). This benefit varied by timing of CR with higher risk reduction in patients who received immediate revascularization (RR 0.40, 95% CI 0.32to 0.5) compared with those who underwent staged revascularization (RR 0.69, 95% CI 0.54 to 0.89; P-interaction = 0.002) (Figure 3). These results persisted throughout the process of the leave out sensitivity analysis.
Figure 2.
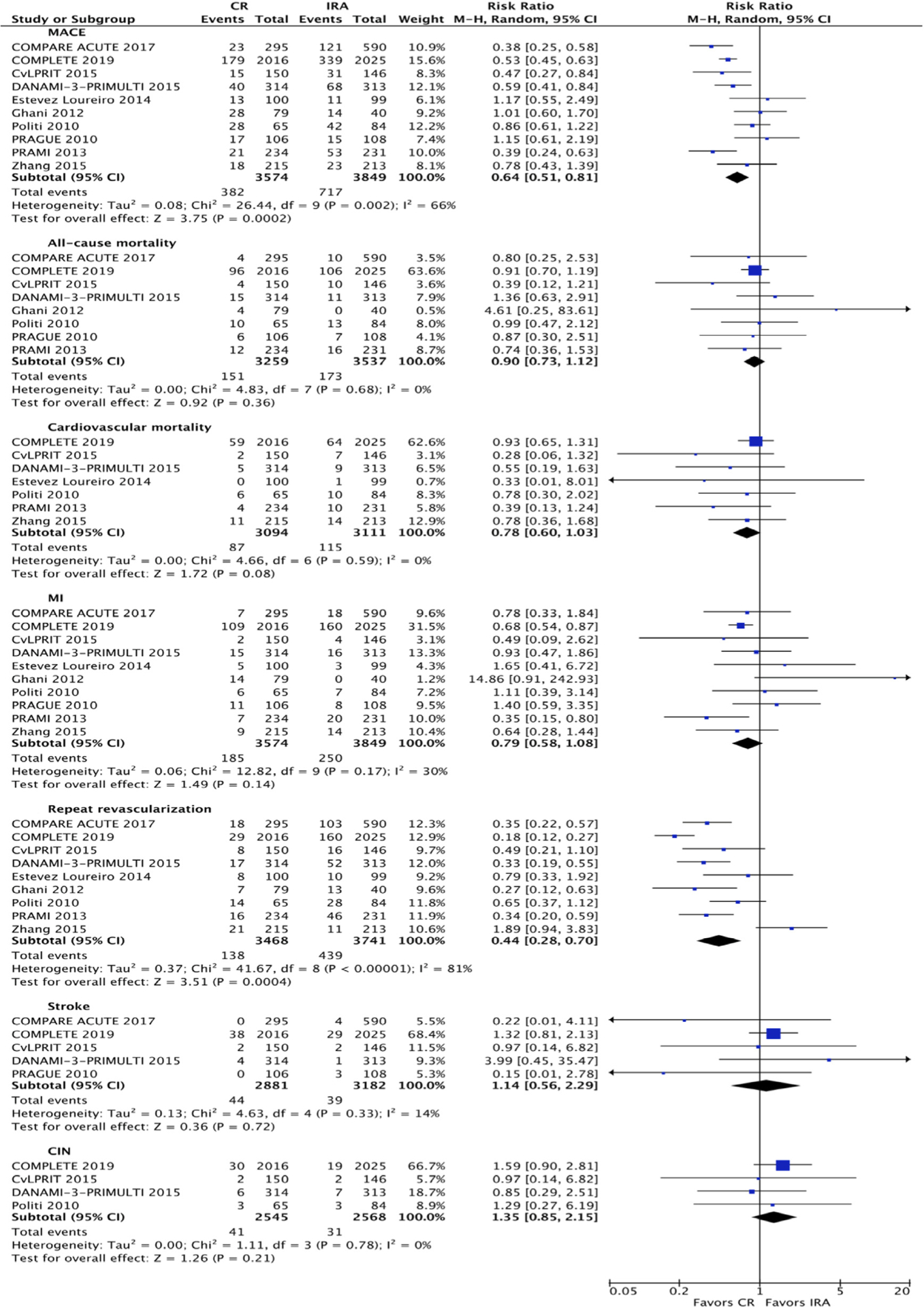
Forest plot comparing complete revascularization and infarct related artery only revascularization. CR = complete revascularization; IRA = infarct-related artery revascularization; CIN = contrast-induced nephropathy; MI = myocardial infarction; RR = risk ratio.
