Abstract
Objective
To evaluate the clinical efficacy of internal fixation versus hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly.
Methods
A search was conducted in PubMed, Web of Science, Embase, and Cochrane Library databases up to April 2020. The present study compared internal fixation and hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly. RevMan5.3 software provided by the International Cochrane Group was used for the meta‐analysis. To compare the differences in the operation time, intraoperative bleeding, length of hospital stay, superficial infection, Harris hip score, mortality within 1 year, mortality within 2 years, reoperation, incidence of deep venous thrombosis (DVT), partial weight‐bearing time, non‐union, and implant‐related complications between an internal fixation group and an hemiarthroplasty group.
Results
A total of 1300 patients were included in nine studies. The results showed that the operation time (MD = −18.09, 95% CI: −27.85–−8.34, P = 0.0003), intraoperative bleeding (MD = −195.31, 95% CI: −244.8–−147.74, P < 0.0001), implant‐related complications (MD = 3.83, 95% CI: 1.74–8.45, P = 0.0008), and partial weight‐bearing time (MD = 17.21, 95% CI: 1.63–32.79, P = 0.03) have statistical significance. However, there is not statistical significance for the Harris hip joint function scale (HHS) (MD = 5.60, 95% CI: −1.13–12.33, P = 0.10), DVT (MD = 1.02, 95% CI: 0.45–2.27, P = 0.97), length of hospital stay (MD = ‐1.08, 95% CI: −2.82–0.66, P = 0.22), superficial Infection (OR = 0.92, 95% CI: 0.43–1.98, P = 0.89), mortality within 1 year (OR = 0.95, 95% CI: 0.61–1.48, P = 0.81), mortality within 2 years (OR = 0.93, 95% CI: 0.61–1.43, P = 0.75), reoperation (MD = 1.80, 95% CI: 0.64–5.04, P = 0.26), and non‐union (OR = 1.20, 95% CI: 0.48–3.03, P = 0.70). The result of the subgroup analysis showed no significant differences between the less than 2 years follow‐up and the 2 years or more follow‐up group. The only difference was for the Harris hip score: the internal fixation group was superior to the hemiarthroplasty group in the less than 2 years subgroup analysis, while there was no difference between the internal fixation group hemiarthroplasty group in the 2 years or more subgroup analysis.
Conclusion
Compared with the internal fixation group, those in the hemiarthroplasty group could carry out weight‐bearing training early and implant‐related complications were reduced, but it requires longer operation time and there is greater intraoperative blood loss. There is no difference in mortality, the incidence of DVT, non‐union, HHS, reoperation, length of hospital stay, and superficial infection. Hemiarthroplasty may be a better choice for unstable intertrochanteric fractures in the elderly.
Keywords: Elderly, Hemiarthroplasty, Hip fractures, Internal fixators, Meta‐analysis
Introduction
Hip fractures are common and are a huge economic burden on the healthcare system. The morbidity of intertrochanteric fractures is rising and the number of hip fractures worldwide could reach 4.5 mn by 2050 1 . Aging and osteoporosis are the main causes of hip fractures. In an epidemiological investigation in Spain of 4415 patients with hip fractures, 4271 (3346 females, 925 males) were diagnosed with osteoporosis 2 . With osteoporosis, the trabeculae become thinner and sparse, the bone cortex becomes thinner, and the bone strength decreases. Slight trauma can easily result in fracture. Once a femoral intertrochanteric fracture occurs, a comminuted fracture can easily occur 3 .
Femoral intertrochanteric fractures account for approximately half of all hip fractures. Intertrochanteric fractures can be divided into stable and unstable fractures based on AO/OTA or Evans–Jensen classification. A2, A3, or Evans–Jensen III, IV, and V are considered unstable intertrochanteric fractures. For unstable intertrochanteric fractures in the elderly, conservative treatment can lead to complications, such as bedsores, deep venous thrombosis (DVT), pendant pneumonia, and death. According to clinical trials, surgical treatment has the advantages of stable fixation and getting out of bed sooner, so it has gradually become the first choice in the clinic 4 . Although the best surgical treatment has always been controversial, the main aims are early rehabilitation and return to social activities. Internal fixation and hip replacement are the main surgical treatments. Internal fixation includes use of cephalomedullary nails, proximal femoral nail antirotation, proximal femoral nails, gamma nails, dynamic hip screws, and compression hip screws. Hip replacement includes application of hemiarthroplasty and total hip arthroplasty. Camurcu 5 points out that hemiarthroplasty has the advantages of early mobilization, acceptable functional results, and lower failure rates in the treatment of unstable intertrochanteric fractures in elderly patients. Kumar et al. conducted a meta‐analysis of proximal femoral nails versus hemiarthroplasty in the treatment of unstable intertrochanteric fractures 6 and Li et al. conducted a meta‐analysis of internal fixation versus external fixation in the treatment of unstable interochanteric 7 . However, there is no meta‐analysis comparing internal fixation versus hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly. We conducted a meta‐analysis to compare the clinical efficacy and safety of internal fixation and hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly. The outcome indicators include operation time, intraoperative bleeding, length of hospital stay, superficial infection, Harris hip joint function scale (HHS), mortality within 1 year, mortality within 2 years, reoperation, DVT, partial weight‐bearing time, implant‐related complications, and non‐union.
Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement was used to guide the study 8 .
Information Sources and Search Strategy
We searched four electronic databases up to April 2020: Embase, Pubmed, Web of Science, and Cochrane Library. We used mesh and free terms to search the electronic databases, Medical Subject Headings (MeSH terms) “hemiarthroplasty” and free terms, MeSH terms “hip fractures” and free terms, MeSH terms “internal fixators” and free terms: (Hemiarthroplasty OR hemiarthroplasties OR hemiarthroplasty OR hemi‐arthroplasties) AND (hip fractures OR intertrochanteric fractures OR intertrochanteric femoral fracture OR trochanteric fracture) AND (internal fixators OR internal fixation OR internal fixator OR cephalomedullary nail OR proximal femoral nail antirotation OR proximal femoral nail OR intramedullary nail OR gamma nail OR InterTAN nail OR DHS OR dynamic hip screw OR CHS OR compression hip screw OR plate).
Inclusion Criteria and Exclusion Criteria
The inclusive selection criteria are as follows:
Elderly patient (patient ≥60 years old) with unstable intertrochanteric fracture.
