ABSTRACT
BACKGROUND
Preliminary data suggest that Coronavirus Disease-2019 (COVID-19) is associated with hypercoagulability and neurovascular events, but data on outcomes is limited.
OBJECTIVE
To report the clinical course and outcomes of a case series of COVID-19 patients with a variety of cerebrovascular events.
METHODS
We performed a multicentric, retrospective chart review at our three academic tertiary care hospitals, and identified all COVID-19 patients with cerebrovascular events requiring neuro-intensive care and/or neurosurgical consultation.
RESULTS
We identified 26 patients between March 1 and May 24, 2020, of whom 12 (46%) died. The most common event was a large-vessel occlusion (LVO) in 15 patients (58%), among whom 8 died (8/15, 53%). A total of 9 LVO patients underwent mechanical thrombectomy, of whom 5 died (5/9, 56%). A total of 7 patients (27%) presented with intracranial hemorrhage. Of the remaining patients, 2 had small-vessel occlusions, 1 had cerebral venous sinus thrombosis, and another had a vertebral artery dissection. Acute Respiratory Distress Syndrome occurred in 8 patients, of whom 7 died. Mortalities had a higher D-dimer on admission (mean 20 963 ng/mL) than survivors (mean 3172 ng/mL). Admission Glasgow Coma Scale (GCS) score was poor among mortalities (median 7), whereas survivors had a favorable GCS at presentation (median 14) and at discharge (median 14).
CONCLUSION
COVID-19 may be associated with hemorrhage as well as ischemia, and prognosis appears poorer than expected—particularly among LVO cases, where outcome remained poor despite mechanical thrombectomy. However, a favorable neurological condition on admission and lower D-dimer may indicate a better outcome.
Keywords: COVID-19, Large-vessel occlusion (LVO), Intracranial hemorrhage, Cerebral venous sinus thrombosis
ABBREVIATIONS
- ACE2
angiotensin-converting enzyme 2
- ARDS
Acute Respiratory Distress Syndrome
- CVST
cerebral venous sinus thrombosis
- COVID-19
Coronavirus Disease-2019
- GCS
Glasgow Coma Scale
- LVO
large-vessel occlusion
- SVO
small-vessel occlusion
- SDH
subdural hematoma
- VTE
venous thromboembolism
Recent reports suggest that COVID-19 is associated with an inflammatory, coagulopathic state that predisposes to strokes, which may occur in 5.7% of critically ill patients and may result in rapid clinical deterioration.1-5 The reported strokes include highly morbid large-vessel occlusions (LVOs), which may occur in younger patients with few or no identifiable risk factors for stroke.1-3,6
However, data describing the hospital course and outcomes of COVID-19 patients with stroke have been limited, and there is minimal discussion of hemorrhagic events, which may also occur in an inflammatory coagulopathy.7 From one of the epicenters of the pandemic, we report a large case series of COVID-19 patients with a spectrum of presenting neurovascular events, including ischemia and hemorrhage, and detail their clinical characteristics, hospital course, laboratory studies, and outcomes.
METHODS
Study Design and Participants
We performed a retrospective, longitudinal study of adult patients age > 18 at our 3 academic, tertiary care centers from March 1 through May 24, 2020. Inclusion criteria were patients who tested positive for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) via nasopharyngeal swab, and had a neurovascular event requiring intensive care unit admission for neuro-intensive care and/or neurosurgical consultation. Institutional Review Board approval was obtained, and individual patient consent was not required.
Data Collection
Using hospital and department datasets, we collected relevant demographic (eg, age and sex), clinical (eg, comorbidities), laboratory (eg, D-dimer), radiological, and outcomes data (eg, death and disposition) from electronic medical records. Neurovascular events were classified according to etiology, including acute ischemic stroke (eg, LVO), cerebral venous sinus thrombosis (CVST), and intracranial hemorrhage (eg, intraparenchymal, subarachnoid, and subdural). Hospital events included intubation, Acute Respiratory Distress Syndrome (ARDS), venous thromboembolism (VTE), and intervention (eg, mechanical thrombectomy and craniotomy). Data were reviewed by a team that included faculty neuro-intensivists, neuro-interventionalists, neurosurgeons, and a neuroradiologist.
