Abstract
Background
The coronavirus 2019 (COVID-19) pandemic is a clinical situation that could be used as prototype for implementation of new systems of care.
Methods
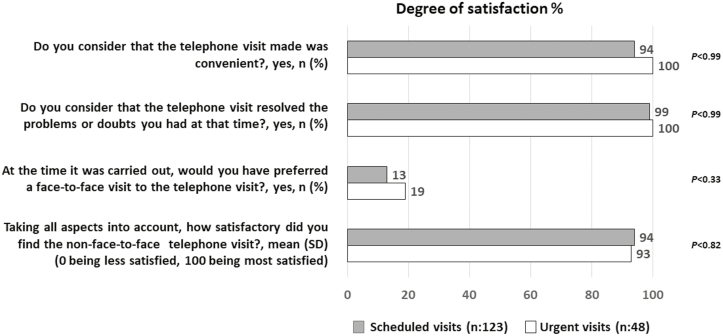
This was a single-center, cross-sectional study. We evaluated the feasibility of a strategy based on the conversion of face-to-face visits to telephone consultations to manage IBD outpatients during the COVID-19 pandemic. A 4-item telephone survey (3 closed questions and a 100-point numeric description scale) was conducted to evaluate satisfaction of patients with telephone consultations.
Results
Between March 11 and April 8, 2020, 98% of the 216 scheduled face-to-face visits could be converted to telephone consultations, and we resolved an additional 162 urgent consultations by telephone. The rate of IBD-related hospitalization and visits to the emergency department decreased by 50% and 58%, respectively, compared with rates in the same period the previous year. The 4-item survey was conducted in 171 outpatients. In closed questions, patients reported a very high degree of satisfaction with telephone consultations, with no differences between scheduled (n = 123) and urgent consultations (n = 48; P = NS). The overall satisfaction rating with the telephone consultation evaluated with the numerical description scale was 94% and 93% for scheduled and urgent consultations, respectively (P < 0.82). Less than 20% of patients would have preferred a face-to-face visit to the telephone consultation at the time.
Conclusions
A strategy based on the conversion of face-to-face visits to telephone consultations was able to guarantee a minimum standard quality of care during the COVID-19 pandemic. Patients reported a very high degree of satisfaction with telephone consultations.
Keywords: COVID-19, inflammatory bowel disease, telemedicine, telephone consultation, SARS-CoV-2, patient-reported experience measures
INTRODUCTION
The World Health Organization recently declared the outbreak of coronavirus 2019 (COVID-19), caused by infection with novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), as a pandemic of international concern. Health facilities in the worst affected regions are struggling, resulting in extensive reallocation of hospital resources to help manage COVID-19 patients. As a consequence, rapidly evolving national and international statements regarding COVID-19 recommended avoiding in-person care for treatment of patients with no suspicion of infection; not only would this alleviate the burden on hospital resources but it would also eliminate the risk of infection in the clinic.1, 2
The safety and management of patients with inflammatory bowel disease (IBD) during the pandemic are of particular concern,3–5 given that management often requires the use of immune-modifying therapies, some of which have well-described risks for severe viral infections.6, 7 Although several studies offer guidance on gold-standard strategies for improved care of IBD patients in western countries, outcomes of such strategies have not been evaluated.8, 9
The aim of this study was to assess the feasibility of a strategy based on the conversion of face-to-face visits to remote telephone consultations to improve care of patients with IBD during the COVID-19 pandemic, and to evaluate satisfaction of patients with telephone consultations.