Participants were treated with internal fixation, such as cephalomedullary nail, proximal femoral nail antirotation, proximal femoral nail, gamma nail, INTERTAN nail, dynamic hip screw, compression hip screw, or plate.
Participants were treated with hemiarthroplasty.
Operation time (minute), intraoperative bleeding (mL), length of hospital stay (days), superficial infection, Harris hip score, mortality within 1 year, mortality within 2 years, reoperation, DVT, partial weight‐bearing time (days), non‐union, and implant‐related complications.
Retrospective comparative control trial, randomized controlled trials, or cohort study.
The exclusion criteria were as follows: (i) age <60 years old; (ii) stable intertrochanteric fracture; (iiii) pathological fracture; (iv) open fracture; (v) repeatedly published article; (vi) non‐English literature; (vii) average follow‐up time less than 12 months; and (viii) low quality literature.
Data Extraction
Data includes general information and clinical outcomes. General information includes author, year of publication, study design, average age, gender, type of fracture, and average follow‐up time. Clinical outcomes include operation time (min), intraoperative bleeding (mL), length of hospital stay (days), superficial infection, HHS, mortality within 1 year, mortality within 2 years, reoperation, DVT, partial weight‐bearing time (days), implant‐related complications, and non‐union.
Risk of Bias Assessment
All the literature was screened by two analysts according to the inclusion and exclusion criteria. When the two analysts had different opinions, they would ask the third analyst for their opinion. If the study was a random controlled trial (RCT), the Cochrane Collaboration tool was used for evaluation. The Cochrane Collaboration tool has seven domains for assessment: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete, outcome, selective outcome reporting, and other sources of bias. The risk of bias includes three types: low risk, high risk, or unclear risk. The quality of the non‐RCT was assessed with the Newcastle–Ottawa scale (NOS). It contains eight items, which are categorized into three dimensions: selection, comparability, and exposure (case‐control study) or outcome (cohort study); a maximum of 4 stars could be given in “selection,” a maximum of 2 stars could be given in “comparability,” a maximum of 4 stars could be given in “exposure or outcome.” One star equated to 1 point, the full score was 10 points, and it was classified as low‐quality literature when NOS score ≤ 5 points. The higher the score, the better the quality of the literature.
Statistical Analysis
RevMan 5.3 software was used for data analysis. The odds ratios (OR) represent the continuous variable; weighted mean differences (WMD) represent a dichotomous variable. Both were assessed with 95% confidence intervals. The I 2‐value and the χ2‐test were used to assess the heterogeneity; if the heterogeneity was small (P > 0.1, I 2 ≤ 50%), a fixed effect model was used. If the heterogeneity was large (P < 0.1, I 2 > 50%), a random effect model was used. The forest plot was used to show the results of the meta‐analysis. It was considered statistically significant when the P‐value was less than 0.05.
Result
Literature Screening
The literature was screened strictly by two evaluators by reading the title, abstract, or full text of the article according to the inclusion and exclusion criteria. In the process of extracting the data, the two researchers would recheck it again and again; if there were any differences, the third evaluator would assist. A total of 481 English language studies was preliminarily obtained from the database; 198 were duplicate articles and 259 articles were removed after reading the title or abstract. The full text of 24 articles was read and, finally, nine articles 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 were included in this study (Fig. 1). There were a total of 1300 patients, forming the IF group (n = 776) and the hemiarthroplasty group (n = 524). General information on the nine studies is shown in Table 1.
Fig 1.
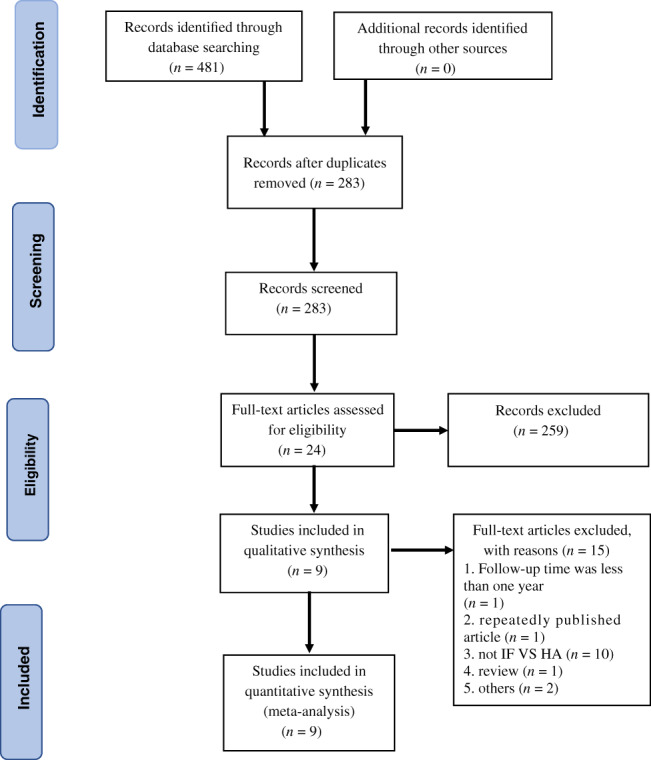
Preferred reporting items for systematic reviews and meta‐analyses flow diagram of study selection.
TABLE 1.
