ABSTRACT
Food insecurity, a well-established determinant of chronic disease morbidity and mortality, is rapidly increasing due to the coronavirus disease 2019 (COVID-19) pandemic. We present a conceptual model to understand the multiple mechanisms through which the economic and public health crises sparked by COVID-19 might increase food insecurity and contribute to poor health outcomes in the short- and long-term. We hypothesize that, in the short-term, increased food insecurity, household economic disruption, household stress, and interruptions in healthcare will contribute to acute chronic disease complications. However, the impact of the pandemic on food security will linger after social-distancing policies are lifted and the health system stabilizes, resulting in increased risk for chronic disease development, morbidity, and mortality among food-insecure households in the long-term. Research is needed to examine the impact of the pandemic-related increase in food insecurity on short- and long-term chronic health outcomes, and to delineate the underlying causal mechanisms. Such research is critical to inform the development of effective programs and policies to address food insecurity and its downstream health impacts during COVID-19 and future pandemics.
Keywords: COVID-19, SARS-CoV-2, food insecurity, chronic disease, social-distancing, stay-at-home orders
See corresponding editorial on page 1160.
Introduction
Food insecurity is highly prevalent in the United States and has risen starkly as a result of the social-distancing policies and economic disruption brought on by the coronavirus disease 2019 (COVID-19) pandemic. Prior to COVID-19, 1 in 9 households in the United States were food insecure (1), which refers to having limited or uncertain access to adequate food (2). Food insecurity disproportionately affects households with children under 6 years of age, female-headed households, adults living alone, adults with disabilities, Black and Hispanic households, and low-income households (1, 3). Such populations are likely to experience even higher rates and more extreme forms of food insecurity during the pandemic and the resulting economic crisis, similar to the way in which these vulnerable populations experienced disproportionate increases in the prevalence, severity, and duration of food insecurity during the Great Recession (4, 5). Thus, increases in food-insecurity rates will likely persist among these populations after social-distancing policies are lifted and the economy stabilizes.
Changes in the depth and breadth of food insecurity during the COVID-19 pandemic could have serious and long-lasting health consequences. Food insecurity is associated with increased risk for chronic diseases such as HIV (6, 7), type 2 diabetes (8, 9), cardiovascular disease (10, 11), dyslipidemia (10, 12), and hypertension (10, 12), as well as chronic disease morbidity (13–17) and mortality (18, 19). Although the impact of COVID-19 on food-insecurity prevalence has been highly visible, the downstream impact on chronic disease will be more challenging to observe. Nonetheless, the pandemic may contribute to a rise in the burden of these chronic diseases as well as increased disease-related morbidity and mortality among individuals with existing chronic diseases. Further, given that chronic diseases such as diabetes and cardiovascular disease are risk factors for COVID-19 complications (20), food insecurity could elevate the risk for worse COVID-19 outcomes.
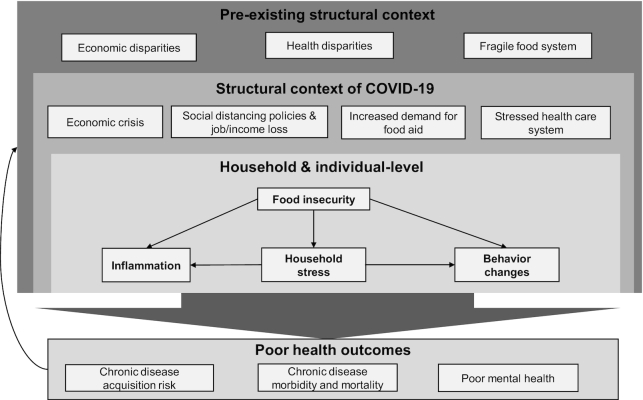
A sound understanding of the complex pathways through which the pandemic-related economic and public health crises contribute to food insecurity and poor health outcomes in the short- and long-term is critical to inform programs and policies that provide food and other support for the most vulnerable during the pandemic; such work may also inform how we approach future public health and economic crises. We propose a conceptual model to inform research priorities and guide the development of effective interventions and policies.
COVID-19 Pandemic and Food Insecurity
The impact of the COVID-19 pandemic on food insecurity and poor health outcomes is complex, multilevel, and bidirectional. Conceptual models are useful for depicting these complex relationships and facilitating analysis of hypothesized causal associations in multidimensional health problems (21, 22). Our conceptual model (Figure 1) demonstrates the multilevel (structural-, household- and individual-level) factors influencing food insecurity and health outcomes during the pandemic, drawing on prior work describing the relationship between food insecurity and health (21, 23).
FIGURE 1.
Social and structural impacts of COVID-19 on food insecurity and health outcomes. COVID-19, coronavirus disease 2019.