METHODS
This was a single-center, cross-sectional study. The eligible population included 1918 patients with an established diagnosis of IBD followed at an IBD referral unit in the Madrid region of Spain (IBD Unit of Hospital Clínico San Carlos, Madrid). Baseline demographic and clinical characteristics, in addition to treatments for IBD, were extracted from the prospectively maintained database ENEIDA (Supplementary Table 1). An appointed committee, which included IBD staff, IBD nurses, data manager, and administrative staff, developed a strategy to promote the use of telehealth care facilities. Face-to-face scheduled visits in the outpatient clinic were converted to telephone consultations at the same time and on the same day as the scheduled visit. Patients were notified of the change by the administrative staff. In addition, the existing nurse advice telephone line was reinforced to receive calls from patients seeking medical attention or health information during the pandemic. Inflammatory bowel disease nurses triaged incoming calls and decided if the case required an urgent remote consultation by staff or if the patient was only requesting health information in the pandemic situation. These IBD nurses advised all patients to maintain their current treatment regimens to avoid relapse due to nonadherence and to strictly follow the general health recommendations to prevent COVID-19, according to international or national guidance. We discouraged IBD patients from coming to the emergency department without prior indication from IBD staff, and hospitalizations were avoided if possible. During virtual consultations, IBD staff and nurses questioned patients for suggestive symptoms or for a confirmed diagnosis of COVID-19, and cases were recorded.
Scheduled or urgent telephone consultations where made by 2 physicians of the IBD Unit. Clinical data including patient-reported outcomes were noted using the Harvey-Bradshaw index (HBI) for Crohn’s disease (CD) and the partial Mayo score (PMS) for ulcerative colitis (UC); blood or fecal test results were taken from the medical chart when available. Based on this information, physicians gave indications about therapy and follow-up procedures. Changes in treatments were introduced in the single prescription module that allows patients to collect their medications at pharmacies. In general, ongoing maintenance therapy was unchanged to avoid severe IBD flares. In patients diagnosed with COVID-19, immunosuppressants or biologic agents were temporarily discontinued according to guidance.3–5 Endoscopic disease assessment was limited to absolutely essential cases, including the most urgent suspected new IBD cases. Biologics clinic visits were maintained to administer IV drugs with rigorous measures to avoid cross-contamination. The day before scheduled IV dosing, patients were called by the IBD nurse and questioned for symptoms suggestive of COVID-19 and/or close contacts with infected cases in the previous 2 weeks. Infusion date was delayed when necessary. Health care workers and patients used surgical masks and latex gloves, and a 2-meter distance between chairs was maintained at the biologics clinic. An IBD staff member attended the biologics clinic daily, and a face-to-face visit was made during infusion. Subcutaneous administration of biologics or small molecules was maintained, ensuring the home administration of these therapies.
Survey Questionnaire
To evaluate patient-reported experience measures (PREMs) with telephone consultations, we developed a cross-sectional 4-item telephone survey that was conducted by an IBD staff member or nurse between 2 and 4 weeks after the initial call. To minimize nonresponse rates, we kept the survey short and focused on 3 closed questions and a last question with a 100-point numeric description scale, where 0 represents the least satisfaction and 100 the most satisfaction, to allow for conversion of subjective answers to quantitative data (Fig. 1). To validate the survey instrument, the initial content was first analyzed by 3 IBD nurses and 2 IBD staff members and corrected as necessary. We then performed a pilot evaluation in a random sample of 20 IBD patients to validate the survey questionnaire before full implementation. To assess intra-individual agreement, we repeated the survey at least 10 days apart in a random sample of 20 patients. The survey was conducted in consecutive patients who had a telephone visit each day to complete a sample size of 50% of the remote consultations that day, and so on.
FIGURE 1.
Results of a cross-sectional 4-item telephone survey (3 closed questions and a last question using a 100-point numeric description scale) that evaluate patient preferences and acceptance with telephone consultations: comparison between scheduled and urgent consultations (n = 171).
Ethical Considerations
The study was approved by the clinical research ethics committee of the Hospital Universitario Clínico San Carlos, Madrid, Spain (C.I. 20/258-E_EPA OD, March 26, 2020). Verbal informed consent was obtained from all surveyed patients.
Statistical Analysis
Study variables were summarized descriptively using numbers and percentages for discrete variables and mean and standard deviation (SD) or median and interquartile range (IQR) as appropriate for continuous variables. Responses for each questionnaire item for scheduled and urgent telephone consultations were compared. We evaluated test-retest reliability using the Cohen kappa for closed questions and intraclass correlation coefficient (ICC) for numeric description scale.
