Abstract
Objective
To evaluate the clinical effect of the one‐stage repair of a posterior oblique ligament avulsion fracture combined with a medial collateral ligament injury.
Methods
This study was a retrospective trial. From February 2007 to May 2017, five patients with posterior oblique ligament avulsion fracture combined with medial collateral ligament injury were included in this study. The patients were aged 37–58 years old with a mean of 45.2 years. All patients underwent the primary repair of a posterior oblique ligament avulsion fracture and medial collateral ligament injury. The main observational index included Lysholm score, International Knee Documentation Committee (IKDC) score, Visual Analogue Scale (VAS) score, and range of motion (ROM).
Results
The results showed that the average time of follow‐up was 53.6 months (range, 20–86 months). When compared to preoperative scores, the preoperative Lysholm score was significantly increased (47.8 ± 5.1 vs 95.0 ± 3.7, P < 0.05), the IKDC score was significantly increased (51.2 ± 5.6 vs 88.6 ± 4.2, P < 0.05), the VAS score was significantly decreased (7.0 ± 0.7 vs 0.4 ± 0.5, P < 0.05), and the ROM was significantly increased (91.6° ± 8.4° vs 129.9° ± 4.4°, P < 0.05).
Conclusion
Our study found that with the combination of the one‐stage repair of a posterior oblique ligament (POL) avulsion fracture and medial collateral ligament injury, the patient's postoperative function recovered well, their pain was relieved, and their knee joint stability was reliable.
Keywords: Avulsion fracture, Clinical analysis, Medial collateral ligament, One‐stage repair, Posterior oblique ligament
Introduction
The knee joint is the largest and most complex joint in the human body. Its stability and good biomechanical function depend on the surrounding muscles and ligaments. The posteromedial complex (PMC) is the last 1/3 of the medial structure of the knee joint: the area between the posterior edge of the medial collateral ligament (MCL) and the medial edge of the posterior cruciate ligament 1 . The dynamic stabilizing structure includes “goosefoot” (spelt muscle, gracilis, semitendinosus), semimembranosus, and the medial head of the gastrocnemius.
The static stability structure includes the posterior oblique ligament (POL), oblique ligament, posteromedial joint capsule, and medial half‐moon. POL also has a significant effect on its static stability on the back angle of the plate. The concept of POL was first proposed by Hughston and Eilers in 1973 2 and was defined as the collagen fiber structure behind the MCL. During this time, it was found that POL is significantly different from the superficial femoral stop of MCL and is an independent thickened joint capsule ligament. More studies have also shown that POL is a structure that is different in anatomy and function from the superficial collateral ligament 2 , 3 , 4 ; it is the main static stability structure of the knee joint. POL injuries are often combined with other injuries when the knee is everted and rotated. Studies have shown that after experiencing an MCL injury, POL bears an increase in the valgus load. Simultaneous injury of the superficial medial collateral ligament and posterior oblique ligaments can cause severe acute and chronic knee valgus instability and anterior rotatory instability (AMRI) 5 , thereby showing the role of POL in the static stability of the medial knee joint. Some clinicians think that POL is not an independent anatomical structure and, therefore, pay insufficient attention to it. However, some studies have shown that in patients with MCL injury and POL injury, only repairing the MCL without treating the POL injury often fails to reconstruct the stability of the knee joint 6 . Therefore, repair or reconstruction after experiencing a POL injury is necessary.
POL ligament injury is common in a clinical setting. However, the avulsion fractures of the femoral attachment point of POL are still rare. We retrospectively analyzed five cases of posterior oblique ligament avulsion fracture combined with medial collateral ligament injury from February 2007 to May 2017. The POL avulsion fracture was not the same as the MCL attachment point. All patients underwent the primary repair of posterior oblique ligament avulsion fracture and medial collateral ligament injury.
The purposes of study were as follows: (i) retrospectively analyze five cases of posterior oblique ligament avulsion fracture combined with medial collateral ligament injury; (ii) evaluate the clinical effect of the one‐stage repair of a posterior oblique ligament avulsion fracture combined with a medial collateral ligament injury by Lysholm score, International Knee Documentation Committee (IKDC) score, Visual Analogue Scale (VAS) score, and range of motion (ROM); and (iii) to evaluate the safety of the one‐stage repair of a posterior oblique ligament avulsion fracture combined with a medial collateral ligament injury.
