The current COVID-19 (SARS-CoV-2 infection) pandemic has had extraordinary socioeconomic and public health impacts globally.1 Population movements (both travel and migration) have been limited worldwide due to the necessary travel restrictions imposed. Two patients presenting with fever during the COVID-19 pandemic were finally diagnosed with travel-associated infections.
Case 1
A previously healthy, 23-year-old Spanish female presented in May 2020 with a 6-day history of fever, chills and headache.
She worked in a rural area of Senegal from March to November 2019, and had taken malaria prophylaxis with mefloquine incorrectly. In mid-September she had fever and was diagnosed with malaria [positive rapid diagnostic test (RDT), blood examination for parasites not performed] which resolved with a full course of artemether–lumefantrine. At the end of October a self-limiting 48-hour history of fever was associated with upper respiratory-tract symptoms. On return to Spain an assessment at the out-patient clinic (including a blood count, serum biochemistry, HIV/hepatitis B and C/syphilis/Schistosoma and Strongyloides serology and polymerase chain reaction (PCR) for Plasmodium) was normal/negative. The patient referred no further international travel since November 2019.
In May 2020, two SARS-CoV-2 PCR tests were performed (nasopharyngeal samples) to investigate the fever (both negative). Due to persisting fever, with no apparent focalizing symptoms/signs, the patient attended the emergency department. Blood tests revealed mild anaemia (Hb 10.3 g/dl), lymphopenia (540 cells/μl), elevated bilirubin (2.59 mg/dl) and elevated LDH (511 U/L), and chest X-ray was normal. A rapid test for SARS-CoV-2 IgM/IgG was negative.
Case 2
A previously healthy 44-year-old Nigerian male presented in May 2020 with a 5-day history of fever and myalgia.
He had been living in Spain for 14 years, returned to his country on several occasions and referred previous malaria episodes. The patient returned from a 4-month trip visiting relatives in Nigeria at the beginning of March 2020, he had taken prophylaxis with atovaquone–proguanil incorrectly and referred a self-limiting non-specific febrile episode during travel. In May 2020 at the emergency department, blood tests showed elevated bilirubin (1.35 mg/dl), LDH level (255 U/L), lymphopenia (280 cells/μl) and thrombocytopenia (70 × 103 cells/μl). Blood and urine cultures, coronavirus PCR, HIV, hepatitis C and syphilis serology were all negative (hepatitis B serology suggestive of past infection).
Given the previous history of travel in both cases, blood smear examinations were requested at the emergency department, revealing Plasmodium ovale (P. ovale), confirmed by PCR, with a parasitemia <1% (malaria RDT negative). Both received standard treatment following diagnosis (see Figure 1).
Figure 1.
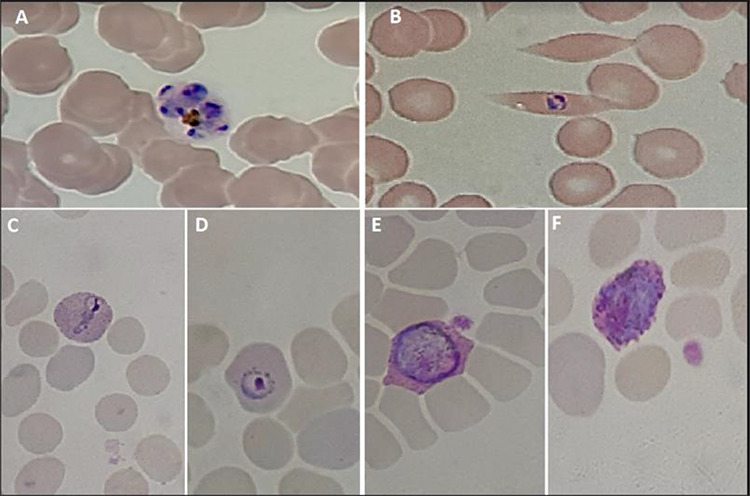
Giemsa-stained thin blood smears from Case 2 (A, B) and Case 1 (C, D, E, F). (A) Typical P. ovale schizont with 4–12 merozoites and a pigment concentrated mass. (B–D) P. ovale trophozoites parasitizing enlarged (C, D) and often distorted (B) erythrocytes. (E, F) P. ovale male (E) and female (F) round gametocytes. Note: Schüffner’s dots, typical of P. ovale and P. vivax, are clearly visible in parasitized erythrocytes of Case 1
Discussion
Imported infections have decreased during the current pandemic but travel history remains relevant, especially in risk groups such as travellers or immigrants visiting friends and relatives and aid workers.2,3 Both patients took malaria prophylaxis incorrectly (although establishment of P. ovale hypnozoites may not have been prevented) and not unexpectedly, RDTs were negative (due to low sensitivity for non-falciparum malaria), serving as a reminder that correct diagnosis of malaria should be based on peripheral blood examination.4 Misdiagnosis of P. ovale may lead to incorrect management through failure to administer anti-hypnozoite therapy (the self-limiting febrile illnesses referred by both patients prior to definitive diagnosis may have represented relapses). Delay in the diagnosis of malaria and other imported infections has occurred during other health crises, such as the recent Ebola outbreaks. Despite the current public health emergency and travel restrictions, imported infections with prolonged incubation periods and possibility of relapse should always be considered in the differential diagnosis of febrile patients especially if alternative, more frequent diagnoses such as COVID-19 are not confirmed.5
Authors’ contribution
All authors contributed to the clinical management of the patients and interpretation of the data. F.F.N. wrote the manuscript.
Acknowledgement
Support was provided by the Instituto de Salud Carlos III project ‘RD16/0027/0020’ Red de Enfermedades Tropicales, Subprograma RETICS del Plan Estatal de I +D+I.
Conflict of Interest
None declared.
References
- 1.World Health Organization https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (28 May 2020, date last accessed)
- 2. Walz EJ, Volkman HR, Adedimeji AA et al. Barriers to malaria prevention in US-based travellers visiting friends and relatives abroad: a qualitative study of west African immigrant travellers†. J Travel Med 2019; 26:tay163. doi: 10.1093/jtm/tay163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kain D, Findlater A, Lightfoot D et al. Factors affecting pre-travel health seeking behaviour and adherence to pre-travel health advice: a systematic review. J Travel Med 2019; 26:taz059. doi: 10.1093/jtm/taz059. [DOI] [PubMed] [Google Scholar]
- 4. Tang J, Tang F, Zhu H et al. Assessment of false negative rates of lactate dehydrogenase-based malaria rapid diagnostic tests for plasmodium ovale detection. PLoS Negl Trop Dis 2019; 13:e0007254. doi: 10.1371/journal.pntd.0007254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Groger M, Fischer HS, Veletzky L et al. A systematic review of the clinical presentation, treatment and relapse characteristics of human plasmodium ovale malaria. Malar J 2017; 16:112. doi: 10.1186/s12936-017-1759-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


