Learning points
Small vessel thrombosis is a well described risk in the context of COVID-19 infection, yet there is little discussion of large vessel thrombo-embolism in these patients.
Our case is a patient with no history of hypercoagulability or embolism who presented multiple large vessel thrombo-emboli in the context of COVID-19 infection.
There is mounting evidence to support increased thrombo-embolic risk associated with coronavirus disease 2019 (COVID-19) infection. Here, we report a case of COVID-19 complicated by a right ventricular apical thrombus and aortic thrombi.
A 61-year-old woman with type 2 diabetes mellitus, hypertension, and hyperlipidaemia presented to the emergency department (ED) with severe sharp epigastric pain and shortness of breath, with an oxygen saturation of 85%. In the ED, her baseline ECG and physical exam were unremarkable but she was placed on 6 L of oxygen due to persistent hypoxia. Subsequent arterial blood gas analysis revealed a PaO2 of 69 mmHg, PaCO2 of 31 mmHg, pH of 7.49, and sO2 of 93%. Initial chest radiograph demonstrated multifocal bilateral patchy opacities, and reverse transcription–PCR (RT–PCR) tested positive for SARS-CoV-2. Laboratory tests revealed mild leukocytosis (13.8 × 103/μL), elevated D-dimer (8264 ng/mL), elevated fibrinogen (682 mg/dL), and elevated anticardiolipin IgM (31.1 MPL) with normal anticardiolipin IgG.
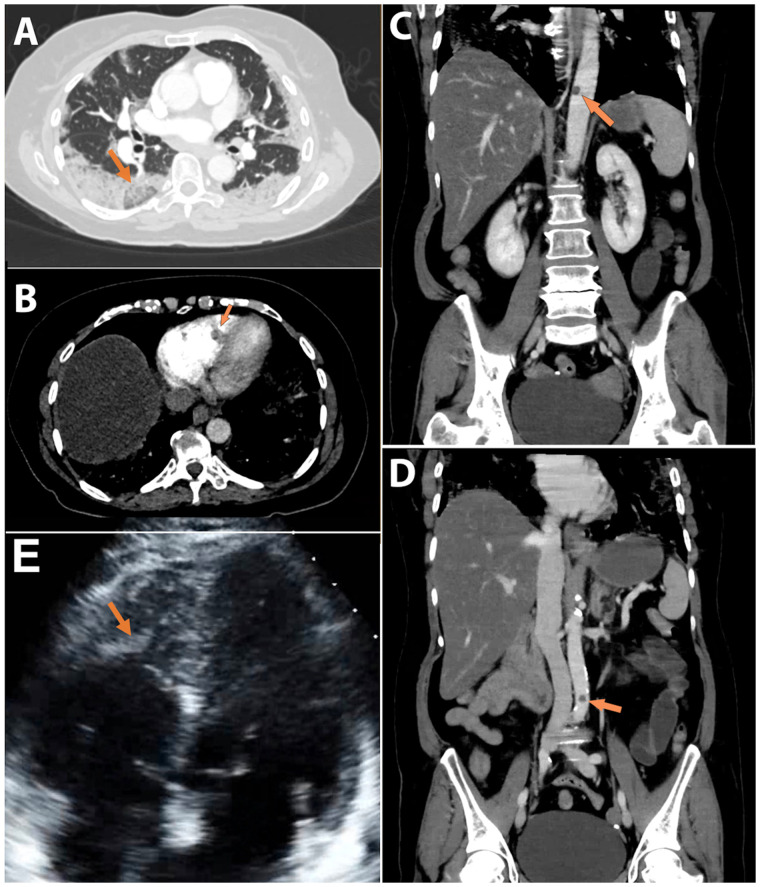
CT pulmonary angiogram and CT of the abdomen/pelvis demonstrated bilateral peripherally located ground-glass and consolidative opacities without evidence of pulmonary embolism (Panel A). There was a prominent hypoattenuating lesion in the right ventricular apex along the interventricular wall representing thrombus (Panel B). Additional rounded filling defects were noted in the thoracic and abdominal aorta, suggestive of vascular thrombi (Panels C and D). Transthoracic agitated saline intravenous echocardiography confirmed the presence of mobile thrombus in the right ventricular apex without evidence of an intracardiac shunt (Panel E).
Figure 1.
(A) Axial image from a contrast-enhanced pulmonary CT angiogram presented at the lung window demonstrates bilateral, peripheral ground-glass opacities and consolidation in the lower lobes, middle lobe, and lingula. Within the right lower lobe, a peripheral round focus of ground-glass opacity containing dilated vessels (arrow) is present. No pulmonary emboli were demonstrated on examination. (B) The soft tissue window demonstrates a 7 mm hypoattenuating thrombus (arrow) within the right ventricular apex, along the medial interventricular wall. Coronal view on the soft tissue window demonstrating (C) a filling defect in the lower thoracic aorta (arrow) superior to the diaphragmatic hiatus and (D) a second filling defect in the lower abdominal aorta (arrow) above the common iliac artery bifurcation. (E) Transthoracic echocardiography apical four-chamber view demonstrates a mobile thrombus (arrow) at the right ventricular apex near the moderator band.
The patient was treated with intravenous tissue plasminogen activator for thrombolysis and was subsequently transitioned to anticoagulation (low molecular weight heparin followed by oral apixaban). After 8 days of hospitalization, the patient was discharged home in stable condition.
Coagulopathy and vascular endothelial damage have been suggested as potential complications of COVID-19 infection. Several reports have shown increased risk for venous thrombo-embolism; in four retrospective studies, the risk of thrombo-embolism ranged from 25% to 69%. The present case raises concern that thrombo-embolic risk associated with COVID-19 infection may not be limited to microthrombosis of small to medium size vessels. Left unrecognized, intracardiac and large vessel thrombi can lead to significant morbidity and mortality.
Consent: Patient informed consent was obtained for publication of this case report.
Conflict of interest: B.P.L. is a textbook author and editor for Elsevier and receives royalties for his previous work.