RESULTS
The health care activities carried out in the IBD unit and hospital facilities between March 11 and April 8, 2020, are summarized in Table 1. Of the 216 scheduled face-to-face visits in this period, 98% could be converted to remote telephone consultations, and we resolved an additional 162 urgent consultations by telephone. In the study period, we performed 58 and 10 face-to-face care visits at the biologics clinic and at the IBD unit, respectively. During the study period, only 2 patients required hospitalization, and 5 required a visit to the emergency department for their IBD, which represents a reduction of 50% and 58% in the rate of IBD-related hospitalization and visits to the emergency department, respectively, compared with the rates in the same period of the previous year. Inflammatory bowel disease nurses provided remote health advice to 584 patients.
TABLE 1.
Health Care Activities Carried Out in the Inflammatory Bowel Disease Unit and Hospital Facilities Between March 11 and April 8, 2020, to Meet the Needs of IBD Patients
| Health Care Activities | No. |
|---|---|
| Face-to-face care scheduled visits converted to remote telephone visits, n (%) | 212 (98%) |
| Missed visits, n (%) | 4 (2%) |
| Urgent remote telephone visits | 162 |
| Face-to-face visits during administration of doses at the biologics clinic | 58 |
| Face-to-face care visits at the IBD unit facilities | 10 |
| IBD nurses remote telephone visits for health advice | 584 |
| Reviews by nurse of safety analysis in patients on immunosuppressant’s | 36 |
| Health advice consultations resolved by email | 48 |
| Emergency department visits for possible IBD complications | 5 |
| Emergency department visits due to symptoms suggestive of COVID-19 | 9 |
| Hospitalizations for complicated IBD | 2 |
| Hospitalizations for COVID-19 | 6 |
| Training in the administration of SC biologics by IBD nurse | 12 |
| Administrative support to ensure home care delivery of SC biologics | 45 |
| Remote telephone visits for patients included in post-authorization safety registries | 10 |
| Face-to-face care visits for patients included in Phase 3 trials | 3 |
The 4-item telephone survey was evaluated in 171 outpatients. Surveys from 14 patients were excluded because they were not included in the ENEIDA database, and 2 patients (1%) did not provide informed consent. Table 2 shows the baseline characteristics of patients and changes in treatment and reason during telephone consultations. During scheduled telephone consultations, a significantly higher percentage of patients were in remission. During urgent consultations, a higher percentage of patients required discontinuation of immunosuppressants or biologics due to diagnosis or high suspicion of COVID-19, needed corticosteroid courses or mesalazine initiation or escalation to treat flares, or received antibiotics for enteral infections.
TABLE 2.
Baseline Characteristics of Patients, Diagnosis, and Changes in Treatment During Remote Telephone Consultations (n = 171)
| Characteristic | Scheduled Visits (n = 123) | Urgent Visits (n = 48) | P |
|---|---|---|---|
| Sex, male, n (%) | 55 (45) | 24 (50) | 0.53 |
| Age (years), mean (SD) | 49 (14) | 47 (13) | 0.39 |
