Abstract
Objectives
The coronavirus disease 2019 pandemic has halted in-person medical student education in many large academic centers, including the University of Washington. We identified a unique opportunity to bring comprehensive and targeted anatomic pathology training to large numbers of medical students who would not receive it otherwise but also need credited coursework.
Methods
We developed a comprehensive 2-week remote-learning course encompassing lectures, virtual slides, discussion groups, and unique case-based activities. Activities are tailored to the nonpathologist future clinician, emphasizing basic microscopy and pathology terminology. We employ multiple strategies and technologies to increase engagement while distance learning, including screen annotation, “flipped classroom” slide presentations, and repetition of common themes.
Results
Given 13 virtual courses to choose between 13% of students enrolled in our course (70 of our 540 rising third- and fourth-year students), a nearly 10-fold increase in average pathology rotators.
Conclusions
This is an unprecedented opportunity to provide tailored anatomic pathology instruction, both helping our medical students continue training during crisis and illuminating the field of pathology for our future colleagues. Preliminary results have been overwhelmingly positive regarding understanding of pathology concepts as well as attitudes toward pathology.
Keywords: Anatomic pathology medical education, COVID-19 pandemic, Remote learning, Coronavirus
Key Points.
• To meet medical student needs during the coronavirus disease 2019 pandemic, we developed a 2-week remote anatomic pathology course comprising lectures, virtual slides, discussions, and case-based activities.
• Given the chance, 13% of our clinical students (third and fourth years) or approximately 20% to 25% of the third-year class have enrolled in the course, a nearly 10-fold increase from our usual monthly rotators.
• Multiple technologies and strategies allowed us to create a highly interactive course with positive preliminary feedback.
Washington State reported the first cases of coronavirus disease 2019 (COVID-19) in the United States.1 The University of Washington School of Medicine (UWSOM) is headquartered in Seattle and serves students in five states, including Washington, Wyoming, Alaska, Montana, and Idaho, with regional sites in each state. In March 2020, as cases of COVID-19 increased in Washington State, the UWSOM halted all in-person clinical clerkships and advised students to return to their home states. Although the UWSOM has experience coordinating our medical education curriculum across a variety of geographies and health care systems, this pandemic has brought profound changes for us—as well as for our colleagues around the world—as pathology educators.
COVID-19 and Pathology Education
To meet the needs of postgraduate pathology trainees (residents and fellows), the pathology education community has mobilized. The College of American Pathologists is live-streaming didactic sessions 5 days a week,2 and the US and Canadian Association of Pathologists has made many of its prerecorded continuing medical education workshops available to trainees free of charge. Leading pathologists offer webinars and “tweetorials,” shared widely in the robust pathology social media community. These resources have been organized in a very short time period and demonstrate a true commitment by pathology leaders to residency education.
Medical student educators are undertaking similarly herculean efforts in all specialties as departments collaborate to offer remote courses to medical students to preserve graduation timelines.3-5 However, medical school pathology instruction is quite distinct from other specialties. Most students at our institution do not complete a dedicated pathology rotation (we typically have around 40 nonpathology students complete anatomic pathology clerkships each year). Anatomic pathology is usually folded into other topics, limited to describing histology and briefly outlining pathophysiology. This leaves many learners without a comprehensive understanding of what pathologists do and, unfortunately, without an appreciation for how critical our work is to the clinical care of patients. Medical students (appropriately) spend a great deal of time perfecting history and physicals, writing “SOAP” (Subjective, Objective, Assessment, and Plan) notes, and honing differential diagnoses—all skills that transfer across many specialties and prepare them for clinical residency training. Those students who do go into pathology residency typically have completed a pathology clerkship and therefore obtain more pathology training than general medical students. Even so, new pathology residents face a steep learning curve as they transition to residency. This creates a large gap between the level of pathology residency training materials and the level of the nonpathology medical student learner. Furthermore, because most medical students do not go into pathology, the goals of medical student pathology education are different. Rather than train students in the practice of pathology, our goal is to prepare them for how pathology and pathologists will affect their practice. Most clinicians do not need to be able to look at a slide and make a diagnosis, but they do need to understand the language that appears on the pathology report and how to apply it to their patients. For all of these reasons, simply modifying current residency training activities is not an appropriate strategy for medical student anatomic pathology education.