General information of included studies
| Study | Year | Study design | Compassion | Number | Age (years) | Female/male | Outcome | Fracture classification | Follow‐up (months) |
|---|---|---|---|---|---|---|---|---|---|
| Elhadi 9 | 2018 | PCS | IF(PFN,DHS) | 57 | 77.2 ± (65–105) | 31:26 | HJKLM | AO/OTA 31.A2.2.A2.3 | 13.6 |
| HA | 60 | 76.1(65–91) | 37:23 | 12 | |||||
| Jolly 10 | 2019 | RCT | IF(PFN) | 50 | 75(75–85) | unclear | ABDFHJKL | Unstable (unclear) | 12 |
| HA | 50 | 75(75–85) | unclear | 12 | |||||
| Kayali 11 | 2006 | CCT | IF(Unclear) | 45 | 75 ± 6 | 24:21 | ACJK | AO/OTA 31.A2.1‐A3.3 | 29 |
| HA | 42 | 73 ± 9 | 31:12 | 24 | |||||
| Kim 12 | 2020 | CCT | IF(NAIL,DHS) | 396 | 79.5 ± (65–102) | 276:120 | FGH | AO/OTA 31.A2.1.A3.3 | 29 |
| HA | 168 | 83 ± (65–102) | 136:32 | 28 | |||||
| Kim 13 | 2005 | RCT | IF(PFN) | 29 | 81 ± 3.2 | 21:8 | ABCDFHJKLM | Unstable (unclear) | 36 |
| HA | 29 | 82 ± 3.4 | 21:6 | 36 | |||||
| Kim 14 | 2014 | CCT | IF(CHS) | 43 | 75.5 ± 6.5 | 31:11 | ACEJKM | AO/OTA 31.A2. | 25 |
| HA | 46 | 79.7 ± 6.5 | 41:5 | 30 | |||||
| Park 15 | 2015 | CCT | IF(Gamma,PFN,PFNA) | 31 | 78.1(73–86) | 19:12 | ABCDFGHJM | AO/OTA 31.A3 | 24 |
| HA | 22 | 76.9(73–84) | 18:4 | 24 | |||||
| Shen 16 | 2012 | CCT | IF(NAIL,DHS) | 64 | 76.8(70–98) | 48:16 | ABFGHJKLM | AO/OTA 31.A2.2‐A3.3 | 24 |
| HA | 60 | 78.2(70–101) | 47:13 | 24 | |||||
| Zhou 17 | 2019 | CCT | IF(PFNA) | 61 | 83.5 ± 4.8 | 25:36 | ABCDEL | Evens–Jensen III IV V | 28 |
| HA | 47 | 83.8 ± 6.4 | 20:27 | 28 |
A, operation time; B, intraoperative bleeding volume; C, length of hospital stay; CCT, retrospective comparative control trial; CHS, compression hip screw; D, Harris hip joint function scale; DHS, dynamic hip screw; E, partial weight‐bearing time; F, mortality within 1 year; G, mortality within 2 years; H, reoperation; HA, hemiarthroplasty; IF, internal fixation; J, implant‐related complications; K, superficial infection; L, deep venous thrombosis; M, non‐union; NAIL, intramedullary nail (unclear); PCS, prospective cohort study; PFN, proximal femoral nails; PFNA, Proximal Femoral Nail Antirotation; RCT, randomized controlled trials.
Quality Assessment of the Eligible Studies
Two reviewers independently used the Cochrane Collaboration tool for assessing risk bias or used the Newcastle–Ottawa scale (NOS) to assess the quality of the eligible studies: two randomized controlled trials 10 , 13 , one prospective cohort study 9 , and six retrospective studies 11 , 12 , 14 , 15 , 16 , 17 . Risk of bias assessment of RCT was assessed using the Cochrane Collaboration tool. The quality of the RCT were accepted: one has three low risks bias, the other has four low risks bias,Jolly10 and kim13 did not describe allocation concealment, blinding of participants and personnel, blinding of outcome assessment, kim13 did not describe selective outcome reporting (Fig. 2). The quality of the non RCT was assessed with the Newcastle–Ottawa scale. Four studies scored 6 points, two studies scored 7 points, and one study scored 8 points (Table 2).
Fig 2.
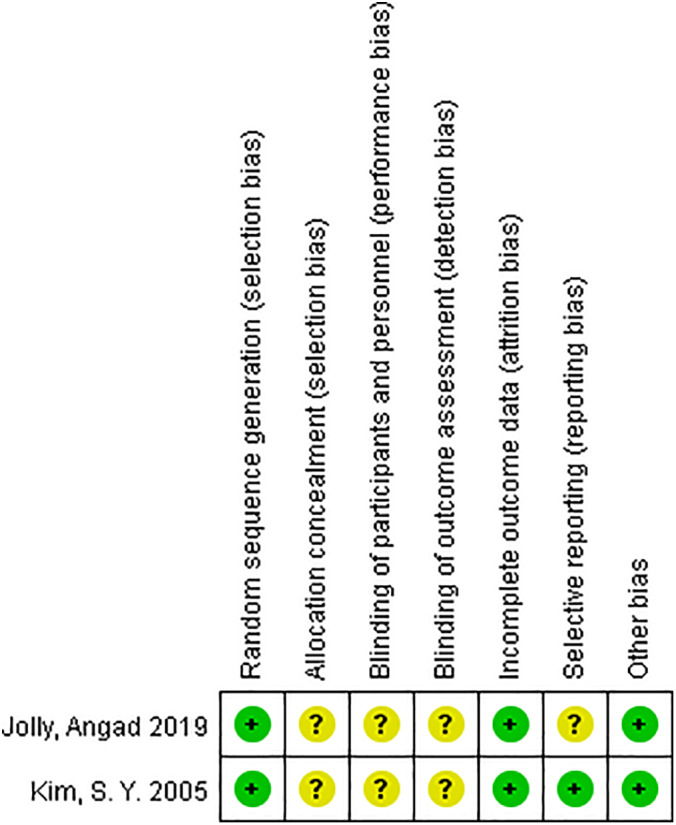
Risk of bias assessment summary of randomized controlled trials.
TABLE 2.
Quality assessment of non‐randomized controlled trials (Newcastle–Ottawa scale for non‐randomized controlled trials)
Intraoperative Bleeding Volume (mL)
Intraoperative blood loss was compared for internal fixation and hemiarthroplasty. Only five articles 10 , 13 , 15 , 16 , 17 mentioned the amount of intraoperative blood loss and included mean and standard deviation. The results of the fixed effect model show that there is statistical heterogeneity among studies (P < 0.00001, I 2 = 96%); the random effect model was then used for analysis. The average intraoperative blood loss of the internal fixation group and the hemiarthroplasty group was 118 mL versus 306 mL. The results showed that the amount of intraoperative bleeding in the internal fixation group was significantly less than that in the hemiarthroplasty group (MD = −195.31, 95% CI: −244.8–−147.74, P < 0.0001) (Fig. 3).
Fig 3.
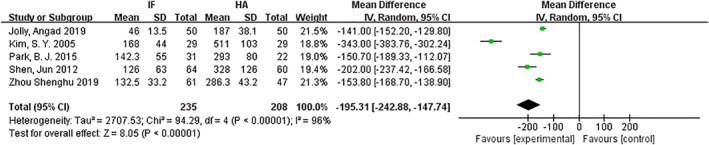
Forest plot diagram of intraoperative bleeding volume compared between internal fixation and hemiarthroplasty.
