Abstract
The 2019 novel coronavirus disease (COVID-19) pandemic has dramatically impacted numerous health and economic fronts. Because of the stay-at-home mandate and practice of physical distancing, nearly all preventive care measures have been halted, including colorectal cancer (CRC) screening. The health consequences of this temporary suspension are of great concern, particularly for underserved populations, who experience substantial CRC-related disparities. In this commentary, we describe challenges and opportunities to deliver COVID-19–adapted CRC screening to medically underserved populations receiving care in community health centers (CHC). This perspective is based on key informant interviews with CHC medical directors, teleconference discussions, and strategic planning assessments. To address the unprecedented challenges created by the COVID-19 pandemic, we identify 2 broad calls to action: invest in CHCs now and support equitable and adaptable telehealth solutions now and in the future. We also recommend 4 CRC-specific calls to action: establish COVID-19–adapted best practices to implement mailed fecal immunochemical test programs, implement grassroots advocacy to identify community gastroenterologists who commit to performing colonoscopies for CHC patients, assess cancer prevention priorities among individuals in underserved communities, and assess regional CRC screening and follow-up barriers and solutions. The COVID-19 pandemic may further exacerbate existing CRC screening disparities in underserved individuals. This will likely lead to delayed diagnosis, a shift to later-stage disease, and increased CRC deaths. To prevent this from happening, we call for timely action and a commitment to address the current extraordinary CRC screening challenges for vulnerable populations.
The 2019 novel coronavirus disease (COVID-19) was declared a public health emergency of international concern on January 30, 2020, by the World Health Organization. This unprecedented public health challenge has impacted numerous health and economic fronts. Among these is the delivery of preventive care, including lifesaving cancer screening and related follow-up, due in part to the stay-at-home mandates and practice of physical distancing. Although preventive care activities are beginning to slowly resume, it is unclear what the near- or longer-term consequences will be. Importantly, as we learn about the pronounced inequities and disparities in COVID-19 morbidity and mortality, largely due to comorbid conditions and socioeconomic and environmental factors (1,2), it is important to recognize that disparities in cancer screening, incidence, and mortality also exist among the same vulnerable populations.
Colorectal cancer (CRC) is the second leading cause of cancer death in the United States (3). Compared with privately insured patients, uninsured and Medicaid-insured individuals are more likely to present with advanced stage disease and experience higher mortality (4‐6). Screening and appropriate follow-up can reduce incidence and mortality from CRC (7). However, CRC screening rates are particularly low in Hispanics, Asians, recent immigrants, those with low incomes, and the uninsured (8‐10).
The COVID-19 pandemic has caused delays in CRC screening, including among medically underserved populations, such as those receiving care at community health centers (CHCs). This will likely lead to delayed diagnosis, a shift to later-stage disease, and as a result, an increase in CRC deaths, further exacerbating existing health disparities. Recent literature based on modeling estimates predicts approximately 4500 excess CRC deaths between 2020 and 2030 (11, 12). CHCs are at the vanguard of addressing healthcare disparities. CRC screening is a required, reportable quality metric for federally qualified health centers in the uniform data system. Although progress in improving CRC screening has been steady, the screening rate averaged 45.6% in 2019 across all CHCs in the United States (13), much lower than the national average of 67% (14), and substantially lower than the 2018 National Colorectal Cancer Roundtable target of 80% (15) or the Healthy People 2020’s goal of 70.5% (16). Furthermore, guideline-appropriate follow-up of abnormal screening tests is a challenge for CHCs, ranging from 18% to 57% (17, 18).
In this commentary, we describe current challenges for delivering CRC screening to medically underserved individuals receiving care in CHC systems, where a large segment of poor and uninsured individuals in the United States receive primary and preventive care (19). The COVID-19 pandemic requires novel solutions to address these challenges. Using the perspectives from leaders at 4 large CHC systems and 1 serving American Indian communities in our region, as well as our experience with CRC screening interventions and strategic planning meetings, we detail potential solutions and opportunities that are adaptive to the COVID-19 pandemic. We also present a commitment in the form of a call to action to systematically document and address the near- and long-term consequences of the COVID-19 pandemic on CRC screening in CHCs and the communities they serve.
