Abstract
We evaluated the performance of X-bar chart, exponentially weighted moving average, and C3 cumulative sums aberration detection algorithms for acute diarrheal disease syndromic surveillance at naval sites in Peru during 2007–2011. The 3 algorithms’ detection sensitivity was 100%, specificity was 97%–99%, and positive predictive value was 27%–46%.
Keywords: outbreak detection algorithms, syndromic surveillance, acute diarrheal disease, resource-limited setting, enteric infections
Syndromic surveillance uses prediagnostic health-related data to signal probable outbreaks warranting public health response (1). Alerta and Vigila are internet-based syndromic surveillance systems successively implemented by Peru’s navy (2–4). Among other disease syndromes, individual cases of acute diarrheal disease (ADD) are self-reported to healthcare workers at sites providing care for service members, dependents, and civilian employees. We assessed the performance of 3 ADD aberration detection algorithms in this resource-limited setting: X-bar chart, exponentially weighted moving average (EWMA), and Early Aberration Reporting System (EARS) C3 cumulative sums (CUSUM) models (5–9).
The Study
We defined ADD as >3 loose stools within 24 hours lasting <14 days, epidemic threshold as the incidence of cases in excess of normal for a given period, outbreak as the detection of ADD incidence above the epidemic threshold, true outbreak as an outbreak identified by the system with confirmation by trained field personnel (e.g., enteropathogen isolation), and epidemiological silence as a period during which no cases were reported. We performed descriptive analysis of ADD cases by using data from all reporting sites during 2007–2011, then conducted subsequent analyses by using data on nonbloody ADD. We calculated ADD incidence from weekly reports from Alerta and Vigila during 2007–2011 for naval bases with population denominator data available. We compared the number of site-weeks during which >1 ADD case was reported on shore-based sites with those of sea-based sites and nonbloody ADD incidence in summer with incidence in nonsummer months by using a Mann-Whitney test.
Sites with <4 months of epidemiologic silence during 2007–2011 (60 months) were included for outbreak detection analysis. We aggregated nonbloody ADD case counts by epidemiologic week and performed a timeseries analysis by using X-bar chart, EWMA, and modified EARS C3 CUSUM aberration detection algorithms to flag potential outbreak weeks (8). Algorithm details are provided in the Appendix.
To account for seasonal variability, nonbloody ADD cases for each week during 2009–2011 (36 months) were compared with an 8-week sliding historical baseline calculated from the current and previous 2 years (10,11). We excluded signals from weeks with <5 cases to minimize false signals associated with epidemiologic silence. Because of ADD’s <1-week incubation period, we did not consider buffer intervals, except when implementing the C3 CUSUM-like algorithm, which sums positive differences in cases from the mean for the past 3 periods. We optimized X-bar k, EWMA k and λ, and CUSUM k and h by exploring X-bar and EWMA k and CUSUM h values ranging from 2 to 6, CUSUM k values 1 to 3.5, and λ values 0.25 to 0.5, choosing parameters to maximize specificity and positive predictive value (PPV) while maintaining perfect sensitivity in predicting outbreaks at a randomly selected site (Policlínico Naval Ancón) (7). We calculated algorithm sensitivity, specificity, and PPV and compared each model’s performance by using pairwise exact McNemar tests with Bonferroni correction, using data from 5 sites capable of confirming true outbreaks through epidemiologic links (517 site-weeks). We performed all analyses in R version 3.6.3 (https://cran.r-project.org/bin/windows/base/old/3.6.3); p values <0.05 were considered statistically significant.
During 2007–2011, a total of 144 sites reported 48,409 ADD cases, 98% of which were nonbloody. A total of 8,860 nonbloody cases were reported from 91 sites in 2007, 10,775 cases from 101 sites in 2008, 9,347 cases from 107 sites in 2009, 9,698 cases from 120 sites in 2010, and 8,588 cases from 118 sites in 2011. Of all these cases, 87% occurred in persons >5 years of age, 9% in children 1–4 years of age, and 4% in children <1 years of age. During 2007–2011, nonbloody ADD incidence peaked in 2008 at 305.2 cases/1,000 population (Figure 1). Seasonal incidence was higher during Peru’s summer months (median 14.3 cases/1,000 population), January through March, compared with other months (median 12.5 cases/1,000 population; p = 0.0003).