Structural context
Existing economic and health disparities
The impact of the COVID-19 pandemic on food insecurity and poor health outcomes occurs in the context of pre-existing economic and health disparities, largely driven by systemic racism (23–26). Prior to COVID-19, Black, Hispanic, and low-income households experienced a disproportionate burden of both food insecurity and chronic disease (1, 27, 28). For example, in 2018, the prevalence of food insecurity was highest among low-income (29.1%), non-Hispanic Black (21.2%), and Hispanic (16.2%) households, compared with 11.1% in the general population (1). These same populations also experience disproportionate rates of diabetes (27), obesity (28), hypertension (28), and HIV (29). Such disparities are driven by inequitable access to resources, including employment, food, housing, education, and healthcare (25, 30). It is within the context of existing health and economic disparities that we can begin to understand how the economic and public health crises of COVID-19 intersect at the household level, exacerbating existing disparities.
Fragile food system
At the same time, the COVID-19 pandemic has exposed fault lines in our existing food system. The US food system is oriented toward 2 separate modes of food consumption: one that supports household food preparation and consumption (e.g., grocery stores, farmers’ markets, food banks, etc.) and another designed for consumption in institutions and outside the home (e.g., restaurants, schools, businesses, etc.). The overnight shutdown of restaurants, schools, worksites, and many other institutions due to COVID-19 increased demand for food at home and created food supply disruptions in grocery stores and the charitable feeding system (e.g., food banks and pantries) (31). This rapid shift in demand simultaneously forced farmers to waste staggering amounts of fruits, vegetables, and dairy originally destined for consumption outside the home (32).
COVID-19 structural context
In addition to the structural context existing prior to the pandemic, COVID-19 introduces its own structural factors. Beginning in late February 2020, news of the spreading virus sparked a global economic crisis (33, 34). In mid-March 2020, municipalities and states across the United States began issuing stay-at-home orders to quell the spread of COVID-19 (35). The majority of such orders required the closure of schools, daycare facilities, and “nonessential” businesses, including dine-in restaurants, gyms, shopping malls, and movie theaters (35). As a result, the unemployment rate in the United States skyrocketed from 3.5% to over 14%, representing the highest levels of unemployment since the Great Depression (36). Many employees who have not been laid off are coping with reduced hours and income. In total, 43% of US adults report that they or someone in their household have lost a job or taken a pay cut because of COVID-19 (37). Lower-income adults report even higher (52%) rates of job upheaval (37).
As a result, the demand for food aid has substantially increased (31, 38, 39). For example, in Los Angeles County in California, the number of applicants for the Supplemental Nutrition Assistance Program (SNAP; formerly known as food stamps) has nearly doubled (39). Reports from across the country also suggest that demand for charitable food services (food banks, food pantries, and “soup kitchens”) has increased 50–140% since February 2020 (31, 38). At the same time, these resources are being stretched in their capacity to access donated food (31). Grocery stores, a main source of food donations to food banks and pantries, have less food to donate as they experience panic purchasing and people shift their dietary habits from eating in restaurants, workplaces, and schools to eating at home (31). As a result, some food banks are purchasing more food, driving up costs, and distributing less food per household (38, 40). Such pressure on the charitable food system may exacerbate rising food insecurity rates.
Finally, in places where COVID-19 has overwhelmed the health system, there may be limited capacity to support patients with non–COVID-related chronic health conditions. Prior research has documented interruptions in medical care and medication adherence during and after disasters such as hurricanes and earthquakes (41, 42). Furthermore, during this pandemic there is some evidence that people are avoiding clinical settings for fear of viral exposure. For example, data from the US Census Bureau suggests that 41.2% of households delayed accessing healthcare because of the pandemic (43). Such interruptions could have implications for both short- and long-term health outcomes (44).
Impact of the structural context of COVID-19 on food insecurity and health outcomes
Data from the US Census Bureau suggest that 38% of adults in the United States experienced an increase in food insecurity since mid-March 2020 when COVID-19 was declared a national emergency (43). These prevalence estimates are likely to increase as the economic crisis and stay-at-home orders persist. Indeed, unprecedented job and income loss sparked by the pandemic has left millions of Americans without the means to purchase the quantity and quality of food needed. At the same time, the price of food sold in grocery stores has increased, further preventing low-income households from accessing food (45). In addition, populations more vulnerable to COVID-19 complications, such as older adults and those with existing chronic diseases, may be unwilling or unable to access food due to fear of viral exposure, further driving food insecurity.
Food-insecure households generally rely on 4 broad strategies to maintain access to food, all of which may be severely impacted by the COVID-19 epidemic (23). First, households may make shifts within their own spending patterns to prioritize food—for example, putting off rent or utilities payments to pay for food (23). This strategy is less feasible when the entire household budget has been severely impacted. Second, households may rely on informal support from social networks (46). During a pandemic, this strategy may be less effective due to social-distancing policies and the desire to limit exposure to the virus. Third, households may access federal nutrition programs such as SNAP. For eligible households, this may be a particularly effective strategy, but benefit levels are often not adequate to fully meet household needs (23). Further, while new federal policies address the increasing demand for food aid during COVID-19, such as expanding SNAP eligibility, implementation has not begun in many states and new policies may not meet the needs of the most vulnerable (47). Finally, households may rely on the charitable food system. Historically, this system was designed to provide emergency food in times of crisis. However, even before COVID-19, national estimates suggest that millions of households were relying on the charitable food system to address long-term gaps in food access (48). Relying on the charitable food system over the long-term can create challenges related to shortages in food supply/donations; limited nutritious, culturally competent, or palatable food options; and accessibility (such as restricted service hours) (48, 49). COVID-19 has placed additional strain on this fragile system due to the sharp increase in demand, food supply disruptions, and volunteer shortages during stay-at-home orders (31, 40). As a result of these factors, the depth of food insecurity is worsening for many households, with implications for health.