Figure 3.
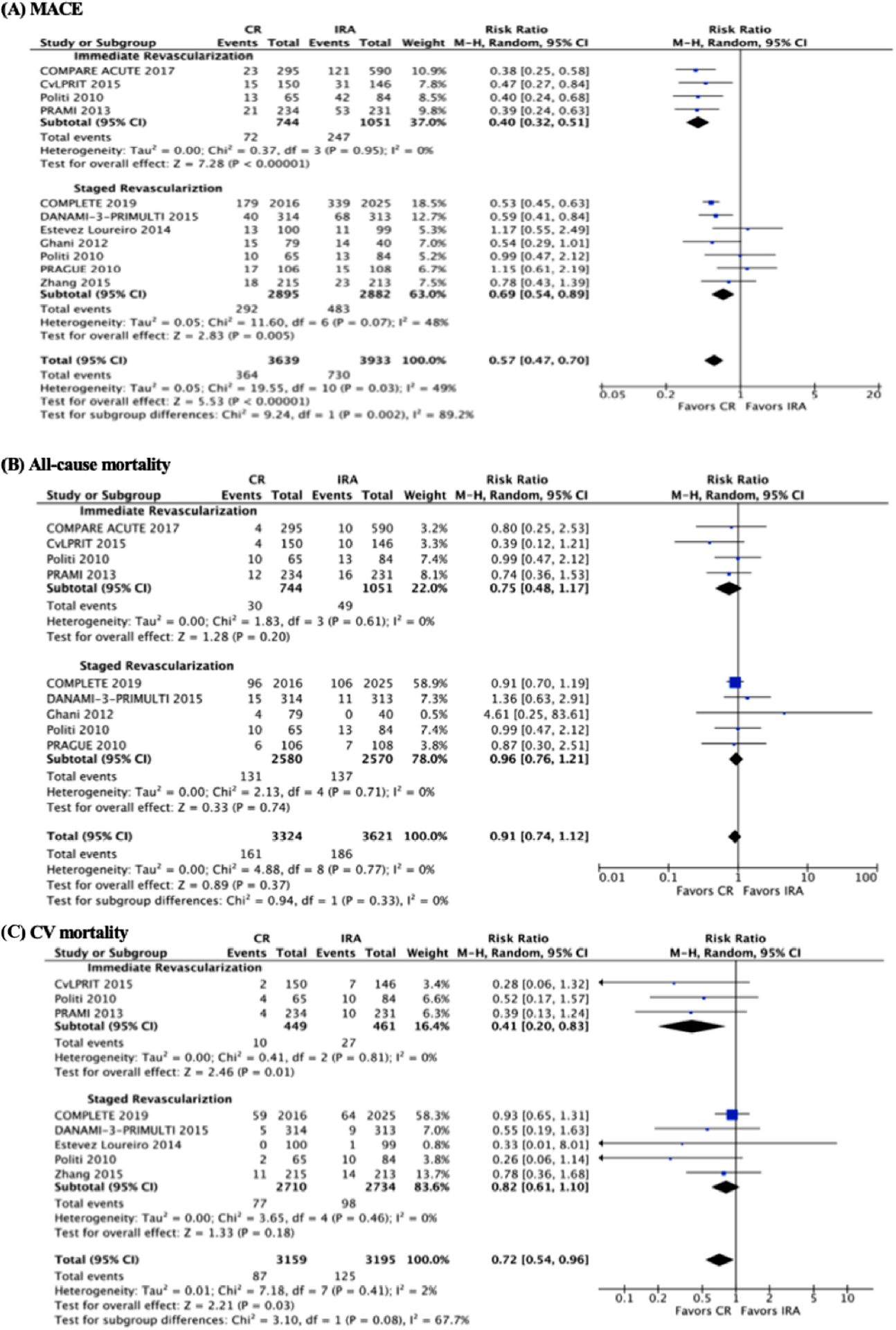
Forest plot comparing complete revascularization and infarct-related artery only revascularization with subgroup analysis based on the timing of revascularization. CR = complete revascularization; IRA = infarct-related artery revascularization; CIN = contrast-induced nephropathy; CV = cardiovascular; MI = myocardial infarction; RR = risk ratio.
