Abstract
Background and Aims
Persons with inflammatory bowel disease (IBD) may be particularly vulnerable to COVID-19 either because of their underlying disease or its management. Guidance has been presented on the management of persons with IBD in the time of this pandemic by different groups. We aimed to determine how gastroenterologists around the world were approaching the management of IBD.
Methods
Members of the World Gastroenterology Organization (WGO) IBD Task Force contacted colleagues in countries largely beyond North America and Europe, inviting them to review the WGO website for IBD and COVID-19 introduction, with links to guideline documents, and then to respond to 9 ancillary open-ended management questions.
Results
Fifty-two gastroenterologists from 33 countries across 6 continents completed the survey (April 14 to May 16, 2020). They were all adhering for the most part to published guidelines on IBD management in the COVID-19 era. Some differences and reductions in services related to access, and some related to approach within their communities in terms of limiting virus spread. In particular, most gastroenterologists reduced in-person clinics (43 of 52), limited steroid use (47 of 51), limited elective endoscopy (45 of 52), and limited elective surgeries (48 of 51). If a patient was diagnosed with COVID-19, immunomodulatory therapy was mostly held.
Conclusions
In most countries, the COVID-19 pandemic significantly altered the approach to persons with IBD. The few exceptions were mostly based on low burden of COVID-19 in individual communities. Regardless of resources or health care systems, gastroenterologists around the world took a similar approach to the management of IBD.
Keywords: COVID-9, pandemic, inflammatory bowel disease, immunomodulatory therapy, management
INTRODUCTION
Inflammatory bowel disease (IBD) is a global disease with high prevalence in the Western world and rapidly rising incidence in newly industrialized countries in Asia, Africa, and Latin America.1–3 The management of IBD may differ by geography with economically more advanced countries having greater access to health care resources such as endoscopy and expensive therapies like biologics.4 Geographic differences and inequities in access to IBD management may be heightened during the coronavirus 2019 disease (COVID-19) pandemic, as lockdown measures have placed significant strain on government and personal finances.
There has been uncertainty to what extent persons with IBD may be at increased risk of being infected with the severe acute respiratory syndrome coronavirus (SARS-CoV-2), whether their outcomes from COVID-19 would be different from the general population, and whether immunomodulatory therapies (including both immunosuppressive and biological therapies) used in the treatment of IBD pose a significant increased risk for adverse outcomes from COVID-19. Despite the uncertainty, there has been some agreement reached among international IBD specialists, including the International Organization for the Study of IBD (IOIBD),5 the American Gastroenterological Association (AGA),6 the British Society for Gastroenterology (BSG),7 and the European Crohn’s and Colitis Organisation (ECCO).8 Recommendations include continuing all immunomodulatory medications in patients with IBD, reducing steroid doses as much as possible, limiting elective endoscopies, and encouraging telemedicine in place of in-person clinic visits.
Although the most severe aspect of COVID-19 infections are respiratory symptoms, gastrointestinal (GI) symptoms are common. A meta-analysis suggested that gastrointestinal symptoms may be seen in 5%–10% of persons presenting with COVID-19.9 Moreover, a report from Hubei Province, China (Wuhan is the capital city), the initial COVID-9 epicenter, suggested that nearly 16% of affected persons had gastrointestinal symptoms.10 In 2 large American series, gastrointestinal symptoms were seen in 32% of 1141 persons with COVID-19 in California11 and in 33% of 1059 affected persons with COVID-19 from New York City.12 In this New York City study, having IBD or being on immunosuppressive therapy were not associated with presenting with gastrointestinal symptoms. However, the possibility that gastrointestinal symptoms are part of a COVID-19 infection poses a particular challenge in managing persons with IBD. For persons with IBD presenting with increasing gastrointestinal symptoms, the challenge for the clinician is whether these symptoms reflect a flare of IBD or COVID-19.
The World Gastroenterology Organization (WGO) has a mandate to deliver education and information to clinicians worldwide. An introduction to management challenges for persons with IBD was presented on the WGO website with links to some of the reports described previously.13 We aimed to develop an understanding of international management approaches to persons with IBD during the pandemic, with an emphasis on countries that were less likely to be represented in guidelines put forth by the IOIBD, AGA, BSG, or ECCO. In particular, we wanted to determine how management of IBD was being handled in countries with fewer resources and to what extent management differed from North America and Europe.
METHODS
Members of the WGO who have worked on global IBD-related practice guidelines (WGO IBD Task Force) reached out to colleagues across the world to review current recommendations regarding management of persons with IBD and to answer ancillary questions about their practices in their communities during the COVID-19 pandemic. Most of these colleagues had leadership roles in the management of IBD in their respective communities. It was not the intention to get as many gastroenterologists as possible to respond but rather to get as many countries represented as possible, especially from countries outside of Canada, the United States, and Europe. Gastroenterologists mostly from North America and Europe participated in the position papers from the AGA, BSG, ECCO, and IOIBD.1–4 Hence, it was the goal to reach out to gastroenterologists who would be practicing in countries less likely to be represented in these guidelines. Some gastroenterologists from North America and Europe were included. Nine questions were sent electronically and allowed for open-ended responses. The 9 questions posed to participants were
1) What is the effect of resource availability on recommendations (referring to recommendations published by international organizations)?
2) Are you still having in-person clinics?
3) Are you conducting any elective endoscopy in IBD patients, and if so, for which indications have you been undertaking endoscopy?
4) If an IBD patient develops COVID-19, how does this affect other treatment?
5) What is the role of surgery in the face of COVID-19? Does COVID-19 affect the indications for surgery or the scope of surgical interventions?
6) If in a low resource area and there is no access to biologicals, how does one address steroid use in the current environment of COVID-19 concerns?
7) How should one investigate and manage someone presenting with potential new onset IBD? How is this affected by resource availability?
8) Considering that at least 5% of persons with COVID-19 present with isolated GI symptoms when a patient with IBD presents with worsening GI symptoms, are you routinely testing for COVID-19?
9) What is the role of noninvasive markers in assessing disease if endoscopy is not available? For example, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), fecal calprotectin, white blood cell count (WBC), platelet count, radiology? How does resource availability affect this?