Health impact of food insecurity during COVID-19 and beyond
Food insecurity is a risk factor for both short- and long-term health through 3 pathways: household stress, behavioral, and inflammatory pathways.
Household stress pathway
Food insecurity is a powerful stressor (50–52). Stress about where and how to access food will likely intersect with stress about job loss and strained finances, disconnection from social support systems, and worry about one's own health and the health of loved ones during the COVID-19 pandemic. Reports suggest intimate partner violence (IPV) has risen since stay-at-home orders went into effect, and experts expect child abuse to also rise, likely resulting from increased household stress and physical proximity brought on by stay-at-home orders (53, 54). Indeed, spikes in IPV and child abuse incidence have been documented during and following other natural disasters (e.g., earthquakes and hurricanes), due in part to increased household stress (55, 56). Similarly, food insecurity is also associated with increased risk for IPV, likely through a pathway of household stress (57). Violence, in turn, is associated with a number of acute and chronic health outcomes including injury, poor mental health (e.g., depression, anxiety, etc.), chronic conditions (e.g., diabetes, cardiovascular disease, etc.), and even death (58, 59).
Individuals experiencing food insecurity are also more likely to experience symptoms of depression (60, 61), anxiety (62), and post-traumatic stress disorder (PTSD) (62), as well as suicidality (60). Qualitative research suggests that financial and food insecurity can fuel feelings of sadness, shame, guilt, anxiety, and hopelessness (52, 63). In the context of COVID-19, it is likely that such feelings will be exacerbated by social isolation, anxiety about the health of oneself and one's loved ones, and stress about unemployment and financial and food insecurity (64). Poor mental health, in turn, contributes to risk for HIV infection (65, 66), and development of diabetes (67) and cardiovascular disease (68) through increased risk behaviors such as high-risk sexual behaviors (66), overeating or undereating (69), and physical inactivity (69). Poor mental health can also increase the risk of chronic disease morbidity and mortality (70, 71) through interruptions in healthcare, including reduced uptake of, and nonadherence to, antiretroviral medication for HIV and hypoglycemic medication for diabetes (61, 72).
Behavioral pathway
Food-insecure individuals engage in a number of strategies to manage their food insecurity, which may place them at increased risk for poor health outcomes in the short- and long-term. For example, some food-insecure individuals engage in high-risk sex such as condomless or transactional sex to access food, which increases the risk of HIV transmission (73, 74). Some food-insecure individuals avoid taking medications when they do not have enough food to eat due to increased side effects such as nausea or fear of adverse effects related to taking medication on an empty stomach (75). Such behaviors contribute to low medication adherence and could lead to disease progression (61, 75–81). Additionally, food-insecure individuals make trade-offs between using their limited resources to purchase food or purchase medications or medical care, resulting in cost-related medication nonadherence and interruptions in healthcare (75, 82). Such behaviors could be exacerbated during the COVID-19 pandemic; overwhelmed healthcare systems are less able to address the needs of chronically ill patients, and individuals may avoid health facilities or pharmacies to reduce viral exposure. Related adverse health outcomes in the short-term could increase the risk for the development of chronic disease or chronic disease complications in the long-term.
To save money, food-insecure individuals often consume cheaper, more-energy-dense foods (e.g., highly processed foods) instead of more expensive and nutritious fresh fruits and vegetables and lean proteins (83–85). Food-insecure individuals, particularly women, also report overeating when food is available to compensate for past deprivation (86). In the first few months of COVID-19, many households, regardless of food-security status, prioritized shelf-stable foods to hedge against supply gaps and reduce viral exposure by extending time between needing to visit grocery stores or food pantries. However, as the food supply disruptions and social-distancing policies lift, it is likely that higher-income households will return to their normal eating and purchasing habits. In contrast, lower-income households, who have borne the brunt of the economic crisis (37), will likely have to rely on shelf-stable and energy-dense foods for a longer period of time, as they did during the Great Recession (4, 5). Shelf-stable foods are generally highly processed and often contain high amounts of sodium, fat, and sugar. Sustained consumption of such foods is likely to partially explain the increased risk of obesity (86), diabetes (8), hypertension (10), and hyperlipidemia (10) observed in food-insecure households.
Individuals living in households experiencing more severe forms of food insecurity may reduce food or skip meals entirely (87). Undernutrition and micronutrient deficiency, although rarely observed in the United States, are associated with poor health outcomes in both the short- and long-term. For example, severe episodes of hypoglycemia among patients with diabetes are more common when food budgets are most likely to be exhausted (88). Disruptions in dietary intake may impact the absorption of certain medications, including some antiretroviral medications for HIV (89), increasing the risk of treatment failure and disease progression.
