Abstract
Countries such as South Africa have limited intensive care unit (ICU) capacity to handle the expected number of patients with COVID-19 requiring ICU care. Remdesivir can prevent deaths in countries such as South Africa by decreasing the number of days people spend in ICU, therefore freeing up ICU bed capacity.
Keywords: SARS-CoV-2, COVID-19, mathematical model, hospital bed capacity, intensive care
The coronavirus disease 2019 (COVID-19) pandemic has already infected millions of people across the globe, with more than 400 000 COVID-related deaths reported worldwide [1]. Case numbers are growing rapidly in low-and middle-income countries, overwhelming health systems. In South Africa, the combined intensive care unit (ICU) capacity of the public and private health sectors combined was estimated to be 3340 before the COVID-19 pandemic took hold. As of the beginning of June 2020, ICU beds in the Western Cape, currently the worst affected of South Africa’s 9 provinces, were already at capacity [2], and other provinces’ capacity is projected to be overwhelmed in the coming weeks. The ICU capacity is expected to be breached, depending on the provinces, for between 3 and 6 months between June and December 2020 by a factor of 6–10 [3].
There are currently no curative therapies available for those with advanced COVID-19 disease, and mortality rates among those requiring ICU care are around 50% [4–6]. Recently, remdesivir has been shown to reduce the total amount of time in the ICU required per patient, from 15 days on average (95% confidence interval [CI], 13–19 days), down to 11 days on average (95% CI, 9–12 days) [7]. Remdesivir also had a nearly statistically significant 30% reduction on mortality [7]. Given the limited ICU capacity in South Africa, we sought to determine the impact that remdesivir could have in preventing deaths through decreasing the amount of time people spend in the ICU, and, as a result, increasing ICU bed turnover. We also evaluated the impact of the potential reduction in mortality due to remdesivir itself alongside increasing ICU capacity.
METHODS
We first determined the number of people requiring ICU admission by province by month as projected by the South African National COVID-19 Epidemiology Model between June and December 2020 and the number of all currently available ICU beds by province [3]. During peak months where ICU capacity is expected to be breached, we calculated the additional benefit that remdesivir could have in terms of increasing ICU capacity by decreasing the average length of stay of patients. We used 10 000 Monte Carlo simulations to sample uniformly within the 95% CI of recovery time for patients treated with and without remdesivir using the results of a recently published remdesivir clinical trial. We assumed that the mortality rate of those requiring ICU care and receiving ICU care was 50% and ranging up to 85% in the event that mortality is higher than expected in ICUs in South Africa [4–6]. We varied the death rate of those requiring ICU care but not receiving ICU care between 85% and 100%, assuming that the death rate of those who need ICU care and do not receive it must be higher than those who need ICU care and do receive care. In an additional analysis, we calculated the potential direct impact of remdesivir on mortality of patients in the ICU for all patients in the ICU between June and December, varying between the 95% CIs reported in a recent trial (reduction in mortality of 47% to an increase of 4%), compared with a baseline of 50% mortality in the ICU. We projected outcomes for 2 scenarios defined by optimistic and pessimistic assumptions regarding the impact of the country’s mitigation strategies since April 2020 on transmission, and report the 2.5th–97.5th percentiles of the Monte Carlo simulations.
RESULTS
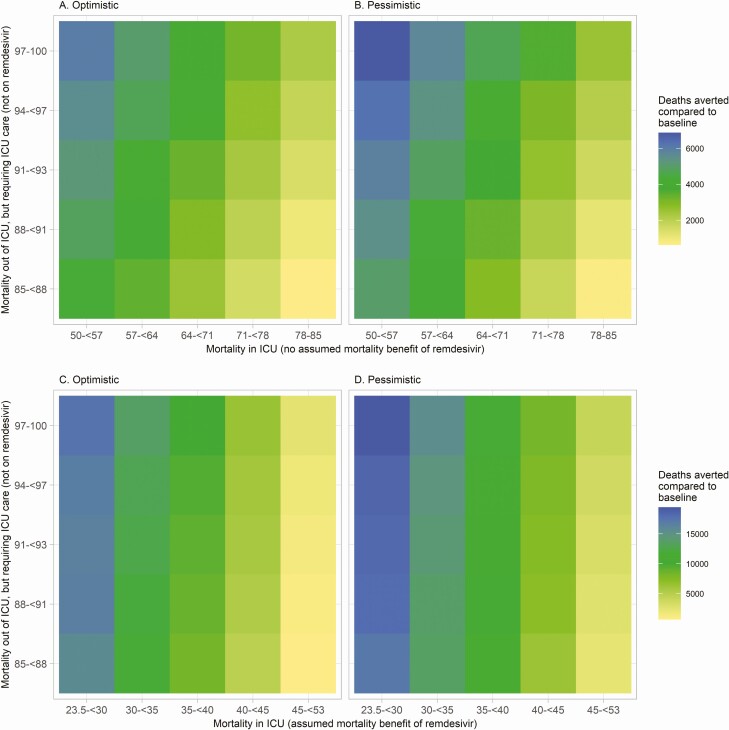
In South Africa, there are an estimated 3450 ICU beds available for patients with COVID-19. Intensive care unit capacity is expected to be breached, depending on the province, for between 3 and 6 months between June and December 2020. Without remdesivir, there is expected to be a total of 23 443–32 284 patients who will occupy an ICU bed during peak months where the ICU is expected to be breached. With remdesivir, that number is expected to grow by 48–55% to 36 383–47 820 treated in the ICU by December 2020. By giving remdesivir to all patients in the ICU during peak months (all to 36 383–47 820 patients), 635–6862 deaths will be averted due to increased capacity alone if assuming an 85–100% death rate among those not receiving ICU care but who require ICU care (Figure 1A and 1B). The fewest deaths averted between June and December were found when the mortality rate both in the ICU (78–85%) and out of the ICU (85–88%) were assumed to be similar (median simulation, 635 deaths averted; 2.5th–97.5th percentile, 172–1247). The greatest number of deaths were averted when the mortality rate for patients who require ICU care and do not receive it was highest (97–100%) and the death rate among those in the ICU was the lowest (50–57%) (6862 deaths averted; 2.5th–97.5th percentile, 4890–8872).