Responses were received between April 14, 2020, and May 16, 2020. All responses were collated by one author (CNB), and responses were inputted into tables. Where there were unique responses underscoring an important management issue, this was highlighted in the report.
RESULTS
Fifty-two gastroenterologists from 33 countries across 6 continents completed the survey (due to potential resource allocation differences, Hong Kong was considered separate from China, and Puerto Rico was considered separate from the United States; Fig. 1). Three respondents were pediatric gastroenterologists. The results are summarized after each question and also in the tables (Tables 1–3). Table 1 also presents whether the country is a high income country or not, as per the World Bank.14
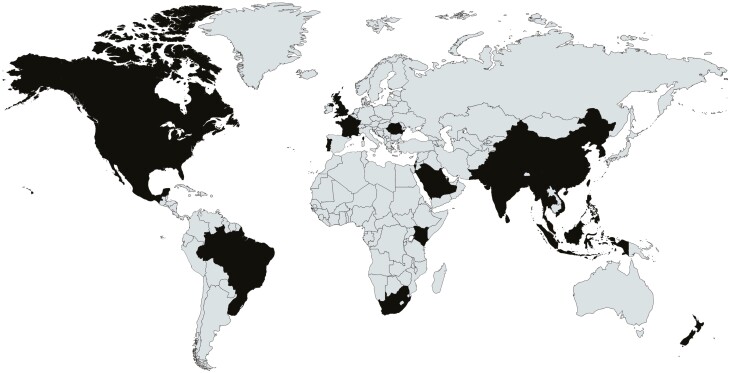
FIGURE 1.
World map highlighting countries represented in this study.
TABLE 1.
Questions 1–3
| Country | High Income* Economy 1=yes 0=No | What is the effect of resource availability on recommendations? | Are you still having in-person clinics? | a) Are you conducting any elective endoscopy in IBD patients; b)for which indications have you been undertaking endoscopy?* |
|---|---|---|---|---|
| Bangladesh (n = 2) | 0 | Significant effect. Limited PPE, COVID-19 testing and hospital beds | Yes but reduced (n = 1) No to private practice, yes in government hospital (n = 2) | a) No (n = 2) |
| Brazil (n = 4) | 0 | No effect. Difference between public and private system | Yes = 1, Yes but reduced = 2, No = 1 | a) No to elective (n = 4) b)Active colitis, cancer, bleeding, obstruction |
| Canada (n = 3) | 1 | No effect | No = 1, Yes but reduced = 2 | a) No to elective (n = 1) Diagnostic endoscopy in IBD to decide on treatment (n = 2) b)Active colitis, bleeding, cancer, obstructions |
| China (n = 4) | 0 | Traffic restrictions limited access. Some limitation on PPE | Yes = 1, Yes but reduced = 1, No = 2 | a)Yes (n = 4) |
| France (n = 1) | 1 | No effect | Yes, but reduced | No to elective Active colitis, bleeding, diagnosis before starting biological therapy. |
| Hong Kong (n = 1) | 1 | No effect | Yes | a)No |
| India (n = 2) | 0 | 1 center had no effect 1 center had limit on testing | Yes, but reduced (n = 2) | a) No b) Active colitis |
| Indonesia (n = 1) | 0 | No effect | Yes | a)No |
| Israel (n = 2) | 1 | No effect | Yes, but reduced (n = 2) | a)No to surveillance but yes to assessing response to biological therapy n = 1 No, n = 1 b)Active colitis, bleeding |
| Kenya (n = 2) | 0 | Limitations (not specified) | Yes, but reduced (n = 2) | a)No (n = 2) |
| Korea (n = 1) | 1 | No effect | Yes | a)No b) Active colitis, newly diagnosed |
| Kuwait (n = 1) | 1 | ? | Yes, but reduced | a)No b) Active colitis, bleeding, anemia, severe diarrhea |
| Malaysia (n = 2) | 0 | No effect | Yes, but reduced (n = 2) | a)No b)undiagnosed lower GI symptoms, bleeding, refractory to therapy, rule out cytomegalovirus |
| Mexico (n = 1) | 0 | No effect | Yes, but reduced | a)No b)prebiological therapy, bleeding, rule out infection |
| Myanmar (n = 2) | 0 | ? | Yes | a)No b)IBD flare having endoscopy |
| Nepal (n = 1) | 0 | No effect | No | a)No |
| New Zealand (n = 1) | 1 | No effect | Yes, but reduced | a) No b) emergency indications |
| Pakistan (n = 2) | 0 | Difference between private and public system | Yes, but reduced (n = 2) | a)No (n = 2) b)if endoscopy necessary COVID-19 test done first |
| Philippines (n = 1) | 0 | Profound effect | No | No |
| Portugal (n = 2) | 1 | No effect | No (n = 1) Yes, but reduced (n = 1) | a)No (n = 2) |
| Puerto Rico (n = 1) | 1 | Remote work not possible for all patients, and not all employers provide appropriate distancing conditions. Limit on PPE availability | No | a)No b)to rule out infection |
| Qatar (n = 1) | 1 | Outpatient endoscopy not available | No | a)No |
| Romania (n = 1) | 0 | No effect | Yes but reduced | a)No |
| Saudi Arabia (n = 1) | 1 | No effect; curfew in place | Yes but reduced | a)No b) disease flares |
| Singapore (n = 1) | 1 | No effect | Yes but reduced | a)No b)disease flares, cancer |
| South Africa (n = 1) | 0 | Patient avoidance of the hospital limits access for blood testing or collecting medicines. Patients with active disease are self- medicating with prednisone that they have stored at home | Yes but reduced | a)No b) acute colitis, newly diagnosed patients pre therapy initiation |
| Sri Lanka (n = 1) | 0 | No effect | Yes but reduced | a) No b) Rectal bleeding |
| Taiwan (n = 1) | 1 | No effect | Yes | a)Yes |
| Thailand (n = 3) | 0 | Limited supply of PPE | Yes but reduced (n = 3) | a)No (n = 3) |
| United Kingdom (n = 1) | 1 | No effect | No | a)No b)acute colitis, GI bleeding |
| United States (n = 2) | 1 | No effect | No = 1, Yes but reduced = 1 | a)No b) large polyp, Endoscopic stricturotomy, balloon dilatation. |
| Uruguay (n = 1) | 1 | No effect | Yes, but reduced | a)No b)Before making major change in therapy |
| Vietnam (n = 1) | 0 | No effect | Yes | a)No b)if change in treatment needed. COVID-19 test done first |
Abbreviations: n refers to number of respondents from that country;? refers to unclear response on that question
*A high-income economy is defined by the World Bank as a country with a gross national income per capita of US$12,376 or more in 2018, calculated using the Atlas method.15
**No response provided in the survey to this question.
TABLE 3.