Inflammatory pathway
Finally, emerging evidence suggests that food insecurity may increase the risk of poor health outcomes through an inflammatory pathway (90, 91). Food insecurity has been independently associated with elevated concentrations of inflammatory markers C-reactive protein (11, 91), IL-6, and TNF receptor 1 (90), which have been linked to chronic diseases such as cardiovascular disease (92), HIV infection (93, 94), HIV progression, and non–AIDS-defining conditions among people living with HIV (93, 94). It is possible this association is driven by a stress response or dietary patterns related to food insecurity. As previously noted, food insecurity is a powerful stressor, and stress is associated with elevated levels of inflammation (95). Higher intake of fat and red and processed meat, as is typical among food-insecure households (85), is also associated with elevated levels of inflammation (96, 97). Both of these mechanisms are likely to be exacerbated during COVID-19, leading to elevated levels of inflammation. The inflammatory response also appears to be an important factor in COVID-19 disease severity (98).
Food insecurity and poor health: Cyclic and mutually reinforcing processes
In the context of COVID-19, links between food insecurity and poor mental and physical health are interconnected and mutually reinforcing. The pandemic can increase the risk of food insecurity due to rising unemployment and household economic disruption, social-distancing policies, and desire to avoid viral exposure. Food insecurity, in turn, increases the risk of chronic disease, including diabetes and cardiovascular disease, which places individuals at increased risk for COVID-19 complications (99, 100). Indeed, the fact that low-income and Black/African American and Hispanic households already experience disproportionate rates of food insecurity and chronic disease due to underlying health and economic disparities may partially explain why such populations are experiencing worse COVID-19 outcomes (101, 102). Finally, either chronic disease or COVID-19 and its sequelae, including severe cognitive dysfunction (103, 104), can limit capacity to maintain employment and increase financial insecurity through out-of-pocket healthcare expenses, ultimately increasing one's risk for food insecurity (3, 23).
Short-term and long-term impacts of COVID-19 on food insecurity and health outcomes
The various social and structural dynamics caused by the COVID-19 pandemic will have differential effects on short- and long-term health outcomes. Specifically, we posit that the social-distancing policies, stressed healthcare and food aid systems, job/income loss, and food insecurity will all contribute to worse health outcomes in the short-term. For example, someone with type 2 diabetes who has lost their job may become hypo- or hyperglycemic if they are unable to access the food or medications they need due to their limited income, the desire to avoid viral exposure, or the stressed healthcare system.
Ultimately, social-distancing policies will be relaxed and the health system will stabilize, but the negative impact of COVID-19 on the economy will likely persist for many years, particularly for low-income workers. First, persistent food insecurity and its associated sustained diet of cheap and energy-dense foods could lead to a rise in rates of chronic disease such as diabetes, obesity, and cardiovascular disease in the years following the COVID-19 outbreak. Second, sustained food insecurity could also lead to chronic mental health conditions such as depression (60, 61), anxiety (62), and PTSD (62), exacerbated by social isolation, stress, and job loss related to COVID-19 (64). Third, those with pre-existing chronic diseases will likely experience sustained challenges in chronic disease self-management, such as cost-related medication nonadherence or having to make trade-offs between accessing food or medication, which could lead to a rise in chronic disease morbidity and mortality. For example, people with stable jobs and controlled HIV prior to COVID-19 who subsequently lose their job for a long period of time and become food insecure may experience long-term barriers to HIV management and increased risk for AIDS-related morbidity and mortality. Fourth, short-term health problems resulting from the COVID-19 pandemic may have long-term sequelae. For example, a person with high blood pressure who has a hypertensive stroke during the pandemic may become permanently disabled. Similarly, a person experiencing acute complications from COVID-19 (such as renal failure) may experience long-term health sequelae that permanently affect employment capacity and therefore risk for food insecurity. Because the epidemic has mostly affected racial and ethnic minorities (101, 102), many of whom are low income, these populations will likely face the greatest long-term risk to their health, further exacerbating health disparities.
Research Implications
There is an urgent need to understand how the pandemic-related increase in food-insecurity prevalence and severity impacts short- and long-term health outcomes. Research should also assess how food insecurity and COVID-19 disease risk and severity are related, and how COVID-19–related disability may contribute to food insecurity. Such research should examine how the pandemic might exacerbate existing disparities in food insecurity and chronic health. This research is necessary to guide the development of programs and policies to meet the needs of food-insecure households during this time and in future public health and economic crises.
Further, we need to elucidate the relative contributions of financial insecurity, food insecurity, household stress, and healthcare interruptions in the development of worse short- and long-term health outcomes, including HIV- and diabetes-related morbidity and mortality. Such information can help public health practitioners and policymakers target their programs and policies to the factors that contribute the most to worse health outcomes.
Qualitative methods are needed to help us understand the lived experiences of food-insecure individuals and families during the pandemic. Such research will improve our ability to prepare for future pandemics by illuminating how households access food, cope with social distancing, and manage their mental and physical health during a public health crisis. Such research can also offer nuanced insights into the mechanisms linking the structural context of COVID-19 to food insecurity and poor health.