RESULTS
We identified 26 patients in our health system meeting inclusion criteria (Table 1). In our cohort, 7/26 (27%) were younger than age 50, 12/26 died (46%), and among deaths, 10/12 (83%) were age 50 or older. The most frequent presenting neurovascular event (see Figure 1) was acute ischemic stroke in 17/26 patients (65%), of whom 15 had a LVO and 2 had a small-vessel occlusion (SVO). Among LVO patients, 13 were older than age 50 and/or had risk factors for stroke (13/15, 87%), 8 died (8/15, 53%), 7 survived with a favorable outcome (median Glasgow Coma Scale [GCS] score, 13), and 3 had hemorrhagic conversion (3/15, 20%). Five LVO patients developed ARDS (5/15, 33%), all of whom died. A total of 9 LVO patients underwent mechanical thrombectomy (9/15, 60%), of whom 5 died (5/9, 56%), and 4 survived with a good outcome (median GCS, 13.5). Two LVO patients underwent a decompressive craniectomy, including one for hemorrhagic conversion after thrombectomy (Figure 2), and another for malignant cerebral edema without prior thrombectomy (the patient later developed an unexplained acute subdural hematoma (SDH) 2 wk postoperatively).
TABLE 1.
Patient Demographics, Comorbidities, Hospitalization Events, and Outcomes
| Variable | All Patients (n = 26) |
|---|---|
| Age, mean (SD)—yr | 59 (16) |
| Age < 50—no. (%) | 7 (27) |
| Age ≥ 50—no. (%) | 19 (73) |
| Sex—no. (%) | |
| Male | 19 (73) |
| Female | 7 (27) |
| Race/ethnicity—no. (%) | |
| White | 5 (19) |
| African-American | 8 (31) |
| Hispanic/Latino | 5 (19) |
| Asian | 2 (8) |
| Other | 6 (23) |
| Pre-exiting conditions/comorbidities – no. (%) | |
| Hypertension | 14 (54) |
| Obesity (BMI ≥ 30) | 9 (35) |
| Antiplatelet agents/anticoagulants – no. (%) | 6 (23) |
| Atrial fibrillation | 5 (19) |
| Diabetes | 6 (23) |
| Cancer | 4 (15) |
| Smoking | 3 (12) |
| Coronary artery disease | 2 (8) |
| Admitting Characteristics | |
| Admission GCS—median (IQR) | 11 (7.25-14.75) |
| Admission GCS (survivors) | 14 (11.25-15) |
| Admission GCS (mortalities) | 7 (3.75-11.25) |
| Admission NIHSS—median (IQR) | 15 (9.75-20.25) |
| Cranial vascular events—no. (%) | |
| Acute ischemic stroke | 17 (65) |
| LVOa | 15 (58) |
| SVO | 2 (8) |
| Hemorrhagic conversion | 3 (12) |
| Intraparenchymal hemorrhage (hypertensive) | 1 (4) |
| Subarachnoid hemorrhage (aneurysmal) | 1 (4) |
| Hemorrhagic tumor | 2 (8) |
| SDH | 4 (15) |
| CVST | 1 (4) |
| Arterial dissection | 1 (4) |
| In-hospital events and complications—no. (%) | |
| Intubated | 14 (54) |
| ARDS | 8 (31) |
| Pneumonia | 12 (46) |
| Seizure | 1 (4) |
| VTE | 2 (8) |
| Treatment/Intervention—no. (%) | |
| Pharmacological treatment for COVIDb | 16 (62) |
| Chemical VTE prophylaxis | 21 (81) |
| Therapeutic anticoagulation | 5 (19) |
| Intravenous (IV) rtPA given | 6 (23) |
| Endovascular intervention | 10 (38) |
| Mechanical thrombectomy | 9 (35) |
| EVD or ICP monitor | 1 (4) |
| Open neurosurgical intervention | 5 (19) |
| Operative complication (SDH) | 1 (4) |
| Laboratory studies (mean, SD) | |
| D-dimer—ng/mL | 10,289 (23,525) |
| D-dimer among survivors | 3172 (3810) |
| D-dimer among mortalities | 20,963 (35,499) |
| White-cell count—thousand per μL | 9.7 (4.7) |
| Hemoglobin—g/dL | 12.7 (2.4) |
| Platelets—thousand per μL | 257 (120) |
| Ferritin—ng/mL | 922 (947) |
| C-reactive protein—mg/L | 45 (67) |
| Prothrombin time—sec | 13.9 (1.7) |
| Activated partial thromboplastin time—sec | 30.7 (5.0) |
| International normalized ratio | 1.1 (0.2) |
| Disposition—no. (%) | |
| Home | 8 (31) |
| Acute rehabilitation facility | 3 (12) |
| Skilled nursing or intermediate care facility | 3 (12) |
| Outcomes | |
| Death—no. (%) | 12 (46) |
| Discharge GCS—median (IQR) | 14 (13-15) |
| Length of stay—median (IQR) | 9 (4.25-10.75) |
SD, Standard Deviation; BMI, Body Mass Index; GCS, Glasgow Coma Scale; IQR, Interquartile Range; NIHSS, National Institutes of Health Stroke Scale; VTE, Venous Thromboembolism; rtPA, Recombinant Tissue Plasminogen Activator; EVD: External Ventricular Drain; ICP: Intracranial Pressure.