Materials and Methods
Subjects
This study was a retrospective trial. From February 2007 to May 2017, five patients with posterior oblique ligament avulsion fracture combined with medial collateral ligament injury were included in this study.
Inclusion and Exclusion Criteria
Inclusion criteria: (i) patients with a posterior oblique ligament avulsion fracture combined with medial collateral ligament injury; (ii) patients that underwent the primary repair of the posterior oblique ligament avulsion fracture and medial collateral ligament injury; (iii) the main outcomes included Lysholm score, IKDC score, VAS score, and ROM.
Exclusion criteria: (i) patients with concomitant injuries or severe fractures around the knee joint; (ii) patients with lost clinical data; and (iii) patients who refused to receive surgery and chose conservative treatment.
Surgical Methods
All patients underwent the primary repair of the posterior oblique ligament avulsion fracture and medial collateral ligament injury. The surgery was performed by the same physician. Spinal anesthesia was given to the patient, who was then placed in the supine position, a tourniquet was used on the limb femur 1/3, and the patient’s knee stability was checked and confirmed under anesthesia.
Posterior Oblique Ligament Avulsion Fracture Suture
Revealing the posterior medial structure of the knee joint, distinguishing the superficial and deep structures of the medial collateral ligament, the posterior oblique ligament is the posterior medial structure rather than the medial structure and is approximately triangular. After confirming the posterior oblique ligament avulsion fracture, the 3.5 mm band anchor was used to reset the posterior oblique ligament avulsion fracture block to the femoral attachment; the ligament tissue was reinforced with the surrounding tissue and the soft tissue of the bone surface was reinforced by a suture with the anchor tail.
Confirming the Location of the Medial Collateral Ligament Tear
A 6–8 cm incision was made from the medial femoral condyle of the knee joint to the upper part of the sacral goosefoot and the medial structure of the knee joint was gradually revealed to confirm the location of the medial collateral ligament tear. Five medial collateral ligament tears were located at the femoral end and were repaired with a suture with a wire anchor; the medial joint capsule was also repaired.
Superficial and Deep Suture of the Medial Collateral Ligament
In the surgery process of these participants, a curved medial skin incision was directed from the medial femoral epicondyle to the medial proximal tibia. The fascia was exposed and incised; it was found that the medial collateral ligament (MCL) was ruptured and the POL was injured at the adductor tubercle with a bony fragment (Fig. 1). The POL and MCL had distinctly different bony attachment points. The bony fragment with the POL was reattached to the insertion site using a 3.5 mm suture anchor. The ligament was sutured with the surrounding and the soft tissue of the bone surface was closed by the sutures. At the femoral attachment site of the medial collateral ligament, the 5 mm suture anchor was wrung and sutured to the medial collateral ligament. The remaining stitches were sutured to the surrounding soft tissue (Fig. 2). During the period immediately following the surgery, the valgus stress test was (−) and ROM was 0° to 120°. The medial femur support band was repaired, the patella trajectory was normal, and there was no dislocation.
Figure 1.
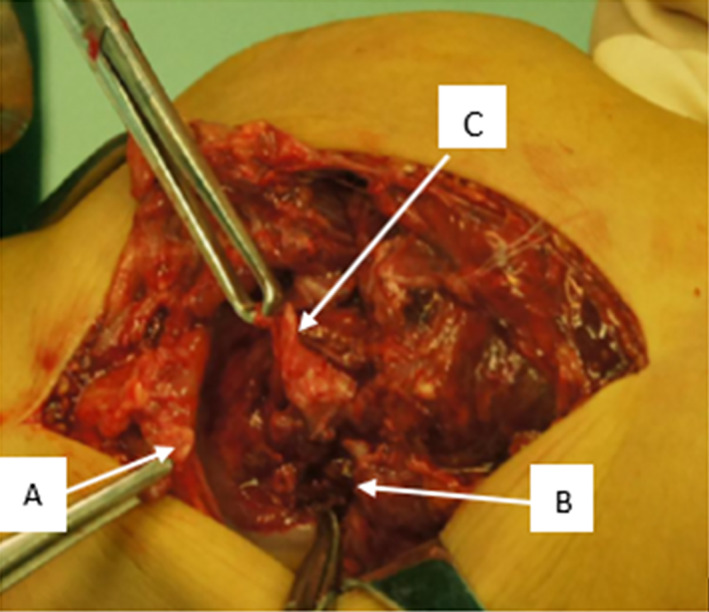
(A) Posterior oblique ligament (POL) was ruptured at adductor tubercle with a bony fragment. (B) The femoral attachment site of POL; (C) medial collateral ligament injury (MCL) injury.
