Abstract
Background:
Previously published findings from a study of university students living in substance use disorder (SUD) recovery housing showed an eight-session heart rate variability biofeedback (HRVB) intervention significantly reduced craving. That study, however, uncovered pronounced inter-participant variability in craving change patterns through the course of HRVB that warranted further exploration. The purpose of the current investigation was to examine how within- and between-person factors may have differentially influenced craving changes.
Methods:
A longitudinal multilevel modeling approach was used with time at level-1 nested within persons at level-2. Multilevel models of change were estimated to model craving trajectories and predictor relationships over time as a function of age, sex, length of abstinence, daily HRVB practice, anxiety, depression, and stress.
Results:
A quadratic pattern of craving reductions was found, indicating that craving reductions accelerated over time for some participants. Daily HRVB practice of > 12 min and older age significantly enhanced craving reductions over time. Increases in depressive symptoms attenuated the effects of HRVB on craving. The other predictors were not significantly associated with craving in this study. The true R2 for the final model indicated that 20.5% of the variance in craving was explained by older age, daily HRVB > 12 min, and within-person changes in depression.
Conclusions:
HRVB shows promise as an accessible, scalable, and cost-effective complementary anti-craving intervention. Healthcare providers may help persons recovering from SUD to better manage substance craving by the routine and strategic use of HRVB practice.
Keywords: Craving, Heart rate variability biofeedback, Substance use disorder, Longitudinal, Multilevel modeling
1. Introduction
1.1. Background and significance
University students in substance use disorder (SUD) recovery face special challenges including widespread peer alcohol and other drug use and a culture that normalizes substance use (Helmer, Mikolajczyk, McAlaney, et al., 2014; Laudet, Harris, Kimball, Winters, & Moberg, 2016). Young adults returning to university after SUD treatment are thus at a heightened risk for relapse (Perron et al., 2011). While many factors may act as precursors to relapse, craving is one of its strongest predictors (Fatseas et al., 2015; Paliwal, Hyman, & Sinha, 2008; Sinha, 2011), and persons recovering from SUD may continue to experience cravings years after achieving abstinence (Addolorato, Leggio, Abenavoli, & Gasbarrini, 2005). Addressing substance craving is, therefore, an essential component of relapse prevention for individuals in both early and sustained SUD remission (NIDA, 2016; Tiffany & Wray, 2012).
The most commonly used non-pharmacological craving interventions are cognitive in nature. Craving, however, is also in part mediated by psychophysiological processes that contribute to pathological motivation to engage in substance use (Robinson & Berridge, 2008). For example, experiences of craving are often associated with physiological responses such as increased heart rate (Kennedy, Epstein, Jobes, et al., 2015) that may amplify psychological responses such as anxiety (Eddie, Vaschillo, Vaschillo, & Lehrer, 2015; Haass-Koffler, Leggio, & Kenna, 2014). Heightened heart rate and anxiety are associated with decreased heart rate variability (i.e., dynamic changes in the time intervals between heart beats) (Eddie et al., 2015; Kemp & Quintana, 2013), an indicator of reduced adaptive capacity and behavioral flexibility (Buckman, Vaschillo, Fonoberova, Mezic, & Bates, 2018). In contrast, high levels of heart rate variability are associated with a flexible autonomic nervous system that provides for rapid modulation of physiological states resulting in improved behavioral control (Lehrer & Eddie, 2013; Porges, 2007). Heart rate variability biofeedback (HRVB) is a form of paced breathing that addresses the psychophysiological processes of craving by acutely increasing heart rate variability (Kemp & Quintana, 2013; Lehrer & Eddie, 2013; Lehrer & Gevirtz, 2014; Stanhope, 2018). In HRVB training, patients are taught to pace their breath at a rate that produces large, synchronous oscillations in respiration and heart rate, thus substantially increasing acute heart rate variability. HRVB amplifies oscillations through the combined effects of respiratory sinus arrhythmia (heart rate acceleration during inhalation and deceleration during exhalation) and stimulation of the baroreflex when breathing is slowed to a resonance frequency of the cardiovascular system at 0.1 Hz (corresponding to approximately 6 breaths per minute). Resonance paced breathing engages the parasympathetic nervous system, leading to greater behavioral control (Gevirtz, 2013).
Earlier work in HRVB for craving supports this idea by showing that brief HRVB interventions have the potential to reduce craving in individuals in treatment for SUD (Eddie, Kim, Bates, Lehrer, & Deneke, 2014; Penzlin et al., 2017; Penzlin, Siepmann, Illigens, Weidner, & Siepmann, 2015). However, a recent review of HRVB as a complementary anti-craving intervention showed inconsistent results of HRVB effectiveness in reducing craving, and identified the need for a longitudinal examination of craving changes during the course of HRVB (Alayan, Eller, Bates, & Carmody, 2018). A recently published longitudinal study of university students in SUD recovery found significant substance craving reductions during a full course of HRVB (i.e., 8 sessions) (Eddie, Conway, Alayan, Buckman, & Bates, 2018). Yet, spaghetti plots of individual participants’ data showed marked variability in the observed craving changes over time. This heterogeneity among participants raised the possibility of identifying participant level factors associated with craving trajectories that may be useful in personalizing HRVB to improve its effectiveness.
The present investigation was a secondary analysis of craving outcomes from that study (Eddie et al., 2018), using longitudinal multilevel modeling (MLM) to examine sources of dependency and interpret craving changes as a function of within- and between-person sources of variance. The use of MLM allowed the simultaneous examination of between- and within-person relationships and permitted the identification of individual differences that relate to craving reductions during HRVB.