Operation Time (Min)
The operation times for internal fixation and hemiarthroplasty were compared. Seven articles 10 , 11 , 13 , 14 , 15 , 16 , 17 mentioned operation time and included mean and standard deviation. The results of the fixed effect model show that there is statistical heterogeneity among studies (P < 0.00001, I 2 = 94%) the random effect model was then used for analysis. The average operation time of the internal fixation group and the hemiarthroplasty group was 63.5 min versus 86.3 min. The results showed that the operation time in the internal fixation group was significantly less than that in the hemiarthroplasty group (MD = −18.09, 95% CI: −27.85–−8.34, P = 0.0003) (Fig. 4).
Fig 4.
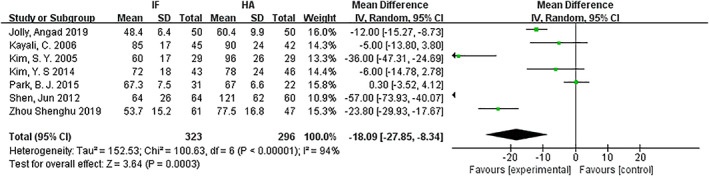
Forest plot diagram of operation time compared between internal fixation and hemiarthroplasty.
Length of Hospital Stay (Days)
Length of hospital stay was compared for internal fixation and hemiarthroplasty. Only five articles 11 , 13 , 14 , 15 , 17 mentioned the hospital stay and included mean and standard deviation. The results of the fixed effect model showed that there is statistical heterogeneity among studies (P < 0.00001, I 2 = 90%); the random effect model was then used for analysis. The results showed that there was no significant difference in length of hospital stay between the internal fixation group and hemiarthroplasty groups (MD = −1.08, 95% CI: −2.82–0.66, P = 0.22) (Fig. 5).
Fig 5.
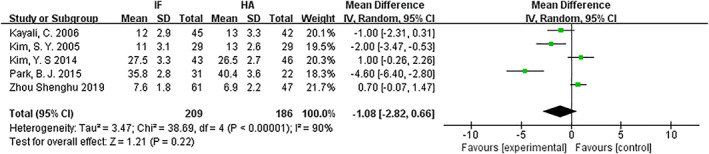
Forest plot diagram of the length of hospital stay compared between internal fixation and hemiarthroplasty.
Harris Hip Joint Function Scale
The HHS at the end of follow up was compared for the internal fixation and the hemiarthroplasty. Only four articles 10 , 13 , 15 , 17 mentioned HHS and included mean and standard deviation. The results of the fixed effect model show that there is statistical heterogeneity among studies (P < 0.00001, I 2 = 87%); the random effect model was then used for analysis. The results showed that there was no significant difference in Harris hip score at the end of follow up between the internal fixation group and the hemiarthroplasty group (MD = 5.60, 95% CI: −1.13–12.33, P = 0.10) (Fig. 6).
Fig 6.
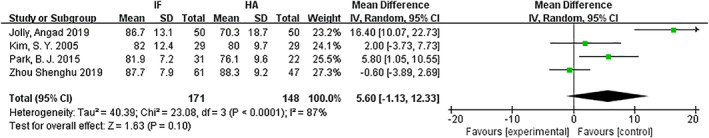
Forest plot diagram of compared Harris hip joint function scale between internal fixation and hemiarthroplasty.
Partial Weight‐Bearing Time (Days)
The partial weight‐bearing times for internal fixation and hemiarthroplasty were compared. Only two articles 14 , 17 mentioned the partial weight‐bearing time and included mean and standard deviation. The results of the fixed effect model show that there is statistical heterogeneity among studies (P < 0.00001, I 2 = 99%); the random effect model was then used for analysis. The average partial weight‐bearing time of the internal fixation group and the hemiarthroplasty group was 25.9 days versus 8.29 days. The results showed that the time of partial weight‐bearing in the internal fixation group was later than that in the hemiarthroplasty group (MD = 17.21, 95% CI: 1.63–32.79, P = 0.03) (Fig. 7).
Fig 7.
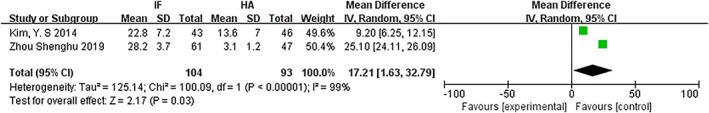
Forest plot diagram of compared partial weight‐bearing between internal fixation and hemiarthroplasty.
Mortality within 1 year
Mortality within 1 year was compared for the internal fixation and hemiarthroplasty. There were seven articles 10 , 12 , 13 , 15 , 16 with references to mortality. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.74, I 2 = 0%). The results showed that there was no significant difference in mortality between the internal fixation group and the hemiarthroplasty group (OR = 0.95, 95% CI: 0.61–1.48, P = 0.81) (Fig. 8).
Fig 8.
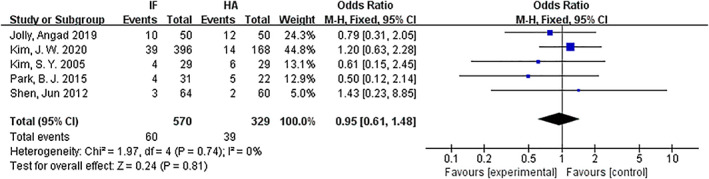
Forest plot diagram of compared mortality within 1 year between internal fixation and hemiarthroplasty.
Mortality within 2 years
Mortality within 2 years was compared for internal fixation and hemiarthroplasty. There were three articles 12 , 15 , 16 with references to mortality. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.36, I 2 = 3%). The results showed that there was no significant difference in mortality within 2 years between the internal fixation group and the hemiarthroplasty group (OR = 0.93, 95% CI: 0.61–1.43, P = 0.75) (Fig. 9).
Fig 9.
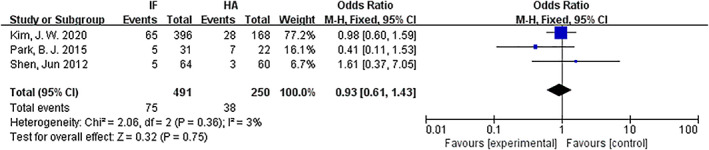
Forest plot diagram of compared mortality within 2 years between internal fixation and hemiarthroplasty.