Figure 2.
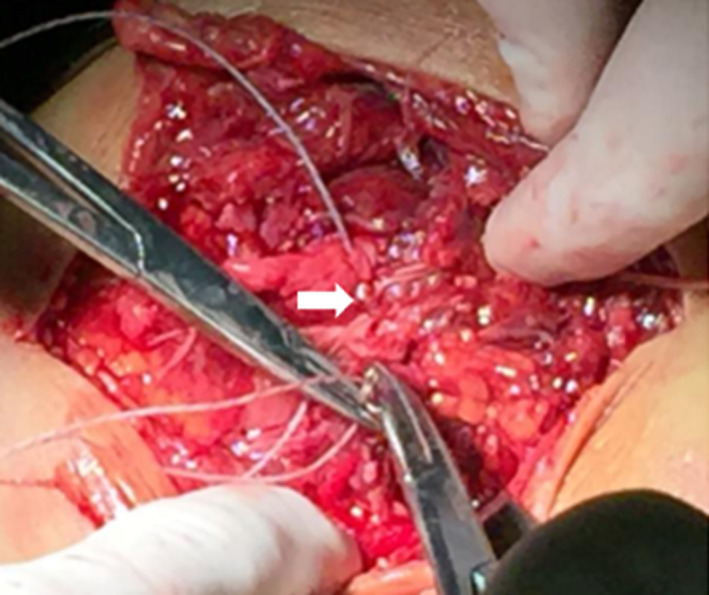
The bony fragment with Posterior oblique ligament (POL) was reattached to the region of the adductor tubercle using a 3.5 mm rivet (white arrow).
Postoperative Treatment
A postoperative protective knee brace was given to the patients to use for 4–6 weeks. On the first day after the operation, the knee extension pump training was started in order to prevent knee joint adhesion; the allowable range of motion of the knee joint is 0° to 90° within 2 to 3 weeks and then gradually increases. After 4 weeks, the full range of activities is allowed and partial weight bearing is permitted. Full weight training is suggested after 6 weeks and the removal of the brace was allowed within 8 weeks. The patients' physical activity can be fully restored after 6 months.
Efficacy Evaluation
Slocum Test
All patients underwent the Slocum test to evaluate the stability of the anterior medial rotation of the knee joint, that is, the knee joint 30° flexion before the drawer test and the internal rotation of the lower limb. If there was a lateral subluxation of the medial tibial plateau, it indicated that there was instability of the anterior medial rotation.
The Knee Function
In this study, the knee function was evaluated by the Lysholm score, IKDC score, VAS score, and ROM. These scores can be used to evaluate the knee function based on the reality of the patient's daily life. The follow‐up was conducted by telephone or outpatient once a week.
Lysholm Knee Score
The Lysholm knee score, first introduced into the medical community in 1982 and modified in 1985, remains one of the most frequently used assessment tools for the results of ACL reconstruction even though it only measures activities of daily living (ADL). Eight factors are rated to produce an overall score on a point scale of 0 to 100. Then an assignment is given as “excellent” for 95 to 100 points, “good” for 84 to 94 points, “fair” for 65 to 83 points, or “poor” for less than 65 points. The factors of limp, support, and locking are worth a potential of 23 points; pain and instability, 25 points each; swelling and stair climbing, 10 points each; and squatting, 5 points. The symptoms of pain, swelling, and instability are graded according to the activity in which they occur.
Knee Documentation Committee Subjective Knee Form (IKDC) Score
Originally published in 1993 in the American Journal of Knee Surgery and most recently revised in 2001 in The American Journal of Sports Medicine, the International Knee Documentation Committee Subjective Knee Form (IKDC) was designed to assess patients with a variety of knee disorders including ligamentous and meniscal injuries as well as patellofemoral pain and osteoarthritis. The IKDC is a patient‐completed tool, which contains sections on knee symptoms (seven items), function (two items), and sports activities (two items). Scores range from 0 points (lowest level of function or highest level of symptoms) to 100 points (highest level of function and lowest level of symptoms).