Questions 7–9
| Country | How should one investigate and manage someone presenting with potentially new onset IBD? How is this affected by resource availability? | Considering that at least 5% of persons with COVID-19 present with isolated GI symptoms when a patient with IBD presents with worsening GI symptoms are you routinely testing for COVID-19? | What is the role of noninvasive markers in assessing disease if endoscopy is not available? For example, ESR, CRP, fecal calprotectin, WBC / platelet count, radiology? How does resource availability affect this testing?* |
|---|---|---|---|
| Bangladesh (n = 2) | No change from pre-COVID Some limitation on access to endoscopy and imaging | Yes (n = 2) | Some limitation on access to imaging (n = 1) All testing done (n = 1) |
| Brazil (n = 4) | Avoid endoscopy | No (n = 3), Yes (n = 1) | All testing done (n = 3) Limited imaging access (n = 1) |
| Canada (n = 3) | Doing colonoscopy. Avoid IV biologicals if possible | No (n = 3) | All testing done (n = 1) Limited imaging access (n = 2) |
| China (n = 4) | Avoid endoscopy and in person testing (n = 2) Doing endoscopy (n = 1) Doing endoscopy and test for COVID 19 first (n = 1) | Yes (n = 4) | All testing done |
| France (n = 1) | Limited endoscopy | Yes | All testing done |
| Hong Kong (n = 1) | Limited endoscopy COVID-19 test first | Yes | All testing done |
| India (n = 2) | Avoid endoscopy (n = 1) Doing endoscopy (n = 1) | No (n = 1) Yes (n = 1) | All testing done |
| Indonesia (n = 1) | No change from pre-COVID | Yes | All testing done |
| Israel (n = 2) | No change from pre-COVID (n = 1) Patients reluctant for testing. Empiric treatment (n = 1) | No (n = 2) | All testing done Fecal calprotectin at home (n = 1) |
| Kenya (n = 2) | No change from pre-COVID-19 (n = 2) | No (n = 2) | All testing done (n = 2) |
| Korea (n = 1) | No change except for avoiding steroids and doing COVID-19 testing | No | All testing done |
| Kuwait (n = 1) | No change from pre-COVID-19 except endoscopy is limited | No | All testing done |
| Malaysia (n = 2) | Avoid endoscopy (n = 1) No change from pre-COVID-19 (n = 1) | Yes (n = 1) No (n = 1) | All testing done (n = 2) |
| Mexico (n = 1) | Endoscopy in suspected UC; diagnosis delayed in CD | No | All testing done |
| Myanmar (n = 2) | Endoscopy is limited | No | All testing done |
| Nepal (n = 1) | Limited access to endoscopy. Using mostly CT scan. | No | Using mostly CT scan and bloodwork. Fecal calprotectin not available. |
| New Zealand (n = 1) | If subacute use labs not endoscopy | No | All testing done |
| Pakistan (n = 2) | Endoscopy being done | No (n = 1) Yes (n = 1) | All testing done |
| Philippines (n = 1) | Endoscopy used to aid in diagnosis and management of IBD in moderate to severe cases | Yes | Imaging tested preferred to serum and stool |
| Portugal (n = 2) | No change (n = 1) Less endoscopy and more imaging, noninvasive testing (n = 1) | No but yes if IBD work up is negative (n = 1) Yes (n = 1) | All testing done (n = 1) More abdominal ultrasound and fecal calprotectin (n = 1) |
| Puerto Rico (n = 1) | Outpatient endoscopy and imaging not available | No | All testing done except limited imaging |
| Qatar (n = 1) | If steroids required patient would be in isolation. Delay biological therapy | Yes for anyone with severe symptoms presenting to the ED. Rest of milder cases managed by telemedicine only and no COVID-19 testing | All testing done but patients avoiding attending clinics for testing |
| Romania (n = 1) | No change | No | All testing done |
| Saudi Arabia (n = 1) | No change except for COVID test first | Yes | All testing done |
| Singapore (n = 1) | No change | No, but yes before biological started | All testing done |
| South Africa (n = 1) | Avoid endoscopy, steroids and thiopurines | No | All testing done |
| Sri Lanka (n = 1) | Flexible sigmoidoscopy and biopsy | No | All testing done |
| Taiwan (n = 1) | No change except for COVID test first | No | All testing done |
| Thailand (n = 3) | Avoid endoscopy | No | Fecal calprotectin and imaging less available |
| Uruguay (n = 1) | No change | No | All testing done. Increased use of fecal calprotectin |
| United Kingdom (n = 1) | Avoid endoscopy; treat empirically | No | All testing done. Fecal calprotectin at home |
| United States (n = 2) | Endoscopy being done (n = 2). COVID-19 testing first (n = 1) empiric 5ASA(n = 1) | No (n = 1) Yes (n = 1) | All testing done except limited imaging |
| Vietnam (n = 1) | No change except for COVID test first | No | All testing done |
Abbreviations: n refers to number of respondents from that country. “?” refers to unclear response on that question.
1) What is the effect of resource availability on recommendations (Table 1)?
Countries across the world were mostly able to abide by the recommendations, but respondents identified several challenges. First, the availability of personal protective equipment (PPE) was limited. Limited supply of PPE was reported from Bangladesh, China, Mexico, Puerto Rico, and Thailand. Further, a discrepancy between private and public hospitals for availability of PPE was reported in Brazil. Second, travel restrictions and home isolation affected availability of resources. For example in China, travel restrictions affected access to medications that was rectified by increased use of e-commerce to facilitate drug delivery. In South Africa, there was concern that patients’ fears of infection reduced their willingness to pick up prescribed medications, leading to patients to use their own personal supplies of prednisone for treatment of flares. From Puerto Rico, there was a comment on limited ability to work from home and limited numbers of employers allowing for proper distancing. Finally, a respondent from India highlighted the problem of limited access to testing.
