Abstract
Objective
To evaluate the clinical outcome of ankle arthrodesis with screw fixation through the transfibular approach for end‐stage ankle arthritis.
Methods
Data of 22 patients (28 ankles) with end‐stage ankle arthritis admitted to the Department of Orthopedics and Surgery of the First Hospital of Jilin University from May 2015 to December 2018 were analyzed retrospectively. The study included 9 men and 13 women, with a mean age of 56.86 ± 11.27 years (range, 37–75 years). The mean duration of the disease was 11.36 ± 12.80 years (range, 3 months‐50 years). A total of 16 patients had posttraumatic arthritis, 5 patients had osteoarthritis, and 1 patient had rheumatoid arthritis. There were 12 cases of the left ankle and 16 cases of the right ankle; 16 cases were unilateral and 6 were bilateral. The same surgical procedure was applied to all patients. Collected data included the operation time, intraoperative and postoperative blood loss, hospitalization time, bone union rate, time to bone union, and complications. The American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score and the visual analogue scale (VAS) were used to evaluate the preoperative status and the postoperative outcome at the last follow up.
Results
The mean follow‐up period was 26.14 ± 10.99 months. The mean operation time was 101.82 ± 33.33 min. The mean blood loss was 116.78 ± 68.86 mL during the procedure and 111.07 ± 52.18 mL after the procedure. The mean hospitalization time was 14.22 ± 5.42 days. Bone union of the ankle joint was achieved in all patients. The mean time to bone union was 14.83 ± 2.14 weeks. There was significant difference in the operation time between the patients undergoing unilateral and bilateral ankle arthrodesis. The AOFAS ankle hindfoot score increased from the preoperative value of 43.46 ± 4.39 points to 80.39 ± 5.37 points at the last follow up. During the same interval, the VAS score improved from 6.14 ± 0.80 points to 1.64 ± 0.73 points. The AOFAS ankle hindfoot score of patients who underwent unilateral ankle arthrodesis improved from the preoperative 43.19 ± 3.95 points to 81.75 ± 5.23 points at the last follow up, and the VAS score improved from 6.19 ± 0.83 points to 1.69 ± 0.70 points. The AOFAS ankle hindfoot score of patients undergoing bilateral ankle arthrodesis improved from the preoperative value of 43.83 ± 5.08 points to 78.67 ± 5.05 points at the last follow up, while the VAS score improved from 6.08 ± 0.82 points to 1.58 ± 0.79 points. There was significant difference in the maximum walking distance and walking on any surface between the patients undergoing unilateral and bilateral ankle arthrodesis. One patient developed superficial peroneal nerve palsy, which resolved within 1 year after the operation. In another patient, healing of the incision skin was delayed. During the follow‐up period, none of the patients developed an infection of the incision or local skin necrosis; screw loosening, withdrawal, or breakage did not occur in any patient.
Conclusion
The ankle arthrodesis with screw fixation through the transfibular approach provides satisfactory clinical outcomes for end‐stage ankle arthritis.
Keywords: End‐stage ankle arthritis, ankle arthrodesis, transfibular approach
Introduction
The ankle joint is composed of the tibia, the lower end of the fibula, and the talus pulley. It is one of the joints bearing the largest biomechanical load; it bears approximately 5 times the body weight during normal walking and up to 13 times the weight during running1. Ankle osteoarthritis (OA) is a chronic degenerative disease characterized by degeneration of the cartilage, subchondral osteosclerosis, periosteal osteophyte formation, and deformities of the joint. Worldwide, approximately 1% of people suffer from ankle OA2, 3. Ankle OA is caused mainly by traumatic factors which include repeated ankle sprains, intra‐ankle fractures, tibial plafond fracture, tibial shaft fracture, talus fracture, and cartilage injury of tibia and talus2, 3, 4. Other triggers of ankle OA are represented by rheumatoid arthritis, neuropathic arthritis, hemochromatosis, hemophilia, clubfoot, avascular talus necrosis, osteochondrosis dissecans, and postinfectious arthritis2. The type of treatment of ankle OA depends on the stage of this condition5. At present, the most commonly used ankle OA staging is the Tanaka modification of the Takakura staging6. It divides ankle OA into four stages ranging from mild to severe. Typically, stage 1 is defined as early, stages 2 and 3 as intermediate, and stage 4 as an end phase. Early and middle‐stage ankle OA is commonly addressed by conservative treatment and ankle‐sparing surgery. However, conservative treatment is not effective for the major clinical manifestations of end‐stage ankle OA, such as intractable pain, dyskinesia, and internal and external deformities of the ankle. These afflictions severely affect the patient’s quality of life, and surgery is currently the only available treatment option. The main types of surgery for end‐stage ankle OA are ankle arthrodesis and total ankle replacement7.
Ankle arthrodesis was introduced in 1878 when Eduard Albert treated a 14‐year‐old child suffering from severe lower limb paralysis by performing knee and ankle arthrodesis8. The purpose of this procedure is to relieve pain, correct deformities, and stabilize joints. Ankle arthrodesis has long been considered the gold standard for the treatment of end‐stage arthritis. With the continuous improvement of surgical techniques, a variety of surgical approaches and fixation methods have been developed. To date, more than 40 different arthrodesis methods have been reported7, 8, including open ankle arthrodesis, arthroscopic ankle arthrodesis, and mini‐open ankle arthrodesis. The approaches include anterior, lateral, posterior, transfibular, and mini‐arthrotomy approaches. The fixation methods include bone grafting, internal fixation, external fixation, or their combination. The internal fixation methods utilize a screw, a plate, and an intramedullary nail. The external fixation can be performed using the Ilizarov external fixator, Steinman pin fixation, a Taylor external fixator, or a Hoffman external fixator. Although all of these techniques have been shown to provide stability, a review of the existing literature indicates that the debate on the best method for ankle arthrodesis has not reached a consensus yet. Moreover, ankle arthrodesis has certain drawbacks, such as the loss of ankle motion, high complication rates, and diminished gait efficiency. Concern has also been raised that the elimination of tibiotalar motion accelerates adjacent joint degeneration due to the loss of a major motion segment. In addition, even in cases of successful arthrodesis, loss of normal ankle motion is found to negatively affect the functional status at long‐term follow up. Increased attention to the management of soft tissue and improved fixation methods has resulted in fewer complications, higher fusion rates, and more predictable pain relief.