Reoperation
Reoperation was compared for internal fixation and hemiarthroplasty. Six articles 9 , 10 , 12 , 13 , 15 , 16 mentioned reoperation. The results of the fixed effect model show that there is statistical heterogeneity among studies (P = 0.06, I 2 = 52%); the random effect model was then used for analysis. The results showed that there was no significant difference in reoperation between the internal fixation group and the hemiarthroplasty group (OR = 1.80, 95% CI: 0.64–5.04, P = 0.26) (Fig. 10).
Fig 10.
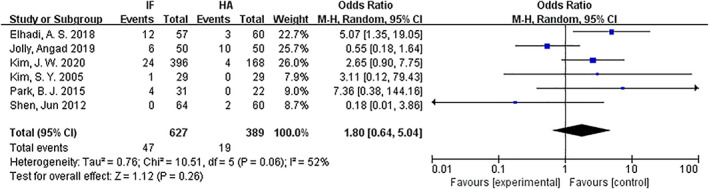
Forest plot diagram of compared reoperation between internal fixation and hemiarthroplasty.
Implant‐Related Complications
Implant‐related complications were compared for internal fixation and hemiarthroplasty. Six articles 9 , 11 , 13 , 14 , 15 , 16 mentioned implant‐related complications. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.31, I 2 = 16%). The implant‐related complications of the internal fixation group and the hemiarthroplasty group were 11.1% versus 3%. The results showed that the implant‐related complications in the internal fixation group were significantly higher than those in the hemiarthroplasty group (OR = 3.83, 95% CI: 1.74–8.45, P = 0.0008) (Fig. 11).
Fig 11.
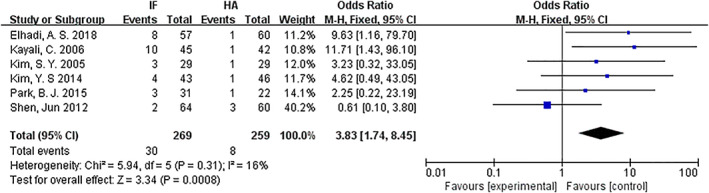
Forest plot diagram of compared implant‐related complications between internal fixation and hemiarthroplasty.
Deep Venous Thrombosis
The DVT for internal fixation and hemiarthroplasty were compared. Five articles 9 , 10 , 13 , 16 , 17 mentioned DVT. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.41, I 2 = 0%). The results showed that there was no significant difference in DVT between the internal fixation group and the hemiarthroplasty group (OR = 1.02, 95% CI: 0.45–2.27, P = 0.97) (Fig. 12).
Fig 12.
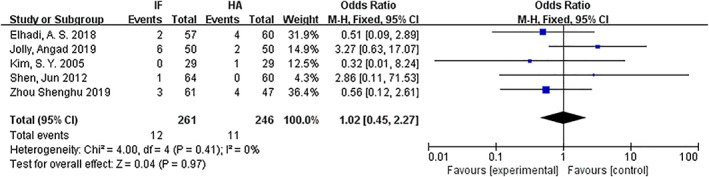
Forest plot diagram of compared deep venous thrombosis between internal fixation and hemiarthroplasty.
Superficial Infection
Superficial infection was compared for internal fixation and hemiarthroplasty. Six articles 9 , 10 , 11 , 13 , 14 , 16 mentioned superficial wound infection. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.56, I 2 = 0%). The results showed that there was no significant difference in superficial infection between the internal fixation group and the hemiarthroplasty group (OR = 0.92, 95% CI: 0.43–1.98, P = 0.89) (Fig. 13).
Fig 13.
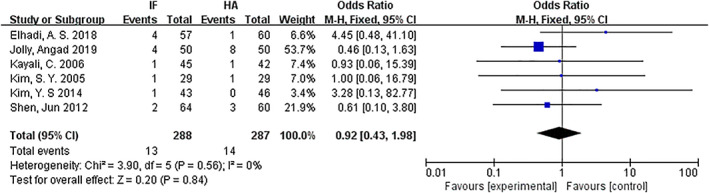
Forest plot diagram of compared superficial infection between internal fixation and hemiarthroplasty.
Non‐union
The non‐union rate was compared for internal fixation and hemiarthroplasty. Five articles 9 , 13 , 14 , 15 , 16 mentioned non‐union. The results of the fixed effect model show that there was no statistical heterogeneity among studies (P = 0.67, I 2 = 0%). The results showed that there was no significant difference in non‐union between the internal fixation group and the hemiarthroplasty group (OR = 1.20, 95% CI: 0.48–3.03, P = 0.70) (Fig. 14).
Fig 14.
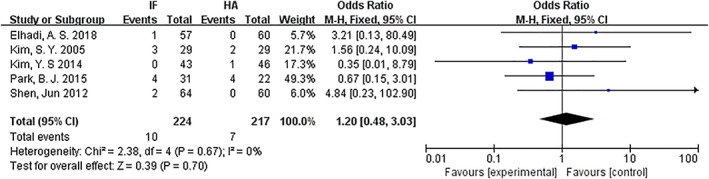
Forest plot diagram of compared non‐union between internal fixation and hemiarthroplasty.
Subgroup Analysis
We performed subgroup analysis based on average follow‐up time. The included studies were classified into less than 2 years and 2 years or more subgroups. The combined results of operation time, intraoperative bleeding, superficial infection, Harris hip score, mortality within 1 year, reoperation, DVT, non‐union, and implant‐related complications are shown in Table 3. Because the study with less than 2 years follow up did not have the outcomes for mortality within 2 years, partial weight‐bearing time, and length of hospital stay, the outcomes were not included in the subgroup analysis. In the less than 2 years subgroup analysis, the combined results showed that the internal fixation group was superior to the hemiarthroplasty group in operation time, intraoperative bleeding, and Harris hip score; the hemiarthroplasty group was superior to the internal fixation group in implant‐related complications. There is no difference in superficial infection, operation time, Harris hip score, mortality within 1 year, reoperation, DVT, non‐union, and implant‐related complications. In the 2 years or more subgroup analysis, the combined results showed that the internal fixation group was superior to the hemiarthroplasty group in operation time and intraoperative bleeding; the hemiarthroplasty group was superior to the internal fixation group in implant‐related complications. There is no difference in superficial infection, Harris hip score, mortality within 1 year, DVT, and non‐union.
TABLE 3.
