This commentary refers to ‘Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy’ by Inciardi et al., doi:10.1093/eurheartj/ehaa388.
Cardiovascular disease (CVD) is a frequent comorbidity in coronavirus disease 2019 (COVID-19). However, it is not clear which diseases are included in the CVD generic group or serious heart conditions, and there is no information at present to conclude whether atrial fibrillation (AF) would contribute to increasing the risk for severe forms of COVID-19, worse prognosis, or even higher mortality. Inciardi et al.1 have collected demographic characteristics, clinical presentation, and outcomes of 53 COVID-19 patients with pneumonia and with a history of cardiac disease hospitalized in Brescia, Lombardy (Italy). Of those patients, 40% had a history of heart failure (HF) and 36% had AF.
Italy’s government provides regular updates on the most common CVD comorbidities observed in deceased COVID-19 patients, divided into pathologies. In the last report published by the Italian National Institute of Health (23 April 2020),2 approximately a quarter of patients who died for COVID-19 had AF, which was hence the fourth most common condition in these patients (present in 22% of cases). Moreover, data provided by the New York State Department of Health also reported that AF is among the top ten COVID-19 comorbidities, specifically occupying the seventh position.3 In effect, some forms of arrhythmia were present in 60% of 85 fatal cases, which suggests that cardiac arrhythmia is associated with an increased risk of mortality in COVID-19 patients.4
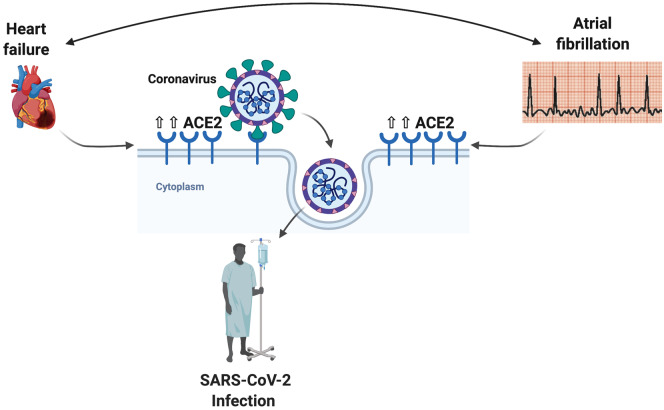
A potential explanation linking severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection with CVD is the higher levels of angiotensin-converting enzyme 2 (ACE2) in individuals with certain CVDs. SARS-CoV-2 penetrates human cells through direct binding with ACE2 at the cell surface. In humans, circulating ACE2 is detectable in individuals with CVD risk factors. Serum ACE2 activity is increased in patients with HF and correlates with disease severity. Interestingly, it has been previously described that plasma ACE2 activity levels are increased in AF and have been suggested as a better marker of disease severity in human AF.4 Moreover, elevated plasma ACE2 levels are also associated with older age, male gender, hypertension, vascular disease, elevated left ventricular (LV) mass, impaired LV diastolic function, and advanced atrial disease.4 Intriguingly, the former is also the most frequent comorbidity associated with worse prognosis in COVID-19 patients.
Accordingly, ACE2 levels and activity are deranged in CVD, including AF. Although it is probable that well-controlled AF does not increase the risk in COVID-19 patients, people living with AF might be more vulnerable to the effects of SARS-CoV-2 infection, thus having an enhanced risk of severe complications and requiring specific cautions. It is paramount that people with AF avoid this viral infection since their condition would be likely to foster the risk of COVID-19 complications. We herein recommend that people with AF shelter at home during this time and do everything possible to avoid exposure to suspected or confirmed COVID-19 cases, following their national guidance for vulnerable people living with chronic disease. It is also mandatory that patients with AF take medications as prescribed, stay in contact with their healthcare teams, and maintain a healthy diet and an appropriate level of physical activity.
Figure 1.
Increased ACE2 expression in individuals with atrial fibrillation, heart failure, or both may make them more vulnerable to SARS-CoV-2 infection. ACE, angiotensin-converting enzyme.
Acknowledgements
F.S.-G. is supported by a postdoctoral contract granted by ‘Subprograma Atracció de Talent – Contractes Postdoctorals de la Universitat de València’.
Conflict of interest: none declared.
References
- 1. Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M.. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J 2020;41:1821–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Characteristics of COVID-19 patients dying in Italy. Report based on available data on April 6th, 2020. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_23_april_2020.pdf (8 April 2020).
- 3.New York State Department of Health. https://covid19tracker.health.ny.gov/views/NYS-COVID19-Tracker/NYSDOHCOVID-19Tracker-Fatalities?%3Aembed=yes&%3Atoolbar=no (30 April 2020).
- 4. Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, Wang X, Hu C, Ping R, Hu P, Li T, Cao F, Chang C, Hu Q, Jin Y, Xu G.. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med 2020;201:1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walters TE, Kalman JM, Patel SK, Mearns M, Velkoska E, Burrell LM.. Angiotensin converting enzyme 2 activity and human atrial fibrillation: increased plasma angiotensin converting enzyme 2 activity is associated with atrial fibrillation and more advanced left atrial structural remodelling. Europace 2017;19:1280–1287. [DOI] [PubMed] [Google Scholar]