1.2. Current study hypotheses
The main objective in the current investigation was to model craving changes at 12 time points over the course of approximately 24 weeks of monitoring, giving special consideration to within- and between-person predictors of craving. Several antecedents of relapse have been consistently linked to craving in the literature, including perceived stress (Sinha, 2008), depression (Witkiewitz & Bowen, 2010), anxiety (Sinha, Fuse, Aubin, & O’Malley, 2000), and length of abstinence (Wang, Shi, Chen, et al., 2013). In the current study, craving levels were hypothesized to decline over time in response to HRVB and at different rates for different persons, partially due to variations in perceived stress, depression, and anxiety. Participating in the HRVB condition was expected to reduce craving over time (Alayan et al., 2018). Individuals with higher, average levels of perceived stress, depression, and anxiety were expected to show greater craving. At the individual level, within-person increases in perceived stress, depression, and anxiety were expected to increase craving during that time period. Longer time abstinence was hypothesized to be associated with greater craving reductions over the course of the HRVB intervention. We also sought to identify a daily breathing practice time that confers optimal clinical benefit because HRVB practice time has not yet been consistently linked to craving reduction (Alayan et al., 2018).
2. Methods
2.1. Study design and setting
This investigation used extant data from a non-randomized study with a wait list control condition, carried out in recovery housing of a public, northeastern, United States university. Participants were assessed at four occasions before the HRVB intervention over the first 12 weeks followed by a 4- or 11-week rest period (depending on whether the rest period occurred over the Summer or Winter university recess). Then, participants were assessed on eight occasions over 12 weeks during the HRVB intervention. See Eddie et al., 2018 for full description (Eddie et al., 2018).
2.2. Participants
Forty-six university students were enrolled in the study. To participate, study volunteers were required to be in recovery from SUD, enrolled as an undergraduate or postgraduate student at the university, and be current or previous residents of the university’s recovery housing. Details of the recruitment procedure have been previously reported (Eddie et al., 2018). The majority of the sample consisted of young (M = 23.6 years; SD = 5.0 years) White (91%) male (72%) students with prolonged abstinence (M = 2.62 years, SD = 1.93 years). Approximately half of the participants (52.10%) reported taking prescribed antidepressant or mood stabilizing medications. Most participants were single (97.6%) and 50% were living outside recovery housing during the study period.
For the purpose of longitudinal analysis, a minimum of three observations per participant was required so that undirected fluctuations in craving were distinguishable from real change (Hoffman, 2015). Two participants had less than three time points on the outcome variable and were thus excluded from the sample (Hoffman, 2015). The final data for analysis consisted of 44 participants for 12 occasions totaling 528 observations. Four participants dropped out from the experimental condition because they felt too busy with school work. There were 128 missing observations in the outcome due to the lack of control condition for 16 of the participants in addition to the 6 dropouts and other missing responses, amounting to 24% of the expected observations.
2.3. Measures
Length of abstinence:
At commencement of control and experimental condition participation, participants self-reported the date of their last alcohol and other drug use. Length of abstinence from alcohol and other drugs was calculated as days since last substance use at day one of control and/or experimental condition participation.
1. Penn Alcohol Craving Questionnaire (PACS):
Participants were asked to rate the severity of their craving using the PACS, a unidimensional 5-item scale. Items are coded on a 7-point scale from “0”, (Not present) to “6” (Severe). A total PACS score ranges from 0 to 30 with higher scores indicating greater substance craving. The scale has high internal consistency (ɑ = 0.92) and has been validated in various clinical samples (Flannery, Volpicelli, & Pettinati, 1999; Hitschfeld et al., 2015; Kim et al., 2008). A previously modified version of PACS that captures both drug and alcohol craving was used in this study. This amended version of PACS had similar internal consistency to the original scale, and convergent and discriminant validity (Eddie et al., 2014). Cronbach’s alpha in this sample ranged from 0.72 to 0.94.
Beck Anxiety Inventory (BAI):
The BAI is a 21-item questionnaire that assesses the severity of an individual’s anxiety in the past week. Items are coded on a 4-point scale ranging from “0=Not at all” to “3 = Severely”. A total BAI score ranges from 0 to 63 with higher scores indicating greater anxiety symptoms (Beck & Steer, 1993). Cronbach’s alpha in this sample ranged from 0.86 to 0.91.
Beck Depression Inventory – II (BDI-II):
The BDI-II is a 21-item questionnaire that assesses the severity of an individual’s depression in the past week. Items are coded on a 4-point scale from “0=Not at all” to “3 = Severely”. A total BDI-II score ranges from 0 to 63 with higher scores indicating greater depression symptoms (Beck, Steer, & Brown, 1996). Cronbach’s alpha in this sample ranged from 0.79 to 0.90.
Perceived Stress Scale (PSS):
The PSS is a 10-item questionnaire that assesses stress frequency in the past month. Items are measured on a 5-point, Likert-type scale (“0 = Never” to “4 = Very often”). A total PSS score ranges from 0 to 40 with higher scores indicating greater perceived stress (Cohen, Kamarck, & Mermelstein, 1983). Cronbach’s alpha in this sample ranged from 0.81 to 0.87.
Daily HRVB practice:
To facilitate accurate assessment of practice, participants were asked to keep a daily practice log using forms provided by experimenters. Participants were asked to record the total number of minutes they practiced each day in the AM and PM. Ranges were not provided; rather participants were asked to record the exact number of minutes practiced. Participants provided this information to research assistants over the phone during weekly timeline follow-back interviews (Sobell and Sobell 2015). If participants forgot to fill out their form on certain days, research assistants used timeline follow-back strategies articulated by Sobell & Sobell (Sobell & Sobell, 1992) to help participants accurately remember their practice times.