The combined results of subgroup analysis based on average follow‐up time
| Outcome | Average follow‐up time | Included studies | Number | I 2 | Statistic effect model | Effect estimate | P‐value |
|---|---|---|---|---|---|---|---|
| Intraoperative bleeding | Less than 2 years | 1 | 100 | 0% | MD (fixed, 95% CI) | −4.90 [−5.69, −4.10] | <0.00001 |
| 2 years or more | 4 | 343 | 92% | MD (random, 95% CI) | −3.11 [−4.25, −1.97] | <0.00001 | |
| Operation time | Less than 2 years | 1 | 100 | 0% | MD (fixed, 95% CI) | −12.00 [−15.27, −8.73] | <0.00001 |
| 2 years or more | 6 | 519 | 95% | MD (random, 95% CI) | −20.01 [−33.92, −6.09] | <0.00001 | |
| HHS | Less than 2 years | 1 | 100 | 0% | MD (fixed, 95% CI) | 16.40 [10.07, 22.73] | <0.00001 |
| 2 years or more | 3 | 219 | 58% | MD (random, 95% CI) | 2.13 [−1.87, 6.14] | 0.30 | |
| Mortality within 1 year | Less than 2 years | 1 | 100 | 0% | OR (fixed, 95% CI) | 0.79 [0.31, 2.05] | 0.63 |
| 2 years or more | 4 | 799 | 0% | OR (fixed, 95% CI) | 1.00 [0.60, 1.65] | 0.99 | |
| Reoperation | Less than 2 years | 2 | 217 | 85% | OR (random, 95% CI) | 1.61 [0.18, 14.41] | 0.67 |
| 2 years or more | 4 | 799 | 10% | OR (fixed, 95% CI) | 2.22 [0.97, 5.09] | 0.06 | |
| Implant‐related complications | Less than 2 years | 1 | 117 | 0% | OR (fixed, 95% CI) | 9.63 [1.16, 79.70] | 0.04 |
| 2 years or more | 5 | 411 | 16% | OR (fixed, 95% CI) | 3.10 [1.31, 7.36] | 0.01 | |
| Deep venous thrombosis | Less than 2 years | 2 | 217 | 56% | OR (random, 95% CI) | 1.29 [0.23, 7.10] | 0.77 |
| 2 years or more | 3 | 290 | 0% | OR (fixed, 95% CI) | 0.69 [0.20, 2.31] | 0.54 | |
| Superficial infection | Less than 2 years | 2 | 217 | 68% | OR (random, 95% CI) | 1.18 [0.13, 10.84] | 0.88 |
| 2 years or more | 4 | 358 | 0% | OR (fixed, 95% CI) | 0.97 [0.29, 3.21] | 0.96 | |
| Non‐union | Less than 2 years | 1 | 117 | 0% | OR (fixed, 95% CI) | 3.21 [0.13, 80.49] | 0.48 |
| 2 years or more | 4 | 324 | 0% | OR (fixed, 95% CI) | 1.08 [0.41, 2.86] | 0.88 |
CI, confidence interval; HHS, Harris hip joint function scale; MD, mean difference; OR, odds ratio
Discussion
Unstable intertrochanteric fractures account for approximately 50% of femoral intertrochanteric fractures. Conservative treatment of unstable intertrochanteric fractures in the elderly will result in a variety of complications and high mortality rates. Surgical treatment can reduce the incidence of complications and death 18 . Controversy exists about the best surgical treatment for unstable intertrochanteric fractures in the elderly 4 . Some authors believe that internal fixation is associated with higher complications in the treatment of unstable intertrochanteric fractures in the elderly. Joint replacement is a better option for unstable intertrochanteric fractures in the elderly 19 . Internal fixation and hemiarthroplasty are widely used in unstable intertrochanteric fractures in the elderly. Internal fixation includes all kinds of plates, dynamic hip screws, and various intramedullary nails. In this meta‐analysis, we evaluated the clinical outcome of elderly patients with unstable intertrochanteric fractures who underwent internal fixation or hemiarthroplasty.
In this meta‐analysis, the operation time and intraoperative blood loss was significantly less in the internal fixation group than in the hemiarthroplasty group. However, in terms of implant‐related complications and partial weight‐bearing time, the hemiarthroplasty group was significantly better than the internal fixation group. There was no difference in Harris hip score, hospital stay, mortality within 1 year, mortality within 2 years, reoperation, superficial infection, non‐union rate, and DVT incidence between the two groups.
Operation time and intraoperative bleeding are important indexes of surgery. The operation time is proportional to the intraoperative blood loss. Long operation time means longer anesthesia time, which will increase the probability of gastrointestinal and respiratory system‐related complications. Operation time and intraoperative blood loss were significantly less for internal fixation than for hemiarthroplasty, but the heterogeneity was relatively large. The selection of internal fixation and the technique of the clinician may be the main reasons for the high heterogeneity. Yang 20 points out that the percutaneous compression plate has more intraoperative blood loss and longer operation time than Gamma3. Prolongation of operation time and increase in intraoperative bleeding will increase the risk of wound infection. Wound infection is related to gender, body mass index, and surgeon's level of experience 21 . Wound infection includes superficial and deep infection. In this article, both groups have 6 cases of deep infection; there were 13 cases of superficial infection in the internal fixation group and 14 cases in the hemiarthroplasty group. There was no difference in the risk of superficial and deep infection between the internal fixation group and the hemiarthroplasty group. In Jolly et al., the infection rate in the hemiarthroplasty group (24%) was significantly higher than that in the internal fixation group (8%) 10 . If the wound is infected, this will lead to a longer stay in hospital and increase the cost of hospitalization. Kim 11 points out that the clinical cost of the hemiarthroplasty group was significantly higher than that of the internal fixation group. In Wang's 22 survey of the clinical cost of hip fractures in China, the cost of joint replacement is slightly higher than that of internal fixation. The cost of hip fracture has become a considerable burden for patients. There is no significant difference in hospital stay between the internal fixation group and hemiarthroplasty group, but the heterogeneity is great. Despite the people in the study all being over 60 years old, the age range is relatively large. Some have more physical diseases and stay in the hospital for a longer time. Yoo 23 points out that the hospital stay was short (less than 10 days), and the mortality rate was as high as 21.7% 1 year later; when hospital stay was 11–20 days, the mortality was only 12.4% 1 year later. In this meta‐analysis, there was no significant difference in mortality within 1 year and within 2 years between the internal fixation group and the hemiarthroplasty group. Morri 24 points out that the main causes of death within 1 year of hip fracture were older age, more comorbidities, and physical weakness.
