Brain tumors are the most frequent solid neoplasm of childhood,1 representing the second cause of death after trauma. Prognosis mainly depends on histology, molecular lesions, and staging.2
The COVID-19 pandemic has dramatically changed health care delivery. Italy is one of the most coronavirus-affected countries, facing unprecedented resource shortages and organizational changes.
Children with brain neoplasms are served best at pediatric hospitals that have multidisciplinary resources.2 COVID-19 disease in the pediatric population has been shown to be less severe than in adults,3 with a milder organizational impact on children’s hospitals. However, delayed referral of severe conditions with a high mortality rate has been reported in pediatrics.4
Bambino Gesù Children’s Hospital in Rome serves approximately 100 of the 400 Italian childhood brain tumor new cases/year, offering a unique scenario to analyze the indirect impact of the COVID-19 outbreak on this population.
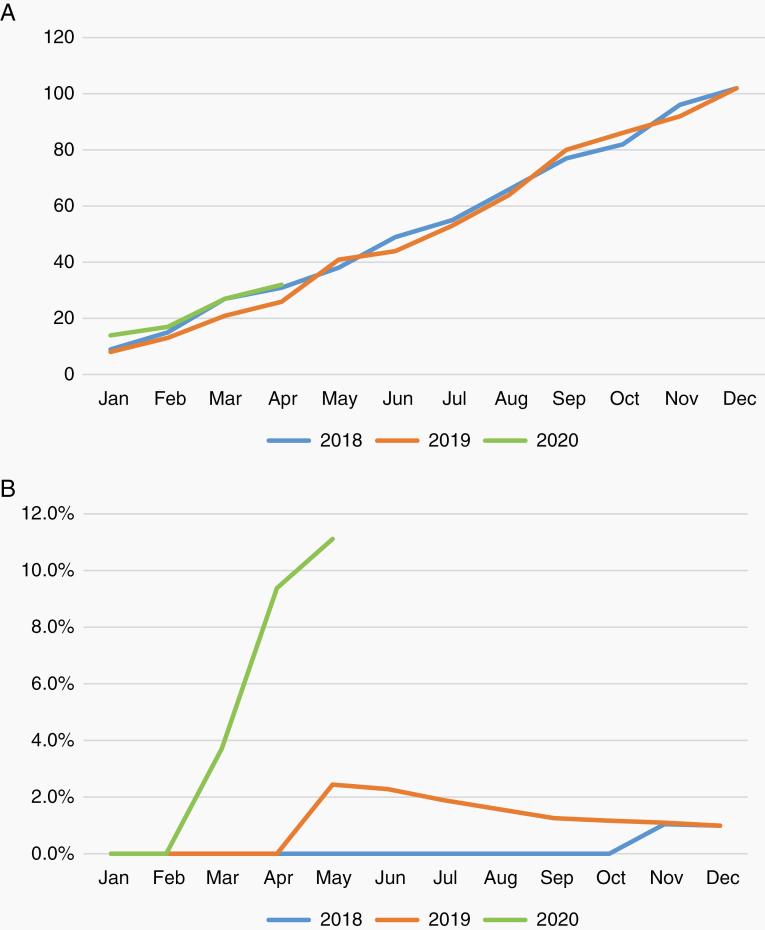
In March–April 2020, the period following the Italian government decision to lock down for the COVID-19 outbreak, we observed 4 patients with new diagnoses, with incipient clinical decompensation needing immediate life-/function-saving treatment. Assuming a stable recruitment for the current year, this corresponds to a 4-fold increase of this rare life-threatening situation, having been observed in 1% of cases in the last 2 years at our center, including those referred from other hospitals (Fig. 1).
Fig. 1.
(A) New central nervous system tumor diagnosis at Bambino Gesù Children’s Hospital in the last 24 months (number of cases/month); (B) cumulative percentage of patients with new diagnoses, showing clinical decompensation at onset.
The first child was a 6-year-old girl, presenting with intracranial hypertension due to an 8.5 cm left parieto-occipital tumor with no signs of bleeding. She had a 2-week history of vomiting, lately associated with loss of consciousness episodes. She finally presented to our center for a suspected generalized seizure, rapidly showing signs of decerebration and anisocoria progressing to bilateral fixed pupils. She died despite emergency resection of a malignant astroblastoma.
The second child was a 5-month-old girl with a one-month history of psychomotor regression. She presented with drowsiness and right gaze and neck deviation. A transfontanellar ultrasound showed a large multicystic lesion with midline shift and hydrocephalus. A subsequent MRI excluded signs of acute tumor volume increase. Clinical stabilization was obtained after drainage of cystic components. Histological diagnosis was desmoplastic infantile astrocytoma.
The third child was an 8-year-old girl with progressive cachexia associated, in the last 2 months, with polyuria and polydipsia. She presented to the emergency room for acute visual impairment. MRI showed a 4 cm infundibular lesion and a pineal region metastasis with intralesional hemorrhage without hydrocephalus. Non-germinomatous germ cell tumor was diagnosed and appropriate medical treatment was urgently started.
The last patient was an 8-year-old girl with a three-week history of vomiting. She presented to the emergency department for acute blindness. MRI showed a fourth-ventricle tumor with hydrocephalus. She was immediately treated for intracranial hypertension and underwent uneventful resection of a medulloblastoma. Unfortunately, she did not recover from her left eye blindness.
None of the families was under quarantine and all had consulted their family pediatrician, receiving symptomatic treatment, without direct clinical evaluation, which was deferred because of the pandemic. All of them presented to the emergency department once neurologic deterioration was evident.
Our 4 cases indicate that children with brain tumors represent a fragile population exquisitely exposed to the indirect effects of the COVID-19 pandemic. Considering the daily life impact of lockdown, it is reasonable to foresee a significant delay in brain tumor diagnosis in the pediatric population. Robust neurologic compensatory mechanisms in children, scarce familiarity with diagnostic clinical signs, and parental fear to expose children to the hospital environment contribute to explain the poor clinical conditions recorded at the time of diagnosis. School closure might also have contributed, as teachers are often the first to notice initial neurologic abnormalities. New onset headache, balance difficulty, and loss of developmental stages are symptoms that should always be valorized for a prompt direct clinical evaluation and possible imaging, not to be deferred due to fear/concern of COVID-19 pandemic.
We strongly advocate initiatives to increase the awareness of early signs of childhood brain tumors, for both pediatricians and families, in order to minimize avoidable mortality/long-term sequel risks.
Funding
The authors received no funding related to the preparation of this manuscript.
Conflict of interest statement. Authors declare no conflicts of interest.
Authorship statement. Study conception: AC, AM. Data collection: AC. Drafting of manuscript: AC, AM. Critical revision of manuscript: all authors. Supervision: FL.
References
- 1. Ostrom QT, Cioffi G, Gittleman H, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro Oncol. 2019;1(21): v1–v100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chintagumpala M, Gajjar A. Brain tumors. Pediatr Clin North Am. 2015;62(1):167–178. [DOI] [PubMed] [Google Scholar]
- 3. Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20(6):689–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4(5):e10–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]