Figure 1.
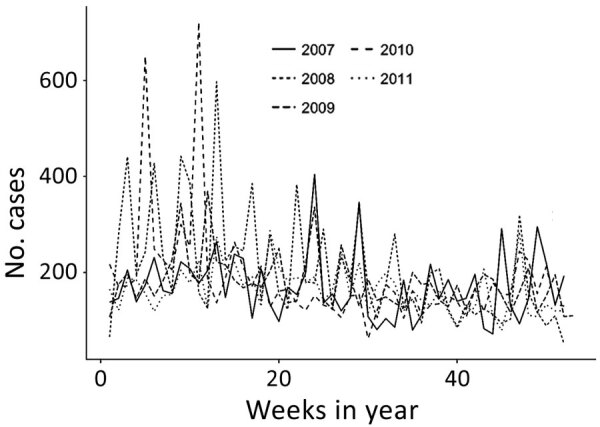
Epidemic curve for nonbloody acute diarrheal disease cases, by week, captured by the Alerta and Vigila Systems, Peru, 2007–2011.
The median proportion of weeks during which a site reported >1 ADD case was 19% (interquartile range [IQR] 5%–44%), and the median length of epidemiologic silence was 58 weeks (IQR 13–147 weeks). We observed no statistically significant difference in the proportion of weeks with >1 ADD case between sea-based and shore-based sites (p = 0.55).
We established the aberration detection algorithm by using 6,962 site-weeks of data from the 45 sites with <4 months of epidemiologic silence during 2007–2011 (Table). These reporting sites consisted of 15 ships and 30 land bases from 20 districts within 14 provinces. Site populations ranged from 35 to 10,000 (median 210, IQR 93.75–450). Algorithm parameter sensitivity analysis yielded optimal results when X-bar k = 4.5, EWMA k = 4 and λ = 0.25, and CUSUM k = 1.5 and h = 3 (Appendix Figures 1–3).
Table. Nonbloody acute diarrheal disease case count and incidence, 2007–2011, and true outbreak detection data and algorithm performance, 2009–2011 for the 45 naval surveillance sites in Peru, analyzed by using X-bar chart, exponentially weighted moving average, and Early Aberration Reporting System C3 cumulative sums models*.
| Surveillance site | Total cases, 2007–2011 | Average cases/week/1,000 population, 2007–2011 | Date of true outbreak detection, case count, incidence, 2009–2011 | Average outbreak detection algorithm performance, 2009–2011 |
|---|---|---|---|---|
| BAP Aguirre |
393 |
13.45 |
2009 Jan 24, 25 cases, 109/1,000 population |
Sensitivity 100%, specificity 97.4%, PPV 20.0% |
| BAP Bolognesi | 334 | 11.04 | ‡ | ‡ |
| BAP Carvajal | 581 | 14.56 | ‡ | ‡ |
| BAP Eten | 129 | 27.95 | ‡ | ‡ |
| BAP Grau | 887 | 9.04 | ‡ | ‡ |
| BAP Mariátegui | 490 | 16.64 | ‡ | ‡ |
| BAP Montero | 321 | 12.39 | ‡ | ‡ |
| BAP Paita | 185 | † | ‡ | ‡ |
| BAP Palacios | 1,118 | 27.16 | ‡ | ‡ |
| BAP Pisagua | 224 | 55.04 | ||
| BAP Pisco | 283 | † | ||
| BAP Quiñones | 289 | 9.17 | ||
| BAP Sánchez Carrión |
156 |
39.90 |
‡ |
‡ |
| BAP Velarde |
114 |
36.54 |
2011 Sep 5, 12 cases, 250 cases/1,000 population |
Sensitivity 100%, specificity 100%, PPV 100% |
| BAP Villavicencio | 251 | 9.20 | ‡ | ‡ |
| Base Aeronaval | 991 | 4.19 | ‡ | ‡ |
| Base Naval Chimbote | 349 | 4.90 | ‡ | ‡ |
| Base Naval Nanay | 596 | 4.54 | ‡ | ‡ |
| Base Naval San Juan | 313 | 25.74 | ‡ | ‡ |
| BCT Aguaytia | 214 | 39.81 | ‡ | ‡ |
| BCT Contamana | 261 | † | ||