Methods and Findings
Background and Context
This commentary was generated in the setting of 2 ongoing CRC screening multilevel implementation science studies: the San Diego Accelerating Colorectal Cancer Screening and Follow-up through Implementation Science (ACCSIS) study, funded by the National Cancer Institute’s Cancer Moonshot Initiative, and the Federally Qualified Health Centers Assessing Colorectal Cancer Screening (FACtS) study funded by the American Cancer Society. Our team is part of the ACCSIS consortium, focused on understanding intervention strategies for evidence-based CRC screening, such as mailed fecal immunochemical test (FIT) outreach. The consortium includes CHC partners across the United States. Drs Nodora, Gupta, Motadel, Rodriguez, and Schultz are also part of the FACtS study, which seeks to address CRC screening inequity by identifying which CRC screening strategies and related evidence-based interventions are feasible for and likely to be sustained within a CHC setting.
Although COVID-19 interrupted usual ACCSIS and FACtS research activities, it afforded a unique opportunity to investigate challenges and potential solutions for conducting COVID-19–adapted CRC screening. Largely because of our partnership with Health Center Partners of Southern California, a consortium of 16 health-center organizations and its subsidiary Health Quality Partners of Southern California, which develops collaborative, innovative programming to improve the quality of services offered by health centers, our group was able to collect data on the early impact of the pandemic on CRC screening. Data from interviews, along with team discussions and strategic planning assessments, were used to identify COVID-19–related barriers and opportunities, with a goal of developing a preliminary plan to move forward. This process helped us develop guidance and recommendations to address emerging challenges for the delivery of CRC screening within our partner health centers.
Key Informant Interviews With San Diego CHC Chief Medical Officers
We developed interview questions to assess health system and patient-level impacts of the COVID-19 pandemic. We conducted individual interviews with all chief medical officers (CMO) and/or medical directors in our 4 ACCSIS study sites located in Southern California. We interviewed one additional CMO who provided a perspective for the Southern Indian Health Council, a CHC serving 7 tribal communities in San Diego County (Ewiiaapaayp Band of Kumeyaay Indians, Jamul Indian Village of California, Manzanita Band of the Kumeyaay Nation, Barona Band of Mission Indians, Campo Band of Mission Indians, La Posta Band of Mission Indians, and Viejas Band of Kumeyaay Indians). These 4 large CHC systems represent 25% of the 16 Health Quality Partners consortium. We conducted interviews via telephone approximately 5-7 weeks after California initiated its stay-at-home mandate. Interviews were transcribed and analyzed using an uncoded rapid analysis approach by 2 investigators, followed by scientific team review (20). Table 1 summarizes the interview findings for health system and patient-level impacts, which are described below.
Table 1.