Visual Analogue Scale (VAS)
The pain VAS is a unidimensional measure of pain intensity, which has been widely used in diverse adult populations, including those with rheumatic diseases. Using a ruler, the score is determined by measuring the distance (mm) on the 10‐cm line between the “no pain” anchor and the patient's mark, providing a range of scores from 0–100. Score interpretation: a higher score indicates greater pain intensity. Based on the distribution of pain VAS scores in postsurgical patients (knee replacement, hysterectomy, or laparoscopic myomectomy) who described their postoperative pain intensity as none, mild, moderate, or severe, the following cut points on the pain VAS have been recommended: no pain (0–4 mm), mild pain (5–44 mm), moderate pain (45–74 mm), and severe pain (75–100 mm). Normative values are not available.
Range of Motion (ROM)
Normal knee range of motion usually refers to how much the knee bends and straightens. The most accurate way to measure knee range of motion is to use a goniometer. A goniometer is essentially a specially designed protractor that measures joint angles. Place the axis of the goniometer over the lateral femoral epicondyle. Line the stationary arm of the goniometer up with the greater trochanter along the outer thigh. Line the other arm of the goniometer up with the lateral malleolus of the ankle. Knee flexion and extension range of motion (ROM) is necessary for functional and sport‐specific activities.
Statistical Methods
The IBM SPSS 21.0 version software was used for statistical analyses of the indices. A paired t‐test was utilized for the data between the preoperative and postoperative results, such as Lysholm score, IKDC score, VAS score, and ROM. Data were expressed as mean ± standard deviation (Mean ± SD). A P‐value of less than 0.05 was considered statistically significant.
Results
General Characteristics
A total of five patients were included in this study. There were four males and one female, aged 37–58 years, with an average of 45.2 years old. All patients underwent one repair of the posterior oblique ligament avulsion fracture and medial collateral ligament injury. The average follow‐up time was 53.6 months (range, 20–86 months) (Table 1).
Table 1.
The patients' characteristics
| Case | Sex | Age | Lysholm sore | IKDC | VAS | ROM | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||
| 1 | Male | 58 | 48 | 97 | 52 | 86 | 7 | 0 | 93 | 130 |
| 2 | Male | 50 | 44 | 91 | 46 | 94 | 7 | 1 | 81 | 127.5 |
| 3 | Male | 39 | 48 | 99 | 44 | 83 | 8 | 0 | 99 | 135 |
| 4 | Male | 37 | 42 | 90 | 55 | 87 | 7 | 0 | 102 | 134 |
| 5 | Female | 42 | 57 | 98 | 59 | 93 | 6 | 1 | 83 | 123 |
IKDC, International Knee Documentation Committee score; ROM, range of motion; VAS, Visual Analogue score.
Knee Function Outcomes
Lysholm Score
The preoperative Lysholm score was 47.8 ± 5.1, the postoperative Lysholm score was 95.0 ± 3.7, the postoperative Lysholm score was 47.2 higher than the preoperative Lysholm score (P = 0.00001).
Knee Documentation Committee Subjective Knee Form (IKDC) Score
The preoperative IKDA score was 51.2 ± 5.6, the postoperative IKDA score was 88.6 ± 4.2, the postoperative IKDA score was 37.4 higher than the preoperative IKDA score (P = 0.0002).
Visual Analogue Scale (VAS)
The preoperative VAS score was 7.0 ± 0.7, the postoperative VAS score was 0.4 ± 0.5, the postoperative VAS score was 6.6 higher than the preoperative VAS score (P = 0.0002).
Range of Motion (ROM)
The preoperative ROM was 91.6° ± 8.4°, the postoperative ROM was 129.9° ± 4.4°, the postoperative ROM was 38.3° higher than the preoperative ROM (P = 0.0001).
Slocum Test
In all five patients, the preoperative Slocum Test was (+), the postoperative Slocum Test was (−).
Complications
Among these participants, no complications were found after the surgery, such as infection, bleeding, liver dysfunction, etc.
Typical Case Analysis
General Characteristics
A 58‐year‐old male had an accident on his way to a farm. His right knee sustained high‐energy valgus stress at the extended position, resulting in a slight swelling, pain, and increased medial gapping of the right knee. After the injury, when he stood up and walked, his lower leg presented with eversion and he fell again. The patient had no history of diseases and no knee‐related problems, such as osteoarthritis.