| Duration of disease (years), median (IQR) | 14 (9–20) | 13 (8–21) | 0.43 |
| Disease: | |||
| CD, n (%) | 57 (46) | 19 (39) | 0.42 |
| UC, n (%) | 66 (54) | 29 (61) | |
| CD localization: L1, n (%); L2, n (%); L3, n (%) | 26 (46); 9 (16); 22 (38) | 10 (53); 4 (21); 5 (26) | 0.61 |
| CD behavior: B1, n (%); B2, n (%); B3, n (%) | 36 (63); 5 (9); 16 (28) | 10 (53); 3 (16); 6 (31) | 0.61 |
| UC extension: E1, n (%); E2, n (%); E3, n (%) | 17 (26); 21 (32); 27 (41) | 3 (10); 8 (27); 18 (62) | 0.12 |
| IBD activity index at visit | |||
| CD (HBI), mean (SD) | 0.23 (0.66) | 2.63 (3.56) | 0.009 |
| UC (PMS), mean (SD) | 0.18 (0.63) | 1.48 (2.05) | 0.003 |
| IMM treatment, n (%) | 45 (36) | 21 (44) | 0.39 |
| Azathioprine, n (%) | 27 (60) | 14 (67) | |
| 6-mercaptopurine, n (%) | 8 (18) | 2 (9) | |
| Methotrexate, n (%) | 6 (13) | 3 (14) | |
| Tofacitiniba, n (%) | 4 (9) | 2 (9) | |
| Biological treatment, n (%) | 26 (21) | 20 (42) | 0.007 |
| Infliximab, n (%) | 4 (15) | 5 (25) | |
| Adalimumab, n (%) | 13 (50) | 7 (35) | |
| Golimumab, n (%) | 5 (19) | 2 (10) | |
| Vedolizumab, n (%) | 0 (0) | 3 (15) | |
| Ustekinumab, n (%) | 4 (15) | 3 (15) | |
| Biological + IMM treatment, n (%) | 11 (9) | 10 (21) | 0.033 |
| IMM alone, n (%) | 34 (28) | 11 (23) | 0.53 |
| Biologics alone, n (%) | 15 (12) | 10 (21) | 0.15 |
| Clinical diagnosis during telephone visit | <0.001 | ||
| Remission, n (%) | 117 (95) | 23 (48) | |
| COVID-19 symptoms, n (%) | 2 (2) | 11 (23) | |
| Flare, n (%) | 2 (2) | 10 (44) | |
| Gastroenteritis, n (%) | 0 (0) | 5 (10) | |
| Other, n (%) | 2 (2) | 1 (2) | |
| Changes in treatment during telephone visit | |||
| IMM and/or biologics delayed, n (%) | 2 (2; 1 AZA, 1 IFX) | 9 (19; 3 AZA, 2 IFX, 2 ADA, 1 TOF) | 0.02 |
| Corticosteroids or budesonide course, n (%) | 2 (2; 1 BUD, 1 BEC) | 5 (10; 3 BUD, 1 BEC, 1 CE) | 0.05 |
| Antibiotics, n (%) | 0 (0) | 5 (10) | 0.04 |
| Oral or topical 5-ASA, n (%) | 1 (1) | 7 (14) | 0.03 |
| 5-ASA dose escalation, n (%) | 0 (0) | 4 (8) | 0.05 |
Abbreviations: IQR, interquartile range; “Montreal classification” of Crohn’s disease (CD); disease location (L): L1 terminal ileum, L2 colon, L3 ileocolon, L4 upper gastrointestinal tract; disease behavior (B): B1 nonstricturing nonpenetrating; B2 stricturing, B3 penetrating; E1: proctitis, E2: left-sided, E3: extensive; IMM, immunomodulator; AZA,azathioprine; IFX, infliximab; ADA, adalimumab; TOFA, tofacitinib; BUD, budesonide; BEC, beclomethasone dipropionate; CE; systemic corticosteroids.
aTofacitinib is a JAKinase inhibitor not similar to conventional.
In the closed questions, patients reported a very high degree of satisfaction with and acceptance of telephone consultations, with no differences between scheduled (n = 123) and urgent consultations (n = 48; Fig. 1). Less than 20% of patients would have preferred a face-to-face visit to the telephone visit at the time. The global satisfaction rating with the telephone consultation evaluated with the numerical scale was 94% and 93% for scheduled and urgent consultations, respectively (P < 0.82). Test-retest reliability of the survey questionnaire was perfect for closed questions (Cohen’s kappa 1), and excellent for the numeric description scale (ICC 0.97; 95% CI, 0.95–0.98).