Total ankle arthroplasty was first proposed by Richard Smith in the 1970s, and after more than 40 years of refining, it has become an option for the treatment of end‐stage ankle OA9. Although the ankle joint mobility is retained, the lifetime of the prosthesis is shorter. Total ankle arthroplasty is characterized by a high failure rate; in fact, the overhaul rate is as high as 32.9%–42%10, 11. With recent progress in the research on ankle joint biomechanics, prosthesis design, and simulation technology, the clinical outcomes of total ankle replacement are now adequate for the early and middle stages of the disease12. However, due to factors such as the type, price, and surgical technique of domestic artificial ankle prostheses, total ankle arthroplasty has not yet gained popularity in China.
Currently, unilateral ankle arthrodesis provides satisfactory clinical outcomes, but there are only a few reports on the bilateral procedure. Performing bilateral ankle arthrodesis is controversial because of associated problems, such as severe gait abnormality and bilateral loss of talocrural joint motion. To the best of our knowledge, the use of ankle arthrodesis with screw fixation through the transfibular approach in the treatment of bilateral ankle OA has never been reported. Therefore, the aims of this study were: (i) to evaluate the clinical effect of ankle arthrodesis with screw fixation through the transfibular approach for end‐stage ankle OA; (ii) to analyze the advantages of ankle arthrodesis with screw fixation through the transfibular approach, to identify possible surgical complications, and indicate methods for their prevention; and (iii) to determine whether the outcome of the patients undergoing bilateral ankle arthrodesis is comparable to that in patients undergoing the unilateral procedure.
Patients and Methods
Inclusion and Exclusion Criteria
The inclusion criteria followed the PICOS principle: (i) patients diagnosed with unilateral or bilateral end‐stage ankle arthritis; (ii) patients treated with unilateral or simultaneous bilateral ankle arthrodesis with screw fixation through the transfibular approach; (iii) preoperative and postoperative comparisons were made with measures including the American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score and the visual analog scale (VAS) and through comparison of unilateral and bilateral ankle arthrodesis, including the operation time, intraoperative and postoperative bleeding, hospitalization time, time to bone union, complications, and preoperative and postoperative AOFAS ankle hindfoot score and VAS; (iv) postoperative AOFAS ankle hindfoot score and VAS are significantly improved compared to preoperatively and there is no significant difference in expected results between patients who underwent unilateral and bilateral ankle arthrodesis; and (v) the study design was a retrospective study.
Exclusion criteria were patients with: (i) severe brain or organ damage; (ii) acute and chronic suppurative joint infection; (iii) ankle plantar flexion contracture caused by neuromuscular injury; (iv) severe osteoporosis; or (v) total necrosis of the talus.
General Information
The analysis included the data of 22 patients who underwent arthrodesis with screw fixation through the transfibular approach in the Department of Joint Surgery at our hospital, from May 2015 to December 2018. There were 9 men and 13 women, with a mean age of 56.86 ± 11.27 years (range, 37–75 years). Sixteen patients had posttraumatic arthritis, 5 patients had osteoarthritis, and 1 patient had rheumatoid arthritis. There were 16 unilateral and 6 bilateral cases, for a total of 28 ankles, which included 12 cases of left ankles and 16 cases of right ankles. The mean height was 166 ± 0.52 cm (range, 155–175 cm). The mean weight was 62.59 ± 3.76 kg (range, 55–68 kg). The mean body mass index (BMI) was 22.71 ± 0.92 kg/m2 (range, 20.32–24.31 kg/m2). The mean duration of the disease was 11.36 ± 12.80 years (range, 3 months‐50 years). In addition, in this study all patients were divided into unilateral ankle arthrodesis and bilateral ankle arthrodesis groups. Those in the bilateral ankle arthrodesis group underwent bilateral simultaneous ankle arthrodesis.
Preoperative Preparation
All patients underwent X‐ray and CT imaging before the surgery to evaluate the degree of ankle joint disease, the change in the force line, the adjacent joint, and the disease of the temporomandibular joint.
Surgical Procedure
Anesthesia and Position
The surgery was performed under general or spinal anesthesia. The patient was placed in a supine position, the balloon of the proximal thigh tourniquet was inflated, the drapes were disinfected, and the hip and lower limbs on the affected side were raised so that the toes pointed upward.
Transfibular Approach and Exposure
A longitudinal skin incision was made, starting 10 cm proximal to the tip of the lateral malleolus and continuing along the posterior border of the fibula in a distal direction. At the level of the tip of the lateral malleolus, the incision continued in an anterior direction toward the base of the fourth metatarsus and ended at the level of the cuboid (Fig. 1). Subperiosteal dissection was performed to expose the distal fibula to the lateral malleolus. At a distance of 6–7 cm from the distal end of the fibula, a pendulum saw was used to cut off the oblique fibula and remove the distal end of the fibula (Fig. 2). The lower tibiofibular union was cleaned up, the external sides of the distal tibia and talus were uncovered, and the tibiotalar joint was exposed with the help of a spreader. Next, the osteophyte was cleaned up and the articular cartilage was removed with a cartilage shovel. The distal end of the fibula was split in the coronal plane, and the cancellous bone was removed completely and trimmed into cancellous bone particles, which were used for bone grafting of the tibiotalar joint.
Figure 1.

An anterolateral longitudinal incision of the distal fibula turning to the base of the fourth metatarsal. The incision length is approximately 10 cm.
Figure 2.

Excised segment of the fibula. The osteotomy was performed 6 to 7 cm from the distal tip.