| BCT Huipoca | 154 | 46.81 | ‡ | ‡ |
| BCT San Alejandro | 118 | 26.22 | ‡ | ‡ |
| Capitanía Puerto Mollendo | 171 | 19.52 | ‡ | ‡ |
| Capitanía Puerto Puno | 246 | 26.74 | ‡ | ‡ |
| Centro Instrucción Técnica Naval | 829 | 3.48 | ‡ | ‡ |
| Clínica Naval de Iquitos | 3,269 | 1.84 | ‡ | ‡ |
| Comandancia Primera Zona Naval |
244 |
21.02 |
‡ |
‡ |
| Comandancia Tercera Zona Naval |
625 |
21.48 |
2010 Aug 14, 31 cases, 207 cases/1,000 population |
Sensitivity 100%, specificity 99.4%, PPV, 50.0% |
| Dirección de Capitanías y Guardacostas | 293 | 5.77 | ‡ | ‡ |
| Dirección de Hidrografía y Navegación | 385 | 8.09 | ‡ | ‡ |
| Escuela Naval | 988 | 4.84 | ‡ | ‡ |
| Estación Naval Isla San Lorenzo | 449 | 24.34 | ‡ | ‡ |
| Estación Naval Mollendo | 343 | 6.42 | ‡ | ‡ |
| Estación Naval Paita | 796 | 8.93 | ‡ | ‡ |
| Estación Naval Pucallpa |
2,098 |
15.22 |
‡ |
‡ |
| Estación Naval Submarinos |
734 |
16.33 |
2010 Feb 8, 21 cases, 100 cases/1,000 population |
Sensitivity 100%, specificity 99.1%, PPV 42.9% |
| Estación Naval de la Comandancia General | 1,260 | † | ‡ | ‡ |
| Hospital Base Naval del Callao |
4,132 |
1.62 |
‡ |
‡ |
| Policlínico Naval Ancón |
2,019 |
5.24 |
2010 Feb 11, 33 cases
18 cases/1,000 population; 2010 Feb 20, 22 cases, 12 cases/1,000 population |
Sensitivity 100%, specificity 98.1%, PPV 40.0% |
| Policlínico Naval San Borja | 2,892 | 134.51 | ‡ | ‡ |
| Posta Naval de Ventanilla | 1,110 | 113.15 | ‡ | ‡ |
| Villa Naval de Tumbes–El Salto | 710 | † | ‡ | ‡ |
*BAP, Buque de la Armada Peruana (Peru Navy ship); BCT, Base Contraterrorist (Counter-terrorist base); PPV, positive predictive value. †No denominator data available. ‡True outbreak data not available because of lack of on-site capability to establish epidemiologic link.
We estimated algorithm sensitivity, specificity, and PPV by categorizing 785 weeks of data into positive and negative outbreak weeks and comparing each algorithm’s outbreak predictions with data from the 5 sites capable of confirming true outbreaks during 2009–2011 (Figure 2). X-bar produced 13 signals, EWMA 13 signals, and CUSUM 20 signals. Six true outbreaks occurred (Table); all were detected by X-bar, EWMA, and CUSUM algorithms, corresponding to 100% sensitivity for each algorithm. Algorithm specificity across the 5 sites was 99.1% for X-bar, 99.1% for EWMA, and 98.2% for CUSUM. PPV was 46.2% for X-bar, 46.2% for EWMA, and 30% for CUSUM. X-bar and EWMA each produced 7 false-positives, and CUSUM produced 14 false-positives. The performance differences were not statistically significant.