Conversely, medical students are well suited to join in with laboratory medicine resident activities, which center on basic science principles (polymerase chain reaction [PCR], microbiology, etc) as applied to patient samples. Our colleagues in laboratory medicine have developed a 2-week companion course that allows medical students to attend lectures, plate rounds, call rounds, signouts, and so on. Given the extraordinary circumstances in which we find ourselves, this laboratory medicine course gives medical students a truly once-in-a-lifetime opportunity to learn, real time, about laboratory-developed tests, scaling testing capacity, supply chain issues, and reference laboratory logistics as we respond to severe acute respiratory syndrome coronavirus 2. This unprecedented educational opportunity is also harnessed in our anatomic pathology course; we include two afternoon lectures given by our laboratory medicine colleagues focusing on both the anatomic pathology and laboratory medicine aspects of COVID-19, including autopsy findings, current laboratory testing techniques, immunologic aspects of the virus, and implications for vaccine development and ascertainment of community immunity. As pathology educators, we have identified the current COVID-19 pandemic as an unprecedented opportunity to address several critical needs simultaneously: (1) provide credited coursework to medical students while in-person courses are unavailable, (2) reach a greater audience from which to recruit future pathologists, and (3) provide comprehensive training in the aspects of anatomic pathology that are critical to all specialties and are unfortunately missing from current medical school curricula. In fact, it is the lack of exposure to pathology in medical school that is often cited as the reason for declining numbers of US anatomic pathology residents. Anatomic pathology, as a diagnostic specialty, is particularly amenable to remote instruction.6,7 With the plethora of high-quality digital platforms and online resources, we see an opportunity to meet students where they are and to support their educational needs by providing a remote course. Our first 2-week session began at the end of April, and two additional offerings were slated for later this spring.
Curriculum and Technology
Our course objectives are (1) to provide an interactive, organ system–based review of pathology at the level of the medical student learner; (2) to educate future nonpathologists in the terminology and workflow of pathology as it relates to their future patients; and (3) to elevate pathology in our students’ minds, increasing interest in and understanding of pathology as a career.
We developed a schedule with a variety of integrated activities Table 1. The 2-week course consists of 10 business days and is structured to include 2 hours of morning, large-group (20-25 students) didactics and 2 hours of afternoon, small-group work (2 groups of 10-13 students). We designed our 2-week curriculum to provide a tour of anatomic pathology by organ system, including anatomy, normal histology review, and a dive into high-yield diagnostic entities. Throughout these organ-based modules, we stress concepts that pathologists use daily but are often poorly understood by clinicians. We describe types of tissue reaction, including inflammation, hyperplasia, metaplasia, and atrophy. Importantly, we use every lecture to review neoplasia, defining the terms benign, malignant, in situ, and invasive, and applying them to the most common processes in each organ system. We outline how tissue is received, processed, and reviewed. We also include a molecular genetics lecture, discussing the methods for determining molecular information (PCR, next-generation sequencing, fluorescence in situ hybridization) and applying them to previously discussed entities as predictive, prognostic, or diagnostic markers. Lectures were developed by E. Parker, L. Koch, and several pathology resident volunteers using a consistent format and designed to build on each other. The content is aimed at clinical students with little pathology exposure; we integrate histologic findings into clinical scenarios in the manner they will see as clinicians—essentially helping them to “see” the disease on the slide. Each afternoon small-group slide session goes over topics discussed in that morning’s lecture, providing repetition and reinforcement.
Table 1.
Daily Schedulea
| Day | Big Topic | Morning Session 1 | Morning Session 2 | Afternoon Session |
|---|---|---|---|---|
| 1 | Introduction | Normal histology | Neoplasia | Orientation, presentation of group case (Detective Case) |
| 2 | The nuts and bolts of pathology processing | Anatomic pathology (biopsies, resections, frozens) | Cytology processing and introduction | Neoplastic vs reactive slide session |
| 3 | GI | Tubular GI (esophagus to colon) | Pancreaticohepatobiliary | GI pathology slide session |
| 4 | Dermatopathology | Inflammatory dermatopathology | Neoplastic dermatopathology | Dermatopathology slide session |
| 5 | Cardiothoracic | The lungs | The heart | Cardiothoracic slide session |
| 6 | GU | Upper GU (medical kidney, cystic kidney, neoplastic kidney) | Lower GU (bladder, male reproductive organs) | GU slide session |
| 7 | Women’s health | Breast | GYN | Breast and GYN slide session, presentation: laboratory-developed tests and the UW COVID-19 experience |
| 8 | Head and neck pathology | ENT | Glands (thyroid, parathyroid, salivary) | ENT pathology slide session |
| 9 | BST and molecular | BST | Molecular genetics | BST slide session, presentation: COVID-19 autopsy findings |
| 10 | Autopsy and neuropathology | Neuropathology | Autopsy and death certificate | Neuropathology slide session, Detective and Good Will Hunting Case wrap-ups |
BST, bone and soft tissue; COVID-19, coronavirus disease 2019; ENT, ear, nose, and throat; GI, gastrointestinal; GU, genitourinary; GYN, gynecology; UW, University of Washington.