There is also a need to determine best practices, feasibility, and acceptability of food-insecurity interventions while social-distancing policies are in effect. We must study novel and cost-effective models for feeding a growing population of food-insecure individuals over time. We also need to assess the efficacy of combination interventions during the pandemic—for example, interventions that simultaneously address food insecurity and its downstream health impacts through food-support programs coupled with nutritional and behavioral counseling. Finally, policies that impact household budgets, such as the Earned Income Tax Credit and cash transfers, also address food insecurity (105, 106) and could serve as an important buffer for households against the COVID-19–related economic crisis.
Conclusions
The number of Americans experiencing food insecurity is rapidly rising due to the economic and public health crises sparked by the COVID-19 pandemic. We expect the pandemic-related increase in food insecurity will have downstream effects on chronic health outcomes through pathways of household stress, behavioral coping mechanisms, and inflammation. Ultimately, the pandemic will exacerbate existing disparities in food insecurity and chronic disease, which will persist after the pandemic. Public health research and programs are urgently needed to characterize and address the effects of the pandemic-related rise in food insecurity on health.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—HS, SDW, and KP: conceived of the project; AML: wrote the manuscript and had primary responsibility for final content; and all authors: read, edited, and approved the final manuscript. The authors report no conflicts of interest.
Notes
This work was supported by the National Institutes of Mental Health of the US Public Health Service under award number T32MH19105; the National Institute of Diabetes and Digestive and Kidney Diseases under award number P30DK092924; and the National Institute of Allergy and Infectious Diseases under award number K24AI134326. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations used: COVID-19, coronavirus disease 2019; IPV, intimate partner violence; PTSD, post-traumatic stress disorder; SNAP, Supplemental Nutrition Assistance Program.
Contributor Information
Anna M Leddy, Department of Medicine, University of California, San Francisco, San Francisco, CA, USA.
Sheri D Weiser, Department of Medicine, University of California, San Francisco, San Francisco, CA, USA.
Kartika Palar, Department of Medicine, University of California, San Francisco, San Francisco, CA, USA.
Hilary Seligman, Department of Medicine, University of California, San Francisco, San Francisco, CA, USA; Department of Epidemiology and Biostatistics, University of California, San Francisco, San Francisco, CA, USA.
References
- 1. Coleman-Jensen AR, Rabbitt MP, Gregory CA, Singh A. Household food insecurity in the United States in 2018, ERR-270. Washington (DC: ): US Department of Agriculture, Economic Research Service; 2019. [Google Scholar]
- 2. National Research Council Food insecurity and hunger in the United States: an assessment of the measure. Panel to review the U.S. Department of Agriculture's measurement of food insecurity and hunger. Washington (DC): The National Academies Press; 2006. [Google Scholar]
- 3. Coleman-Jensen AN, Rabbitt MP. Food insecurity among households with working-age adults with disabilities, ERR-144. Washington (DC): US Department of Agriculture, Economic Research Service; 2013. [Google Scholar]
- 4. Balistreri KS. A decade of change: measuring the extent, depth and severity of food insecurity. J Fam Econ Iss. 2016;37(3):373–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005–2012. PLoS One. 2017;12(6):e0179172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chop E, Duggaraju A, Malley A, Burke V, Caldas S, Yeh PT, Narasimhan M, Amin A, Kennedy CE. Food insecurity, sexual risk behavior, and adherence to antiretroviral therapy among women living with HIV: a systematic review. Health Care Women Int. 2017;38(9):927–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, Phaladze N, Iacopino V, Heisler M. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4(10):e260; discussion 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fitzgerald N, Hromi-Fiedler A, Segura-Perez S, Perez-Escamilla R. Food insecurity is related to increased risk of type 2 diabetes among Latinas. Ethn Dis. 2011;21(3):328–34. [PMC free article] [PubMed] [Google Scholar]
- 10. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ford ES. Food security and cardiovascular disease risk among adults in the United States: findings from the National Health and Nutrition Examination Survey, 2003–2008. Prev Chronic Dis. 2013;10:E202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830–9. [DOI] [PubMed] [Google Scholar]
- 13. Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, Hunt PW, Emenyonu NI, Mattson JE, Martin JN et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26(1):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Spinelli MA, Frongillo EA, Sheira LA, Palar K, Tien PC, Wilson T, Merenstein D, Cohen M, Adedimeji A, Wentz E et al. Food insecurity is associated with poor HIV outcomes among women in the United States. AIDS Behav. 2017;21(12):3473–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36(10):3093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Bataineh S, Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin Nutr. 2012;31(2):250–4. [DOI] [PubMed] [Google Scholar]