Tibia and Talus Osteotomy
In the osteotomy, the length of the tibia was be kept as long as possible, and the thin layer of subchondral bone at the top of ankle point was removed so that the medial end was situated at the corner of internal ankle point, 10 mm short of the medial tibial cortex, to prevent an accidental osteotomy of the medial malleolus. The talus osteotomy was performed parallel to the tibial osteotomy surface, forming a smooth cancellous bone surface (Fig. 3), and the 4.0‐mm Kirschner wire was used to drill evenly on the articular surface. The lamina spreader was used to expand the operation field, the cartilage surface of the medial space of ankle joint was scraped further, and the joint capsule and surrounding fibrous tissue were completely loosened.
Figure 3.

Osteotomy of the cartilage at the distal tibia and proximal talus.
Fixation and Reconstruction
To adjust the tibiotalar position, the ankle joint was placed in the position of 0° flexion and extension, 5° valgus, and 10° external rotation. The talus was moved back so that the front edge of the talus joint corresponded to the front cortex of the tibia. In cases of limb shortening of up to 2 cm caused by tibial distance osteotomy, the fibula and the entire plate of the autogenous iliac bone were used for bone grafting. Temporary fixation of the tibia and talus was accomplished with Kirschner wire under fluoroscopy after achieving a satisfactory force line (Fig. 4). The fixation was performed using two or three 7.3 × 60 mm headless compression full‐thread hollow screws. The first screw was driven from the outside of the tibia into the anteromedial talus process and the second from the posterolateral process of the talus into the anterior medial portion of the tibia. The fibula was fixed to the tibia and talus with three or four 3.5 × 34 mm cortical screws (Fig. 5). After the surgery, a drainage tube was placed, the surgical incision was closed using the conventional method, and a U‐shaped plaster was fixed.
Figure 4.

Use of the Kirschner wire to temporarily fix the tibiotalar joint.
Figure 5.
Under the guidance of the C‐arm X‐ray machine, the tibiofibular joint was fixed with two headless full‐thread hollow screws, and the fibula was fixed to the tibia and talus with four cortical bone screws.
Postoperative Treatment
Postoperative anti‐infective treatment was provided for 3–5 days, and the drainage tube was removed 48 h after the surgery. Positive and lateral radiographs of the ankle were performed and evaluated 1 week after the procedure. Two weeks postsurgery, the sutures were removed, and the U‐shaped plaster was replaced with a short tubular plaster to limit ankle movement and prevent failure of internal fixation. Weight bearing was avoided for 6 weeks after the operation. Partial weight‐bearing walking was allowed after 6 weeks.
Clinical and Radiological Evaluation
The operation time, intraoperative and postoperative bleeding, hospitalization time, bone union rate, time to bone union, and complications were recorded. The AOFAS ankle hindfoot score and the VAS score were used to evaluate the preoperative status and postoperative outcome at the last follow up.
American Orthopedic Foot and Ankle Society Ankle Hindfoot Scores
The AOFAS ankle hindfoot Score is among the most commonly used instruments for measuring the outcome of treatment in patients who have sustained a complex ankle or hindfoot injury. The AOFAS hindfoot score system includes primarily nine aspects: pain, function, maximum walking distance (blocks), walking surfaces, gait abnormality, sagittal motion (flexion plus extension), hindfoot motion (inversion plus eversion), ankle‐hindfoot stability (anteroposterior, varus–valgus), and alignment. The maximum value of the AOFAS ankle hindfoot score is 100 points, but it reaches only 92 points in ankle arthrodesis patients due to the limited range of ankle motion. A score of 80–92 was considered an excellent result, 70–79 a good result, 60–69 a fair result, and less than 60 a poor result13.
Visual Analogue Scale
Ankle pain is an important sign and a frequent patient complaint. A self‐reported score on the 10‐point visual analog scale (VAS) was used for the assessment of patients’ pain. A minimum of 0 indicates no pain. A score of 1–3 indicates mild pain, with the sleep quality of patients not affected; 4–6 indicates moderate pain, with sleep quality affected; 7–10 indicates severe pain, with patients not able to sleep due to pain; the maximum value is 10.
Radiographic Evaluation
All patients were examined at 6 weeks, 12 weeks, 6 months and 12 months after the surgery and every year thereafter through the outpatient service. X‐ray images of the ankle joint were taken to assess the fusion of the ankle joint. Complete weight‐bearing walking was permitted depending on the X‐ray or CT results. Follow‐up exams were conducted every 6 months after the completion of the bone union. Union was judged to have occurred when trabeculae could be seen crossing the joint line on plain radiographs or CT, together with the presence of a pain‐free, clinically united joint. Delayed union was defined as union taking longer than 6 months. Non‐union was defined as no evidence of fusion on CT at 12 months postoperatively.
Statistical Analysis
SPSS Statistics 19.0 software (IBM SPSS, Chicago, IL, USA) was used for all statistical analyses. The Shapiro–Wilk test was used to determine whether the measurement data were normally distributed, as well as the operation time, intraoperative and postoperative bleeding, hospitalization time, time to bone union, age, follow‐up time, AOFAS ankle hindfoot score, and VAS score. The homogeneity of variance was expressed as mean ± standard deviation. A comparison between the unilateral and bilateral ankle arthrodesis was performed using the t‐test with two independent samples. Categorical variables such as gender and etiology were expressed as absolute values and percentages, and the χ2‐test and Fisher’s exact test were used to compare the data between the unilateral and bilateral ankle arthrodesis groups. A 5% significance level was applied for all tests (P < 0.05).
Results
Follow‐up
All patients were examined at 6, and 12 weeks, and 6 and 12 months, after the surgery and every year thereafter through the outpatient service. The mean follow‐up time was 26.14 ± 10.99 months (range, 12–54 months). The mean follow‐up times of the unilateral and bilateral ankle arthrodesis groups were 24.68 ± 8.60 months (range, 15–37 months) and 29.83 ± 16.38 months (range, 12–54 months), respectively (P = 0.491).