The degree of hip function recovery affects patients' quality of life. The commonly used score for hip function is the HHS. The higher the score, the better the recovery of hip function 25 . The HHS is a rating scale with a total of 100 points (excellent, ≥90 points; good, 80–89 points; fine, 70–79 points; and poor, <70 points): it includes deformity, motion, the domains of pain, and function. In the comparison of the HHS, there was no significant difference between the two groups. In the less than 2 years subgroup analysis, the internal fixation group was superior to hemiarthroplasty group in the HHS. The main reason may be that only one study was included in the subgroup analysis. Salpakoski 26 point out that there are more patients with difficulty walking after internal fixation than hemiarthroplasty or total hip arthroplasty. Early postoperative walking ability is a significant predictor of postoperative survival in elderly patients with hip fractures 27 . Partial weight‐bearing can be carried out earlier in the hemiarthroplasty group than in the internal fixation group. Kim 12 points out that most of the patients (140/168) in the hemiarthroplasty group can start to walk with crutches or with a walker within 1 week after the hemiarthroplasty. Early partial weight‐bearing can reduce complications, such as bedsores and decreased lung function, caused by prolonged bedrest 28 .
Implant‐related complications mainly include implant loosening, implant stimulation, cut‐out, prosthesis dislocation, re‐fracture, shortening, protrusion of neck screw, and breakage of the screw. In this meta‐analysis, the implant‐related complications in the internal fixation group were significantly higher than those in the hemiarthroplasty group. Screw cut‐out is the most common complication in the internal fixation group, while prosthesis dislocation is the most common in the hemiarthroplasty group. In Nie's 29 meta‐analysis, he also points out that hip joint replacement has fewer implant‐related complications than intramedullary fixation in the treatment of intertrochanteric fractures. Most reoperations are due to implant‐related complications. There are many factors affecting reoperation; despite the need for reoperation, some patients still refuse a reoperation. Authen points 30 out that doctors with less than 3 years of clinical experience have a higher revision rate than clinicians with more than 3 years of clinical experience. In this study, there was no significant difference in the rate of reoperation between the internal fixation group and the hemiarthroplasty group.
Deep venous thrombosis is a problem that cannot be ignored in hip fractures. Mula points out that the probability of DVT after hip fracture is 0.55%. Suspected DVT should be detected by Doppler ultrasonography in time 31 . The perioperative period is crucial for the prevention of DVT; the use of warfarin, low molecular weight heparin, and elastic socks can effectively reduce the incidence of venous embolism. The occurrence of venous embolism will increase the cost of hospitalization 32 . In this meta‐analysis, there was no significant difference in the incidence of DVT between the two groups. In most of the included studies, there is no detailed information on how to prevent venous thrombosis.
With the development of artificial joint technology, hemiarthroplasty is being used increasingly in unstable intertrochanteric fractures in the elderly; most of time the results are satisfactory 33 . The main reason is that artificial joint replacement can obtain anatomical, physiological, and stable joints 34 . Most of the elderly suffer from osteoporosis; internal fixation often can not achieve a stable fixation and can easily to lead to complications. Therefore, hemiarthroplasty has some advantages for unstable intertrochanteric fractures in the elderly: it can reduce postoperative complications, allows early weight‐bearing, and achieves a stable fixation. However, hemiarthroplasty has the disadvantages of potential enormous trauma, longer operation time, and greater intraoperative bleeding volume. The service life of prostheses is limited, which will increase the risk of reoperation.
Limitations of the Study
Only two RCT were included in the study; seven articles were non‐RCT. Moreover, surgeons have different clinical experience and use different techniques and the follow‐up time varies. The range of ages of the elderly in the studies is large and and they have different physical health conditions, which may lead to high heterogeneity. There are too few studies (<10) to make an adequate evaluation of publication bias. In future clinical studies, it is necessary to conduct a large sample, multicenter study on the therapeutic effects of internal fixation versus hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly, to draw more reliable conclusions.
Conclusion
Compared with internal fixation, the hemiarthroplasty group can carry out weight‐bearing training early and has reduced implant‐related complications, but the operation time is longer and intraoperative blood loss is greater. There is no difference in mortality, DVT, reoperation, length of hospital stay, and infection. Hemiarthroplasty may be a better choice for unstable intertrochanteric fractures in the elderly.
Disclosure: The authors have no potential conflicts of interest to disclose.
Contributor Information
Chao Xu, Email: docxuchao@126.com.
Xiao‐lin Shi, Email: xlshi-2002@163.com.
