A 52-year-old man was admitted to the medical intensive care unit for abdominal pain. His medical history included right nephrectomy for renal neoplasia and stenting in the aorta and left renal artery after aortic dissection. He presented with asthenia over recent weeks. Clinical examination revealed normal blood pressure, apyrexia, distended abdomen and oligo-anuria. His initial laboratory test were as follows: serum creatinine 486 μmol/L, haemoglobin 15.9 g/dL, platelets 400 G/L, lactate deshydrogenase 1795 U/L (normal <246), protein C reactive 82, D-dimer 16 354 ng/mL and fibrinogen 7.2 g/L. A thoraco-abdominopelvic computed tomography scan was performed and showed intra-stent thrombosis of the left renal artery with extensive ischaemical lesions of the renal parenchyma as well as images suggestive of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia (bilateral, subpleural ground-glass opacities) (Figure 1). An angioplasty failed to restore revascularization of the left renal artery. A tunnelled dialysis catheter was placed for the initiation of chronic haemodialysis. SARS-CoV-2 RNA was detectable in nasopharyngeal swabs. A diagnosis of renal artery thrombosis induced by coronavirus disease 2019 (COVID-19) was made. The outcome was favourable without specific treatment and pursuit of chronic haemodialysis.
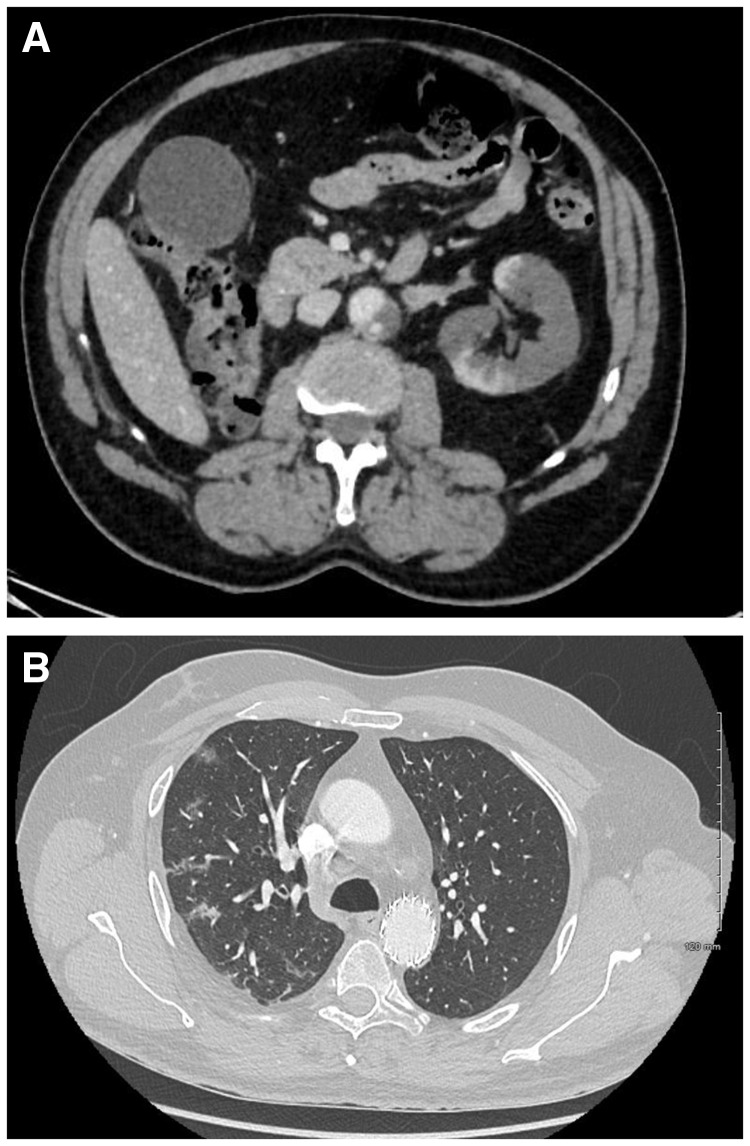
FIGURE 1:
CT scan. (A) Intrastent thrombosis of the left renal artery with extensive ischaemical lesions of the renal parenchyma. (B) Bilateral, subpleural ground-glass opacities suggestive of SARS-CoV-2 pneumonia.
It is now known that COVID-19 may predispose patients to thrombotic disease, both in the venous and arterial circulations, due to excessive inflammation, platelet activation, endothelial dysfunction and stasis. The initial coagulopathy of COVID-19 presents with prominent elevation of fibrin/fibrinogen and degradation products, while abnormalities in prothrombin time, partial thromboplastin time and platelet counts are relatively uncommon in initial presentations.
CONFLICT OF INTEREST STATEMENT
None declared.