2.4. Study procedures
Participants in the waitlist condition completed the PACS, BAI, BDI, and PSS on four occasions over the 12-week semester (occasions 1–4). They were allowed to continue any treatment as usual including conventional recovery services offered by the Recovery House and/or outside therapies. Participants in the HRVB condition responded to the PACS and PSS at each occasion and to the BAI and BDI on occasions 5, 8, 11, and 12. They received 8 sessions of manualized HRVB training (Lehrer, Vaschillo, & Vaschillo, 2000) over the course of a university semester (~12 weeks), starting on occasion 5. Participants were trained to practice breathing at their own resonance frequency (identified when respiration and heart rate oscillations achieved phase) with the help of visual pacers and electronic monitoring of the heart rate. In addition, they were asked to practice resonance frequency breathing for 15-min periods twice daily on their own. For practice, participants were provided with either a StressEraser HRVB device (Heilman, Handelman, Lewis, & Porges, 2008) or Stress Doctor HRVB app for smartphone (Azumio, Inventor, 2012) depending on their preference. This study was conducted in accordance with the institutional review board guidelines at the home institution. Details of the study procedures were previously reported (Eddie et al., 2018).
2.5. Analytical procedures in multilevel modeling
A multilevel modeling approach was used to perform a longitudinal analysis of craving changes over time and across conditions using the Statistical Package for the Social Sciences (SPSS) version 23.0. The purposes of these analyses were to (1) describe the average pattern of craving changes over time, (2) describe the individual differences within these changes, and (3) predict between-person differences and the remaining within-person variation over time. A series of mixed effects random coefficient models were analyzed with observations at level-1 nested within persons at level-2. These analyses modeled within-person and between-person craving variations simultaneously at both levels. Within-person predictors of craving included depression, anxiety, and perceived stress. Between-person predictors of craving included age, sex, length of abstinence, and dose of daily HRVB practice.
Because the actual time intervals between measurement occasions differed per participant, time was entered as a covariate in the models and was centered such that 0 indicated the first observation. Time observations were balanced across persons by using the actual number of weeks in the study for each participant, starting with week one after the first control session (occasion 1) and week 24 before the last experimental session (occasion 12). Time models were estimated using restricted maximum likelihood (REML) whereas Maximum Likelihood (ML) was used when fixed predictors were added to the models (Hoffman, 2015). The significance of individual fixed effects was evaluated using their Wald test p values. The significance of multiple fixed effects and random effects variances and covariances was evaluated using likelihood ratio tests including −2 Log Likelihood (−2LL), Akaike Information Criterion (AIC), and Bayesian Information Criterion (BIC). Unstructured residual covariance was used because neither first-auto-regressive correlation nor lag-1 Toeplitz residual covariance resulted in significant improvement in model fit (p > .05). The proportion of explained total outcome variance (R2) was determined by calculating the square of the Pearson correlation between the predicted outcome and the actual outcome. This method generates a true R2 since it is based on the total original outcome variance.
The steps were: 1) Calculating the IntraClass Correlation (ICC) statistic based on covariance parameters from the null model with craving as the outcome variable and no predictors. The ICC is the proportion of the variance ranging from 0 to 1 explained by the grouping structure in the population (Hoffman, 2015). 2) Estimating the baseline time model to determine a trajectory of substance craving changes over time. 3) Centering continuous predictors to have a meaningful zero. 4) Estimating the practice and final models by adding between-person (age, sex, length of abstinence, daily breathing practice) and within-person (anxiety, depression, perceived stress) predictors incrementally. A stepwise approach was used to build the final model to maintain a balance between the need for complexity and the need for parsimony (Hoffman, 2015; McCoach & Black, 2012). Predictors that did not improve model fit were therefore removed from the final model.
3. Results
3.1. Unconditional and time models of craving changes
Three empty models were first estimated to test for random effects of time before adding any fixed effects (see Table 1). The ICC was 0.49 indicating that 49% of the variability was attributable to differences between participants, thus indicating the need for a two-level model for time within persons in modeling craving changes over time. Adding a random slope of time significantly improved model fit (−2ΔLL (2) = 54, p < .001) and caused a 47% increase in intercept variance. We then added a quadratic slope of time to assess for non-linear change. The empty quadratic model significantly improved fit (−2ΔLL (3) = 10.6, p < .05) and positive quadratic intercept and slope were found, indicating an accelerating rate of craving reduction over time. While the fixed quadratic effect of time was not significant, the random quadratic time model was significant. The final baseline model (Table 2) included a fixed effect of time and random effects of linear and quadratic time, indicating that the acceleration of craving reductions over time was due to individual differences and did not occur for all participants on average. There was a significant rate of linear reduction in craving on average. However, the random variation around the linear slope indicated that craving reductions were expected to occur at different rates by participant over time. The R2 for the baseline model was determined by calculating the square of the correlation between predicted PACS and actual PACS, yielding an R2 of 0.018.
Table 1.