General Results
There were 22 patients in this study, including 16 patients with unilateral ankle arthrodesis and 6 patients with bilateral ankle arthrodesis. Basic information for patients with unilateral and bilateral ankle arthrodesis is listed in Table 1. The mean duration of the surgery was 101.82 ± 33.33 min (range, 65–175 min). Mean blood loss was 116.78 ± 68.86 mL (range, 50–300 mL) during the operation and 111.07 ± 52.18 mL (range, 50–260 mL) after the operation. The average hospitalization time was 14.22 ± 5.42 days (range, 8–30 days). The perioperation information of patients in the unilateral and bilateral ankle arthrodesis groups is listed in Table 2. The mean duration of surgery of the bilateral ankle arthrodesis group is significantly longer than that of the unilateral ankle arthrodesis group (150.83 ± 16.86 min vs 83.44 ± 11.79 min, P < 0.001).
Table 1.
Basic information on patients in the unilateral and bilateral ankle arthrodesis group
| Variable | Unilateral (n = 16) | Bilateral (n = 6) | χ2/t | P‐value |
|---|---|---|---|---|
| Age (years) | 56.75 ± 12.13 | 57.17 ± 9.62 | −0.835 | 0.940 |
| Male sex (n, %) | 8, 50% | 1,16.7% | 2.006 | 0.157 |
| Height (cm) | 165.94 ± 5.67 | 166.17 ± 4.26 | −0.09 | 0.930 |
| Weight (kg) | 62.37 ± 3.86 | 63.17 ± 3.76 | −0.431 | 0.671 |
| BMI (kg/m2) | 22.65 ± 0.91 | 22.87 ± 0.99 | −4.87 | 0.631 |
| Etiology OA/PA (n, %) | 16, 100% | 5, 83.3% | 2.794 | 0.095 |
| Duration of the disease (years) | 10.61 ± 14.33 | 13.38 ± 7.71 | −0.603 | 0.552 |
| Follow‐up time (months) | 24.68 ± 8.60 | 29.83 ± 16.38 | −0.733 | 0.491 |
BMI, body mass index; OA, osteoarthritis; PA, posttraumatic arthritis
Table 2.
Perioperation information of patients in the unilateral and bilateral ankle arthrodesis groups (mean ± SD)
| Variable | Unilateral (n = 16) | Bilateral (n = 6) | t | P‐value |
|---|---|---|---|---|
| Duration of the surgery (min) | 83.44 ± 11.79 | 150.83 ± 16.86 | −10.632 | 0.00* |
| Blood loss during the operation (mL) | 126.25 ± 80.57 | 104.17 ± 49.81 | 0.835 | 0.411 |
| Blood loss after the operation (mL) | 120.0 ± 55.65 | 99.17 ± 46.80 | 1.047 | 0.305 |
| Hospitalization time (days) | 13.56 ± 5.48 | 16.0 ± 5.29 | −0.938 | 0.360 |
*Statistically significant
American Orthopedic Foot and Ankle Society Ankle Hindfoot Scores
The AOFAS ankle hindfoot score increased from the preoperative value of 43.46 ± 4.39 points to 80.39 ± 5.37 points at the last follow up, and significant difference existed between them (t = −26.833, P < 0.001). Excellent results were obtained in 17 of the 28 cases, and good results in 11 cases. The mean values of preoperative and postoperative AOFAS ankle hindfoot scores of patients in the unilateral and bilateral ankle arthrodesis groups are listed in Tables 3 and 4. There were no significant differences in these values between patients undergoing unilateral and bilateral procedures. However, in daily activities, such as climbing stairs or slopes and walking long distances, patients who received bilateral ankle arthrodesis scored lower than those treated with unilateral arthrodesis. Significant differences were also present in maximum walking distance (4.31 ± 0.79 points vs 3.17 ± 1.27 points, P = 0.013) and walking on any surface (3.50 ± 0.89 points vs 1.50 ± 1.57 points, P = 0.001).
Table 3.
Preoperative American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score and visual analogue scale (VAS) score between patients with unilateral and bilateral ankle arthrodesis group (mean ± SD)
| Characteristic | Unilateral | Bilateral | P‐value |
|---|---|---|---|
| Pain | 17.50 ± 6.83 | 18.33 ± 5.77 | 0.736 |
| Activity limitations | 2.00 ± 2.07 | 1.67 ± 2.06 | 0.676 |
| Maximum walking distance | 2.38 ± 1.68 | 1.83 ± 1.03 | 0.331 |
| Walking on any surface | 2.25 ± 1.34 | 2.00 ± 1.47 | 0.644 |
| Gait abnormality | 3.00 ± 1.78 | 2.33 ± 2.06 | 0.369 |
| Sagittal motion | 1.75 ± 2.05 | 2.33 ± 2.06 | 0.464 |
| Hindfoot motion | 4.88 ± 1.50 | 5.00 ± 1.48 | 0.828 |
| Ankle‐hindfoot stability | 1.00 ± 2.73 | 2.00 ± 3.62 | 0.412 |
| Alignment | 8.44 ± 2.39 | 8.33 ± 2.46 | 0.911 |
| Total score | 43.19 ± 3.95 | 43.83 ± 5.08 | 0.708 |
| VAS | 6.19 ± 0.83 | 6.08 ± 0.82 | 0.741 |
VAS, visual analogue scale
Table 4.
Postoperative American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score, visual analogue scale (VAS) score, and bone union time between patients with unilateral and bilateral ankle arthrodesis (mean ± SD)
| Characteristic | Unilateral | Bilateral | P‐value |
|---|---|---|---|
| Pain | 36.88 ± 4.79 | 38.33 ± 3.89 | 0.397 |
| Activity limitations | 8.88 ± 1.50 | 7.59 ± 2.15 | 0.057 |
| Maximum walking distance | 4.31 ± 0.79 | 3.17 ± 1.27 | 0.013* |
| Walking on any surface | 3.50 ± 0.89 | 1.50 ± 1.57 | 0.001* |
| Gait abnormality | 5.50 ± 2.00 | 5.33 ± 1.97 | 0.828 |
| Hindfoot motion | 4.69 ± 1.54 | 4.75 ± 1.55 | 0.916 |
| Ankle‐hindfoot stability | 8.0 ± 0.0 | 8.0 ± 0.0 | 1 |
| Alignment | 10.0 ± 0.0 | 10.0 ± 0.0 | 1 |
| Total score | 81.75 ± 5.23 | 78.67 ± 5.05 | 0.124 |
| VAS | 1.69 ± 0.70 | 1.58 ± 0.79 | 0.717 |
| Bone union time (weeks) | 15.13 ± 2.28 | 14.83 ± 1.70 | 0.713 |
*Statistically significant
Visual Analogue Scale
The VAS score improved from 6.14 ± 0.80 points to 1.64 ± 0.73 points. Postoperative VAS scores were markedly improved in comparison with the preoperative values, and the difference was statistically significant (t = 23.812, P < 0.001). The mean values of preoperative and postoperative VAS score of patients with unilateral and bilateral ankle arthrodesis are listed in Tables 3 and 4. There were no significant differences in VAS score between patients undergoing unilateral and bilateral procedures.