Complete revascularization did not reduce the risk of all-cause mortality compared with IRA (4.6% vs 4.8%, RR 0.90, 95% CI 0.73 to 1.12, p = 0.36, I2 = 0%) (Figure 2). This persisted in the subgroup analysis as both immediate and staged revascularization groups did not show difference in all-cause mortality rates compared with the IRA group (p for interaction = 0.94) (Figure 3). These results persisted throughout the process of the leave out sensitivity analysis.
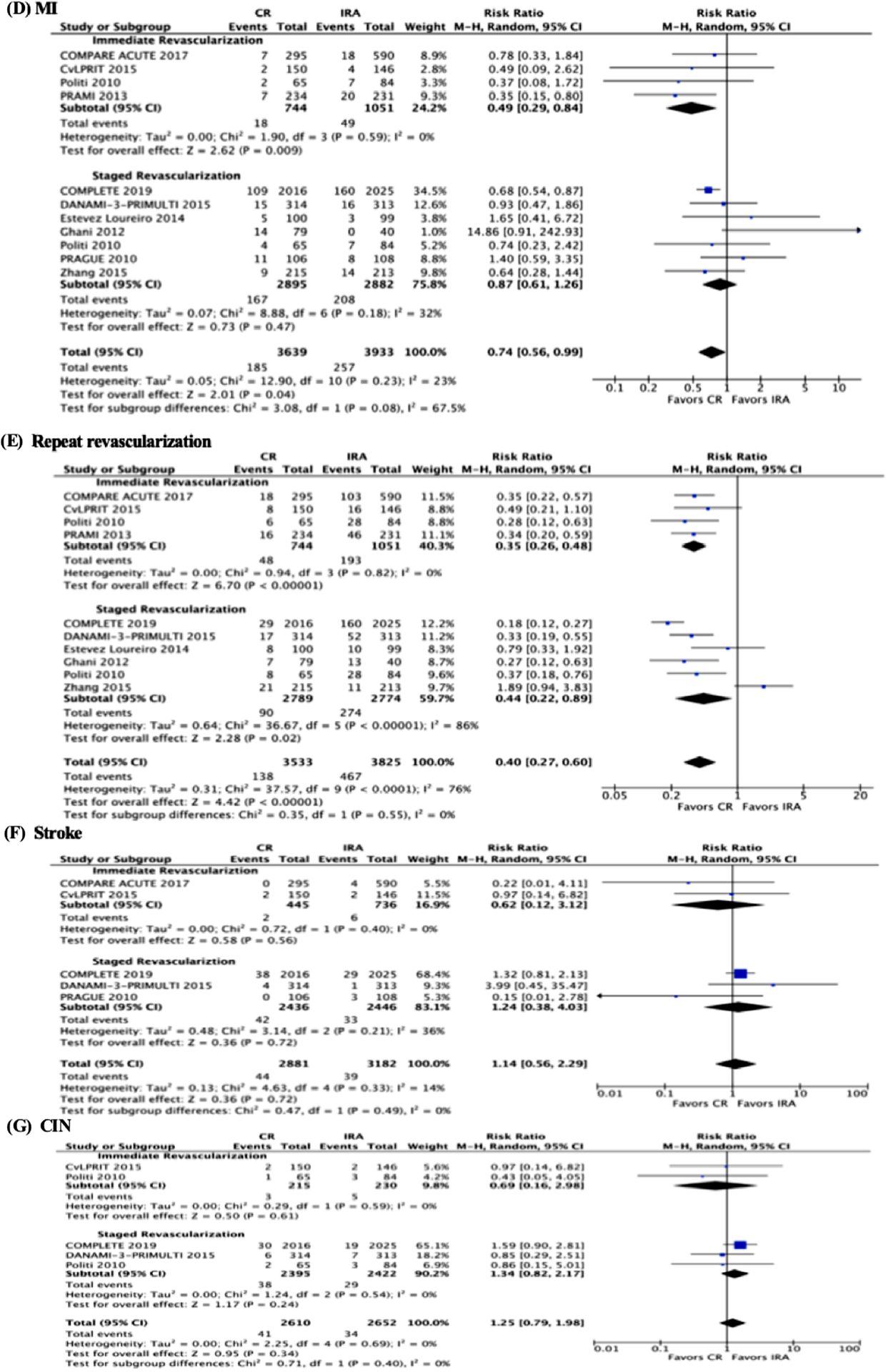
Although there was a trend for less cardiovascular mortality in the complete revascularization group compared with IRA, this did not achieve statistical significance (2.8% vs 3.7%, RR 0.78, 95% CI 0.60 to 1.03, p = 0.08, I2 = 0%) (Figure 2). In the subgroup analysis, we observed a trend for better outcomes in the immediate revascularization group compared with the IRA group (RR 0.41, 95% CI 0.20 to 0.83, p = 0.01, I2 = 0%). On the other hand, the staged revascularization group did not show a statistically significant difference compared with the IRA group (RR 0.82, 95% CI 0.61 to 1.10, p = 0.46, I2 = 0%). However, this did not translate into statistical significance difference between the 2 group (p for interaction = 0.08) (Figure 3). During the process of the leave out sensitivity analysis, after removal of COMPLETE trial, the results showed a statistically significant lower cardiovascular mortality in the CR group versus the IRA group (2.5% vs 4.7%, RR 0.59, 95% CI 0.38 to 0.93, p = 0.02, I2 = 0%) (Figure 4).
Figure 4.
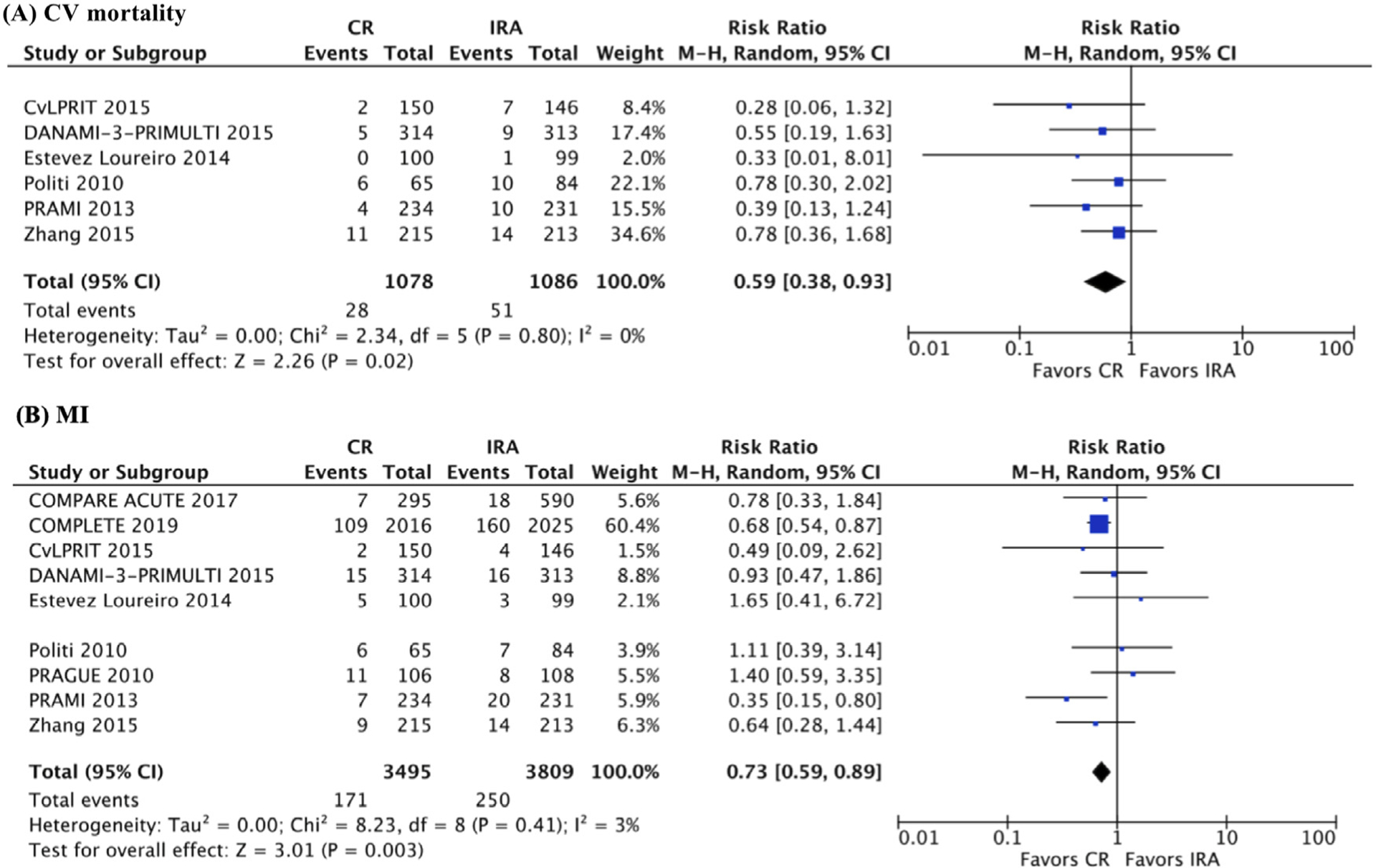
Forest plot comparing complete revascularization and infarct-related artery only revascularization. (A) Myocardial infarction outcome after excluding COMPLETE trial. (B) Cardiovascular mortality outcome after excluding Ghani et al trial. CR = complete revascularization; IRA = infarct-related artery revascularization; CV = cardiovascular; MI = myocardial infarction; RR = risk ratio.