Empty models of time (N = 44).
| Model parameters | Empty random intercept model | Empty random slope model | Empty random quadratic model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |
| Fixed effects: | |||||||||
| Intercept | 3.95 | 0.46 | 0.000 | 3.93 | 0.49 | 0.000 | 3.87 | 0.45 | 0.000 |
| Variance components: | |||||||||
| Intercept variance | 8.40 | 2.08 | 0.000 | 16.46 | 6.48 | 0.011 | 14.38 | 5.40 | 0.008 |
| Residual variance | 8.68 | 0.65 | 0.000 | 7.24 | 0.60 | 0.000 | 6.74 | 0.57 | 0.000 |
| Intercept-linear covariance | - | - | - | −0.34 | 0.20 | 0.085 | −0.52 | 0.40 | 0.194 |
| Linear slope variance | - | - | - | 0.02 | 0.01 | 0.021 | 0.11 | 0.05 | 0.029 |
| Quadratic intercept variance | - | - | - | - | - | - | 0.006 | 0.01 | 0.553 |
| Intercept-quadratic covariance | - | - | - | - | - | - | −0.002 | 0.00 | 0.044 |
| Quadratic slope variance | - | - | - | - | - | - | 0.004 | 0.00 | 0.044 |
| REML model fit: | |||||||||
| -2LL | 2096.7 | 2042.7 | 2032.1 | ||||||
| AIC | 2100.7 | 2050.7 | 2046.1 | ||||||
| BIC | 2108.7 | 2066.6 | 2073.9 | ||||||
| Number of parameters | 3 | 5 | 8 | ||||||
| Significance of fit change: | |||||||||
| Absolute -2LL difference | - | 54 | 10.6 | ||||||
| DF difference | - | 2 | 3 | ||||||
| Exact p value | - | 0.000 | 0.014 | ||||||
Bolded numbers are statistically significant parameters with p < 0.05
Table 2.
Baseline, practice, and final model parameters (N = 44).
| Model parameters | Baseline model | Practice model | Final model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |
| Fixed effects: | |||||||||
| Intercept | 5.40 | 0.64 | 0.000 | 6.54 | 0.67 | 0.000 | 6.08 | 0.73 | 0.000 |
| Linear time | −0.07 | 0.02 | 0.002 | −0.07 | 0.02 | 0.003 | −0.05 | 0.02 | 0.038 |
| Age centered at median (0 = 23) | - | - | - | −0.28 | 0.08 | 0.002 | −0.26 | 0.09 | 0.008 |
| Daily practice > 12min | - | - | - | −2.26 | 0.78 | 0.006 | −1.83 | 0.87 | 0.044 |
| Within-person BDI | - | - | - | - | - | - | 0.27 | 0.04 | 0.000 |
| Between-person BDI centered at mean (0 = 8) | - | - | - | - | - | - | 0.09 | 0.08 | 0.289 |
| Variance components: | |||||||||
| Intercept variance | 11.53 | 4.03 | 0.004 | 5.30 | 2.65 | 0.046 | 6.06 | 3.34 | 0.070 |
| Residual variance | 6.73 | 0.56 | 0.000 | 6.73 | 0.59 | 0.000 | 7.38 | 0.85 | 0.000 |
| Intercept-linear covariance | −0.42 | 0.36 | 0.247 | −0.35 | 0.34 | 0.308 | −0.10 | 0.10 | 0.297 |
| Linear slope variance | 0.11 | 0.49 | 0.025 | 0.13 | 0.06 | 0.020 | 0.01 | 0.00 | 0.083 |
| Quadratic intercept variance | 0.01 | 0.01 | 0.512 | 0.01 | 0.01 | 0.453 | - | - | - |
| Intercept-quadratic covariance | 0.00 | 0.00 | 0.028 | 0.00 | 0.00 | 0.022 | - | - | - |
| Quadratic slope variance | 0.00 | 0.00 | 0.026 | 0.00 | 0.00 | 0.023 | - | - | - |
| ML model fit: | |||||||||
| -2LL | 2022.5 | 1816.6 | 1153.6 | ||||||
| AIC | 2040.5 | 1838.6 | 1173.6 | ||||||
| BIC | 2076.3 | 1881.3 | 1207.7 | ||||||
| Number of parameters | 9 | 11 | 10 | ||||||
| Fit change: | |||||||||
| Absolute -2LL difference | 205.9 | 663 | |||||||
| DF difference | 2 | 1 | |||||||
| Exact p value | 0.000 | 0.000 | |||||||
Bolded numbers are statistically significant parameters with p < 0.05
3.2. Conditional model of between-person predictors of craving changes
During the experimental phase, participants reported practicing HRVB breathing for an average of 11.46 min per day (SD = 7.88). Notably, the amount of daily HRVB practice differed by age. Using a median split of age, we found that participants younger than 23 years practiced more than participants who were 23 years and older. The mean daily reported HRVB practice time was 14.32 min (SD = 7.84) for age < 23 versus 9.23 min (SD = 7.16) for age 23 and older. The addition of mean daily practice to the baseline model was not significant. A dichotomous variable of low and high practice was created to differentiate the effects of low versus high amounts of HRVB practice outside experimental sessions. High practice was coded as 1 indicating > 12 min of daily HRVB breathing, which is more than the sample mean daily practice; low practice was coded as 0 indicating < 12 min of daily HRVB practice. Controlling for age, sex, and length of abstinence (between-person covariates), a fixed effect of practice was added to the baseline model. The parameters of the baseline, practice, and final models are reported in Table 2.
Sex and length of abstinence did not significantly influence craving changes as indicated by their Wald test (p > .05). Age and practice however were significant covariates. This model significantly improved fit (−2ΔLL (2) = 205.9, p < .001) and accounted for 58% of the total level-2 craving variance. The true R2 for the practice model was 0.140.