Figure 2.
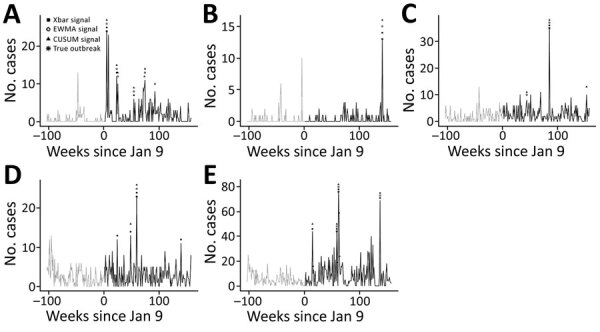
Epidemic curves for nonbloody acute diarrheal disease over time, demonstrating outbreaks identified by the Alerta and Vigila Systems, by identifying algorithm and surveillance site, Peru, 2009-2011. A) Buque de la Armada Peruana Aguirre; B) BAP Velarde; C) Comandancia Tercera Zona Naval; D) Estación Naval Submarinos; and E) Policlínico Naval Ancón. Shapes correspond with identifying algorithms; asterisks indicate outbreaks confirmed through epidemiologic links (i.e., true positives). CUSUM, C3 cumulative sums; EWMA, exponentially weighted moving average.
Conclusions
X-bar, EWMA, and C3 CUSUM aberration detection algorithms identified all ADD outbreaks during 2009–2011, and approximately one third to one half of algorithm outbreak signals corresponded to true outbreaks. These findings suggest that these algorithms can usefully inform outbreak asset deployment, particularly in resource-limited settings.
Overall, X-bar and EWMA performed marginally better than CUSUM (PPV 46% vs. 30%). CUSUM frequently produced false-positives in the weeks after large outbreaks (e.g., after the 76-case outbreak at Policlínico Naval Ancón) (Table). X-bar’s successful detection of ADD in the context of weekly reporting schedules and short disease incubation periods is consistent with its design, which favors detection of events lasting 1 epidemiologic period. In contrast, EWMA and CUSUM were designed for earlier detection of consecutive small baseline deviations (12). Whereas EWMA can be tuned to favor shorter outbreaks through its weighting parameter (λ), the C3 CUSUM algorithm is more rigid. In the context of weekly ADD reporting, EWMA and CUSUM algorithm performance might improve by counting consecutive weeks with outbreak signals as a single alert.
Our study has limitations, including the number of sites capable of confirming outbreaks, which reduced the statistical power to detect differences between algorithms, and the inability to distinguish a lack of reporting versus a lack of ADD cases to report during periods of epidemiologic silence. Combined, these factors limited the evaluation to 3,925 site-weeks of observation, reducing the reliability of algorithm parameter estimates. Furthermore, model parameters were established on only 1 of the 5 evaluation sites; a larger development set would better optimize model parameters while avoiding overfitting.
Characterizing algorithm parameter tradeoffs might aid system capability alignment with health priorities. Lower detection thresholds are advantageous for high-risk diseases with distinct syndromes, such as cholera, Ebola, and Middle East respiratory syndrome. Conversely, changing parameters, such as changing EWMA’s weighting parameter (λ), can affect algorithm PPV (increasing to >60% during sensitivity analysis). Context-focused exploration could inform which parameters should be tuned to improve PPV, sensitivity, or specificity. Because smaller populations and stable disease baselines improve algorithm performance, tuning algorithm parameters for specific sites during implementation by using historical data might improve overall system performance, as might periodic evaluation of model assumptions, parameter tuning, and model performance.
Additional information about assessing 3 outbreak detection algorithms in an electronic syndromic surveillance system in a resource-limited setting
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the governments of the United States or Peru.