aThe remote anatomic pathology course is 2 weeks long, consisting of 10 days of remote instruction. Morning sessions are large group with all students calling into the same live lectures. During each session, the presenter explores a topic (organized by organ system) to review anatomy, normal histology, and pathologic entities, toggling back and forth between a PowerPoint and a virtual slide set. Afternoon sessions consist of unknown cases from the organ system of the day with Detective Case workup discussions. Two days include lectures on the University of Washington Medical Center pathology experience with COVID-19.
A key consideration in online education is student engagement. In a traditional lecture, the presenter can make eye contact, look for confusion or agreement, and ask questions. We use Zoom Meetings & Chat (Zoom Video Communications) to present our lectures; all University of Washington members have free access to Zoom Pro. While this platform is a fantastic tool during social distancing, it does allow for students to take a passive approach. Given that this is a new curriculum and new information for most of the students, we were concerned about how to gauge whether it was being delivered effectively. We use several strategies to assess and increase engagement.
Morning didactics are delivered to the entire group via Zoom with PowerPoint (Microsoft) slides supplemented with virtual slides presented through the online digital platform PathPresenter (PathPresenter.net). Lectures are presented by L. Koch, E. Parker, and several volunteer pathology trainees. In these first iterations, we wanted as much participation as possible. We do not provide the PowerPoint slides until after the lecture, to allow students to “be there” with us as we discuss the material in real time. While we may record future sessions of the course, we decided that the existence of recordings would be an excuse for students to not come to class. We will assess student desire for recordings and, if we implement them, will evaluate attendance to determine if recordings will help or harm engagement. While in class, students are encouraged to turn on their video feed. Questions are encouraged at any time, through voice or the chat box. We make heavy use of the “annotate” function, which allows students to write or answer questions directly on the screen if they like. In addition, we ask for frequent participation, having the students annotate where on the slide they see a mitosis, outline the neoplasm, or vote for the answer to a question (“if you think this is neoplastic, put a stamp on the left side of the screen; if you think it’s reactive, put a stamp on the right”). We are finding that this method allows all students, even those who feel uncomfortable speaking up or turning on their cameras, to be actively engaged. Each lecture concludes with a series of “board-style” questions, where students give their responses using the annotation tools.
Afternoon sessions consist of small-group work led by teaching assistants (TAs, our former pathology postsophomore fellows) with support from O. Chang, who holds daily training sessions with the TAs. Afternoon small group work reinforces concepts learned during that morning’s didactic sessions. A shared log-in was created for PathPresenter, where students go to preview virtual slide trays curated from PathPresenter’s vast public library of whole-slide images. Students are each assigned one unknown slide to preview, which they present to their small group in a modified flipped classroom model. Engagement is encouraged both by this model as well as by the fact that TAs are their peers, providing a more informal environment in which to ask questions and discuss cases. The slides are chosen for maximum-level appropriate educational value; they contain common entities with normal background tissue, allowing students to compare normal to abnormal and learn how to use pathology terminology as they describe the differences. Notably, camera usage is much higher during these sessions (L.K., personal observation, 2020).
In addition, the small groups are assigned a diagnostically challenging case to work through as a group (the so-called Detective Case, due to the mystery and team effort required). This Detective Case is introduced to the small groups at the beginning of the course, and the students work together throughout the duration of the course to solve the mystery. They discuss the case and then “order” tests from the TAs, who report the results, including whole-slide images on PathPresenter, imaging studies, and pathology reports, adapted from real patient cases. Each group elects a “chief resident,” who is in charge of communicating orders. The TA may offer advice to keep them on track, but the bulk of the discussion is led by the students. At the end of the course, they present their diagnosis and reasoning. Additional follow-up questions and teaching points are discussed as a large group with the entire class. This case is designed to be relatively solvable and to demonstrate fundamental pathology principles. It centers on carcinoma of unknown primary, requiring students to judiciously order imaging and tissue sampling to make the diagnosis and decide on treatment (surgery vs chemotherapy). Examples include a woman presenting with a broken hip (metastatic breast carcinoma) and a man with gross hematuria and anemia (noninvasive papillary urothelial carcinoma and metastatic colon carcinoma).
