Abstract
The recent outbreak of coronavirus disease 2019 (COVID-19) provides a further challenge in the battle against outbreaks of novel virus infections and has been declared a public health emergency of international concern. Much has been learnt in the course of preceding epidemics, including severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and H1N1 influenza, and it is now recognized that their overall health burden may be under-estimated since extra-pulmonary manifestations are frequent.1 Acute and chronic cardiovascular complications of pneumonia are common and result from various mechanisms, including relative ischaemia, systemic inflammation, and pathogen-mediated damage. There is, however, only limited published data concerning cardiovascular presentations in the wake of viral epidemics. The present COVID-19 outbreak emphasizes the need for greater awareness of the immediate and long-term cardiovascular implications of viral infection and the significant gaps in knowledge that future research will need to address.
Epidemiological overview of recent outbreaks of respiratory virus infection
Respiratory virus infection is a major source of global pandemics as a consequence of swift human-to-human respiratory tract transmission. Within the past two decades, coronaviruses and influenza viruses have hit the world several times, causing significant mortality, economic loss, and global panic. The SARS outbreak in 2002 triggered 916 deaths among more than 8000 patients in 29 countries, followed by the emergence of MERS in 2012, which resulted in at least 800 deaths among 2254 patients in 27 countries.2 Besides coronaviruses, avian and swine influenza remain a concern for global public health—in the 2009 H1N1 pandemic alone, there were 18 500 laboratory-confirmed deaths and more than 200 000 deaths from respiratory disease worldwide (based upon epidemiological modelling).3
In late 2019, a cohort of patients presenting with pneumonia of varying acuity and unknown aetiology in Wuhan, China heralded the outset of COVID-19. As of 16 March 2020, a total of 167 511 confirmed cases (including 6606 deaths in 152 geographical territories) have been reported to the World Health Organization (Take home figure), and this number is still increasing. Although COVID-19 appears to have greater infectivity and lower mortality than SARS and MERS, many uncertainties (including route of infection, viral evolution, epidemic dynamics, appropriate anti-viral treatment, and strategies for disease control) remain.
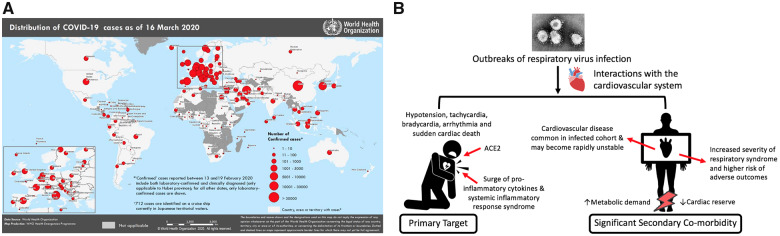
Take home figure.
Current global distribution of COVID-19 and cardiovascular consequences of respiratory virus infection. (A) The global distribution of COVID-19 on 16 March 2020 (figure source: COVID-19 situation reports from World Health Organization). (B) Direct and indirect cardiovascular consequences of respiratory virus infection.
Cardiovascular complications of respiratory virus infection
Cardiovascular complications of influenza infection, including myocarditis, acute myocardial infarction, and exacerbation of heart failure have been well-recognized during previous historical epidemics and make a significant contribution to mortality.4 Likewise, previous coronavirus outbreaks have been associated with a significant burden of cardiovascular comorbidities and complications (Table 1). Furthermore, the severity of the primary respiratory syndrome and risk of adverse outcomes is increased in patients with pre-existing cardiovascular diseases.11 Hypotension, tachycardia, bradycardia, arrhythmia, or even sudden cardiac death are common in patients with SARS. Electrocardiographic changes and troponin elevation may signal underlying myocarditis, and echocardiography frequently demonstrates sub-clinical left ventricular diastolic impairment (with a higher likelihood of the need for mechanical ventilation in those with systolic impairment and reduced ejection fraction).7,12
Table 1.