Radiographic Evaluation Results
Bone union of the ankle joint was achieved in all patients, and in all 28 ankles subjected to arthrodesis, the bone union rate was 100%. The mean time to bone union was 14.83 ± 2.14 weeks (range, 12–21 weeks). The mean time to bone union of patients with unilateral and bilateral ankle arthrodesis is listed in Table 4. There were no significant differences in time to bone union between patients undergoing unilateral and bilateral procedures. In all patients, the tibia and talus were fixed firmly with headless compression full‐thread hollow screws and the fibula was firmly fixed to the tibia and talus, without screw loosening, withdrawal, or breakage. Typical cases are shown in Figs 6 and 7.
Figure 6.
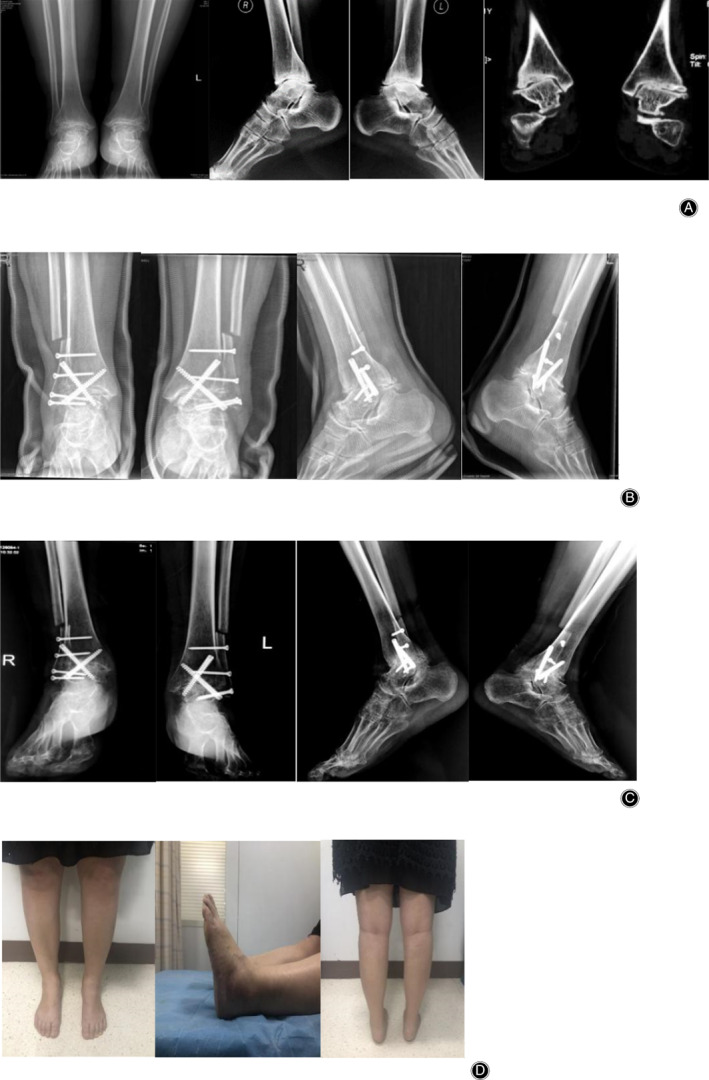
Female patient, 51 years old, with bilateral ankle osteoarthritis (OA). Ankle arthrodesis was performed with screw fixation through the transfibular approach. (A) X‐ray and CT of bilateral ankle before surgery. (B) X‐ray of ankle joint 6 weeks after surgery. (C) Ankle X‐ray 1 year after surgery. (D) Outward observation of ankle 1 year after the surgery. The American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score improved significantly after surgery, and the patient expressed satisfaction with the outcome.
Figure 7.

Male patient, 42 years old, with post‐traumatic osteoarthritis of the left ankle. Ankle arthrodesis was performed with screw fixation through the transfibular approach. (A) X‐ray of ankle joint before surgery. (B) X‐ray of ankle joint 6 weeks after surgery. (C) X‐ray of ankle joint 1 year after surgery. The American Orthopedic Foot and Ankle Society (AOFAS) ankle hindfoot score improved significantly after surgery, and the patient expressed satisfaction with the outcome.
Intraoperative Recommendations
When cleaning up the articular surface, the osteophyte on the medial side of the talus should be removed as much as possible; otherwise, it will lead to a forward positioning of the talus and affect the optimal position of the ankle joint. The spreader was used to expand the osteophyte on the medial side of the talus. For the patients with more osteophyte on the medial side of the talus, a medial incision can be performed to clean up the osteophyte on the medial side.
Care should be taken when drilling the articular surface, because the drill may penetrate the subchondral bone and damage the tibia and talus, particularly in patients with osteoporosis.
The tibia and talus should be in a vertical position during osteotomy. The vertical orientation is difficult to judge by the naked eye, and excessive osteotomy may result in limb shortening or ankle joint varus and valgus. Kirschner wire can be used to assist in judging whether the direction of the osteotomy is vertical. In addition, the best positions of the talus and tibia can be fixed by Kirschner wire. Intraoperative fluoroscopy can help to achieve the best fixation position.
Complications
One patient developed superficial peroneal nerve palsy after the surgery, manifested predominantly as numbness and pain on the lateral calf and back of the foot, and a marked decrease in sensation when touched. This condition resolved 1 year after the operation with the use of neurotrophic drugs. Healing of the incision skin was delayed in another patient, which resolved within 1 month after the operation with continuous dressing change.