Complete revascularization did not reduce the risk of MI compared with IRA (5.2% vs 6.5%, RR 0.73, 95% CI 0.58 to 1.08, p = 0.08, I2 = 30%) (Figure 2). Moreover, in the subgroup analysis, there was no difference between the immediate and staged revascularization groups (p for interaction = 0.08) (Figure 3). During the process of the leave out sensitivity analysis, after removal of Ghani et al trial, the results showed statistically significant trend of lower MI in the CR group versus the IRA group (5% vs 6.5%, RR 0.73, 95% CI 0.59 to 0.89, p = 0.003, I2 = 3%) (Figure 4).
Complete revascularization reduced the risk of repeat revascularization compared with IRA (4% vs 11.7%, RR 0.44, 95% CI 0.28 to 0.70, p <0.0001, I2 = 81%) (Figure 2). This persisted in the subgroup analysis with no difference between the immediate and staged revascularization groups (p for interaction = 0.55) (Figure 3). These results persisted throughout the process of the leave out sensitivity analysis.
There were no significant differences between CR and IRA in terms of stroke and CIN (1.5% vs 1.2%, RR 1.14, 95% CI 0.56 to 2.29, p = 0.33, I2 = 14%) and (1.6% vs 1.2%, RR 1.35, 95% CI 0.85 to 2.15, p = 0.78, I2 = 0%) (Figure 2), respectively. Moreover, in the subgroup analysis, there was no difference between the immediate and staged revascularization groups for both outcomes (Figure 3). These results persisted throughout the process of the leave out sensitivity analysis.
Discussion
This meta-analysis comparing clinical outcomes of complete versus IRA revascularization in patients with STEMI and multivessel disease offers a comprehensive up-to-date summary of studies comparing the 2 strategies. The salient finding of this analysis is that a CR strategy significantly reduced the risk of MACE typically defined as composite mortality, nonfatal MI, repeat revascularization, and stroke or cardiac hospitalizations. Timing of CR may also play an important role with higher magnitude of benefit in patients who underwent immediate versus staged CR.