Examination
The patient was examined immediately after the injury. His right knee was slightly swollen, the medial joint gapping tenderness was (+), the anterior and posterior drawer test was (+), the valgus stress test was (+), ROM was 0 to 93 degrees, the Lachman was (+), and the Slocum test was (+). The Lysholm score: was 48 points; IKDC score was 52 points; VAS score was 7 points. The initial diagnosis was an injury of the medial collateral ligament of the right knee and an injury of the posterior medial structure of the right knee. On the anteroposterior plain radiographs, there were no abnormal findings, but a bony fragment was present at the posteromedial aspect of the femur on the lateral radiographs. The valgus stress position showed a significant increase in the medial joint gap opening (Fig. 3). Plain radiographs also showed the presence of a bony fragment at the adductor tubercle of the femur (Fig. 4). The medial collateral ligament injury was seen on the computed tomography (CT) image (Fig. 5).
Figure 3.
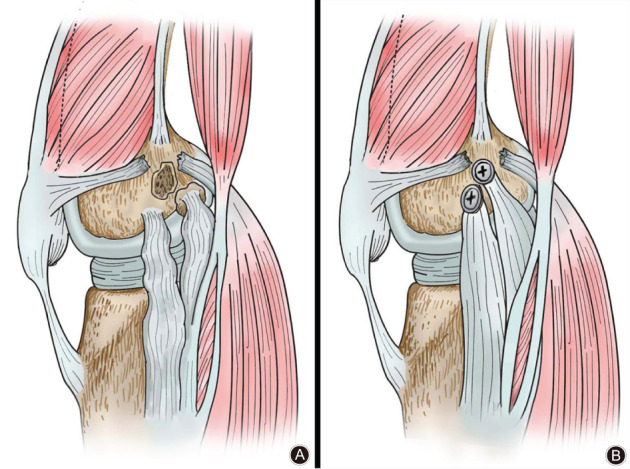
Schematic illustration of the key procedure in surgery. (A) POL was ruptured at adductor tubercle with a bony fragment, and MCL injury. (B) Using a 3.5 mm rivet to fix the bony fragment with POL.
Figure 4.

Plain radiographs of the right knee immediately after injury. (A) Anteroposterior Radiographs; (B) Lateral Radiograph, a bony fragment was present at the posteromedial aspect of the femur (white arrow); (C): Valgus Stress Radiographs, increasing medial compartmental gapping (white arrow).
Figure 5.
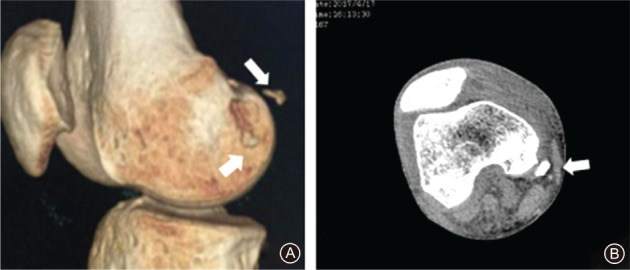
Preoperative CT image of the injured knee. A bony fragment was located at the posteromedial aspect of the femur (white arrow).
Treatment
After definite diagnosis, the patient received the primary repair of the posterior oblique ligament avulsion fracture and medial collateral ligament injury. After the treatment, the X‐ray of the patient's right knee showed that the posterior oblique ligament avulsed fracture was restored well (Figs 6, 7).The knee was immobilized for 2 weeks and then ROM exercises were started. Weight‐bearing was permitted 3 weeks after the surgery and 6 weeks after the operation, the clinical examination revealed normal ROM, no medial instability was present, the Lachman test was negative, and the anterior and posterior drawer test was (−). Twenty months after the operation, ROM was 0 to 130. The Lysholm score was 97 points; IKDC score was 86 points; VAS score was 0 points; and the patient returned to his regular daily life.
Figure 6.