Figure 1.
Deaths averted due to spare ICU capacity attributable to remdesivir use in months where capacity is expected to be breached (A, optimistic; B, pessimistic); deaths averted from spare ICU capacity during peak months plus reductions in mortality from remdesivir in all months (C, optimistic; D, pessimistic). Direct mortality reductions due remdesivir use in panels C and D compare back to an underlying 50% mortality rate in the ICU. Abbreviation: ICU, intensive care unit.
When accounting for the reduction in mortality due to remdesivir use in all months as well as the reduction in deaths due to increasing ICU capacity, 691–19 453 deaths averted are predicted (Figure 1C and 1D).
DISCUSSION
The use of remdesivir use in patients with COVID-19 has the potential to save many lives. The substantial life-saving impact predicted by our model is partially mediated through reducing the number of ICU days required per patient, and thereby creating additional capacity to treat more patients through more rapid patient turnover. Therefore, should the direct mortality benefit of remdesivir not be realized in practice, the potential for decreasing COVID-19 mortality is substantial. The results are, however, sensitive to the underlying mortality estimates of patients in the ICU and patients who require ICU care but do not receive it.
This analysis has several limitations. First, if the epidemic curve is altogether flatter than predicted in our model projections, then the total number of deaths averted could be higher, as the number requiring ICU care would be spread out over a greater number of months. As the epidemic matures, the composition of the patient population entering the ICU may change, particularly if any rationing of resources occurs. While this may affect the point estimate of our results, it is unlikely to affect the magnitude of difference between scenarios. Importantly, while the simple mechanism of reducing the number of ICU days required will have a large impact on mortality, it can only have an impact that is only as large as its ICU infrastructure. For countries that have an even more constrained ICU bed capacity, such as Zambia with just 91 ICU beds [8], the absolute benefit will be much smaller. As additional treatment options become available, such as dexamethasone [9] and other options under investigation, it will be important to understand how improvements in mortality also affect length of ICU stay and time to recovery, given the direct impact between breached ICU capacity and mortality. Finally, remdesivir and similar treatments may be used outside the ICU, possibly resulting in an additional reduction in mortality that we were not able to quantify without additional effectiveness data.
To conclude, above and beyond any direct impact on mortality, remdesivir can play a significant role in freeing up highly constrained ICU capacity, and therefore reduce the number of deaths caused by limited capacity. South Africa and countries with similarly constrained healthcare system capacity are expected to benefit the most and should consider remdesivir, or any other interventions that can reduce length of ICU stay, for patients in the ICU with COVID-19 if prices (which are currently still under negotiation) are acceptable.
Notes
Disclaimer. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors’ views expressed in this publication do not necessarily reflect the views of USAID or the US government.
Financial support. This work was supported by the US Agency for International Development (USAID; grant number 72067419CA00004).
Potential conflicts of interest. B. E. N. and I. S. report grants from USAID during the conduct of the study. S. S. reports grants from Wellcome Trust during the conduct of the study. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Coronavirus pandemic (COVID-19). 2020. Available at: https://ourworldindata.org/coronavirus. Accessed 6 June 2020.
- 2. Low M. As ICUs fill up in the Western Cape, some lockdown measures must be reconsidered. Maverick 2020. Available at: https://www.dailymaverick.co.za/article/2020-06-02-as-icus-fill-up-in-the-western-cape-some-lockdown-measures-must-be-reconsidered/#gsc.tab=0. Accessed 3 June 2020. [Google Scholar]
- 3. Silal S, Jamieson L, Meyer-Rath G, Nichols BE, Pulliam J; MASHA; HE2RO; SACEMA. Estimating cases for COVID-19 in South Africa: Long-term national projections. South Africa: National Institute of Communicable Diseases, 2020. Available at: https://www.nicd.ac.za/wp-content/uploads/2020/05/SACovidModellingReport_ProvincialLongTermProjections_Final.pdf [Google Scholar]
- 4. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020; 323:2052–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NICD. COVID-19 sentinel hospital surveillance update: week 24. Pretoria, South Africa: National Institute for Communicable Diseases, 2020. [Google Scholar]
- 7. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report. N Engl J Med 2020; NEJMoa2007764. doi: 10.1056/NEJMoa2007764. [DOI] [PubMed] [Google Scholar]
- 8. Dart PJ, Kinnear J, Bould MD, Mwansa SL, Rakhda Z, Snell D. An evaluation of inpatient morbidity and critical care provision in Zambia. Anaesthesia 2017; 72:172–80. [DOI] [PubMed] [Google Scholar]
- 9. University of Oxford. Low-cost dexamethasone reduces death by up to one third in hospitalised patients with severe respiratory complications of COVID-19. University of Oxford News. 2020. Available at: http://www.ox.ac.uk/news/2020-06-16-low-cost-dexamethasone-reduces-death-one-third-hospitalised-patients-severe. Accessed 16 June 2020.