Major efforts have been dedicated to examine the benefit of CR in patients with STEMI. However, studies attempting to address this issue have repeatedly produced conflicting results. Observational studies initially showed poorer outcomes for CR and stood up to small, poorly powered RCTs leading to a recommendation against CR.3 Larger RCTs subsequently showed a significant decrease in the need for repeat revascularization with CR, and no adverse impact of this strategy on other outcomes.15 Guidelines were hence updated to consider CR as IIb and IIa recommendations in United States and Europe, respectively.16 In recent years, meta-analyses and the large COMPLETE trial (Complete versus Culprit-Only Revascularization Strategies to Treat Multivessel Disease after Early Percutaneous Coronary Intervention for STEMI) demonstrated clinical benefit for CR using hard outcomes including composite cardiovascular mortality and MI, cardiovascular mortality alone, and composite total mortality and MI.7,8,17−19
To date, this is the only meta-analysis to include the COMPLETE trial. In this study, Mehta et al randomized 4,041 patients with severe nonculprit lesions in a 1:1 ratio to undergo either staged CR or IRA revascularization. At a median follow-up of 3 years, CR reduced the risk of composite cardiovascular death or MI by more than 25% (HR 0.74, p = 0.004). Not only is this the largest study of its kind, but it is the only RCT at this time to show benefit in hard clinical outcomes.20 Their primary outcome was driven by myocardial infarction, which in our analysis only showed a trend toward risk reduction.