- 17. Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, Montaner JS, Hogg RS. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Anema A, Chan K, Chen Y, Weiser S, Montaner JS, Hogg RS. Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. PLoS One. 2013;8(5):e61277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Weiser SD, Palar K, Hatcher AM, Young S, Frongillo EA, Laraia B. Food insecurity and health: a conceptual frameworkIn: Ivers L.editor. Food insecurity and public health(pp. 23–50). Boca Raton (FL): CRC Press; 2015. [Google Scholar]
- 22. Victoria CGH, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26:224–7. [DOI] [PubMed] [Google Scholar]
- 23. Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the United States. Annu Rev Public Health. 2019;40:319–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389(10077):1475–90. [DOI] [PubMed] [Google Scholar]
- 25. Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- 26. Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7–14. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control Prevention Diabetes report card 2017. Atlanta (GA): CDC; 2018. [Google Scholar]
- 28. Centers for Disease Control and Prevention [cited May 10, 2020] [Internet]. Health, United States spotlight: Racial and ethnic disparities in heart disease. Available from: https://www.cdc.gov/nchs/hus/spotlight/HeartDiseaseSpotlight_2019_0404.pdf. [Google Scholar]
- 29. Centers for Disease Control and Prevention [cited May 14, 2020] [Internet]. HIV and African Americans. Available from: https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html. [Google Scholar]
- 30. Berkman LF, Kawachi I. Social epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- 31. Lakhani N. [cited April 10, 2020] [Internet]. “A Perfect Storm”: US facing hunger crisis as demand for food banks soars. Available from: https://www.theguardian.com/environment/2020/apr/02/us-food-banks-coronavirus-demand-unemployment. [Google Scholar]
- 32. Yaffe-Bellany DC, Corkery M[cited May 1, 2020] [Internet]. Dumped milk, smashed eggs, plowed vegetables: food waste of the pandemic. Available from: https://www.nytimes.com/2020/04/11/business/coronavirus-destroying-food.html. [Google Scholar]
- 33. Davies R, Partington R, Wearden G. [cited Apr 16, 2020] [Internet]. Coronavirus fears trigger biggest one-day fall on US stock market. Available from: https://www.theguardian.com/business/2020/feb/27/coronavirus-could-trigger-damage-on-scale-of-2008-financial-crisis-covid-19. [Google Scholar]
- 34. Lederer EM. [cited May 15, 2020] [Internet]. U.N. forecasts pandemic to shrink world economy by 3.2%. Available from: https://www.pbs.org/newshour/economy/u-n-forecasts-pandemic-to-shrink-world-economy-by-3-2. [Google Scholar]
- 35. Kaiser Family Foundation [cited Apr 4, 2020] [Internet]. State data and policy actions to address coronavirus. Available from: https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/. [Google Scholar]
- 36. Bureau of Labor Statistics [cited May 11, 2020] [Internet]. The employment situation-- June 2020. Available from: https://www.bls.gov/news.release/pdf/empsit.pdf. [Google Scholar]
- 37. Parker K, Horowitz JM, Brown A. [cited Apr 27, 2020] [Internet]. About half of lower-income Americans report household job or wage loss due to COVID-19. Available from: https://www.pewsocialtrends.org/2020/04/21/about-half-of-lower-income-americans-report-household-job-or-wage-loss-due-to-covid-19/. [Google Scholar]
- 38. Kulish N. [cited May 15, 2020] [Internet]. “Never seen anything like it”: cars line up for miles at food banks. Available from: https://www.nytimes.com/2020/04/08/business/economy/coronavirus-food-banks.html. [Google Scholar]
- 39. McGreevy P. [cited May 11, 2020] [Internet]. Demand for food stamps surges in California as virus takes economic toll. Available from: https://www.latimes.com/california/story/2020-03-31/california-demand-food-stamps-calfresh-coronavirus. [Google Scholar]
- 40. Lakhani NS, Singh M, Salam E [cited May 5, 2020] [Internet]. “We may have to ration”: US food banks face shortages as demand surges. Available from: https://www.theguardian.com/us-news/2020/apr/17/us-food-banks-over-budget-demand-coronavirus. [Google Scholar]
- 41. Krousel-Wood MA, Islam T, Muntner P, Stanley E, Phillips A, Webber LS, Frohlich ED, Re RN. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336(2):99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Clark RA, Besch L, Murphy M, Vick J, Gurd C, Broyles S, Lincoln K. Six months later: the effect of Hurricane Katrina on health care for persons living with HIV/AIDS in New Orleans. AIDS Care. 2006;18(Suppl 1):59. [DOI] [PubMed] [Google Scholar]
- 43. US Census Bureau [cited May 21, 2020] [Internet]. Household pulse survey data tables. Available from: https://www.census.gov/programs-surveys/household-pulse-survey/data.html. [Google Scholar]
- 44. Rothfeld MS, Sengupta S, Goldstein J, Rosenthal BM [cited May 3, 2020] [Internet]. 13 Deaths in a Day: an 'Apocalyptic' Coronavirus Surge at an N.Y.C. Hospital. https://www.nytimes.com/2020/03/25/nyregion/nyc-coronavirus-hospitals.html. [Google Scholar]