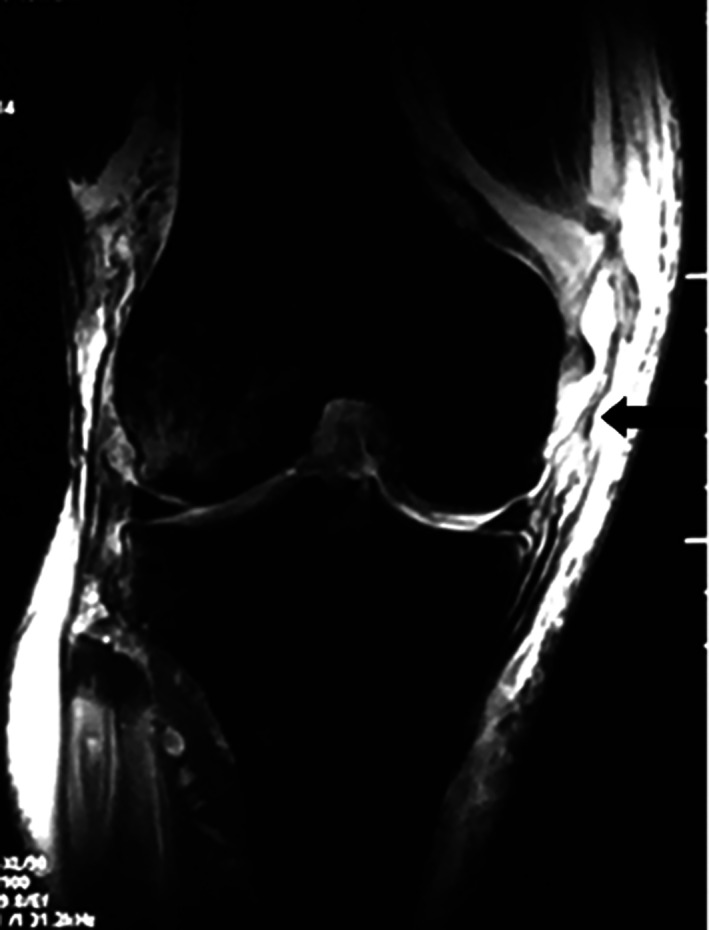
Preoperative T2‐weighted MRI of the right knee:Medial collateral ligament (MCL) and Posterior oblique ligament (POL) injury (black arrow).
Figure 7.
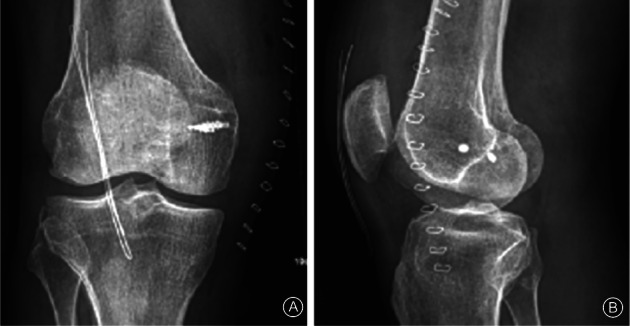
Postoperation radiograph of the right knee. (A) Anteroposterior radiographs, (B) Lateral radiograph. The X‐ray showed that the posterior oblique ligament avulsed fracture was restored well.
Discussion
The knee joint is the largest and most complex joint in the human body. Its stability and good biomechanical function depend on the surrounding muscles and ligaments. The PMC is the posterior third of the medial structure of the knee joint, including a static stable structure and a dynamic stable structure. The dynamic stabilizing structure includes “goosefoot” (spelt muscle, gracilis, semitendinosus), semimembranosus, and the medial head of the gastrocnemius. The static stability structure includes the POL, oblique ligament, posteromedial joint capsule, and medial half‐moon. POL also has a significant effect on its static stability on the back angle of the plate 7 .
However, POL is a controversial structure that some clinicians do not consider as independent anatomy. Loredo et al. confirmed the presence of POL structures by MRI studies 4 . Fischer et al. also confirmed, by anatomical studies, that the POL structure is independent 3 . Hughston et al. showed that POL originated from the femoral adductor nodules, while the MCL originated from the medial malleolus and the anterior and distal adductor nodules were approximately 1 cm 2 . However, some studies have suggested that the starting point of the POL is located at the distal end and the posterior aspect of the muscle nodules 5 , 8 .