Last, students are invited to spend the 2 weeks independently working through a particularly challenging case (the so-called Good Will Hunting Case due to its rigor and the independent nature of the workup). Students seek (by email) expert advice from pathology consultants (volunteer pathology trainees who do not have access to the case answer key), and course instructors provide requested test results and periodic updates as the patient’s status changes. Our first Good Will Hunting Case was an unusual presentation of Fabry disease, requiring physical examination findings, biopsy, enzyme testing, and genetic testing, among other testing modalities. On the final day of the course, students compare their workups, and the diagnosis is revealed and discussed. The small group who arrives at the correct diagnosis in the fewest number of steps “wins.” In addition to being a fun, interactive, and challenging exercise, this creates a forum in which to discuss health care utilization, test performance, and laboratory management. In this way, students engage with multiple learning modalities combining lecture, interactive virtual slides, small groups, and independent study.
The course is administered through Canvas (Instructure), the learning management system used by UWSOM. The course site includes the schedule, Zoom links, small group assignments, reading assignments, additional resources, surveys, and PowerPoint slides (following the lecture). Lecturers access their PowerPoints from the Canvas teaching module, which is not accessible to students. Course materials are housed permanently in Microsoft Teams (Microsoft), including lectures, detective case presentations and test results, and materials in development. The teams “post” function serves to significantly cut down on email. Team members include the three course faculty (authors), TAs, and graduate medical education administrators, who help maintain the Canvas site.
To determine the effectiveness of this remote course, we administer a questionnaire at the beginning and completion of the course to assess cohort shifts in understanding and use of pathology terminology Figure 1. The questionnaire is anonymous (pre- and postcourse surveys are paired by a course administrator and given to us deidentified). The course is pass/fail; our requirements for passing are attendance and completion of these surveys. In addition, we solicit anonymous feedback at the completion of the course regarding the format of the remote learning sessions as well as changes in attitudes toward pathology, including likelihood of pursuing pathology as a specialty Figure 2. We will use these data to improve future versions of the course. Surveys are also provided and submitted via Canvas using Microsoft Forms (Microsoft), which will also be used for data analysis.
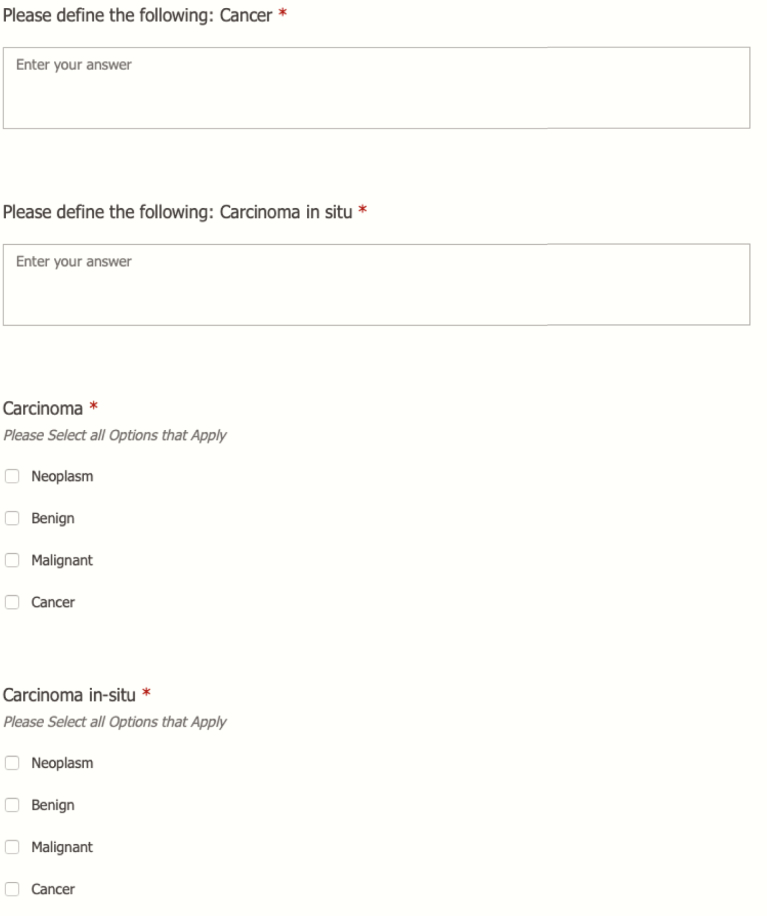
Figure 1.