3.3. Conditional models of within-person predictors of craving changes
BDI was person-mean-centered by creating two separate predictor variables of BDI. The within-person BDI represents the deviation from each person’s mean BDI across all his or her occasions (level-1 effect) and the level-2 between-person BDI represents the person’s mean BDI across weeks centered at the grand mean. Controlling for age and practice, the level-1 effect of BDI was statistically significant indicating that reporting greater depression than their usual level was related to less craving reduction on that week. The level-2 effect of BDI was not significant. No statistically significant effects were observed when the same person-mean-centering method was used to add BAI and PSS as predictors of craving changes.
The final model included age, practice, and within-person BDI as significant predictors of craving. At level-2, the significant effects of age and practice indicated that PACS scores decreased with greater age and with 12 or more minutes of daily HRVB practice. At level-1, the significant effect of within-person BDI predicted less craving reduction. The final model with age, practice, and within-person depression explained 20.5% of the total variance in craving over time. Thus, the R2 increased significantly from the baseline model (0.018), to the practice model (0.140) to the final model (0.205). The significant changes in fit indices indicated the improvement in model fit with the addition of practice and psychological factors.
3.4. The effect of HRVB on craving reductions
Table 3 presents the parameters of a piecewise random coefficient model examining the effect of the HRVB intervention on craving reductions over time. The first HRVB training session (occasion 5) was identified as the breakpoint in the craving trajectory. The slope15 described the change in slope from occasion 1 to occasion 5 and slope512 described the change in slope from occasion 5 to occasion 12. Both slopes were significant (p < .05). Adding random variances and covariances for the random slope before occasion 5 and the random slope after occasion 5 improved model fit (−2ΔLL(5) = 32.3, p < .001) with a smaller AIC and BIC. However, only slope 512 for experimental assessments remained significant.
Table 3.
Piecewise model parameters (N = 44).
| Fixed slope15, Fixed slope512, Model | Random slope15, Random slope512, Model | |||||
|---|---|---|---|---|---|---|
| (Time 0 = Occasion 1) | (Time 0 = Occasion 1) | |||||
| Model parameters | Estimate | SE | p | Estimate | SE | p |
| Fixed effects: | ||||||
| Intercept | 5.36 | 0.60 | 0.000 | 5.35 | 0.70 | 0.000 |
| Slope15 | −0.31 | 0.14 | 0.026 | −0.28 | 0.20 | 0.179 |
| Slope512 | −0.19 | 0.07 | 0.008 | −0.21 | 0.10 | 0.044 |
| Variance components: | ||||||
| Intercept variance | 7.99 | 1.96 | 0.000 | 11.77 | 3.99 | 0.003 |
| Residual variance | 8.25 | 0.62 | 0.000 | 6.41 | 0.53 | 0.000 |
| Intercept-Slope15 covariance | - | - | - | −1.47 | 1.03 | 0.152 |
| Linear Slope15/time variance | - | - | - | 0.92 | 0.40 | 0.021 |
| Intercept-Slope512 covariance | - | - | - | −0.11 | 0.51 | 0.822 |
| Slope 15–512 covariance | - | - | - | −0.30 | 0.16 | 0.065 |
| Linear Slope512 variance | - | - | - | 0.23 | 0.09 | 0.013 |
| REML model fit: | ||||||
| -2LL | 2080.1 | 2047.8 | ||||
| AIC | 2084.1 | 2061.8 | ||||
| BIC | 2092.0 | 2089.7 | ||||
| Number of parameters | 5 | 10 | ||||
Bolded numbers are statistically significant parameters with p < 0.05
3.5. The moderation effect of practice time
A post-hoc regions-of-significance analysis was conducted to further explore the moderation effect of practice time on the longitudinal relationship between HRVB and craving (Fig. 1). The analysis considered the effect for several alternate cutoff scores representing the 10th, 20th, 30th, 40th and 50th percentiles of practice time. Using 99% confidence intervals, practice time moderated the slope between HRVB and craving by nine minutes of daily HRVB practice while accounting for age and levels of depression.
Fig. 1.
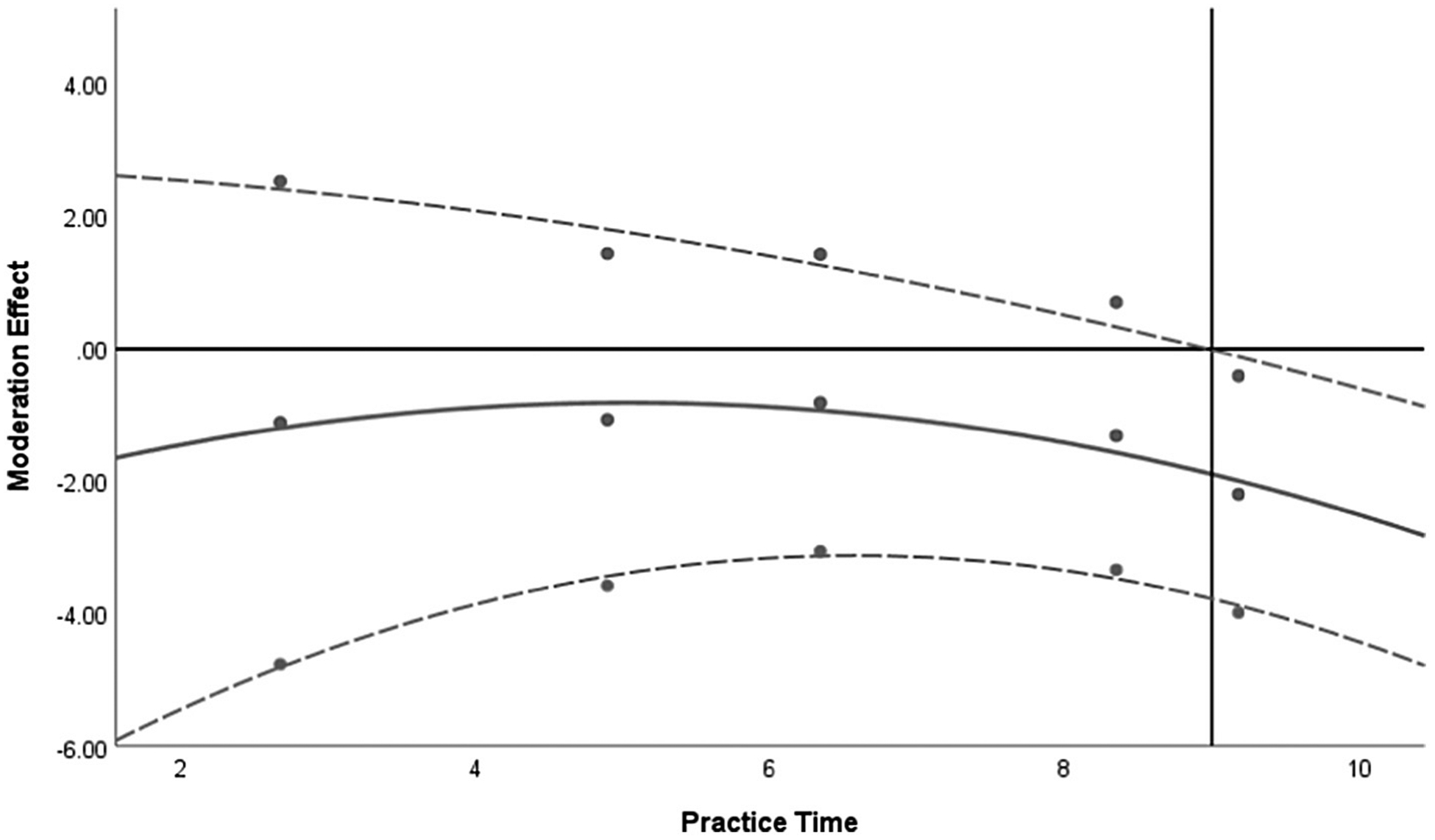
The moderation effect of Practice Time on the longitudinal relation between HRVB and PACS.