- 45. USDA [cited Apr 27, 2020] [Internet]. Summary findings: food price outlook, 2020. Available from: https://www.ers.usda.gov/data-products/food-price-outlook/summary-findings.aspx. [Google Scholar]
- 46. Martin KS, Rogers BL, Cook JT, Joseph HM. Social capital is associated with decreased risk of hunger. Soc Sci Med. 2004;58(12):2645–54. [DOI] [PubMed] [Google Scholar]
- 47. USDA [cited Apr 30, 2020] [Internet]. FNS actions to respond to COVID-19. Available from: https://www.fns.usda.gov/disaster/pandemic/covid-19. [Google Scholar]
- 48. Weinfield NSM, Mills G, Borger C, Gearing M, Macaluso T, Montaquila J, Zedlewski S. Hunger in America 2014: national report. Chicago (IL): Feeding America; 2014. [Google Scholar]
- 49. Gany F, Bari S, Crist M, Moran A, Rastogi N, Leng J. Food insecurity: limitations of emergency food resources for our patients. J Urban Health. 2013;90(3):552–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136(1):177–82. [DOI] [PubMed] [Google Scholar]
- 51. Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–68. [DOI] [PubMed] [Google Scholar]
- 52. Knowles M, Rabinowich J, Ettinger de Cuba S, Cutts DB, Chilton M. "Do you wanna breathe or eat?": parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern Child Health J. 2016;20(1):25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Taub A. [cited May 11, 2020] [Internet]. A new COVID-19 crisis: domestic abuse rises worldwide. Available from: https://www.nytimes.com/2020/04/06/world/coronavirus-domestic-violence.html. [Google Scholar]
- 54. Santhanam L. [cited May 11, 2020] [Internet]. Why child welfare experts fear a spike of abuse during COVID-19. Available from: https://www.pbs.org/newshour/health/why-child-welfare-experts-fear-a-spike-of-abuse-during-covid-19. [Google Scholar]
- 55. Serrata JVA, Alvarado MGH Understanding the impact of Hurricane Harvey on family violence survivors in Texas and those who serve them. Austin (TX): Texas Council on Family Violence; 2019. [Google Scholar]
- 56. Curtis T, Miller BC, Berry EH. Changes in reports and incidence of child abuse following natural disasters. Child Abuse Negl. 2000;24(9):1151–62. [DOI] [PubMed] [Google Scholar]
- 57. Conroy AA, Cohen MH, Frongillo EA, Tsai AC, Wilson TE, Wentz EL, Adimora AA, Merenstein D, Ofotokun I, Metsch L et al. Food insecurity and violence in a prospective cohort of women at risk for or living with HIV in the U.S. PLoS One. 2019;14(3):e0213365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, Parks SE. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015;48(3):345–9. [DOI] [PubMed] [Google Scholar]
- 59. Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–6. [DOI] [PubMed] [Google Scholar]
- 60. Nagata JM, Palar K, Gooding HC, Garber AK, Whittle HJ, Bibbins-Domingo K, Weiser SD. Food insecurity is associated with poorer mental health and sleep outcomes in young adults. J Adolesc Health. 2019;65(6):805–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The relationship between food insecurity and depression, diabetes distress and medication adherence among low-income patients with poorly-controlled diabetes. J Gen Intern Med. 2015;30(10):1476–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Whittle HJ, Sheira LA, Wolfe WR, Frongillo EA, Palar K, Merenstein D, Wilson TE, Adedimeji A, Weber KM, Adimora AA et al. Food insecurity is associated with anxiety, stress, and symptoms of posttraumatic stress disorder in a cohort of women with or at risk of HIV in the United States. J Nutr. 2019;149(8):1393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Whittle HJ, Palar K, Seligman HK, Napoles T, Frongillo EA, Weiser SD. How food insecurity contributes to poor HIV health outcomes: qualitative evidence from the San Francisco Bay Area. Soc Sci Med. 2016;170:228–36. [DOI] [PubMed] [Google Scholar]
- 64. Beutel ME, Klein EM, Brahler E, Reiner I, Junger C, Michal M, Wiltink J, Wild PS, Munzel T, Lackner KJ et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hutton HE, Lyketsos CG, Zenilman JM, Thompson RE, Erbelding EJ. Depression and HIV risk behaviors among patients in a sexually transmitted disease clinic. Am J Psychiatry. 2004;161(5):912–4. [DOI] [PubMed] [Google Scholar]
- 66. El-Bassel N, Gilbert L, Vinocur D, Chang M, Wu E. Posttraumatic stress disorder and HIV risk among poor, inner-city women receiving care in an emergency department. Am J Public Health. 2011;101(1):120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BH. Meta-analysis of anxiety as a risk factor for cardiovascular disease. Am J Cardiol. 2016;118(4):511–9. [DOI] [PubMed] [Google Scholar]
- 69. Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103–15. [DOI] [PubMed] [Google Scholar]
- 70. Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26(10):2822–8. [DOI] [PubMed] [Google Scholar]