Impact of COVID-19 on CHC health system and patients based on interviews with chief medical officers and directorsa
| Levels of impact and recommendations | Examples of impact and recommendations |
|---|---|
| CHC health system impact | |
| Economic | CHCs face revenue loss because of clinic closures within the CHC systems, especially dental facilities; patient visits have decreased 50%-70%: no elective or preventive services, few pediatric visits (well-child visits postponed, immunizations for children younger than aged 2 years available), most labs deferred; most chronic disease management visits are deferred; telehealth (largely by phone) represents 80%-85% of consultations. |
| Staffing |
Staff reductions include furloughs, layoffs, and reduction in hours. Telehealth services have changed staff routines. Most CHC systems were able to quickly establish effective telehealth services, covered under emergency plan funds. Physical distancing measures impact clinical staff functions. Staff anxiety and fear related to contamination have been addressed through education (morning clinical team question-and-answer sessions) and clear procedures for use of PPE. |
| CRC screening practice (workflow) |
Lab staff is available to process FITs at most CHCs (although CHCs are not ordering FIT tests routinely). Colonoscopies currently performed only for symptomatic and emergency patients. Community gastroenterologists inquiring about restarting CHC referrals. |
| CRC screening funding | Preventive services (including CRC screening) are considered elective procedures and not performed. |
| Markers of readiness for reinitiating in-person CRC screening | Most CMOs shared their support for reinitiating in-person CRC screening, providing the following practices were in place: adequate PPE supply; sufficient COVID-19 testing capacity (viral and antibody testing); lifting of stay-at-home orders; permission to do elective procedures; sufficient staff to handle previsit screening and assessments. |
| Patient-level impact | |
| Anticipated patient hesitancy for preventive services and clinic visits |
Patients will prioritize immediate concerns over disease prevention. Patients will be hesitant to leave home. |
| Recommended additions and modifications to patient CRC screening materials and process |
Recommended modifications for CRC screening because of COVID-19 include the following: use newly created COVID-19 information where applicable and review and update existing CRC screening guidelines accounting for COVID-19 impacts. Telehealth is a huge silver lining; patients are grateful they don’t have to travel to clinic and wait around in the clinic. Telehealth funding postpandemic is a concern (but telehealth benefits during the pandemic are evidence of success). |
CHC = community health center; CMO = chief medical officer; COVID-19 = 2019 novel coronavirus disease; CRC = colorectal cancer; FIT = fecal immunochemical test; PPE = personal protective equipment.
CHC Health System Impacts
As a result of the COVID-19 pandemic, CHCs are facing considerable revenue loss because of closure of clinics. This led to a large reduction of in-person patient visits, with chronic disease management being the focus for patients visiting CHC facilities. During the early response to the pandemic, CHCs did not offer elective or preventive services. The pandemic has also resulted in staff reductions, which have occurred via furloughs, layoffs, and reduction in hours; changes in workflows; and temporary closure of some sites. Staff who remain employed onsite face anxiety and fear related to infection.
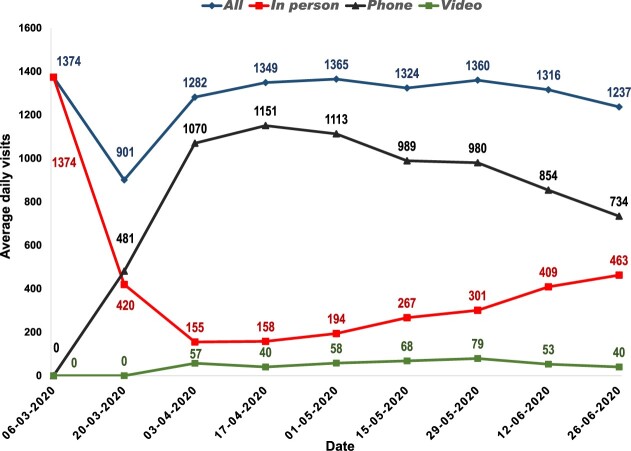
Clinical consults have largely transitioned to telehealth (80%-85%), and most of these occur by telephone. Figure 1 illustrates this transition for 1 of the participating health centers that collected detailed data. As shown, a dramatic drop for in-person visits occurred in the middle of March 2020, with a corresponding rapid rise in telehealth visits. Of note, the vast majority of telehealth visits were telephone based; video calls were minimal. Overall, most CHC systems were able to quickly establish effective telehealth services (covered under emergency plan funds). Generally, patients who can be reached and scheduled for a telehealth consultation appointment are adherent, largely eliminating missed appointments. Notably, most CMOs were not optimistic that funding for telehealth will continue after the pandemic ends; however, their hope is that current success will show the benefits of telehealth in CHCs.
Figure 1.
Average daily visits by visit type at 1 community health center following COVID-19 pandemic stay-at-home mandate in California.