2) Are you still having in-person clinics (Table 1)?
The vast majority (43 of 52) reported a marked reduction in in-person clinics, restricting clinics to persons who were at least moderately ill. Practices were effectively closed to in-person outpatient visits in Nepal, New Zealand, Philippines, Puerto Rico, the UK, in practices from Canada (a pediatric practice), in 2 of 4 clinics in China, in one of 3 in Brazil, in 1 of 2 in Portugal, and 1 of 2 in the US surveys. Practices from Indonesia, Korea, Myanmar, Taiwan, and Vietnam and 2 of 4 from China and 1 of 3 from Brazil were open to seeing outpatients without reduction.
3) Are you conducting any elective endoscopy in IBD patients, and if so, for which indications have you been undertaking endoscopy (Table 1)?
There was general consensus (45 of 52) that elective endoscopy was not offered. Respondents reported the use of endoscopy in emergencies (eg, bleeding or acute severe disease or cancer) or when endoscopy would change management or be therapeutic. The responses included provisos for urgent indications from 1 of 2 centers in India, Romania, Portugal, Pakistan, and Hong Kong. In Myanmar and Saudi Arabia, elective endoscopy was cancelled, but endoscopy would be undertaken in the setting of an IBD flare. In contrast, a few practices maintained nonurgent endoscopy. For example, 1 center in Israel performed endoscopy to assess mucosal healing, and Taiwan carried out endoscopy for clinical trials and to document rationale for drug reimbursement.
4) If an IBD patient develops COVID-19, how does this affect other treatment (Table 2)?
TABLE 2.
Questions 4–6
| Country | If an IBD patient develops COVID-19, how does this affect other treatment? | What is the role of surgery in IBD in the face of COVID-19? Does COVID-19 affect the indications for surgery or the scope of surgical interventions? | If, in a low resource area and there is no access to biologicals, how does one address steroid use in the current environment of COVID-19 concern? |
|---|---|---|---|
| Bangladesh (n = 2) | No cases yet (n = 2) | Limited surgery availability (n = 1) Urgent surgeries only (n = 1) | Avoid steroids or use lowest possible dose (n = 1) No change in steroid dosing unless COVID-19 positive (n = 1) |
| Brazil (n = 4) | D/C immunomodulatory therapy | Urgent surgeries only | Avoid steroids (n = 1) Selective use (n = 2) Only use budesonide (n = 1) |
| Canada (n = 3) | D/C immunomodulatory therapy Rapid steroid taper | Urgent surgeries only | Selective use (n = 3) Use budesonide (n = 2) |
| China (n = 4) | Reduce or discontinue immunomodulatory therapy D/C steroids (n = 2) | Urgent surgeries only Pre-op testing for COVID-19 (n = 1) | Avoid steroids (n = 3). Use budesonide (n = 1) |
| France (n = 1) | D/C immunomodulatory therapy D/C steroids | Urgent surgeries only | Avoid steroids. Good access to biological therapy |
| Hong Kong (n = 1) | D/C immunomodulatory therapy D/C steroids | Urgent surgeries only | Avoid steroid use; use budesonide |
| India (n = 2) | D/C immunomodulatory therapy (n = 1) May continue therapy depending on severity of and IBD (n = 1) | Urgent surgeries only Laparoscopy after COVID testing (n = 1) | Steroids use more selective, taper more rapid |
| Indonesia (n = 1) | D/C immunomodulatory therapy | No change in approach to surgery | Avoid steroid use |
| Israel (n = 2) | D/C immunomodulatory therapy | Urgent surgeries only (n = 1) No change in surgeries (n = 1, pediatric) | Steroids as needed |
| Kenya (n = 2) | Impact on steroid use (No = 1) No change (n = 1) | No change in approach to surgery (n = 1) Urgent surgeries only (n = 1) | Use more thiopurines and if using steroids patient is in isolation (n = 1) Taper rapidly, reduce dose (n = 1) |
| Korea (n = 1) | D/C immunomodulatory therapy D/C steroids | Urgent surgeries only | Avoid steroid use, rapid tapering Use budesonide |
| Kuwait (n = 1) | Switch IV biological therapy to SC Avoid steroids | ? | Avoid steroids |
| Malaysia (n = 2) | Continue maintenance therapy (n = 1) D/C immunomodulatory therapy (n = 1) | Urgent surgeries only | Rapid steroid taper |
| Mexico (n = 1) | 5ASA, budesonide, vedolizumab continued; D/C other immunomodulatory therapy D/C steroids | Urgent surgeries only | Selective steroid use where biological therapy can not be accessed budesonide used. |
| Myanmar (n = 2) | D/C immunomodulatory therapy | Urgent surgeries only. Done in negative pressure operating room. | Avoid steroids; use budesonide |
| Nepal (n = 1) | Use lower dose steroids | Urgent surgeries only | Avoid steroid use, rapid tapering |
| New Zealand (n = 1) | D/C immunomodulatory therapy | Urgent surgeries only | Avoid steroid use |
| Pakistan (n = 2) | Continue 5ASA, thiopurines, reduce steroids, biological therapy not available (n = 1) No cases yet (n = 1) | Urgent surgeries only Pre-op testing for COVID-19 (n = 1) | No change in steroid use (n = 1) Use as little as possible (n = 1) |
| Philippines (n = 1) | No change in mild cases | Avoiding surgery as much as possible | Shorten period of steroid use |
| Portugal (n = 2) | D/C immunomodulatory therapy Rapid steroid taper | Urgent surgeries only | Use steroids if needed even if Covid-19 positive (n = 1) Using steroids to induce remission if starting biologicals but otherwise avoiding doses above 10 mg (n = 1) |
| Puerto Rico (n = 1) | No cases yet | Urgent surgeries only | Avoid steroids; good access to biologicals |
| Qatar (n = 1) | Only biological therapy discontinued | Urgent surgeries only | If steroids required patient would be in isolation |
| Romania (n = 1) | No cases yet | Urgent surgeries only | Avoid steroids; good access to biologicals |
| Saudi Arabia (n = 1) | Continue 5ASA, thiopurines; Continue biological therapy depending on disease severity D/C steroids | Urgent surgeries only | Avoid steroids |