Representative studies addressing the acute cardiovascular manifestations of coronavirus infection and their clinical implications
| Outbreaks | First author and cohort size | Cardiovascular manifestations | Outcomes |
|---|---|---|---|
| SARS | Yu et al.5 (n = 121) | Hypotension, tachycardia, bradycardia, cardiomegaly, and arrhythmia | Mostly transient |
| Pan et al.6 (n = 15) | Cardiac arrest | Death | |
| Li et al.7 (n = 46) | Sub-clinical diastolic impairment without systolic involvement on echocardiography | Reversible on clinical recovery | |
| MERS | Alhogbani8 (n = 1) | Acute myocarditis and acute-onset heart failure | Recovered |
| COVID-19 | Huang et al.9 (n = 41) | Myocardial injury (manifesting with increased high-sensitivity cardiac troponin I) in five patients | Four patients required intensive care |
| Wang et al.10 (n = 138) | Acute cardiac injury (7.2%), shock (8.7%), and arrhythmia (16.7%) | Most patients required intensive care |
Early COVID-19 case reports suggest that patients with underlying conditions are at higher risk for complications or mortality—up to 50% of hospitalized patients have a chronic medical illness (40% cardiovascular or cerebrovascular disease). In the largest published clinical cohort of COVID-19 to date, acute cardiac injury, shock, and arrhythmia were present in 7.2%, 8.7%, and 16.7% of patients, respectively,10 with higher prevalence amongst patients requiring intensive care.
Viral pathology and links to the cardiovascular system
Chronic cardiovascular disease may become unstable in the setting of viral infection as a consequence of imbalance between infection-induced increase in metabolic demand and reduced cardiac reserve. Patients with coronary artery disease and heart failure may be at particular risk as a result of coronary plaque rupture secondary to virally induced systemic inflammation, and rigorous use of plaque stabilizing agents (aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors) has been suggested as a possible therapeutic strategy. Pro-coagulant effects of systemic inflammation13 may increase the likelihood of stent thrombosis and assessment of platelet function and intensified anti-platelet therapy should be considered in those with a history of previous coronary intervention.
The beta-coronavirus virus underlying COVID-19 strains from the same species as SARS and has recently been named SARS-CoV-2. SARS-CoV binds to cells expressing appropriate viral receptors, particularly angiotensin-converting enzyme 2 (ACE2).14 Angiotensin-converting enzyme 2 is also expressed in the heart, providing a link between coronaviruses and the cardiovascular system. Murine models and human autopsy samples demonstrate that SARS-CoV can down-regulate myocardial and pulmonary ACE2 pathways, thereby mediating myocardial inflammation, lung oedema, and acute respiratory failure.15 Pro-inflammatory cytokines are up-regulated in the lungs and other organs of SARS patients, and the systemic inflammatory response syndrome provides a possible mechanism for multi-organ failure (usually involving the heart) in severe cases.
Does the risk of cardiovascular disease persist?
Heightened systemic inflammatory and pro-coagulant activity can persist in survivors of hospitalization for community-acquired pneumonia long after resolution of the index infection. The clinical effects of pneumonia have been linked to increased risk of cardiovascular disease up to 10-year follow-up16 and it is likely that cases infected via respiratory virus outbreaks will experience similar adverse outcomes. Therapeutic use of corticosteroids further augments the possibility of adverse cardiovascular events. However, long-term follow-up data concerning the survivors of respiratory virus epidemics are scarce. Lipid metabolism remained disrupted 12 years after clinical recovery in a metabolomic study amongst 25 SARS survivors,17 whereas cardiac abnormalities observed during hospitalisation in eight patients with H7N9 influenza returned to normal at 1-year follow-up.18 Whilst viral phenotype, baseline clinical characteristics, initial disease severity, and immediate management impact on short-term survival, long-term prognosis following outbreaks of respiratory virus infection may equally depend upon the extra-pulmonary manifestations. Serial follow-up studies amongst the survivors of acute infection are sorely needed.