Our nonsignificant outcome for MI was impacted by the negative study of Ghani et al which was a staged CR strategy that did not show improvement in MACE. In the sensitivity analysis after excluding Ghani et al trial, the results showed that CR significantly reduced the risk of MI. Ghani et al was published in 2012 and recruited patients from 2004 to 2007 to form a randomized sample of 121 participants who had worse death or MI at 3 years for CR (20.3% vs 0%). Comparing these participants to that of COMPLETE, their sample was the same age, seemingly healthier with less co-morbidities including diabetes mellitus, hyper-tension, and dyslipidemia, and had a lower Killip class on admission (5.0% vs 10.8% ≥Killip class II). Furthermore, the generalizability of the COMPLETE sample has been questioned due to their low SYNTAX scores and relative low risk.20 Nonetheless, with advances in DES technology and antiplatelet strategies, CR in the COMPLETE sample may have had inherent benefit that postdated Ghani et al.
Our meta-analysis has several limitations including variability with study outcomes and definitions. Important outcomes we assessed were MACE and cardiovascular mortality which were not completely uniform for all trials. Additionally, CR strategies including timing of staged PCI were not uniform. Each study had particular inclusion and exclusion criteria which may have introduced confounders. Moreover, the current analysis was study-level meta-analysis which lacked patient-level data. Although meta-analyses display compelling data, guidelines will continue to be driven by large, well-performed RCTs.
In conclusion, this large up-to-date meta-analysis including 7,423 patients from 10 randomized trials documented a significance reduction in the rate of MACE in patients who underwent CR versus IRA after STEMI. This significant reduction is derived mainly by the low rates of repeat revascularization in the CR group and was more pronounced when CR was undertaken at the time of STEMI rather than in a staged fashion.
Supplementary Material
Funding:
None.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
Supplementary materials
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2019.11.017.
References
- 1.Pineda AM, Carvalho N, Gowani SA, Desouza KA, Santana O, Mihos CG, Stone GW, Beohar N. Managing multivessel coronary artery disease in patients with ST-elevation myocardial infarction: a comprehensive review. Cardiol Rev 2017;25:179–188. [DOI] [PubMed] [Google Scholar]
- 2.Sorajja P, Gersh BJ, Cox DA, McLaughlin MG, Zimetbaum P, Costantini C, Stuckey T, Tcheng JE, Mehran R, Lansky AJ, Grines CL, Stone GW. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J 2007;28:1709–1716. [DOI] [PubMed] [Google Scholar]
- 3.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Ting HH, O’Gara PT, Kushner FG, Ascheim DD, Brindis RG, Casey DE Jr., Chung MK, de Lemos JA, Diercks DB, Fang JC, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol 2016;67:1235–1250. [DOI] [PubMed] [Google Scholar]
- 4.Engstrom T, Kelbaek H, Helqvist S, Hofsten DE, Klovgaard L, Holm-vang L, Jorgensen E, Pedersen F, Saunamaki K, Clemmensen P, De Backer O, Ravkilde J, Tilsted HH, Villadsen AB, Aaroe J, Jensen SE, Raungaard B, Kober L, Investigators D-P. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3-PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665–671. [DOI] [PubMed] [Google Scholar]
- 5.Gershlick AH, Khan JN, Kelly DJ, Greenwood JP, Sasikaran T, Curzen N, Blackman DJ, Dalby M, Fairbrother KL, Banya W, Wang D, Flather M, Hetherington SL, Kelion AD, Talwar S, Gunning M, Hall R, Swanton H, McCann GP. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, Berry C, Oldroyd KG, Investigators P. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115–1123. [DOI] [PubMed] [Google Scholar]