Students completed a two-part survey prior to starting the course. The first part of the survey asks participants to define basic pathology terminology, and the second part of the survey asks participants to categorize various disease entities as neoplasm, benign, malignant, and/or cancer. After the course, the students were invited to complete the second part of the survey again.
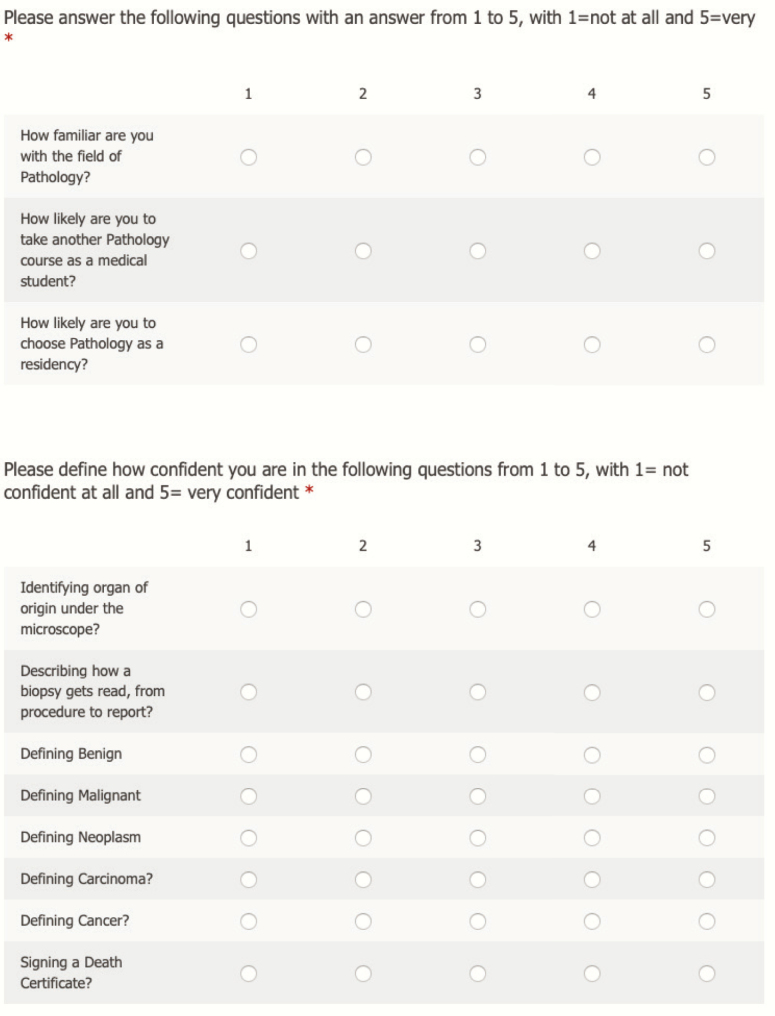
Figure 2.
In addition to asking basic demographic questions, we included survey questions about attitudes toward pathology as a specialty as well as confidence in various pathologically relevant skills.
Results
In March 2020, we discussed this opportunity with UWSOM leadership and by early April 2020, we developed a 2-week remote learning anatomic pathology course. Early April 2020 was dedicated to curricular and didactic development; late April 2020 was used to fine-tune content and the small-group cases. See Table 1 for a summary of our course content. Our remote course was one of 13 courses available to students learning from home. Importantly, a concurrent course was being developed by our laboratory medicine colleagues with the goal of initially rolling out separate 2-week courses for students and later combining them into one 4-week course.
Strikingly, this opportunity has greatly increased the number of medical students completing pathology-specific coursework. At our institution, we have on average six medical students each month rotating in anatomic pathology across several sites. Over the past 3 years, we have hosted between 61 and 68 students annually, including both UWSOM students and visiting students (students who are interested in our residency). This is a small footprint given that UWSOM accepts 270 students in each entering class. From a total of 13 online course offerings, 70 clinical students enrolled in three sessions of this 2-week course, many of whom are third-year students. This means that, when given the opportunity, 13% of our clinical students (70 out of 540 clinical third- and fourth-year students) and closer to 20% to 25% of our third-year class signed up for a pathology rotation. This is a nearly 10-fold increase in students per month as we now have nearly 50 students a month who will be rotating with us remotely. This is a tremendous increase in exposure to anatomic pathology and the resultant understanding of anatomic pathology by our graduating medical students.