DISCUSSION
The COVID-19 pandemic is a clinical situation that could be used as prototype for implementation of a telehealth consultation system for evaluation of high-risk populations like IBD patients. Although an increasing number of studies have recommended strategies to reorganize IBD units in western countries during the pandemic,8, 9 the outcomes of such procedures have only been briefly evaluated in one study.10
Here, we report the outcomes and patient perception of a strategy based on the conversion of face-to-face visits to remote telephone consultations to improve care of outpatients with IBD during the COVID-19 pandemic. The conversion of outpatient follow-up visits to virtual consultations was feasible, with 98% of consultations resolved by telephone or email, avoiding travel to in-person care sites, and with a very low rate of missed visits. During remote consultations, we were able to escalate treatment due to IBD flares, avoiding face-to-face clinic visits. In accordance with guidance, we temporarily discontinued immune-modifying therapies in patients with diagnosis or strong clinical suspicion of COVID-19.3–5 During the study period, very few patients required hospitalization or emergency department visits related to IBD, which was important in the days when hospitals’ health facilities were overwhelmed. Twelve patients were diagnosed with COVID-19.11 Of these, 8 were hospitalized, and 4 self-isolated at home. All COVID-19 cases were community-acquired rather than linked to visits to hospital facilities. The biologics clinic was maintained following the strict protocol to avoid cross contamination, and no cases of COVID-19 were detected. A recent study reported that implementation of virtual clinics, drug home delivery, and IBD networking was able to maintain acceptable standards of care for IBD patients.10 The outcomes of the new system of care implemented during the pandemic helped us determine what kind of patients could be attended and what problems could be resolved without a face-to-face consultation and supported efforts to reorganize the activities of the IBD clinic during the de-escalation period.
Some surveys have assessed health care providers’ perceptions of the implementation of new care systems during the pandemic, but studies that evaluate patient-reported indicators for assessing health system performance are lacking. As part of this study, we administered for the first time a survey evaluating consumer perceptions and preferences with the new system of care. Patient experience is one important measure of the quality and efficiency of health care, and the use of PREMs is recommended. Outpatients reported a very high degree of satisfaction with telephone consultations, with no differences between scheduled and urgent consultations, and very few patients would have preferred a face-to-face visit at the time. Home patient management is a well-accepted approach by patients with IBD, as evidenced by the high adherence to home therapies or recommendations from physicians.12 Telemedicine has also been associated with a reduction in face-to-face visits and hospitalizations and could be a valid alternative to improve the quality of IBD patient care.13–15 These studies were performed before the COVID-19 outbreak, and we believe that results of our study confirmed the validity of telemedicine to manage patients with IBD while still maintaining quality standards of care. Results of a global telemedicine survey among gastroenterologists by the International Organization for the Study of Inflammatory Bowel Disease (IOIBD) demonstrated the shift from face-to face clinics to remote telemedicine during COVID-19, with telephone consultations increasing the most, currently accounting for over half of all IBD visits.16 A survey among IBD gastroenterologists in Spain reproduces the global results, reflecting the rapid structural changes in the IBD units to guarantee virtual, non-face-to-face consultations.17
Our study has some limitations. The reduction in visits to the emergency department and hospitalization may not be attributable to telehealth intervention. During the pandemic, avoidance of hospital health facilities was a conscious choice by patients (and providers to some degree) due to fear of contracting COVID-19. Furthermore, a period of 1 month may be insufficient to assess the impact on medical resource usage. We were not able to evaluate provision of telemedicine by video consultation due to the lack of appropriate equipment and technological skills at our outpatient clinics. The surveys were carried out by staff from the IBD unit and not by independent surveyors, which could have biased the responses of the patients.
In conclusion, the reorganization of the IBD clinic following a strategy of switching face-to-face visits to remote telephone consultations when possible was able to guarantee a minimum standard quality of care to our patients during the COVID-19 pandemic. The implementation of the new care system could have contributed to a reduction in emergency department visits and hospitalization when the pandemic was at its worst. Considering the high degree of satisfaction in all PREMs with remote consultations, once the pandemic is over, health care providers could consider applying some of the principles of telemedicine permanently. Doing so, always in accordance with patient preferences, would represent a deeper commitment to patient-centered care.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Dr. G. Morley for reviewing the English manuscript.