CRC Screening Impacts
Prior to the pandemic, all CHC clinics were using FIT for CRC screening. Among the 4 ACCSIS CHCs, all except 1 required that FIT kits be picked up during a clinic visit. Return of FIT kits was done primarily by in-person drop-off at the clinic or a contract lab site. By the third week of March, respondents noted that laboratory staff continued to be employed at most CHCs, meaning that FIT kits could be processed. However, most CHCs were not ordering FITs routinely. For colonoscopy capacity, it appears that the few colonoscopies that were taking place were for symptomatic patients or in emergency situations, although referral gastroenterologists are beginning to consider more referrals for colonoscopies and other procedures. In our San Diego region, wide variation exists with respect to availability of screening and follow-up colonoscopy services. At least 1 large gastroenterology group offers full range of colonoscopies, including for screening and diagnostic test follow-up, whereas others are limiting these to urgent and semiurgent cases. Novel preprocedure strategies (eg, preprocedure testing to rule out COVID-19 infection and prioritization of urgent vs less urgent procedures), intraprocedure strategies (careful consideration of appropriate usage of personal protective equipment), and postprocedure follow-up (to check for absence of infection), both locally developed and with input from national gastroenterology societies, are challenging efficient delivery of gastrointestinal procedures, including colonoscopy (21).
Our team was particularly interested in querying health-center medical directors about readiness to resume routine CRC screening. Most CMOs shared their support for reinitiating CRC screening. Respondents noted the following best indicators for initiating in-person visits, including CRC and other cancer screening: sufficient personal protective equipment, adequate COVID-19 testing capacity (for active and prior infection), lifting of stay-at-home order, permission to do elective procedures, and sufficient staff to handle previsit screening and assessments. One respondent indicated that its personal protective equipment supply would last approximately 7 weeks at the current 10% health-center capacity, further noting that this equipment was mainly from its own stockpile, donations, and some new orders.
Patient-Level Impacts
When asked about patient readiness for reinitiating preventive services, CHC chief medical officers and directors noted that many patients will prioritize immediate concerns (eg, employment and housing) over disease prevention, with uncertainty regarding how long this will persist. They also stated that many patients will be hesitant to leave home. To overcome this, CMOs highlighted the importance of emphasizing to patients that the FIT can be done at home, reiterating that telehealth is a huge silver lining. In addition, they recommended that we modify the mailed FIT materials as follows: provide up-to-date COVID-19 information, where applicable, and review and update existing CRC screening guidelines accounting for COVID-19 impacts.
Although findings from these brief interviews are extremely valuable, in-depth patient, provider, and additional system-level data are urgently needed to fully understand the impact of the pandemic on CRC screening in the CHCs. At present, it is not possible to collect these data because of staff shortages and shifting of health-care personnel to address the COVID-19 crisis.
COVID-19 Adaptations Based on Lessons Learned
Based on our experience with CRC screening interventions, our recent COVID-19 data collection, and key informant interviews with CHC leaders, we have developed guidance on delivering CRC screening in CHCs that considers the multifaceted and multilevel challenges created by the pandemic. In Table 2, we summarize the key lessons learned by our team, as well as COVID-19–adapted solutions to overcome challenges related to CRC screening. Below, we summarize key COVID-19–adapted strategies to promote CRC screening informed by the lessons learned.
Table 2.
Lessons learned and COVID-19 adaptations for delivering colorectal cancer screening in community health centersa
| Strategies and interventions | Lessons learned | COVID-19 adaptations |
|---|---|---|
| Mailed FIT screening |
CHCs can deliver mailed FIT without requiring a patient visit. Centralization of delivery is possible. CHCs confirmed interest in mailed FIT as key strategy for CRC screening. |
Assess and accommodate real-world experience of mailed FIT. Review current CRC screening strategies and evidence-based interventions to consider needed modifications. |
| Patient navigation for abnormal FIT follow-up |
Uniform delivery is possible by telehealth. Challenges remain regarding staff changes and turnover because of layoffs. |
Shift patient navigation to virtual delivery. Adopt the train-the-trainer model to accommodate anticipated staff turnover. |
| Colonoscopy completion for patients with abnormal FIT |
Colonoscopy capacity can remain a challenge for CHCs that are not part of an integrated system with specialty care. Access to colonoscopy and willingness to complete exam may remain particularly low and decrease further. Increasing Medicare and Medicaid reimbursement for colonoscopy and supporting enhanced telehealth-based care coordination may help optimize follow-up. |
Conduct survey of community gastroenterologists to assess capacity for CHC patients. Monitor follow-up rates and funding policies to increase access and participation. Encourage grassroots advocacy to form a list of community gastroenterologists who commit to performing colonoscopies for CHC patients. Consider strategies to prioritize patients with abnormal FIT waiting for colonoscopy who develop signs and symptoms such as iron deficiency anemia, weight loss, and frank hematochezia. |
| Telehealth capability and capacity |
CHCs report high participation in telehealth appointments with few missed appointments. Visits are largely phone-based vs video. Patients are afraid or hesitant to come to the clinic. Phone visits more likely to be successful if caller identification is known. |
Enhance telemedicine capability and capacity. Ensure caller identification capability. Conduct needs assessment of patients and providers to assess barriers for telehealth, especially video calls. Support change in policies for telehealth reimbursement. |
CHC = community health center; COVID-19 = 2019 novel coronavirus disease; CRC = colorectal cancer; FIT = fecal immunochemical test.