| Singapore (n = 1) | No cases yet | Urgent surgeries only | Avoid steroids; good access to biologicals |
| South Africa (n = 1) | No cases yet | Surgeries on hold (no mention of urgent cases) | Avoid steroid use except in acute severe colitis |
| Sri Lanka (n = 1) | No cases yet | Urgent surgeries only (i.e. obstruction or abscess in Crohn’s disease) | Lower doses and short courses when needed |
| Taiwan (n = 1) | Continue immunomodulatory therapy D/C steroids | No change | Avoid steroids; good access to biologicals |
| Thailand (n = 3) | D/C immunomodulatory therapy D/C steroids | Urgent surgeries only (n = 2) Avoid surgery when possible (n = 1) | Use steroids with taper |
| Uruguay (n = 1) | No cases yet | Urgent surgeries only | ? |
| United Kingdom (n = 1) | D/C immunomodulatory therapy | Urgent surgeries only Laparoscopy after COVID testing | Rapid steroid taper |
| United States (n = 2) | D/C thiopurine and anti TNF; Continue Vedolizumab and Ustekinumab (n = 1) D/C immunomodulatory therapy D/C steroids (n = 1) | Urgent surgeries only | Use steroids if necessary after 7 days of infection onset (n = 1) Avoid steroids (n = 1) |
| Vietnam (n = 1) | No cases yet | Urgent surgeries only Pre-op testing for COVID-19 (n = 1) | No change in steroid use; confirm COVID-19 negative |
Abbreviations: n refers to number of respondents from that country. “?” refers to unclear response on that question. D/C, discontinue.
There was consensus to stop or rapidly taper steroids. The slim majority of respondents (30 of 52) would stop or reduce immunomodulatory, therapy but responses varied, including some who reported they had yet to experience such cases and did not present a plan in case that occurred. One American suggested continuing ustekinumab and vedolizumab, a respondent from Mexico would continue vedolizumab and budesonide, and a respondent from Taiwan discontinued steroids but maintained other immunomodulatory drugs. Respondents from Saudi Arabia, Singapore, and India suggested the approach to the immunomodulatory drugs would depend on the severity of the COVID-19 infection and the severity of the IBD. One respondent from Malaysia reported continuing usual maintenance therapy, and 1 respondent from Malaysia reported stopping immunomodulatory therapy. When specified, 5-ASA was consistently continued. A respondent from Kuwait reported switching intravenous biological therapy to subcutaneous. A respondent from Pakistan reported that the fear and stigma of testing positive for SARS-CoV-2 infection inhibited patients in his jurisdiction from accessing medical care. Several respondents stated that they had yet to encounter IBD cases with COVID-19, so they did not state a specific plan of management.
5) What is the role of surgery in the face of COVID-19? Does COVID-19 affect the indications for surgery or the scope of surgical interventions (Table 2)?
Broadly, only urgent surgeries were undertaken. However, in Indonesia, Kenya, Taiwan, and 1 Israeli center (a pediatric center), approaches to surgery did not change, suggesting that elective surgeries in IBD continued. In 1 center each from China, Indian, Pakistan, and Vietnam, surgery was undertaken after a negative COVID-19 test. It was not clear whether emergency surgery would have been undertaken in these centers in a patient with a positive test, especially if asymptomatic.
6) If in a low resource area and there is no access to biologicals, how does one address steroid use in the current environment of COVID-19 concern (Table 2)?
Some respondents declared avoidance of steroids, but the majority declared selective steroid use and a more rapid taper than usual. The use of steroids in ulcerative colitis (UC) was singled out as more likely. Vietnam, Portugal, 1 of the 2 Pakistani sites, 1 of 4 Chinese sites, and both Israeli sites would use steroids. Two of the 3 pediatricians answering would use steroids. One clinician from Bangladesh would use steroids after the patient is proven to be COVID-19 negative. A respondent from Kenya stated that if a patient was using steroids, the patient would be kept in isolation. One respondent each from Hong Kong, Korea, Mexico, Myanmar, and Brazil and 2 from Canada and 1 from China would use more locally acting steroids (eg, budesonide).
7) How should one investigate and manage someone presenting with potential new onset IBD? How is this affected by resource availability (Table 3)?
Colonoscopy was still being performed for diagnosis of IBD in 1 of 2 US centers, 1 of 2 Indian centers, 1 of 2 Israeli centers, 1 of 2 Malaysian centers, 1 of 2 Pakistani centers, and centers in Canada, Indonesia, Kenya, Korea, Portugal, Romania, Singapore, and Taiwan. In one of the Portuguese centers, there was a preference for imaging and noninvasive testing such as fecal calprotectin. In the Philippines, endoscopy was undertaken in more active cases. In 1 center each in China, Hong Kong, Korea, Saudi Arabia, Taiwan, and Vietnam, endoscopy was only undertaken after negative COVID-19 viral testing. Some centers were avoiding endoscopy even in this scenario of new onset disease, including centers in Brazil, South Africa, Thailand, the UK, and 2 of 4 centers from China, 1 of 2 centers from India, and 1 of 2 centers from Malaysia. In cases of likely colitis, responses from 1 of 2 US centers, 1 of 2 Pakistani centers, and the UK reported use of empiric treatment, particularly with 5-ASA. Canadian respondents reported avoiding intravenous biologicals in favor of subcutaneous dosing when biologicals were being initiated to avoid attendance at in-person infusion clinics. Respondents from Taiwan, Uruguay, Vietnam, and a pediatric center in Israel reported no change in their approach to IBD management.
8) Considering that at least 5% of persons with COVID-19 present with isolated GI symptoms when a patient with IBD presents with worsening GI symptoms are you routinely testing for COVID-19 (Table 3)?