- 71. Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, Fawzi MC. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J Acquir Immune Defic Syndr. 2007;44(4):470–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. 2014;11(3):291–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Whittle HJ, Palar K, Napoles T, Hufstedler LL, Ching I, Hecht FM, Frongillo EA, Weiser SD. Experiences with food insecurity and risky sex among low-income people living with HIV/AIDS in a resource-rich setting. J Int AIDS Soc. 2015;18:20293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Vogenthaler NS, Kushel MB, Hadley C, Frongillo EA Jr, Riley ED, Bangsberg DR, Weiser SD. Food insecurity and risky sexual behaviors among homeless and marginally housed HIV-infected individuals in San Francisco. AIDS Behav. 2013;17(5):1688–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kalichman SC, Grebler T, Amaral CM, McKerney M, White D, Kalichman MO, Cherry C, Eaton L. Food insecurity and antiretroviral adherence among HIV positive adults who drink alcohol. J Behav Med. 2014;37(5):1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, Hunt PW, Ragland K, Martin J, Bangsberg DR. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS Behav. 2015;19(8):1510–26. [DOI] [PubMed] [Google Scholar]
- 80. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303. [DOI] [PubMed] [Google Scholar]
- 81. Leddy AM, Sheira LA, Tamraz B, Sykes C, Kashuba ADM, Wilson TE, Adedimeji A, Merenstein D, Cohen MH, Wentz EL et al. Food insecurity is associated with lower levels of antiretroviral drug concentrations in hair among a cohort of women living with HIV in the United States. Clin Infect Dis. 2019. doi: 10.1093/cid/ciz1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–92. [DOI] [PubMed] [Google Scholar]
- 84. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. [DOI] [PubMed] [Google Scholar]
- 85. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–53 e2. [DOI] [PubMed] [Google Scholar]
- 86. Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107(11):1952–61. [DOI] [PubMed] [Google Scholar]
- 87. Bhattacharya J, DeLeire T, Haider S, Currie J. Heat or eat? Cold-weather shocks and nutrition in poor American families. Am J Public Health. 2003;93(7):1149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Seligman HK, Bolger AF, Guzman D, Lopez A, Bibbins-Domingo K. Exhaustion of food budgets at month's end and hospital admissions for hypoglycemia. Health Aff. 2014;33(1):116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Bristol-Myers Squibb Reyataz (Atazanavir) [package insert] New York, NY: Bristol-Myers Squibb. Revised September 2016. [Google Scholar]
- 90. Leddy AM, Roque A, Sheira LA, Frongillo EA, Landay AL, Adedimeji AA, Wilson TE, Merenstein D, Wentz E, Adimora AA et al. Food insecurity is associated with inflammation among women living with HIV. J Infect Dis. 2019;219(3):429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Gowda C, Hadley C, Aiello AE. The association between food insecurity and inflammation in the US adult population. Am J Public Health. 2012;102(8):1579–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342(12):836–43. [DOI] [PubMed] [Google Scholar]
- 93. Borges AH, O'Connor JL, Phillips AN, Ronsholt FF, Pett S, Vjecha MJ, French MA, Lundgren JD, Insight Sand Groups ES et al. Factors associated with plasma IL-6 levels during HIV infection. J Infect Dis. 2015;212(4):585–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Tenorio AR, Zheng Y, Bosch RJ, Krishnan S, Rodriguez B, Hunt PW, Plants J, Seth A, Wilson CC, Deeks SG et al. Soluble markers of inflammation and coagulation but not T-cell activation predict non-AIDS-defining morbid events during suppressive antiretroviral treatment. J Infect Dis. 2014;210(8):1248–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Marsland AL, Walsh C, Lockwood K, John-Henderson NA. The effects of acute psychological stress on circulating and stimulated inflammatory markers: a systematic review and meta-analysis. Brain Behav Immun. 2017;64:208–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Lopez-Garcia E, Schulze MB, Fung TT, Meigs JB, Rifai N, Manson JE, Hu FB. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2004;80(4):1029–35. [DOI] [PubMed] [Google Scholar]
- 97. Schulze MB, Hoffmann K, Manson JE, Willett WC, Meigs JB, Weikert C, Heidemann C, Colditz GA, Hu FB. Dietary pattern, inflammation, and incidence of type 2 diabetes in women. Am J Clin Nutr. 2005;82(3):675–84.; quiz 714-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Garg SK, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, Prill M, Chai SJ, Kirley PD, Alden NB et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Centers for Disease Control and Prevention [cited May 14, 2020] [Internet]. Coronavirus disease 2019 (COVID-19): Health equity considerations and racial and ethnic minority groups. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html. [Google Scholar]
- 103. Hurley D. [cited June 22, 2020] [Internet]. Some COVID-19 patients taken off ventilators are taking days or even weeks to wake up. Available from: https://www.washingtonpost.com/health/2020/06/07/coronavirus-ventilators-prolonged-comas/. [Google Scholar]
- 104. Needham EJ, Chou SH, Coles AJ, Menon DK. Neurological implications of COVID-19 infections. Neurocrit Care. 2020;32(3):667–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Simon DM, McInerney M, Goodell S. The Earned Income Tax Credit, poverty and health. Health Aff; airs Health Policy Brief, October 4, 2018. [Google Scholar]
- 106. Tiwari S, Daidone S, Ruvalcaba MA, Prifti E, Handa S, Davis B, Niang O, Pellerano L, Van Ufford PQ, Seidenfeld D. Impact of cash transfer programs on food security and nutrition in sub-Saharan Africa: a cross-country analysis. Glob Food Sec. 2016;11:72–83. [DOI] [PMC free article] [PubMed] [Google Scholar]