The central, solid curved line represents the point estimate for the effect at several levels of practice time (dots represent 10th, 20th, 30th, 40th, and 50th percentiles). The upper and lower dashed, curved lines represent the 99% confidence intervals of this effect relative to zero. The horizontal reference line indicates an effect estimate of zero. The vertical reference line is the boundary between the 99% confidence interval of the slope that includes zero effect for levels of Practice Time (below a value of 9 min) and the region of significance (above a value of 9 min).
4. Discussion
The present investigation used MLM to model substance craving changes in university students recovering from SUD, before and during HRVB intervention. This study’s longitudinal design allowed the examination of within- and between person sources of variance. In this sample, there was a similar amount of craving variation within-persons (51%) and between-persons (49%), indicating the importance of addressing within-person craving changes over time. Substance craving trajectories across ~24 weeks of monitoring showed random effects of linear and quadratic time, indicating that the acceleration of craving reductions over time was due to individual differences. The piecewise model showed that substance craving reductions before HRVB were not statistically significant supporting that participation in the eight-session HRVB protocol contributed to craving reductions over time.
The effects of time-invariant predictors of craving changes, including age, sex, length of abstinence, and average daily HRVB practice also were examined. Craving changes did not differ by sex or length of abstinence. Yet, of the between-persons mean differences found in the empty model (49% of the total craving variance), more than half (58%) was due to consistent daily HRVB practice of > 12 min and older age. Notably, a post hoc, regions-of-significance exploratory analysis suggested nine minutes of daily practice may in fact be all that is necessary to effect changes in craving while accounting for age and levels of depression. These are important findings since previous studies have not found such dose-dependent HRVB practice effects (Eddie et al., 2014; Zucker, Samuelson, Muench, Greenberg, & Gevirtz, 2009). It is possible that previous null findings for dose-dependent HRVB practice effects were due to various challenges associated with craving research (Alayan et al., 2018). For instance, the measurement of craving itself is challenging because of its temporal and subjective nature. Only a longitudinal study with three or more observations has the ability to differentiate real change from undirected fluctuations (Hoffman, 2015).
With regards to dose-dependent HRVB practice effects, two other important factors include adherence to recommended daily practice and the reliability of practice reporting. This sample showed age differences in terms of adherence to daily HRVB practice. Younger participants did more daily HRVB practice than older participants. This may be partly explained by the fact that participants younger than 23 years reported higher craving scores than older participants. It may be that participants experiencing greater craving felt more need to practice HRVB. The > 12 min daily practice dose-effect relationship found in this study, and the nine-minute effect observed in the post hoc analysis should be tested in future SUD studies, particularly in samples experiencing higher craving levels, and at earlier stages of recovery. Clinically, a nine-minute daily breathing practice guideline may facilitate adherence and be of greater popularity than the current recommended practice of 15 min twice daily.
Although sex differences in experiences of craving have been previously reported (Hitschfeld, Schneekloth, Ebbert, et al., 2015; Kennedy, Epstein, Phillips, & Preston, 2013), none were found in this study. Women however were under-represented in the present sample which may have contributed to a Type II error. In addition, there was insufficient variability to allow for a strong test of abstinence length due to the long abstinence times found in this sample. Given that craving is expected to decline with prolonged abstinence (Li, Caprioli, & Marchant, 2015; Wang et al., 2013), exploring this relationship in persons early in recovery may show differences in HRVB dose requirements that are dependent on the length of abstinence. The extent of daily practice may be dependent on the stage of SUD recovery.