Clinicians from 17 countries did not test for COVID-19 on flare of gastrointestinal symptoms. This included both high resource countries like Canada, Korea, and Taiwan and lower resource countries like Vietnam. In Korea and Taiwan, this was a response to the relatively low community prevalence of COVID-19 in their countries. In Canada, though, clinicians did not have open access to testing, so it was limited to persons with respiratory symptoms. Respondents from 8 countries, both low and high resource regions, reported that they routinely tested persons with IBD with new gastrointestinal symptoms. In Brazil, India, Malaysia, Pakistan, Portugal, and the United States, there were those who reported testing and those who did not. Hence, it was not uniform in all countries. Indications for testing have been rapidly changing, so these approaches may have even been different for those who responded at the beginning of the study period compared with the end of the period of survey collection.
9) What is the role of noninvasive markers in assessing disease if endoscopy is not available? For example, ESR, CRP, fecal calprotectin, WBC, platelet count, radiology? How does resource availability affect this (Table 3)?
Blood testing, fecal calprotectin, and imaging were widely performed. However, imaging access was limited in 1 of 4 Brazilian centers, 2 of 3 Canadian centers, both American centers, Puerto Rico, and Thailand. In some Canadian regions, access and funding for fecal calprotectin was limited. In Qatar, patients tended to avoid clinics, and therefore, it was difficult to investigate them. This was also reported in response to question 1 by a South African respondent and in question 6 by an Israeli respondent.
Table 4 shows the number of COVID-19 cases, the number of COVID-19 cases per 1 million people, and the number of COVID-19 tests undertaken as of May 16, 2020.15
TABLE 4.
Number of COVID-19 Cases and COVID-19 Tests Done as of May 16 202016
| Country | Number of COVID-19 cases | COVID-19 Cases/1 million | COVID-19 Tests/1 million |
|---|---|---|---|
| Bangladesh (n = 2) | 23,870 | 145 | 1125 |
| Brazil (n = 4) | 245,595 | 1156 | 3464 |
| Canada (n = 3) | 78,017 | 2069 | 34,816 |
| China (n = 4) | 82,954 | 58 | ? |
| France (n = 1) | 179,927 | 2757 | 21,218 |
| Hong Kong (n = 1) | 1056 | 141 | 22,470 |
| India (n = 2) | 100,340 | 73 | 1671 |
| Indonesia (n = 1) | 18,010 | 66 | 698 |
| Israel (n = 2) | 16,643 | 1927 | 58,540 |
| Kenya (n = 1) | 912 | 17 | 836 |
| Korea (n = 1) | 11,065 | 216 | 14,693 |
| Kuwait (n = 1) | 15,691 | 3681 | 58,253 |
| Malaysia (n = 2) | 6941 | 215 | 13,717 |
| Mexico (n = 1) | 49,219 | 382 | 1338 |
| Myanmar (n = 1) | 188 | 3 | 268 |
| Nepal (n = 1) | 375 | 13 | 3450 |
| New Zealand (n = 1) | 1499 | 311 | 47,892 |
| Pakistan (n = 2) | 42,125 | 191 | 1754 |
| Philippines (n = 1) | 12,718 | 116 | 2238 |
| Portugal (n = 2) | 29,209 | 2864 | 63,969 |
| Puerto Rico (n = 1) | ? | ? | ? |
| Qatar (n = 1) | 33,969 | 11,816 | 56,243 |
| Romania (n = 1) | 17,036 | 885 | 16,290 |
| Saudi Arabia (n = 1) | 57,345 | 1650 | 17,324 |
| Singapore (n = 1) | 28,343 | 4849 | 42,132 |
| South Africa (n = 1) | 16,433 | 278 | 8023 |
| Sri Lanka (n = 1) | 992 | 46 | 2074 |
| Taiwan (n = 1) | 440 | 18 | 2914 |
| Thailand (n = 1) | 3031 | 43 | 4099 |
| UK (n = 1) | 246,406 | 3632 | 39,543 |
| United States (n = 2) | 1,544,557 | 4670 | 36,646 |
| Uruguay (n = 1) | 734 | 211 | 9752 |
| Vietnam (n = 1) | 324 | 3 | 2828 |
DISCUSSION
The management of persons with IBD across the world in the setting of the COVID-19 pandemic shares many similarities. Gastroenterologists were heeding the recommendations of established gastroenterology bodies with adaptations based on local resources. Of note, gastroenterologists from some high resource countries, such as Canada, and from lower resource countries both reported impediments in access to PPE. Some clinicians reported unique issues limiting patient access to clinics or completing diagnostic testing, such as traffic restrictions in China or patient fear of attending clinics in Israel, Qatar, and South Africa. Some gastroenterologists reported no change in their approaches to IBD patients including no reduction in endoscopy services. This was mostly reported in countries with low COVID-19 patient burdens and was true of both higher and lower resource countries. Most countries had reduced outpatient clinics, reduced outpatient endoscopy and reduced surgery. Several countries retained outpatient endoscopy for persons with IBD as part of management decision-making. Nearly all who responded as to which endoscopies would be allowed reported undertaking endoscopy for urgent IBD scenarios such as active bleeding, severe colitis to assess for infection, certain bowel obstructions, and cancers. Many centers were undertaking endoscopy for new onset IBD to assist with diagnosis. There was near uniform agreement on reducing or avoiding steroid use. Most clinicians reduced or stopped oral immunomodulatory therapy or steroids. However, multiple clinicians from Romania, Singapore, Taiwan, and Uruguay and 1 from Malaysia did not change their management approaches. In the Surveillance Epidemiology of Coronavirus Under Research Exclusion (SECURE)-IBD database, steroid use was associated with worse outcomes in IBD patients who were affected by COVID-19.16 Others reported not having dealt with a case of COVID-19 in an IBD patient and hence did not respond as to how they would manage that dilemma.