Discussion
Summary of the Major Results of the Study
The primary aim of this study was to evaluate the clinical effect of ankle arthrodesis with screw fixation through the transfibular approach for end‐stage ankle OA. In comparison with the preoperative values, postoperative AOFAS ankle hindfoot scores and VAS scores were markedly improved. In this single‐surgeon series, a 100% bone union rate with a 7.1% overall complications rate was achieved in 22 patients (28 ankles), showing that ankle arthrodesis with screw fixation through the transfibular approach provides satisfactory clinical outcomes for end‐stage ankle OA. This procedure ensures a high bone union rate and strong stability, eliminates ankle pain, corrects the deformity, and significantly improves ankle function. The postoperative AOFAS ankle hindfoot score and the VAS score in patients undergoing bilateral ankle arthrodesis were not significantly different from those in patients undergoing the unilateral procedure.
Advantages of Ankle Arthrodesis with Screw Fixation through the Transfibular Approach
Successful ankle arthrodesis depends on a proper surgical approach, fixation with a tight compression, proper limb force lines, and a good bone union by achieving broad, flat cancellous surfaces placed in apposition13, 14. The advantages of ankle arthrodesis with screw fixation through the transfibular approach are analyzed below.
Transfibular Approach
Horwitz (1942) was the first to describe a transfibular approach to ankle fusion that used the fibula as an additional source of stabilization of the fusion construct15. Later, Holt and coworkers16 modified the transfibular ankle arthrodesis by using a fibular‐onlay strut graft combined with rigid internal fixation. The transfibular approach can fully expose the joints, completely remove cartilage and sclerotic bone, and facilitate the correction of varus and valgus deformities of the foot. In addition, the transfibular approach retains subchondral bone, reduces limb shortening, and ensures a wide contact area and good stability17. Arthroscopic ankle arthrodesis shortens the length of surgery and hospitalization, and reduces postoperative complications. The union rate is not significantly different from that of open ankle arthrodesis 18, 19. However, with this technique, the scope of arthroscopic treatment of joints is limited, the rectifying ability is not as good as that of open surgery, and the correction of severe deformities is challenging. Compared with the soft tissue encountered in the anterior incision of the ankle, the lateral soft tissue of the ankle is thicker, reducing the incidence of complications such as incision infection, dehiscence, and delayed healing17. Moreover, the risk of intraoperative nerve damage is low with the transfibular approach18. In addition, this technique ensures good condition of the soft tissue in front of the ankle, making future total ankle replacement more feasible20.
Autologous bone graft, harvested from the fibula21, can facilitate bone union. Autologous graft bone can be obtained from the inside of the fibula. In addition, Ieong and collaborators21 described a safe and effective method of osteotomy to obtain a structural bone graft. In this protocol, the osteotomy is performed with an inclination of approximately 30° at an interval of 2–3 mm at the distal fibula. In a manner similar to the fracture healing process, the osteotomy provides sufficient blood supply to the arthrodesis surface and improves the union rate14, 20. However, this approach requires additional screws to fix the severed fibula. Biomechanical experiments have documented that a screw‐fixed fibula functions as a stable support structure, similarly to the lateral compression steel plate, counteracting internal and external rotation and improving the stability of the ankle joint22. In addition, the distal fibula maintains the shape of the original ankle joint, improving patient satisfaction20.
Screw Fixation
Tight compression fixation is critical for successful ankle arthrodesis14, 20. The types of fixation of ankle arthrodesis can be divided into internal and external fixation. Internal fixation is most commonly used because it provides good stability and a compression effect. Internal fixation requires screws, steel plates, and a retrograde intramedullary screw. Screw fixation is most frequently used for internal fixation due to its high stability, maintenance of the normal shape of the ankle joint, and preservation of the equal length of lower limbs7. In the published literature, arthrodesis through the trainsfibular approach has demonstrated satisfactory bone fusion rates13, 14, 17, 23, 24, 25, 26 (Table 5). In the present study, two or three 7.3 × 60 mm headless compression full‐threaded cannulated screws were used to cross‐fix the tibiotalar joint, and three or four 3.5 × 34 mm cortical screws were used to fix the fibula to the tibia and talus. As a new type of internal fixation screw, a headless compression hollow screw is designed to have the mechanical characteristics of taper, full thread, and thread pitch change, which can continuously compress the tibia and talus, promoting the healing of bone and enhancing the stability of the joint complex. In addition, the headless design eliminates the need for conventional countersunk head treatment. Hollow screws are more resistant to bending than cancellous screws. A hollow screw could be easily inserted under the guidance of real‐time radiography using a guide pin, and accurately fixed in the required position. This approach ensured that a strong union was achieved in all cases.
Table 5.
Published studies involving more than 20 patients reporting on arthrodesis with screw fixation through the transfibular approach with different types and numbers of screws, and different directions of implantation
| Author, reference number, year | Number of patients | Screw type and size | Screw direction | Union rate (%) | Mean AOFAS |
|---|---|---|---|---|---|
| Fluckiger and Weber 23 | 19 (20 ankles) |
3, 4.5, or 6.5‐mm lag screws, cannulated 6.5‐mm screw Two 3.5‐mm cortical screws. |
Cross | 100 | 78.5 |
| Colman and Pomeroy (2007)24 | 48 |
Three 6.5‐mm compression screws Two 6.5‐mm compression screws |
Cross | 96 |
High‐risk group: 74 low‐risk group: 69 |
| Akra et al. (2010)14 | 25 (26 ankles) |
Two partially threaded cancellous bone screws Two to four parallel lag screws |
Parallel from the lateral tibia to the medial talus | 100 | NA |
| Napiontek and Jaszczak (2015)25 | 23 |
Two 6.3‐mm or 7.0‐mm cannulated screws Two cortical screws |
Parallel from the lateral talus to the medial tibia | 95.7 | 76 |
| Lee et al. (2016)26 | 23 |
Two partially threaded 7.0‐mm cannulated screws Two fully threaded 3.5‐mm cannulated screws |
Parallel from the lateral talus to the posteromedial tibia | 92 | 71 |
| Balaji et al. (2017)13 | 29 |
Two 6.5‐mm × 16‐mm cancellous screws Two 4.5‐mm cortical screws |
Cross 45° | 100 | 74 |
| Kim et al. 17 | 22 |
Two 7.0‐mm hollow screws Two 3.5‐mm cortical screws |
Cross | 95.5 | 60.7 |
AOFAS, American Orthopedic Foot and Ankle Society; NA, not available
Ankle Force Line
A proper ankle force line is critical for postoperative ankle function and prevention of complications. Ideal alignment includes a neutral ankle flexion, 0–5° of valgus, and neutral to a slight external rotation position. Intraoperative position, incision exposure range, osteotomy angle, and the ability to assess the perspective image after temporary fixation all affect the final angle and position of arthrodesis. In ankle alignment, the varus and talus being placed forward should be avoided, because this results in domed gait and knee joint pain. Mild valgus can facilitate the dispersion of stress and maximize the compensatory ability of subtalar and transverse tarsal joints. For tibial osteotomy, the axis of the tibia should be vertical to avoid multiple osteotomies and unnecessary bone loss.