Importantly, this study examined the effects of within-person predictors of craving changes including depression, anxiety, and perceived stress. The within-person aspect of depression had the only statistically significant effect among the three within-person predictors of craving changes over time. This finding indicated that persons who had depressive symptoms more than usual (relative to their mean depression score) had less craving reduction during that period. This finding is especially noteworthy given that the between-person effect of depression on change in craving was not significant. It emphasizes the importance of dynamic within-person changes over time in the way depressive symptoms influence treatment compliance and efficacy. Treating depressive symptoms may, therefore, enhance the effectiveness of HRVB in reducing substance craving during SUD recovery. Fluctuation in anxiety and perceived stress did not significantly affect craving in this sample, although a different pattern may emerge in samples with elevated clinical symptoms and shorter periods of recovery.
The results of this study should be interpreted in light of its design, sampling, and measurement limitations. The non-random convenience and homogenous sample may have increased selection bias affecting both internal and external validity. The small sample size (N = 44) did not provide enough power for building a more comprehensive model of craving trajectories that includes interactions among the assessed predictors. Participants in this study reported subclinical craving levels and all were in sustained SUD remission. Thus, our findings may not be generalizable to all university students recovering from SUD. In addition, daily HRVB practice was measured using a weekly timeline follow-back method but was not confirmed externally. A larger population-based sample would yield results generalizable to a broader population of recovering university students and greater power for the detection of potential interactions over time.
5. Conclusions
HRVB is a novel and easily accessible intervention that offers the advantage of addressing the psychophysiological processes of craving. This study provided longitudinal evidence that HRVB can enhance the efficacy of conventional craving support in recovery housing. The use of MLM in this study allowed the simultaneous examination of between-and within-person relationships and permitted us to identify individual differences and within-person changes that relate to craving reductions during the HRVB intervention. The outcomes of this study have implications for hypothesized HRVB practice-dose relationships. Daily paced breathing practice of > 12 min contributed to greater craving reductions in this study, and a post hoc, exploratory analysis suggests as little as nine minutes of daily practice may be sufficient for effecting significant reductions in craving. Younger participants and those reporting higher craving levels completed more daily HRVB practice. In addition, the experience of within-subjects, elevated from baseline depressive symptoms were found to attenuate craving reductions over time. These findings should be replicated in larger, more diverse samples with higher baseline craving levels and with participants earlier in SUD recovery. Future studies should attempt to determine the long-term effects of HRVB, whether the craving reductions achieved during HRVB are sustained after the intervention ends, and whether a continued daily practice is needed to keep craving at bay.
HIGHLIGHTS.
Over time, craving levels changed more within persons than between persons.
Daily HRVB practice of > 12 min produced larger craving reductions.
Depressive symptoms more than the person’s usual attenuated craving reductions.
Acknowledgments
This paper was based on the dissertation work of Nour Alayan, Ph.D., R.N. at Rutgers University. The original study was conducted at Rutgers University and was supported in part by NIAAA grants K24 AA021778, R01 AA023667, and F32 AA025251. The funding sources had no role in the study design, collection, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the article for publication.
Footnotes
Conflicts of interest
We have no conflicts of interest to disclose.
References
- Addolorato G, Leggio L, Abenavoli L, & Gasbarrini G (2005). Neurobiochemical and clinical aspects of craving in alcohol addiction: A review. Addictive Behaviors, 30(6), 1209–1224. [DOI] [PubMed] [Google Scholar]
- Alayan N, Eller L, Bates ME, & Carmody DP (2018). Current evidence on heart rate variability biofeedback as a complementary anticraving intervention. Journal of Alternative and Complementary Medicine, 00(00), 1–12. 10.1089/acm.2018.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azumio Inventor (2012). Stress doctor.
- Beck AT, & Steer RA (1993). Beck Anxiety Inventory Manual. San Antonio: TX Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Buckman JF, Vaschillo EG, Fonoberova M, Mezic I, & Bates ME (2018). The translational value of psychophysiology methods and mechanisms: Multi-level, dynamic, personalized. Journal of Studies on Alcohol and Drugs, 79(2), 229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Eddie D, Conway FN, Alayan N, Buckman J, & Bates ME (2018). Assessing heart rate variability biofeedback as an adjunct to college recovery housing programs. Journal of Substance Abuse Treatment, 92, 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddie D, Kim C, Bates ME, Lehrer P, & Deneke E (2014). A pilot study of brief heart rate variability biofeedback to reduce craving in young adult men receiving inpatient treatment for substance use disorders. Applied Psychophysiology and Biofeedback, 39(3–4), 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddie D, Vaschillo E, Vaschillo B, & Lehrer P (2015). Heart rate variability biofeedback: Theoretical basis, delivery, and potential for treating sud. Addiction Research and Theory, 23(4), 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatseas M, Serre F, Alexandre JM, Debrabant R, Auriacombe M, & Swendsen J (2015). Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: A comparison of substance- and person-specific cues. Addiction, 110(6), 1035–1042. [DOI] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, & Pettinati HM (1999). Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research, 23(8), 1289–1295. [PubMed] [Google Scholar]
- Gevirtz R (2013). The promise of heart rate variability biofeedback: Evidence-based applications. Biofeedback, 41(3), 110–120. [Google Scholar]