Identify COVID-19 Adapted Strategies for Implementing Mailed FIT
Mailed FIT is a well-established, evidence-based strategy for promoting CRC screening participation, well suited for addressing the challenges posed by the pandemic (22). Given that mailed FIT is feasible during the pandemic and is endorsed by CHC directors, adaptations will need to involve a continuous assessment to accommodate real-world experiences. Centralization of delivery for multiple CHCs is also possible where a coordinating organization exists, such as the case for our region through Health Quality Partners of Southern California. This would be similar but in smaller scale to what is done through organized population-level screening programs in countries outside the United States. Some aspects related to implementation of a mailed FIT program, such as patient navigation for abnormal FIT, would need to shift to virtual delivery.
Monitor Colonoscopy Access and Consider Policies That Can Boost Access and Colonoscopy Participation for Vulnerable Populations
Diagnostic colonoscopy follow-up for an abnormal FIT is a challenge for CHCs in a nonintegrated health center system (17, 18). The general lack of gastroenterology services during the pandemic exacerbate this challenge. Access to colonoscopy and willingness to participate in colonoscopy for abnormal FIT may remain particularly low for vulnerable populations, and even decrease further. Monitoring follow-up rates and funding policies to increase access and participation will be needed. Policies such as increasing Medicare and Medicaid reimbursement for colonoscopy and supporting enhanced telehealth-based care coordination may help optimize follow-up. Additionally, CHCs may need to monitor patients with abnormal FIT waiting for colonoscopy to prioritize those who develop signs and symptoms of CRC such as iron deficiency anemia, weight loss, and frank hematochezia.
Determine How CRC Screening Telehealth Works Best for Providers and Patients
Telehealth could provide a silver lining. CHCs report high participation in telehealth visits, although these tend to be telephone based. Although our regional health centers all have capability for telehealth, patient-related limitations for video use were evident. Delivery of mailed FIT, communication of results, and follow-up for abnormal tests could be done virtually. Understanding and addressing patient and provider challenges to telehealth will be key for successful adaptation. For CRC screening, caller identification capability will enhance mailed FIT follow-up calls, including return of results. Follow-up for mailed FIT return reminders and for abnormal screening results could take place via telehealth.
Unique opportunities to provide CRC screening exist in the participating CHCs, including confirmation by CHCs that mailed FIT is feasible given the lack of patient contact required, as was recently reported (23). Prior to the onset of the pandemic, our group was gathering feasibility and pilot data to assess a centralized mailed FIT operation coordinated by a consortium organization. This centralization has the potential to eliminate the clinical staff implementation burden of setting up and sustaining individual mailed outreach programs. During public health crises, like the COVID-19 pandemic, centralization may be even more desirable because this will allow clinic personnel to concentrate their efforts on urgent clinical needs while centralized screening continues.