Author Contributions: CT designed the study, collected and analyzed the data, and wrote the article. CA designed the questionnaire, collected data, and treated patients. DO extracted data from database, performed statistical analysis, and designed tables. MM and MC triaged telephone consultations, conducted the survey, and offered health advice. AV collected data and treated patients. All authors read and approved the final manuscript.
Conflicts of Interest: CT has served as a speaker, consultant, and advisory board member for MSD, Abbvie, Hospira, Pfizer, Takeda, Janssen, Ferring, Faes Farma, Shire Pharmaceuticals, Dr. Falk Pharma, Gebro Pharma, and Tillots. CA has served as a speaker for Janssen and has prepared promotional material for Falk Pharma. These activities were not related to the present work. The remaining authors have no conflicts of interest to declare.
REFERENCES
- 1.Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html. Accessed 8 July 2020.
- 2. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 3. Rubin DT, Feuerstein JD, Wang AY, et al. AGA clinical practice update on management of inflammatory bowel disease during the COVID-19 pandemic: expert commentary. Gastroenterology. 2020;159:350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kennedy NA, Jones GR, Lamb CA, et al. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID-19 pandemic. Gut. 2020;69:984–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IOIBD. COVID 19 and IBD Webinars and Guidelines. https://ioibd.org/covid-19-and-ibd-webinars-and-guidelines. Accessed 8 July 2020.
- 6. Wisniewski A, Kirchgesner J, Seksiket P, et al. Increased incidence of systemic serious viral infections in patients with inflammatory bowel disease associates with active disease and use of thiopurines. United Eur Gastroenterol J. 2019;0:1–11. doi: 10.1177/2050640619889763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ford AC, Peyrin-Biroulet L. Opportunistic infections with anti-tumor necrosis factor-α therapy in inflammatory bowel disease: meta-analysis of randomized controlled trials. Am J Gastroenterol. 2013;108:1268–1276. 10.1038/ajg.2013.138. [DOI] [PubMed] [Google Scholar]
- 8. Fiorino G, Allocca M, Furfaro F, et al. Inflammatory bowel disease care in the COVID-19 pandemic era: the Humanitas, Milan experience. J Crohns Colitis. 2020. 10.1093/ecco-jcc/jjaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Occhipinti V, Pastorelli L. Challenges in the care of IBD patients during the CoViD-19 pandemic: report from a “Red Zone” area in Northern Italy. Inflamm Bowel Dis. 2020;26:793–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Allocca M, Fiorino G, Furfaro F, et al. Maintaining the quality standards of care for inflammatory bowel disease patients during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2020. doi: 10.1016/j.cgh.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Taxonera C, Sagastagoitia I, Alba C, et al. 2019 Novel Coronavirus Disease (COVID-19) in patients with inflammatory bowel diseases. Aliment Pharmacol Ther. 2020. doi: 10.1111/apt.15804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cross RK, Finkelstein J. Feasibility and acceptance of a home telemanagement system in patients with inflammatory bowel disease: a 6-month pilot study. Dig Dis Sci. 2007;52:357–364. 10.1007/s10620-006-9523-4. [DOI] [PubMed] [Google Scholar]
- 13. de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390:959–968. [DOI] [PubMed] [Google Scholar]
- 14. Cross RK, Langenberg P, Regueiro M, et al. A randomized controlled trial of TELEmedicine for patients with inflammatory bowel disease (TELE-IBD). Am J Gastroenterol. 2019;114:472–482. [DOI] [PubMed] [Google Scholar]
- 15. Li SX, Thompson KD, Peterson T, et al. Delivering high value inflammatory bowel disease care through telemedicine visits. Inflamm Bowel Dis. 2017;23:1678–1681. [DOI] [PubMed] [Google Scholar]
- 16. Lees CW, Regueiro M, Uma Mahadevan M, et al. Innovation in IBD care during the COVID-19 pandemic: results of a global telemedicine survey by the international organization for the study of inflammatory bowel disease. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin Arranz E, Suarez Ferrer C, García Ramírez L, et al. Management of COVID-19 pandemic in Spanish inflammatory bowel disease units: results from a national survey. Inflamm Bowel Dis. 2020;26:1149–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.