- 7.Elgendy IY, Mahmoud AN, Kumbhani DJ, Bhatt DL, Bavry AA. Complete or culprit-only revascularization for patients with multivessel coronary artery disease undergoing percutaneous coronary intervention: a pairwise and network meta-analysis of randomized trials. JACC Cardiovasc Interv 2017;10:315–324. [DOI] [PubMed] [Google Scholar]
- 8.Bajraktari G, Jashari H, Ibrahimi P, Alfonso F, Jashari F, Ndrepepa G, Elezi S, Henein MY. Complete revascularization for patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease: a meta-analysis of randomized trials. Coron Artery Dis 2018;29:204–215. [DOI] [PubMed] [Google Scholar]
- 9.Khan SU, Rahman H, Okunrintemi V, Riaz H, Khan MS, Sattur S, Kaluski E, Lincoff AM, Martin SS, Blaha MJ. Association of lowering low-density lipoprotein cholesterol with contemporary lipid-lowering therapies and risk of diabetes mellitus: a systematic review and meta-analysis. J Am Heart Assoc 2019;8 e011581–e011581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kunz LM, Normand S-LT, Sedrakyan A. Meta-analysis of rate ratios with differential follow-up by treatment arm: inferring comparative effectiveness of medical devices. Stat Med 2015;34:2913–2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwarzer G, Carpenter JR, R€ucker G. Small-Study Effects in Meta-Analysis with R. Cham: Springer International Publishing; 2015:107–141. [Google Scholar]
- 12.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan SU, Duran CA, Rahman H, Lekkala M, Saleem MA, Kaluski E. A meta-analysis of continuous positive airway pressure therapy in prevention of cardiovascular events in patients with obstructive sleep apnoea. Eur Heart J 2018;39:2291–2297. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad Y, Cook C, Shun-Shin M, Balu A, Keene D, Nijjer S, Petraco R, Baker CS, Malik IS, Bellamy MF, Sethi A, Mikhail GW, Al-Bustami M, Khan M, Kaprielian R, Foale RA, Mayet J, Davies JE, Francis DP, Sen S. Resolving the paradox of randomised controlled trials and observational studies comparing multi-vessel angioplasty and culprit only angioplasty at the time of STEMI. Int J Cardiol 2016;222:1–8. [DOI] [PubMed] [Google Scholar]
- 16.Pasceri V, Patti G, Pelliccia F, Gaudio C, Speciale G, Mehran R, Dangas GD. Complete revascularization during primary percutaneous coronary intervention reduces death and myocardial infarction in patients with multivessel disease: meta-analysis and meta-regression of randomized trials. JACC Cardiovasc Interv 2018;11:833–843. [DOI] [PubMed] [Google Scholar]
- 17.Xu H, Zhang X, Li J, Liu H, Hu X, Yang J. Complete versus culprit-only revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease: a meta-analysis of randomized trials. BMC Cardiovasc Disord 2019;19:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta SR, Wood DA, Storey RF, Mehran R, Bainey KR, Nguyen H, Meeks B, Di Pasquale G, Lopez-Sendon J, Faxon DP, Mauri L, Rao SV, Feldman L, Steg PG, Avezum A, Sheth T, Pinilla-Echeverri N, Moreno R, Campo G, Wrigley B, Kedev S, Sutton A, Oliver R, Rodes-Cabau J, Stankovic G, Welsh R, Lavi S, Cantor WJ, Wang J, Nakamya J, Bangdiwala SI, Cairns JA, Committee CTS, Investigators. Complete revascularization with multivessel PCI for myocardial infarction. N Engl J Med 2019;381:1411–1421. [DOI] [PubMed] [Google Scholar]
- 19.Shah R, Berzingi C, Mumtaz M, Jasper JB, Goswami R, Morsy MS, Ramanathan KB, Rao SV. Meta-analysis comparing complete revascularization versus infarct-related only strategies for patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. Am J Cardiol 2016;118: 1466–1472. [DOI] [PubMed] [Google Scholar]
- 20.Kober L, Engstrom T. A more COMPLETE picture of revascularization in STEMI. N Engl J Med 2019;381:1472–1474. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