Moving Forward
The COVID-19 pandemic has allowed us to pause and “look behind the curtain” to learn about the fragile state of our health-care system and the existing cancer prevention disparities among poor and underserved communities. For CRC, some facts were already evident: low CRC screening and follow-up rates, late stage at diagnosis, and high mortality among medically underserved populations. We also knew that these communities and the CHC-based primary care providers that serve them face many challenges. The pandemic has permitted us to examine the potentially bleak future of exacerbated disparities. Investment to address low CRC screening rates in underserved populations had been underway, including the National Cancer Institute’s Cancer Moonshot Initiative, funded by the 21st Century Cures Act passed by US Congress in December 2016. A mandate of the Cancer Moonshot is to accelerate cancer research and produce more clinically relevant results. How does the information from our “peek” into overburdened health-care systems compounded by existing historical health disparities influence the potential for accelerated cancer research? We must ensure that continued acceleration of this national investment is not halted.
To move forward and address the unprecedented challenges created by the COVID-19 pandemic, we propose 2 broad calls to action: invest in CHCs now and support equitable and adaptable telehealth solutions now and in the future. We also recommend 4 CRC-specific calls to action: establish COVID-19–adapted best practices that address mailed FIT programs in CHCs, implement grassroots advocacy to identify community gastroenterologists who commit to performing colonoscopies for CHC patients, assess cancer prevention priorities among individuals in underserved communities, and assess regional CRC screening and follow-up barriers and solutions. As has been proposed (2), calls to action, such as these, need to take the form of a commitment. This commitment should come from key stakeholders, including patients, health-care providers (CHCs and affiliated specialists), academic institutions, relevant government agencies (local and national), industry, and philanthropy. Importantly, some of these actions have the potential to benefit populations receiving care outside of CHCs. Details of the calls to action are presented below.
Broad Call to Action
Invest in CHCs Now
CHCs are community-based and patient-directed organizations that deliver comprehensive, culturally competent, high-quality primary health-care services. According to the Health Resources and Services Administration, CHCs deliver services in areas where economic, geographic, or cultural barriers limit access to affordable health care. As such, these health centers provide care to our country’s most vulnerable individuals and families, including people experiencing homelessness, agricultural workers, residents of public housing, and approximately 385 000 US veterans. More than 29 million individuals, 1 in 12 nationwide, rely on these Health Resources and Services Administration–funded centers for affordable, accessible primary care, including CRC screening. Given the economic consequences that we face as a nation, including joblessness and an increase in the number of uninsured, the number of individuals seeking primary care in CHCs will rise, further increasing the burden on these health centers. The economic impact of the COVID-19 crisis on CHCs has been dramatic, directly affecting the 345 CHCs, which represent 1370 sites and 7.2 million patients across the United States. In California alone, CHCs are projected to lose approximately $251 million in revenue by the end of 2020, and 17% of staff was furloughed or laid off because of the pandemic (24).
Support Equitable and Adaptable Telehealth Solutions Now and in the Future
The use of telehealth and related technologies for health-care delivery during disasters is not a new concept (25). In fact, the growing frequency of these disasters should be a warning for us to fully develop this technology, along with high-quality internet services that are readily accessible to all. Despite the variety of telehealth modalities (phone, video teleconferencing, remote monitoring, mobile applications, text, and email) and the many benefits, CHCs have not fully adopted telehealth, primarily because of cost, reimbursement, and technical issues (26). Continued assessment of multilevel barriers for telehealth, including patient-related factors, is essential. Recognizing a digital divide characterized by race and ethnicity, age, and sociodemographic status (27), future success will require that all CHC patients can access telehealth services adequately, especially for video consults. Payment and regulatory structures, state licensing, credentialing, and implementation of these programs in an equitable fashion need to take place to move forward. We cannot afford to continue to leave underserved populations behind as we search for solutions. As technologies are considered and developed, we must actively involve CHC leaders and advocates for the most vulnerable communities in these efforts.