The use COVID-19 testing as part of management approach for persons with IBD was variable. In Taiwan and 1 American center, COVID-19 testing was undertaken before further IBD-related diagnostics; a respondent from Vietnam would test for COVID-19 if changing drug treatment; in Bangladesh, they would only reduce steroids if the patient was COVID-19 positive; and in 1 center each from China, Pakistan, and Vietnam, they would undertake COVID-19 testing before surgery. Of note, when IBD patients had new or increased gastrointestinal symptoms, a minority reported testing for COVID-19. The survey was not structured to determine if this was because the jurisdictions within which they practiced had limited access to COVID-19 testing or if the clinicians simply thought this was unnecessary. All centers had access to standard blood testing, most had access to fecal calprotectin (including some centers accessing a home version, which facilitated patient isolation practices), and most had usual access to imaging. Some centers (2 in Canada, 1 in the United States, 1 in Bangladesh, and 1 in Thailand) had limited access to cross-sectional imaging. In the case of Canada and the United States, this was deliberate on the part of the health system to reduce patient contact with hospital staff for nonurgent testing.
Table 4 shows the distribution of cases of COVID-19 and of tests for COVID-19 per 1 million inhabitants. One can see that there were several countries with fewer than 400 per 1 million cases; however, there was a marked discrepancy in testing frequency. Testing ranged from 268 out of 1 million inhabitants (Myanmar) to 47,892 out of 1 million inhabitants (New Zealand). Undoubtedly, the experience of respondents was impacted by the burden of disease in their communities. Several had yet to experience cases of IBD in which patients were infected with COVID-19. It will be important to repeat this survey again to determine if views changed as the disease burden changes.
This study had some notable limitations. Clinicians within every country may have different practice approaches so that a survey response from 1 or 2 clinicians does not necessarily reflect what may be done by most clinicians in that country. It is unknown to what extent the responses reflect the majority of gastroenterologists managing IBD patients in each jurisdiction, especially because the respondents were leaders in IBD management in their respective countries. However, even with reports from 1 or 2 clinicians from each country, it allows insight into the uniformity or key differences in the practice of IBD around the world during the COVID-19 pandemic. Though some respondents reported limitations to PPE access or COVID-19 testing, not reporting such limitations does not mean that they did not exist in those jurisdictions. in several countries, there are dual private and publicly funded health care systems. Respondents were not asked to distinguish their answers for each of the 2 systems, although some respondents did report those differences.
In summary, regardless of resources and health care system, gastroenterologists around the world were generally taking a similar approach to the management of IBD. For the most part, they were adhering to published guidelines on IBD management in the COVID-19 era. There were some notable differences in care approach due to reduced service availability, resource availability, and community prevalence of COVID-19. Countries that had 2 or more respondents showed how responses could vary within a country, and so these results should not be taken to reflect a consensus of an entire country’s approach to managing IBD.
Author Contribution: All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, and (3) final approval of the version to be submitted.
Conflicts of Interest: CB is supported in part by the Bingham Chair in Gastroenterology. He has been on the advisory boards of Abbvie Canada, Janssen Canada, Pfizer Canada, Takeda Canada, and Roche Canada and consulted for Takeda and Mylan Pharmaceuticals. He has been on the speaker’s bureau for Abbvie Canada, Janssen Canada, Takeda Canada, and Medtronic Canada. He has received unrestricted educational grants from Abbvie Canada, Janssen Canada, Pfizer Canada, and Takeda Canada and has done contract research with Abbvie, Janssen, Pfizer, Celgene, Boeringher Ingelheim, and Roche. SN has recived speaker’s fees from Abbvie, Ferring, Janssen, Pfizer, Menarini, Takeda, and Tillots and research grants from Abbvie and Ferring. RB has received speaker’s fee from Ferring, Janssen, Menarini, Cipla, Takeda, and Microlabs and has been an advisory committee/board member for Janssen, Ferring, and Cipla. FS is an advisory board member or speaker for Abbvie, Eurofarma, Ferring, Janssen, Pfizer, and Takeda. BS has been a consultant and on the speaker’s bureaus of Abbvie, Janssen, and Takeda. FC received honoraria from Amgen, BMS, Celltrion, Enterome, Ferring, Janssen, Medtronic, Pfizer, Pharmacosmos, and Roche, in addition to lecture fees from Abbvie, Astra, BMS, Ferring, Janssen, MSD, Pfizer, Pileje, Takeda, and Tillotts. JKYF is an advisory committee/board member for Takeda Pharmaceuticals Company Ltd; has received honoraria from AbbVie, Takeda, Janssen, Farmasa, Ferring, Alfasigma, Hospira, UCB, Celltrion, Danone, Almirall, and Pfizer as a speaker, key opinion leader, and member of national and international advisory boards; has received research funds from Bristol, Shire, Pfizer, and Takeda. AG has received investigator-initiated research support from Abbvie, speaker fees from Abbvie, Janssen, Nestle, and Shire, and has consulted for Abbvie, Amgen, Bristol Myers Squibb, Janssen, Lilly, Merck, and Roche. EB was supported by a New Investigator Award from the Canadian Institutes of Health Research, Crohn’s and Colitis Canada, and the Canadian Association of Gastroenterology. He was also supported by the Career Enhancement Program of the Canadian Child Health Clinician Scientist Program. ST has received research support from AbbVie, Buhlmann, Celgene, International Organization for the Study of Inflammatory Bowel Disease, Janssen, Lilly, Pfizer, Takeda, UCB, Vifor, and Norman Collisson Foundation; consulting fees from AbbVie, Allergan, Amgen, Arena, Asahi, Astellas, Biocare, Biogen, Boehringer Ingelheim, Bristol-Myers Squibb, Buhlmann, Celgene, Chemocentryx, Cosmo, Enterome, Ferring, Giuliani SpA, GSK, Genentech, Gilead, Immunocore, Immunometabolism, Indigo, Janssen, Lexicon, Lilly, Merck, MSD, Neovacs, Novartis, NovoNordisk, NPS Pharmaceuticals, Pfizer, Proximagen, Receptos, Roche, Sandoz, Sensyne, Shire, Sigmoid Pharma, SynDermix, Takeda, Theravance, Tillotts, Topivert, UCB, VHsquared, Vifor, Zeria; speaker fees from AbbVie, Amgen, Biogen, Ferring, Janssen, Pfizer, Shire, Takeda; and declares no stock or share options. DR has received research funding from Takeda and has served as a consultant to Abbvie, Abgenomics, Allergan, Inc., Arena Pharmaceuticals, Biomica, Bristol-Myers Squibb, Dizal Pharmaceuticals, Ferring Pharmaceuticals, Inc., Genentech/Roche, Janssen Pharmaceuticals, Lilly, Mahana Therapeutics, Medtronic, Merck & Co., Inc, Napo Pharmaceuticals, Pfizer, Prometheus Laboratories, Shire, Takeda, and Target PharmaSolutions, Inc. GK has received honoraria for speaking or consultancy from Abbvie, Janssen, Pfizer, and Takeda. He has received research support from Ferring, Janssen, Abbvie, GlaxoSmith Kline, Merck, and Shire. He has been a consultant for Gilead. He shares ownership of a patent: Treatment of inflammatory disorders, autoimmune disease, and PBC. UTI Limited Partnership, assignee. Patent WO2019046959A1. PCT/CA2018/051098. 7 Sept. 2018. DA has participated in advisory boards for Pendopharm, Shire and Takeda and has received funding from Medtronic for investigator-initiated research. RG is an advisory board member for AbbVie, Zespri; has received honoraria from AbbVie, Takeda, Janssen, Zespri; and has received research funds from AbbVie and Zespri.