Internal carotid artery, basilar artery, intracranial vertebral artery, first segment of the middle cerebral artery (M1), first segment of the anterior cerebral artery (A1), and/or first segment of posterior cerebral artery (P1).
Including, but not limited to, hydroxychloroquine, azithromycin, and remdesivir.
FIGURE 1.
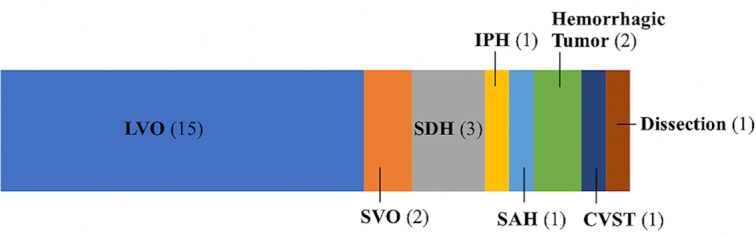
Spectrum of major neurovascular events among COVID-19 patients (n = 26).
FIGURE 2.
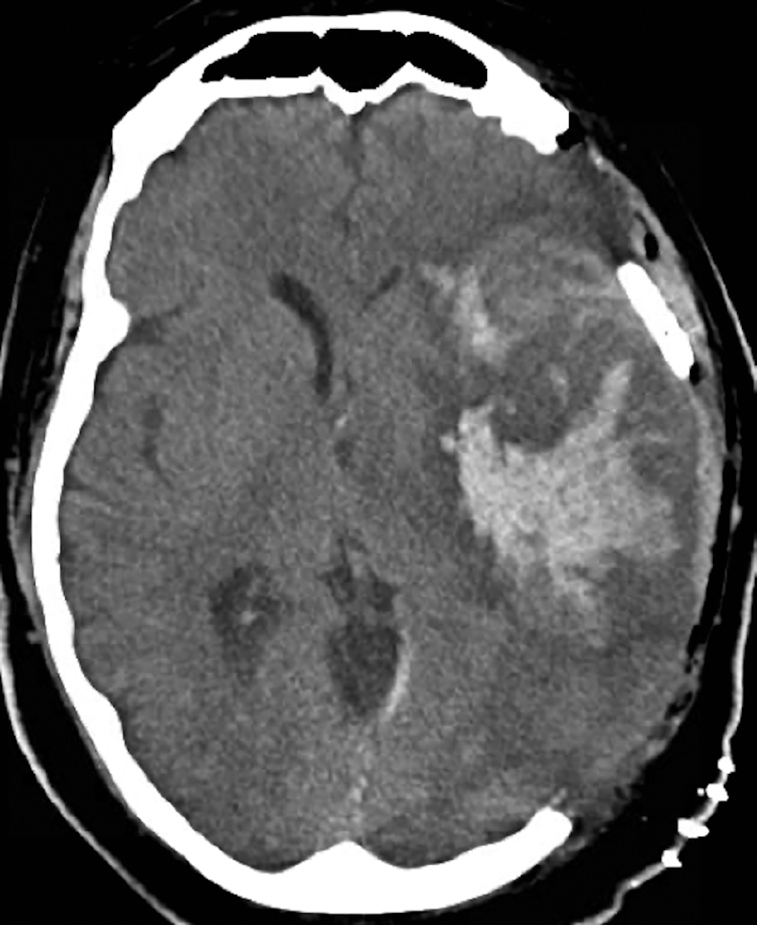
Postoperative axial noncontrast head computed tomography scan of a patient who had a left internal carotid artery occlusion, underwent thrombectomy, and then developed hemorrhagic conversion that required a decompressive craniectomy.
A total 7 of the 26 patients had an initial hemorrhagic event on presentation (7/26, 27%), including SDH (3/26) and hypertensive intraparenchymal hemorrhage (1/27). In addition, 1 patient had aneurysmal subarachnoid hemorrhage, who died after developing severe vasospasm and COVID-19-related ARDS, another had apoplexy from a known and previously stable pituitary adenoma, and a third had a hemorrhagic cerebellar metastasis with previously unknown metastatic disease in the brain.