Conclusions
Increased human mobility and ready access to international travel have accelerated the rate of microbial transmission around the world and global pandemics are a persistent threat. Outbreaks of viral respiratory illness threaten public health but the associated extra-pulmonary manifestations and their prolonged consequences are frequently overlooked. COVID-19 is a rapidly evolving epidemic with uncertain clinical characteristics and further acceleration seems likely.19 Pre-existing cardiovascular disease may contribute to adverse early clinical outcomes and infection may have longer-term implications for overall cardiovascular health (Take home figure). Inter-disciplinary management of severe cases (with priority for those with pre-existing cardiovascular disease) and prolonged clinical follow-up are therefore essential.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Sellers SA, Hagan RS, Hayden FG, Fischer WA.. The hidden burden of influenza: a review of the extra-pulmonary complications of influenza infection. Influenza Other Respir Viruses 2017;11:372–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Song Z, Xu Y, Bao L, Zhang L, Yu P, Qu Y, Zhu H, Zhao W, Han Y, Qin C.. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses 2019;11:E59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dawood FS, Iuliano AD, Reed C, Meltzer MI, Shay DK, Cheng P-Y, Bandaranayake D, Breiman RF, Brooks WA, Buchy P, Feikin DR, Fowler KB, Gordon A, Hien NT, Horby P, Huang QS, Katz MA, Krishnan A, Lal R, Montgomery JM, Mølbak K, Pebody R, Presanis AM, Razuri H, Steens A, Tinoco YO, Wallinga J, Yu H, Vong S, Bresee J, Widdowson M-A.. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis 2012;12:687–695. [DOI] [PubMed] [Google Scholar]
- 4. Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL.. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol 2016;1:274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yu C-M. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J 2006;82:140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan S, Zhang H, Li C, Wang C.. [Cardiac arrest in severe acute respiratory syndrome: analysis of 15 cases]. Zhonghua Jie He He Hu Xi Za Zhi 2003;26:602–605. [PubMed] [Google Scholar]
- 7. Li SS, Cheng C, Fu C, Chan Y, Lee M, Chan JW, Yiu S.. Left ventricular performance in patients with severe acute respiratory syndrome: a 30-day echocardiographic follow-up study. Circulation 2003;108:1798–1803. [DOI] [PubMed] [Google Scholar]
- 8. Alhogbani T. Acute myocarditis associated with novel Middle East respiratory syndrome coronavirus. Ann Saudi Med 2016;36:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;doi:10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Badawi A, Ryoo SG.. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis 2016;49:129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris JE, Shah PJ, Korimilli V, Win H.. Frequency of troponin elevations in patients with influenza infection during the 2017–2018 influenza season. Int J Cardiol Heart Vasc 2019;22:145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Libby P, Simon DI.. Inflammation and thrombosis: the clot thickens. Circulation 2001;103:1718–1720. [DOI] [PubMed] [Google Scholar]
- 14. Wit E D, Doremalen N. V, Falzarano D, Munster VJ.. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016;14:523–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, Butany J.. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest 2009;39:618–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-C, Newman A, Loehr L, Folsom AR, Elkind MS, Lyles MF, Kronmal RA, Yende S.. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA 2015;313:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, Xu L, Li X, Liu H, Yin P, Li K, Zhao J, Li Y, Wang X, Li Y, Zhang Q, Xu G, Chen H.. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep 2017;7:9110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang J, Xu H, Yang X, Zhao D, Liu S, Sun X, Huang J, Guo Q.. Cardiac complications associated with the influenza viruses A subtype H7N9 or pandemic H1N1 in critically ill patients under intensive care. Braz J Infect Dis 2017;21:12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Madjid M, Solomon SD, Vardeny O, Mullen B. Cardiac implications of coronavirus (COVID-19). https://www.acc.org/latest-in-cardiology/articles/2020/02/13/12/42/acc-clinical-bulletin-focuses-on-cardiac-implications-of-coronavirus-2019-ncov. Accessed18 Feb 2020.