CRC-Specific Call to Action
Establish COVID-19–Adapted Best Practices for Implementing Mailed FIT Programs in CHCs
FIT is the primary CRC screening modality for many CHCs. Health centers can deliver invitations to complete FIT by mail without requiring a patient visit, making it adaptable to the current public health crisis. Laboratory staff are working at most CHCs, meaning that FIT kits can be processed. Organizations setting clinical practice recommendations, such as the National Colorectal Cancer Roundtable (15) and the Community Preventive Services Task Force (28), should assess existing FIT screening strategies and related evidence-based interventions to ensure they address COVID-19 impacts. Furthermore, revising the steps guide to reflect implementation strategies relevant to the new COVID-19 context could support the timely and efficient uptake of these new recommendations.
Implement Grassroots Advocacy to Identify Community Gastroenterologists Who Commit to Performing Colonoscopies for CHC Patients
Colonoscopy follow-up after abnormal FIT is low and is not monitored by CHCs. This problem is exacerbated by the lack of gastroenterology services during the pandemic. Community gastroenterologists can be a part of the solution by committing to provide colonoscopies to patients with abnormal FIT, including those with Medicaid insurance.
Assess Cancer Prevention Priorities Among Individuals in Underserved Communities
The COVID-19 crisis has resulted in an economic burden for many communities. Claims for unemployment are at a historic high. The pandemic has exacerbated existing health disparities in underserved and racial and ethnic minority communities. This undoubtedly is the result of long-standing inequities related to the social determinants of health. Because of the economic challenges currently faced by low-income and underserved communities (eg, unemployment, loss of housing, and debt), CRC screening, as well as screening for other cancers, may be a low priority. It is important that we assess the immediate and anticipated long-term impacts on readiness and barriers of individuals in these communities to engage in cancer screening and that providers adapt process and workflow to address their needs and challenges.
Assess Regional CRC Screening and Follow-up Barriers and Solutions
Some of the lessons and experiences we describe may not be applicable to CHCs and underserved communities in regions outside ours. For example, rural communities may face comparable but undoubtedly different challenges. As the saying goes, “If you have seen one CHC, you have seen one CHC.” Regional barriers require regional solutions. It will be important for other CHCs to conduct their own assessment and provide their unique call to action to address CRC screening in their communities.
Conclusion
We currently face, and are likely to continue to experience, unprecedented health-care delivery challenges posed by the COVID-19 pandemic. Like the call for global unity to combat this public health crisis, there is a need for national and local solidarity to ensure that cancer screening continues to be delivered to those at greatest need. Following the emergence of COVID-19, the case for CRC screening became even more urgent, given the already low screening rates and disproportionate and pronounced disparities experienced by medically underserved communities. The many challenges ahead should give us enough pause to consider Dr Martin Luther King Jr's insightful words delivered in his last Christmas sermon before his assassination: “It really boils down to this: that all life is interrelated. We are all caught in an inescapable network of mutuality, tied in a single garment of destiny. Whatever affects one directly, affects all indirectly.”
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health (UG3 CA233314-01 to MEM, SG, and SFC; U54CA132384 to SFC; and U54CA132379 to MEM; 5 R37 CA222866-02 to SG) and the American Cancer Society (RSG-17-232-01-CPPB to JNN).
Notes
Role of the funder: Funding bodies had no role in the study design, analysis, interpretation of data, writing of manuscript, or decision to submit manuscript for publication.
Disclosure: All authors declare that they have no conflict of interest.
Acknowledgments: We are grateful to Savannah Bradley, MPH; Jennifer Covin, MPH; Lita Hinton; and Valesca Largaespada, MPH, for their valuable contributions.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Supplementary Material
References
- 1. Webb Hooper M, Nápoles AM, Pérez-Stable EJ.. COVID-19 and racial/ethnic disparities [published online ahead of print May 11, 2020]. JAMA 2020; doi:10.1001/jama.2020.8598. [Google Scholar]
- 2. Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. [DOI] [PubMed] [Google Scholar]
- 3. Siegel RL, Miller KD, Jemal A.. Cancer statistics, 2020. CA: A Cancer J Clin. 2020;70(1):7–30. [DOI] [PubMed] [Google Scholar]
- 4. Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58(1):9–31. [DOI] [PubMed] [Google Scholar]
- 5. Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9(3):222–231. [DOI] [PubMed] [Google Scholar]
- 6. Ellis L, Canchola AJ, Spiegel D, et al. Trends in cancer survival by health insurance status in California from 1997 to 2014. JAMA Oncol. 2018;4(3):317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116(3):544–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. National Health Interview Survey: Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/nhis/. Accessed May 30, 2020.