Several authors of this manuscript are employees of the US Government. This work was prepared as part of their duties. Title 17 U.S.C. § 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. § 101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Biography
Ms. Alsentzer is a PhD student in the Harvard–MIT Program in Health Science and Technology. Her background is in computer science and biomedical informatics, and her research focuses on machine learning applications to healthcare. Dr. Ballard is a medical epidemiologist in the Epidemic Intelligence Service at the Centers for Disease Control and Prevention. Her background is in tropical diseases, surveillance, and global public health.
Footnotes
Suggested citation for this article: Alsentzer E, Ballard SB, Neyra J, Vera DM, Osorio VB, Quispe J, et al. Assessing 3 outbreak detection algorithms in an electronic syndromic surveillance system in a resource-limited setting. Emerg Infect Dis. 2020 Sep [date cited]. https://doi.org/10.3201/eid2609.191315
These first authors were co–principal investigators and contributed equally to this article.
References
- 1.Henning KJ. Overview of syndromic surveillance: what is syndromic surveillance? MMWR Morb Mortal Wkly Rep. 2004;53(Suppl):5–11. [Google Scholar]
- 2.Margevicius KJ, Generous N, Abeyta E, Althouse B, Burkom H, Castro L, et al. The Biosurveillance Analytics Resource Directory (BARD): facilitating the use of epidemiological models for infectious disease surveillance. PLoS One. 2016;11:e0146600. 10.1371/journal.pone.0146600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blazes DL, Lewis SH. Disease surveillance: technological contributions to global health security. Boca Raton (Florida): CRC Press; 2016. p. 120–1. [Google Scholar]
- 4.Soto G, Araujo-Castillo RV, Neyra J, Fernandez M, Leturia C, Mundaca CC, et al. Challenges in the implementation of an electronic surveillance system in a resource-limited setting: Alerta, in Peru. BMC Proc. 2008;2(Suppl 3):S4. 10.1186/1753-6561-2-s3-s4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burkom H. Development, adaptation, and assessment of alerting algorithms for biosurveillance. Johns Hopkins APL Tech Dig. 2003;24:335–42 [cited 2020 Apr 4]. https://www.jhuapl.edu/content/techdigest/pdf/v24-n04/24-04-burkom.pdf
- 6.Hutwagner L, Thompson W, Seeman GM, Treadwell T. The bioterrorism preparedness and response Early Aberration Reporting System (EARS). J Urban Health. 2003;80(Suppl 1):i89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fricker RD Jr, Hegler BL, Dunfee DA. Comparing syndromic surveillance detection methods: EARS’ versus a CUSUM-based methodology. Stat Med. 2008;27:3407–29. 10.1002/sim.3197 [DOI] [PubMed] [Google Scholar]
- 8.Fricker R. Introduction to statistical methods for biosurveillance: with an emphasis on syndromic surveillance. Cambridge: Cambridge University Press; 2013. p. 178–215. [Google Scholar]
- 9.Hutwagner LC, Thompson WW, Seeman GM, Treadwell T. A simulation model for assessing aberration detection methods used in public health surveillance for systems with limited baselines. Stat Med. 2005;24:543–50. 10.1002/sim.2034 [DOI] [PubMed] [Google Scholar]
- 10.Murphy SP, Burkom H. Recombinant temporal aberration detection algorithms for enhanced biosurveillance. J Am Med Inform Assoc. 2008;15:77–86. 10.1197/jamia.M2587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathes RW, Lall R, Levin-Rector A, Sell J, Paladini M, Konty KJ, et al. Evaluating and implementing temporal, spatial, and spatio-temporal methods for outbreak detection in a local syndromic surveillance system. PLoS One. 2017;12:e0184419. 10.1371/journal.pone.0184419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lombardo J. Disease surveillance: a public health approach. Hoboken (NJ): John Wiley & Sons, Inc.; 2007. p. 158. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional information about assessing 3 outbreak detection algorithms in an electronic syndromic surveillance system in a resource-limited setting