The posterior oblique ligament includes three fascia structures: joint capsule bundle, shallow bundle, and central bundle. They extend to the distal end of the semimembranosus tendon, fuse with the posteromedial joint capsule, and enhance its function 8 , 9 . Hughston and Eilers pointed out that the central bundle of the posterior oblique ligament is the largest and thickest of the POL three fascia structures, therefore, it is of the utmost importance 2 . POL is an important stable structure of the knee joint PMC. Its main function is to limit the internal rotation of the tibia. It also plays an important role in resisting valgus and external rotation. POL and posterior cruciate ligament (PCL) cooperate to limit the femur shift. When the PCL has functional defects, POL is an important ligament that limits the posterior movement of the femur 9 , 10 .
The PMC examination mainly uses the knee valgus stress test and the Slocum test 11 . The knee joint valgus stress test at 0° and 30° knee flexion were used to examine the damage of the medial structure. If there was valgus instability when the knee was only 30°, it indicated that the MCL injury was simple and the PMC structure was intact. If the 0° and 30° knee flexion were unstable, the PMC injury was suggested. The PMC injury also often occurs in the anterior medial rotatory instability (AMRI) of the knee joint, that is, the knee joint is unstable at the knee flexion 30° under the valgus stress and the anterior medial subluxation occurs on the medial tibial plateau 11 , 12 . This rotational instability makes it possible to distinguish it from the enlargement of the medial joint space when knee valgus is caused by a simple MCL injury 13 , 14 .
When the superficial MCL (sMCL) and POL are simultaneously damaged, severe acute and chronic AMRI can be produced. Most of the simple sMCL lesions are treated well after conservative treatment. However, patients with sMCL and POL injury have chronic instability in the knee joint. Conservative treatment may cause knee function limitation and accelerate the development of osteoarthritis 15 . Previous clinical studies have found that only repairing MCL without repairing POL cannot completely restore the static stability of the knee joint 2 , 16 , since, with a separate MCL damage, POL has become an important stable structure for controlling the rotation and valgus stress in the knee 5 , 17 , 18 .
POL injury is not clinically uncommon. Sims et al. reported their findings in a study of 620 patients with surgically‐treated knee joint medial structure injury, of which 93 (15%) required reoperation for clinical or functional AMRI in the knee joint. Of the 93 patients, 31 had sMCL injury and dMCL injury. In 93 cases, there were 65 cases of semimembranosus tendon injury, 92 cases of POL injury (99%) 19 . In another study, almost all patients with ACL and MCL injuries who underwent surgery had POL injuries 20 .
Common POL injuries in the clinic include the partial or complete rupture of the ligament, avulsion fracture of the femur, and chronic injury 21 , 22 , 23 , 24 . Avulsion fractures of the POL femoral end are rare. When we searched PUBMED, NCBI, and CNKI databases, we only found a document on POL femoral avulsion fractures 6 . In this study, they repaired MCL injury and POL femoral avulsion fracture through one‐stage repair. The patients' ligament and activity recovered well after the operation and the normal function was restored. The POL and MCL femur attachment points were found to be significantly different during surgery, confirming that POL and MCL are two separate structures and the clinical importance of POL should be considered and valued. Understanding the anatomy of the inside of the knee, grasping the correct indications for surgery, and mastering the precise surgical techniques are the keys to good results.
Limitations
There were several limitations in this study. Firstly, this trial was not a randomized controlled trial. Secondly, this study was only a single‐center trial and the sample size was limited. Another multi‐center randomized controlled trial with large sample size about the efficacy of the one‐stage repair of a posterior oblique ligament avulsion fracture combined with a medial collateral ligament injury is still needed in the future.
Conclusion
Our study showed that when MCL injury combined with a POL avulsion fracture, the patients' pain was relieved after the one‐stage repair, their knee joint stability was restored, and their clinical efficacy was significantly improved.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Grant Sources: This research was financially supported by the Shanxi Provincial Department of Human Resources and Social Security (approval no. 2017–19).
Disclosure: We declare that we have no conflict of interest.