- 9. Gupta S, Sussman DA, Doubeni CA, et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014;106(4):dju032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. White A, Thompson TD, White MC, et al. Cancer screening test use-United States. MMWR Morb Mortal Wkly Rep. 2017;66(8):201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Degeling K, Baxter NN, Emery J, et al. An inverse stage-shift model to estimate the excess mortality and health economic impact of delayed access to cancer services due to the COVID-19 pandemic. medRxiv. 2020;10.1101/2020.05.30.20117630:2020.05.30.20117630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sharpless NE. COVID-19 and cancer. Science. 2020;368(6497):1290. [DOI] [PubMed] [Google Scholar]
- 13.Health Resources & Service Administration. 2019 National Health Center Data. https://bphc.hrsa.gov/uds/datacenter.aspx. Accessed May 30, 2020.
- 14. Quickstats: Percentage of adults aged 50-75 years who met colorectal cancer (CRC) screening recommendations*(dagger)—national health interview survey, United States, 2018( section sign). MMWR Morb Mortal Wkly Rep. 2020;69(11):314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Colorectal Cancer Roundtable. Working toward the shared goal of 80% screened for colorectal cancer by 2018. http://nccrt.org/what-we-do/80-percent-by-2018/. Accessed May 30, 2020.
- 16.Office of Disease Prevention and Health Promotion. Healthy People 2020. https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services/data. Accessed May 30, 2020.
- 17. Bharti B, May FFP, Nodora J, et al. Diagnostic colonoscopy completion after abnormal fecal immunochemical testing and quality of tests used at 8 federally qualified health centers in Southern California: opportunities for improving screening outcomes. Cancer. 2019;125(23):4203–4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liss DT, Brown T, Lee JY, et al. Diagnostic colonoscopy following a positive fecal occult blood test in community health center patients. Cancer Causes Control. 2016;27(7):881–887. [DOI] [PubMed] [Google Scholar]
- 19.National Association of Community Health Centers. http://www.nachc.org/. Accessed May 30, 2020.
- 20. Palinkas LA, Mendon SJ, Hamilton AB.. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40(1):423–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sultan S, Lim JK, Altayar O, et al. AGA Institute rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020; doi:10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gupta S, Coronado GD Argenbright K, et al. Mailed fecal immunochemical test outreach for colorectal cancer screening: summary of a Centers for Disease Control-sponsored summit. CA Cancer J Clin. 2020;70(4):283–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Issaka RS, Somsouk M. Colorectal Cancer Screening and Prevention in the COVID-19 Era. JAMA Health FOrum.2020;1(5):e200588. [DOI] [PMC free article] [PubMed]
- 24.California Primary Care Association. Data source: 2020 California Primary Care Association financial survey for California Health Centers. https://www.cpca.org/cpca/CPCA/HEALTH_CENTER_RESOURCES/Operations/EP_Resources.aspx? WebsiteKey=4190cf54-8e68-4858-9a19-e7253d7d94e1. Accessed May 30, 2020.
- 25. Lurie N, Carr BG.. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745–746. [DOI] [PubMed] [Google Scholar]
- 26. Lin CC, Dievler A, Robbins C, et al. Telehealth in health centers: key adoption factors, barriers, and opportunities. Health Aff. 2018;37(12):1967–1974. [DOI] [PubMed] [Google Scholar]
- 27. Din HN, McDaniels-Davidson C, Nodora J, et al. Profiles of a health information-seeking population and the current digital divide: cross-sectional analysis of the 2015-2016 California health interview survey. J Med Internet Res. 2019;21(5):e11931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Community Preventive Services Task Force. Guide to community preventive services. https://www.thecommunityguide.org/task-force/about-community-preventive-services-task-force. Accessed May 30, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.