We have completed the first iteration of the course, and preliminary feedback has been overwhelmingly positive. The first group of students rated “the educational quality of this remote course vs an in-person course” an average of 4.5 on a 5-point scale. The content appears to be effective as well; for example, nine of 25 students thought a tubular adenoma was “cancer” or “malignant” prior to the class; after class, only one still did. On a scale of 1 to 5, precourse students rated their confidence in signing a death certificate, on average, at 1.6; this increased to 3.2 after the course. Confidence in identifying organ of origin under the microscope went from 2 to 3.3. Coincidentally, we had a spot open up in our postsophomore fellowship during the first session, and two of our students applied for a yearlong position beginning in less than 6 weeks; both said our course had made them more interested in pathology.
The course evaluation comments included the following:
“I really enjoyed the structure of having lecture in the mornings followed by interactive sessions in the afternoon looking at, describing, and work[ing] through actual slides that helped to apply and ingrain the knowledge from the morning sessions. Having all of this followed by an interactive and engaging case study was also terrific!”
“Didactics with annotation function were fun and engaging. Small group leaders were also engaging and helpful in creating a comfortable learning environment.”
“I liked that this rotation was more geared to understanding pathology from a clinical perspective rather than focusing on all the nitty-gritty!”
“I like the structure of doing large group lecture and then small group reading of the slides. I need repetition and practice and this gave me that.”
Discussion
While there are limitations to what can be conveyed and experienced via remote teaching, this is an unprecedented opportunity for pathology educators to dramatically increase medical students’ exposure to and understanding of the field of pathology. This is an opportunity to demonstrate to medical leadership the value of pathology education to our students in an age when many medical schools are curtailing preclinical contact education for medical students and the number of students going into pathology is dwindling. Our ability to provide a meaningful clinical experience for students during this time of limited interpersonal contact and social distancing enhances the visibility of and appreciation for pathology within our institution.
Technology has been key in engaging our learners. In particular, Zoom’s annotation function, encouraging web camera use, and virtual slide sessions via PathPresenter were viewed highly by both our instructors and our students. Organizational tools, including Canvas and Microsoft Teams, have allowed us to centralize information and documents, as well as to communicate efficiently.
The course has resulted in a dramatic increase in the number of students who enrolled in a pathology rotation. Given the opportunity, 13% of our clinical students (both third- and fourth-year students) or approximately 20% to 25% of the third-year class have enrolled in our remote pathology course. This is a nearly 10-fold increase in our average number of monthly student rotators. Preliminary results indicate the course is effective in both increasing knowledge of pathology and elevating student opinions about anatomic pathology, including enticing two students to apply for our postsophomore fellowship.
We have a tremendous opportunity to meet the unique needs of our students during the COVID-19 pandemic and to simultaneously elevate pathology understanding in our future nonpathology colleagues. Our future work will focus on collaborating with our laboratory medicine colleagues in the creation of a comprehensive 4-week remote anatomic pathology rotation. We envision this future course as a tool to meet the needs of medical students facing nonpandemic obstacles to on-site pathology training, including family obligations, disability, and financial concerns.
Most important, we remain optimistic that in this time of terrible disease and disruption we can make pathology an accessible and valuable learning experience for all of our students.
Acknowledgments
We thank the University of Washington Department of Pathology community for supporting and collaborating to create this remote course. Special thanks to Rochelle Garcia, MD, for pioneering neoplasia education and to Allie Correll-Buss and Alisa Ulrich-Herrera for administrative support.
References
- 1. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. https://www.cap.org/calendar/virtual-lecture-series-for-pathology-residents. Accessed April 16, 2020.
- 3. Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education. Lancet Infect Dis. 2020;20:777-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moszkowicz D, Duboc H, Dubertret C, et al. Daily medical education for confined students during COVID-19 pandemic: a simple videoconference solution [published online April 6, 2020]. Clin Anat. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rose S. Medical student education in the time of COVID-19 [published online March 31, 2020]. JAMA. [DOI] [PubMed] [Google Scholar]
- 6. Wilbur DC. Digital pathology and its role in cytology education. Cytopathology. 2016;27:325-330. [DOI] [PubMed] [Google Scholar]
- 7. Fung K-M, Hassell LA, Talbert ML, et al. Whole slide images and digital media in pathology education, testing, and practice: the Oklahoma experience. Anal Cell Pathol. 2012;35:37-40. [DOI] [PMC free article] [PubMed] [Google Scholar]