- Haass-Koffler CL, Leggio L, & Kenna GA (2014). Pharmacological approaches to reducing craving in patients with alcohol use disorders. CNS Drugs, 28(4), 343–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilman KJ, Handelman M, Lewis G, & Porges SW (2008). Accuracy of the StressEraser in the detection of cardiac rhythms. Applied Psychophysiology and Biofeedback, 33(2), 83–89. [DOI] [PubMed] [Google Scholar]
- Helmer SM, Mikolajczyk RT, McAlaney J, et al. (2014). Illicit substance use among university students from seven European countries: A comparison of personal and perceived peer use and attitudes towards illicit substance use. Preventive Medicine, 67, 204–209. [DOI] [PubMed] [Google Scholar]
- Hitschfeld MJ, Schneekloth TD, Ebbert JO, et al. (2015). Female smokers have the highest alcohol craving in a residential alcoholism treatment cohort. Drug and Alcohol Dependence, 150, 179–182. [DOI] [PubMed] [Google Scholar]
- Hoffman L (2015). Longitudinal analysis: Modeling within-person fluctuation and change (1st ed.). New York: Routledge. [Google Scholar]
- Kemp AH, & Quintana DS (2013). Review: The relationship between mental and physical health: Insights from the study of heart rate variability. International Journal of Psychophysiology, 89, 288–296. [DOI] [PubMed] [Google Scholar]
- Kennedy AP, Epstein DH, Jobes ML, et al. (2015). Continuous in-the-field measurement of heart rate: Correlates of drug use, craving, stress, and mood in polydrug users. Drug and Alcohol Dependence, 151, 159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy AP, Epstein DH, Phillips KA, & Preston KL (2013). Sex differences in cocaine/heroin users: Drug-use triggers and craving in daily life. Drug and Alcohol Dependence, 132(1–2), 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MJ, Kim SG, Kim HJ, Kim HC, Park JH, Park KS, & Kim CM (2008). A study of the reliability and validity of the Korean Version of the Penn Alcohol Craving Scale for alcohol-dependent patients. Psychiatry Investigation, 5, 175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Harris K, Kimball T, Winters KC, & Moberg DP (2016). In college and in recovery: Reasons for joining a Collegiate Recovery Program. Journal of American College Health, 64(3), 238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer P, & Eddie D (2013). Dynamic processes in regulation and some implications for biofeedback and biobehavioral interventions. Applied Psychophysiology and Biofeedback, 38, 143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer PM, & Gevirtz R (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5(756), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer PM, Vaschillo E, & Vaschillo B (2000). Resonant frequency biofeedback training to increase cardiac variability: rationale and manual for training. Applied Psychophysiology & Biofeedback, 25(3), 177–191. [DOI] [PubMed] [Google Scholar]
- Li X, Caprioli D, & Marchant NJ (2015). Recent updates on incubation of drug craving: A mini-review. Addiction Biology, 20(5), 872–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoach DB, & Black AC (2012). Introduction to estimation issues in multilevel modeling. New Directions for Institutional Research, 2012(154), 23–39. [Google Scholar]
- NIDA (2019). DrugFacts: Treatment approaches for drug addiction. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction on 2019 May 16. [Google Scholar]
- Paliwal P, Hyman SM, & Sinha R (2008). Craving predicts time to cocaine relapse: Further validation of the Now and Brief versions of the cocaine craving questionnaire. Drug and Alcohol Dependence, 93, 252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penzlin AI, Barlinn K, Illigens BM, Weidner K, Siepmann M, & Siepmann T (2017). Effect of short-term heart rate variability biofeedback on long-term abstinence in alcohol dependent patients—A one-year follow-up. BMC Psychiatry, 17(1), 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penzlin AI, Siepmann T, Illigens BMW, Weidner K, & Siepmann M (2015). Heart rate variability biofeedback in patients with alcohol dependence: A randomized controlled study. Neuropsychiatric Disease and Treatment, 11, 2619–2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perron BE, Grahovac ID, Uppal JS, Granillo MT, Shutter J, & Porter CA (2011). Supporting students in recovery on college campuses: Opportunities for student affairs professionals. J Stud Aff Res Pract. 48(1), 47–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges SW (2007). The polyvagal perspective. Biological Psychology, 74, 116–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, & Berridge KC (2008). Review. The incentive sensitization theory of addiction: Some current issues. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 363(1507), 3137–3146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141(1), 105–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R (2011). New findings on biological factors predicting addiction relapse vulnerability. Current Psychiatry Reports, 13(5), 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fuse T, Aubin LR, & O’Malley SS (2000). Psychological stress, drug-related cues and cocaine craving. Psychopharmacology. 152(2), 140–148. [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline followback: A technique for assessing self-reported alcohol consumption In Allen RZLJ (Ed.). Measuring alcohol consumption: Psychosocial and biological methods (pp. 41–72). New Jersey: Humana Press. [Google Scholar]
- Sobell LC, & Sobell MB (2015). Excel Generic Quantitative Behaviors TLFB PC 2015. https://www.nova.edu/gsc/forms/timeline-followback-forms.html.
- Stanhope V (2018). Implementing SBIRT for adolescents within community mental health organizations: A mixed methods study. Journal of Substance Abuse Treatment, 90, 38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiffany ST, & Wray JM (2012). The clinical significance of drug craving. Annals of the New York Academy of Sciences, 1248, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G, Shi J, Chen N, et al. (2013). Effects of length of abstinence on decision-making and craving in methamphetamine abusers. PLoS One, 8(7), e68791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, & Bowen S (2010). Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology, 78(3), 362–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker TL, Samuelson KW, Muench F, Greenberg MA, & Gevirtz RN (2009). The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: a pilot study. Applied Psychophysiology & Biofeedback, 34(2), 135–143. 10.1007/s10484-009-9085-2. [DOI] [PubMed] [Google Scholar]