Surgical Complications and Prevention
In the current study, 1 patient with severe deformity of an old ankle fracture suffered from poor healing of the incision due to the contracture of the soft tissue around the lateral malleolus and poor blood supply around the surgical margin. The dressing was changed daily through the incision, and the incision finally healed 1 month after the surgery. Therefore, the skin and blood circulation of patients should be evaluated before the operation. For patients with old surgical scars, smoking history, diabetes, skin disease, and other diseases impacting the healing of the incision, an active adjustment should be made before the operation. In addition, the anterior tibial artery and its branches may be injured by the transfibular approach. Therefore, attention should be paid to avoid injury of blood vessels during the procedure. Another patient experienced damage to the superficial peroneal nerve, and the symptoms resolved within 1 year after surgery through the use of neurotrophic drugs. Using the transfibular approach may damage the superficial peroneal nerve due to several risk factors, such as the proximity of its intermediate branch and the deep peroneal nerve to the interosseous membrane, and its highly variable course27. The superficial peroneal nerve should be protected during surgery. During the follow‐up period, none of the patients developed an infection of the incision or local skin necrosis; loosening, withdrawal, or breakage of the screws also did not occur.
Bilateral Ankle Arthrodesis
Currently, unilateral ankle arthrodesis provides good clinical outcomes but there are only a few reports on the bilateral procedure. Houdek and coworkers28 analyzed the ankle function and radiological results in 31 patients who underwent bilateral ankle arthrodesis. The mean follow‐up time was 11.2 years. Although most patients had adjacent arthritis at the last follow up, the ankle function was adequate. From the preoperative evaluation to 2, 5, and 10 years postsurgery, the improvement in the AOFAS ankle hindfoot score of the bilateral ankle joints was significant, despite a downward trend between 2 and 10 years after the surgery. At 10 years, the foot and ankle ability were close to normal in 71% of the patients. Vaughan and collaborators29 reported 8 patients who underwent bilateral ankle arthrodesis, with a median follow‐up time of 58.5 months. At the last evaluation, the median AOFAS ankle hindfoot score was 79.5, and the patient satisfaction rate was 87.5%. Henricson and colleagues30 performed 35 bilateral ankle arthrodesis procedures, with a mean follow‐up period of 47 months. The patients were satisfied or very satisfied with the outcomes for 64 of the 70 ankles (91%). Maenoharay and coworkers31 analyzed 20 patients with ankle arthrodesis, including 10 patients with bilateral and 10 patients with unilateral surgery, and used the Japanese Society for Surgery of the Foot (JSSF) scale and the Self‐Managed Foot Evaluation Questionnaire (SAFE‐Q) to evaluate clinical results. Except for the social function in SAFE‐Q, the scores of patients with bilateral ankle arthrodesis were significantly lower than in patients with unilateral ankle arthrodesis. The other scoring items proved that there was no significant difference in the clinical effect of unilateral and bilateral ankle arthrodesis. The current study did not identify significant differences in the AOFAS ankle hindfoot score and VAS score between unilateral and bilateral ankle arthrodesis. However, in daily activities, such as climbing stairs or slopes and walking long distances, patients who received bilateral ankle arthrodesis scored lower than those treated with unilateral arthrodesis. Therefore, we conclude that bilateral ankle arthrodesis represents an acceptable treatment for bilateral end‐stage ankle arthritis.
Limitations of the Study
The study included a small number of patients, was designed as a retrospective analysis, and did not include a comparison with other internal fixation methods. In addition, the follow‐up time was short. Due to these factors, the conclusion reached may be biased. A prospective clinical study is planned to compare the efficacy of arthrodesis performed using screw fixation through the transfibular approach with other techniques. To compare the difference between unilateral and bilateral ankle arthrodesis, more patients will be included. We will continue to follow up medium‐term and long‐term clinical effects of ankle arthrodesis with screw fixation through the transfibular approach.
Conclusion
The ankle arthrodesis with screw fixation through the transfibular approach provides satisfactory clinical outcomes for end‐stage ankle arthritis.
Acknowledgments
This work was supported by the Science and Technology Department of Jilin Province (grant number 20190304039YY) and the Health Technology Innovation Project of Jilin Province (grant number 2018J054).
Disclosure:The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest. All authors agree to the content of the manuscript. The content has not been published or submitted for publication elsewhere, except as a brief abstract in the proceedings of two scientific meetings.