References
- 1. Lundquist RB, Matcuk GR Jr, Schein AJ, et al Posteromedial corner of the knee: the neglected corner. Radiographics, 2015, 35: 1123–1137. [DOI] [PubMed] [Google Scholar]
- 2. Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am, 1973, 55: 923–940. [PubMed] [Google Scholar]
- 3. Fischer RA, Arms SW, Johnson RJ, Pope MH. The functional relationship of the posterior oblique ligament to the medial collateral ligament of the human knee. Am J Sports Med, 1985, 13: 390–397. [DOI] [PubMed] [Google Scholar]
- 4. Loredo R, Hodler J, Pedowitz R, Yeh LR, Trudell D, Resnick D. Posteromedial corner of the knee: MR imaging with gross anatomic correlation. Skeletal Radiol, 1999, 28: 305–311. [DOI] [PubMed] [Google Scholar]
- 5. Wijdicks CA, Griffith CJ, RF LP, et al Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med, 2009, 37: 1771–1776. [DOI] [PubMed] [Google Scholar]
- 6. Kuroda R, Muratsu H, Harada T, et al Avulsion fracture of the posterior oblique ligament associated with acute tear of the medial collateral ligament. Arthroscopy, 2003, 19: E18. [DOI] [PubMed] [Google Scholar]
- 7. Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am, 1979, 61: 56–62. [PubMed] [Google Scholar]
- 8. LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am, 2007, 89: 2000–2010. [DOI] [PubMed] [Google Scholar]
- 9. Tibor LM, Marchant MH Jr, Taylor DC, Hardaker WT Jr, Garrett WE Jr, Sekiya JK. Management of medial‐sided knee injuries, part 2: posteromedial corner. Am J Sports Med, 2011, 39: 1332–1340. [DOI] [PubMed] [Google Scholar]
- 10. Petersen W, Loerch S, Schanz S, Raschke M, Zantop T. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament‐deficient knee. Am J Sports Med, 2008, 36: 495–501. [DOI] [PubMed] [Google Scholar]
- 11. Slocum DB, Larson RL. Rotatory instability of the knee: its pathogenesis and a clinical test to demonstrate its presence 1968. Clin Orthop Relat Res, 2007, 454: 5–13. [DOI] [PubMed] [Google Scholar]
- 12. Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior–posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am, 1980, 62: 259–270. [PubMed] [Google Scholar]
- 13. Bauer KL, Stannard JP. Surgical approach to the posteromedial corner: indications, technique, outcomes. Curr Rev Musculoskelet Med, 2013, 6: 124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Geiger D, Chang EY, Pathria MN, Chung CB. Posterolateral and posteromedial corner injuries of the knee. Magn Reson Imaging Clin N Am, 2014, 22: 581–599. [DOI] [PubMed] [Google Scholar]
- 15. Kannus P. Long‐term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res, 1988, 226: 103–112. [PubMed] [Google Scholar]
- 16. Kim SJ, Lee DH, Kim TE, Choi NH. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br, 2008, 90: 1323–1327. [DOI] [PubMed] [Google Scholar]
- 17. Robinson JR, Bull AM, Thomas RR, Amis AA. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med, 2006, 34: 1815–1823. [DOI] [PubMed] [Google Scholar]
- 18. Cohen M, Astur DC, Branco RC. An anatomical three‐dimensional study of the posteromedial corner of the knee. Knee Surg Sports Traumatol Arthrosc, 2011, 19: 1614–1619. [DOI] [PubMed] [Google Scholar]
- 19. Sims WF, Jacobson KE. The posteromedial corner of the knee: medial‐sided injury patterns revisited. Am J Sports Med, 2004, 32: 337–345. [DOI] [PubMed] [Google Scholar]
- 20. Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med, 2006, 34: 1134–1140. [DOI] [PubMed] [Google Scholar]
- 21. Beltran J, Matityahu A, Hwang K. The distal semimembranosus complex: normal MR anatomy, variants, biomechanics and pathology. Skeletal Radiol, 2003, 32: 435–445. [DOI] [PubMed] [Google Scholar]
- 22. Tiftikçi U, Serbest S. Does the location of placement of meniscal sutures have a clinical effect in the all‐inside repair of meniscocapsular tears? J Orthop Surg Res, 2017, 12: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tiftikçi U, Serbest S. Repair of isolated horizontal meniscal tears with all‐inside suture materials using the overlock method: outcome study with a minimum 2‐year follow‐up. J Orthop Surg Res, 2016, 11: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tiftikci U, Serbest S, Kilinc CY, Karabicak GÖ, Vergili Ö. Return to work in miners following anterior cruciate ligament reconstruction. Pan Afr Med J, 2015, 22: 173. [DOI] [PMC free article] [PubMed] [Google Scholar]