References
- 1. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury, 2018, 49: 1458–1460. [DOI] [PubMed] [Google Scholar]
- 2. Mazzucchelli Esteban R, Perez‐Fernandez E, Crespi‐Villarias N, et al Trends in osteoporotic hip fracture epidemiology over a 17‐year period in a spanish population: Alcorcon 1999‐2015. Arch Osteoporos, 2017, 12: 84. [DOI] [PubMed] [Google Scholar]
- 3. Bhattacharya A, Watts NB, Dwivedi A, Shukla R, Mani A, Diab D. Combined measures of dynamic bone quality and postural balance—a fracture risk assessment approach in osteoporosis. J Clin Densitom, 2016, 19: 154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Knobe M, Gradl G, Ladenburger A, Tarkin IS, Pape HC. Unstable intertrochanteric femur fractures: is there a consensus on definition and treatment in Germany?. Clin Orthop Relat Res, 2013, 471: 2831–2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Camurcu Y, Cobden A, Sofu H, et al What are the determinants of mortality after cemented bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients?. J Arthroplasty, 2017, 32: 3038–3043. [DOI] [PubMed] [Google Scholar]
- 6. Kumar P, Rajnish RK, Sharma S, Dhillon MS. Proximal femoral nailing is superior to hemiarthroplasty in ao/ota a2 and a3 intertrochanteric femur fractures in the elderly: a systematic literature review and meta‐analysis. Int Orthop, 2020, 44: 623–633. [DOI] [PubMed] [Google Scholar]
- 7. Li AB, Zhang WJ, Wang J, Guo WJ, Wang XH, Zhao YM. Intramedullary and extramedullary fixations for the treatment of unstable femoral intertrochanteric fractures: a meta‐analysis of prospective randomized controlled trials. Int Orthop, 2017, 41: 403–413. [DOI] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med, 2009, 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 9. Elhadi AS, Gashi YN. Unstable intertrochanteric fracture in elderly patients: outcome of primary cemented bipolar hemiarthroplasty versus internal fixation. SA Orthop J, 2018, 17: 22–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jolly A, Bansal R, More AR, Pagadala MB. Comparison of complications and functional results of unstable intertrochanteric fractures of femur treated with proximal femur nails and cemented hemiarthroplasty. J Clin Orthop Trauma, 2019, 10: 296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kayali C, Agus H, Ozluk S, Sanli C. Treatment for unstable intertrochanteric fractures in elderly patients: internal fixation versus cone hemiarthroplasty. J Orthop Surg, 2006, 14: 240–244. [DOI] [PubMed] [Google Scholar]
- 12. Kim JW, Shon HC, Song SH, Lee YK, Koo KH, Ha YC. Reoperation rate, mortality and ambulatory ability after internal fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: a study on korean hip fracture registry. Arch Orthop Trauma Surg, 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13. Kim SY, Kim YG, Hwang JK. Cementless calcar‐replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am, 2005, 87: 2186–2192. [DOI] [PubMed] [Google Scholar]
- 14. Kim YS, Hur JS, Hwang KT, Choi IY, Kim YH. The comparison of compression hip screw and bipolar hemiarthroplasty for the treatment of ao type A2 intertrochanteric fractures. Hip Pelvis, 2014, 26: 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Park BJ, Cho HM, Min WB. A comparison of internal fixation and bipolar hemiarthroplasty for the treatment of reverse oblique intertrochanteric femoral fractures in elderly patients. Hip Pelvis, 2015, 27: 152–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shen J, Wang DL, Chen GX, et al Bipolar hemiarthroplasty compared with internal fixation for unstable intertrochanteric fractures in elderly patients. J Orthop Sci, 2012, 17: 722–729. [DOI] [PubMed] [Google Scholar]
- 17. Zhou S, Liu J, Zhen P, et al Proximal femoral nail anti‐rotation versus cementless bipolar hemiarthroplasty for unstable femoral intertrochanteric fracture in the elderly: a retrospective study. BMC Musculoskelet Disord, 2019, 20: 500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cobden A, Camurcu Y, Duman S, Kocabiyik A, Kıs M, Saklavcı N. Mid‐term survivals of cemented calcar‐replacement bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients. Injury, 2019, 50: 2277–2281. [DOI] [PubMed] [Google Scholar]
- 19. Fan L, Dang X, Wang K. Comparison between bipolar hemiarthroplasty and Total hip arthroplasty for unstable intertrochanteric fractures in elderly osteoporotic patients. PLoS One, 2012, 7: e39531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang S, Liu Y, Yang T, Zou J, Yang H. Early clinical efficacy comparison study of Gamma3 nail, percutaneous compression plate (PCCP) and femoral head replacement (FHR) treatment on senile unstable intertrochanteric fractures. J Invest Surg, 2018, 31: 130–135. [DOI] [PubMed] [Google Scholar]
- 21. Kurmann A, Vorburger SA, Candinas D, Beldi G. Operation time and body mass index are significant risk factors for surgical site infection in laparoscopic sigmoid resection: a multicenter study. Surg Endosc, 2011, 25: 3531–3534. [DOI] [PubMed] [Google Scholar]
- 22. Wang Y, Cui H, Zhang D, Zhang P. Hospitalisation cost analysis on hip fracture in China: a multicentre study among 73 tertiary hospitals. BMJ Open, 2018, 8: e019147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yoo J, Lee JS, Kim S, et al Length of hospital stay after hip fracture surgery and 1‐year mortality. Osteoporos Int, 2019, 30: 145–153. [DOI] [PubMed] [Google Scholar]
- 24. Morri M, Ambrosi E, Chiari P, et al One‐year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep, 2019, 9: 18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement?. Clin Orthop Relat Res, 2001, 384: 189–197. [DOI] [PubMed] [Google Scholar]
- 26. Salpakoski A, Kallinen M, Kiviranta I, et al Type of surgery is associated with pain and walking difficulties among older people with previous hip fracture. Geriatr Gerontol Int, 2016, 16: 754–761. [DOI] [PubMed] [Google Scholar]
- 27. Iosifidis M, Iliopoulos E, Panagiotou A, Apostolidis K, Traios S, Giantsis G. Walking ability before and after a hip fracture in elderly predict greater long‐term survivorship. J Orthop Sci, 2016, 21: 48–52. [DOI] [PubMed] [Google Scholar]
- 28. Kuru T, Olcar HA. Effects of early mobilization and weight bearing on postoperative walking ability and pain in geriatric patients operated due to hip fracture: a retrospective analysis. Turk J Med Sci, 2020, 50: 117–125. [DOI] [PubMed] [Google Scholar]
- 29. Nie B, Wu D, Yang Z, et al Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: a meta‐analysis. Medicine, 2017, 27: e7446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Authen AL, Dybvik E, Furnes O, Gjertsen JE. Surgeon's experience level and risk of reoperation after hip fracture surgery: an observational study on 30,945 patients in the norwegian hip fracture register 2011‐2015. Acta Orthop, 2018, 89: 496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mula V, Parikh S, Suresh S, Bottle A, Loeffler M, Alam M. Venous thromboembolism rates after hip and knee arthroplasty and hip fractures. BMC Musculoskelet Disord, 2020, 21: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Trivedi NN, Sivasundaram L, Wang C, et al Chemoprophylaxis for the hip fracture patient: a comparison of warfarin and low‐molecular‐weight heparin. J Orthop Trauma, 2019, 33: 216–219. [DOI] [PubMed] [Google Scholar]
- 33. Cui Q, Liu YS, Li DF, et al Cemented hip hemiarthroplasty clinical observations on unstable intertrochanteric fracture in elderlies. Eur J Trauma Emerg Surg, 2016, 42: 651–656. [DOI] [PubMed] [Google Scholar]
- 34. Xie Y, Zhou H. Primary cemented hemiarthroplasty for unstable intertrochanteric fractures in elderly severe osteoporotic patients. Injury, 2020, 16: 34. [DOI] [PubMed] [Google Scholar]