References
- 1. Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma, 2016, 30: 232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res, 2009, 467: 1800–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomas AC, Hubbard‐Turner T, Wikstrom EA, Palmieri‐Smith RM. Epidemiology of posttraumatic osteoarthritis. J Athl Train, 2017, 52: 491–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delco ML, Kennedy JG, Bonassar LJ, Fortier LA. Post‐traumatic osteoarthritis of the ankle: a distinct clinical entity requiring new research approaches. J Orthop Res, 2017, 35: 440–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu Y. Treatment options of ankle osteoarthritis by stage. Zhonghua Yi Xue Za Zhi, 2019, 99: 1608–1610. [DOI] [PubMed] [Google Scholar]
- 6. Tanaka Y, Takakura Y, Hayashi K, Taniguchi A, Kumai T, Sugimoto K. Low tibial osteotomy for varus‐type osteoarthritis of the ankle. J Bone Joint Surg Br, 2006, 88: 909–913. [DOI] [PubMed] [Google Scholar]
- 7. Yasui Y, Hannon CP, Seow D, Kennedy JG. Ankle arthrodesis: a systematic approach and review of the literature. World J Orthop, 2016, 7: 700–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zwipp H, Rammelt S, Endres T, Heineck J. High union rates and function scores at midterm followup with ankle arthrodesis using a four screw technique. Clin Orthop Relat Res, 2010, 468: 958–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shane A, Sahli H. Total ankle replacement options. Clin Podiatr Med Surg, 2019, 36: 597–607. [DOI] [PubMed] [Google Scholar]
- 10. Gramlich Y, Neun O, Klug A, et al Total ankle replacement leads to high revision rates in post‐traumatic end‐stage arthrosis. Int Orthop, 2018, 42: 2375–2381. [DOI] [PubMed] [Google Scholar]
- 11. Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br, 2011, 93: 293–297. [DOI] [PubMed] [Google Scholar]
- 12. Barg A, Wimmer MD, Wiewiorski M, Wirtz DC, Pagenstert GI, Valderrabano V. Total ankle replacement. Dtsch Arztebl Int, 2015, 112: 177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Balaji S, Selvaraj V, Devadoss S, Devadoss A. Transfibular ankle arthrodesis: a novel method for ankle fusion ‐ a short term retrospective study. Indian J Orthop, 2017, 51: 75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Akra GA, Middleton A, Adedapo AO, Port A, Finn P. Outcome of ankle arthrodesis using a transfibular approach. J Foot Ankle Surg, 2010, 49: 508–512. [DOI] [PubMed] [Google Scholar]
- 15. Horwitz T. The use of the transfibular approach in arthrodesis of the ankle joint. Am J Surg, 1942, 55: 550–552. [Google Scholar]
- 16. Holt ES, Hansen ST, Mayo KA, Sangeorzan BJ. Ankle arthrodesis using internal screw fixation. Clin Orthop Relat Res, 1991, 268: 21–28. [PubMed] [Google Scholar]
- 17. Kim JG, Ha DJ, Gwak HC, et al Ankle arthrodesis: a comparison of anterior approach and transfibular approach. Clin Orthop Surg, 2018, 10: 368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yasui Y, Vig KS, Murawski CD, Desai P, Savage‐Elliott I, Kennedy JG. Open versus arthroscopic ankle arthrodesis: a comparison of subsequent procedures in a large database. J Foot Ankle Surg, 2016, 55: 777–781. [DOI] [PubMed] [Google Scholar]
- 19. Townshend D, Di Silvestro M, Krause F, et al Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Joint Surg Am, 2013, 95: 98–102. [DOI] [PubMed] [Google Scholar]
- 20. Sung W, Greenhagen RM, Hobizal KB, Burns PR, Wukich DK. Technical guide: transfibular ankle arthrodesis with fibular‐onlay strut graft. J Foot Ankle Surg, 2010, 49: 566–570. [DOI] [PubMed] [Google Scholar]
- 21. Ieong E, Mahapatra P, Nathan S. Fashioning autologous bone graft from the fibula in the transfibular approach to open ankle arthrodesis. Foot Ankle Surg, 2014, 20: 149–150. [DOI] [PubMed] [Google Scholar]
- 22. Thordarson DB, Markolf KL, Cracchiolo AR. Arthrodesis of the ankle with cancellous‐bone screws and fibular strut graft. Biomechanical analysis. J Bone Joint Surg Am, 1990, 72: 1359–1363. [PubMed] [Google Scholar]
- 23. Fluckiger G, Weber M. The transfibular approach for ankle arthrodesis. Oper Orthop Traumatol, 2005, 17: 361–379. [DOI] [PubMed] [Google Scholar]
- 24. Colman AB, Pomeroy GC. Transfibular ankle arthrodesis with rigid internal fixation: an assessment of outcome. Foot Ankle Int, 2007, 28: 303–307. [DOI] [PubMed] [Google Scholar]
- 25. Napiontek M, Jaszczak T. Ankle arthrodesis from lateral transfibular approach: analysis of treatment results of 23 feet treated by the modified Mann's technique. Eur J Orthop Surg Traumatol, 2015, 25: 1195–1199. [DOI] [PubMed] [Google Scholar]
- 26. Lee HJ, Min WK, Kim JS, Yoon SD, Kim DH. Transfibular ankle arthrodesis using burring, curettage, multiple drilling, and fixation with two retrograde screws through a single lateral incision. J Orthop Surg (Hong Kong), 2016, 24: 101–105. [DOI] [PubMed] [Google Scholar]
- 27. Yassin M, Garti A, Khatib M, et al The utility and limitations of the transfibular approach in ankle trauma surgery. Case Rep Orthop, 2014, 2014: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Houdek MT, Wilke BK, Ryssman DB, Turner NS. Radiographic and functional outcomes following bilateral ankle fusions. Foot Ankle Int, 2014, 35: 1250–1254. [DOI] [PubMed] [Google Scholar]
- 29. Vaughan P, Gordon D, Goldberg A, Cullen N, Singh D. Patient satisfaction and function after bilateral ankle arthrodeses. Foot Ankle Surg, 2015, 21: 160–163. [DOI] [PubMed] [Google Scholar]
- 30. Henricson A, Kamrad I, Rosengren B, Carlsson A. Bilateral arthrodesis of the ankle joint: self‐reported outcomes in 35 patients from the Swedish ankle registry. J Foot Ankle Surg, 2016, 55: 1195–1198. [DOI] [PubMed] [Google Scholar]
- 31. Maenohara Y, Taniguchi A, Tomiwa K, et al Outcomes of bilateral vs unilateral ankle arthrodesis. Foot Ankle Int, 2018, 39: 530–534. [DOI] [PubMed] [Google Scholar]