Contributor Information
IBD-Emerging Nations Consortium and the WGO IBD Task Force on COVID-19:
Dr. M Masudur Rahman, Dr. Mostafa N Mohsin, Dr. Andrea Vieira, Dr. Nayara Carvalho Salgado, Dr. Marta Brenner Machado, Dr. Hao Wu, Dr. Joyce W Y Mak, Dr. Ying-Lei Miao, Dr. Murdani Abdullah, Dr. Yehuda Chowers, Dr. Elly Ogutu, Dr. Smita Devani, Dr. Suk-Kyun Yang, Dr. Mahmoud Omar, Dr. K L Goh, Dr. Ida Hilmi, Dr. Raja Affendi Raja Ali, Dr. Than Than Aye, Dr. Tin Moe Wai, Dr. Neeraj Joshi, Dr. Zaigham Abbas, Dr. Fernando Magro, Dr. Jose Sollano, Dr. Esther A Torres, Dr. Syed Adnan Mohiuddin, Dr. Mircea Diculescu, Dr. Majid Almadi, Dr. David Ong, Dr. Gillian Watermeyer, Dr. Navarathne Metthananda, Dr. Shuchen Wei, Dr. Julajak Limsrivilai, Dr. Nonthalee Pausawasdi, Dr. Pises Pisepongsa, Dr. Gursimran Kochhar, Dr. Ximena Rodríguez, and Dr. Dao Viet
REFERENCES
- 1. Molodecky N, Soon IS, Rabi D, et al. Increasing incidence of inflammatory bowel disease with time and among regions, based on systematic review. Gastroenterol. 2012;142:46–54. [DOI] [PubMed] [Google Scholar]
- 2. Ng SC, Shi HY, Hamidi N, et al. The worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769–2778. [DOI] [PubMed] [Google Scholar]
- 3. Kotze PG, Underwood FE, Damião AOMC, et al. Progression of inflammatory bowel diseases throughout Latin America and the Caribbean: a systematic review. Clin Gastroenterol Hepatol. 2020;18:304–312. [DOI] [PubMed] [Google Scholar]
- 4. Ananthakrishnan AN, Kaplan GG, Ng SC. Changing global epidemiology of inflammatory bowel diseases: sustaining health care delivery into the 21st century. Clin Gastroenterol Hepatol. 2020;18:1252–1260. [DOI] [PubMed] [Google Scholar]
- 5. IOIBD Update on COVID19 for Patients with Crohn’s Disease and Ulcerative Colitis | IOIBD. Accessed May 16, 2020. https://www.ioibd.org/ioibd-update-on-covid19-for-patients-with-crohns-disease-and-ulcerative-colitis/.
- 6. Rubin DT, Feuerstein JD, Wang AY, et al. AGA clinical practice update on management of inflammatory bowel disease during the COVID-19 pandemic: Expert Commentary. Gastroenterology. 2020; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. BSG Expanded Consensus Advice for the Management of IBD During the COVID-19 Pandemic. Accessed May 16, 2020. https://www.bsg.org.uk/covid-19-advice/bsg-advice-for-management-of-inflammatory-bowel-diseases-during-the-covid-19-pandemic.
- 8. D’Amico F, Danese S, Peyrin-Biroulet L; on behalf of the ECCO COVID taskforce. Inflammatory bowel disease management during the COVID-19 outbreak: a survey from the European Crohn’s and Colitis Organization (ECCO). Gastroenterology. 2020; in press. [Google Scholar]
- 9. Sultan S, Altayar O, Siddique SM, et al. AGA institute rapid review of the GI and liver manifestations of COVID-19, meta analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology. 2020; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Luo S, Zhang X, Xu Het al. Don’t overlook digestive symptoms in patients with 2019 Novel Coronavirus Disease (COVID-19). Clin Gastroenterol Hepatol. 2020;18:1636–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cholankeril G, Podboy A, Aivaliotis VI, et al. High prevalence of concurrent gastrointestinal manifestations in patients with SARS-CoV-2: early experience from California. Gastroenterology. 2020;S0016-5085(20)30471-6. doi: 10.1053/j.gastro.2020.04.008.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hajifathalian K, Krisko T, Mehta A, et al. Gastrointestinal and hepatic manifestations of 2019 novel Coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterology. 2020;S0016-5085(20)30602-8. doi: 10.1053/j.gastro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bernstein CN. Management of Patients with Inflammatory Bowel Disease. Accessed May 16, 2020. https://www.worldgastroenterology.org/UserFiles/file/COVID19/ManagementofPatientswithInflammatoryBowelDiseaseIBD_Intro.pdf.
- 14.Worldometer COVID-19 Coronavirus Pandemic. Accessed May 16, 2020. datahelpdesk.worldbank.org/knowledgebase/articles/906519#High_income.
- 15.World Bank Country and Lending Groups. Accessed May 16, 2020. www.worldometers.info/coronavirus/.
- 16. Brenner EJ, Ungaro RC, Gearry RB, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology. 2020. S0016-5085(20)30655-7. doi: 10.1053/j.gastro.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]