One postpartum woman developed extensive CVST of multiple deep and superficial veins (Figure 3), but recovered with anticoagulation. Another had a spontaneous vertebral artery dissection, without resulting ischemia or hemorrhage, and was discharged neurologically intact. Two patients had subcortical SVOs.
FIGURE 3.
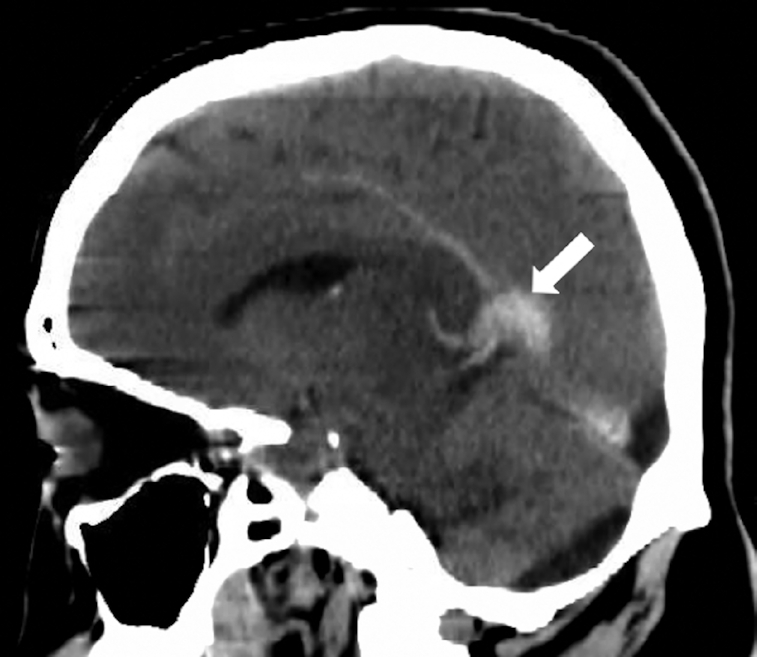
Sagittal noncontrast head computed tomography scan showing cerebral venous thrombosis. Arrow indicates thrombosis of the vein of Galen.
During hospitalization (median 9 d), 14 patients required intubation (14/26, 54%) and 8 developed ARDS (8/26, 31%), of whom 7 died (7/8, 88%). Two patients had venous thromboembolic events (2/26, 7.7%). Mortalities had a substantially higher D-dimer on admission (mean 20 963 ng/mL) than those ultimately discharged (3172 ng/mL) (see Figure 4). Ferritin was also noted to be elevated (mean 922 ng/mL overall). Mortalities had a lower GCS on admission (median 7) than survivors, whose median GCS was 14 on presentation and at discharge.
FIGURE 4.
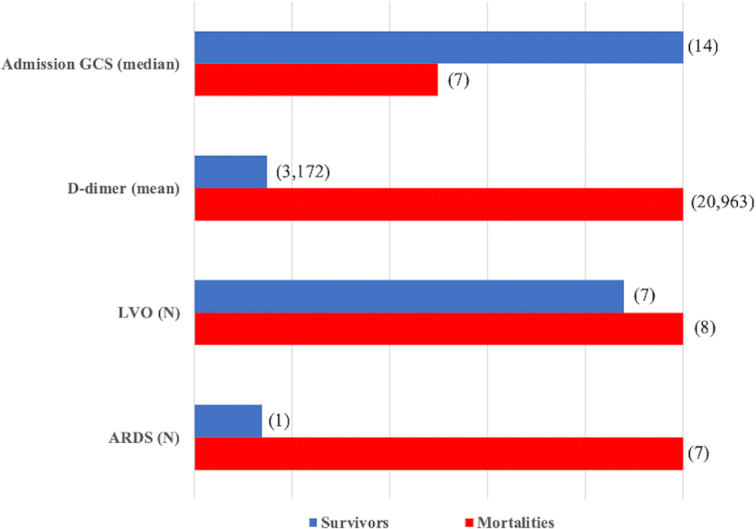
Characteristics of survivors and mortalities.
DISCUSSION
Our data supports the growing body of evidence that manifestations of COVID-19 may include neurologically devastating ischemic events.2,6,7 In particular, we found that the high mortality among COVID-19 patients with LVOs (8/15, 53%) was true even among those receiving mechanical thrombectomy (5/9, 56%), similar to a prior report of COVID-19 patients,6 and substantially greater than the generally cited rate of 15% prior to the pandemic.8 Although most patients in our series were older than age 50, we found that several younger patients presented with a LVO of unexplained etiology, consistent with prior reports.1
A subset of our patients (27%), however, presented with hemorrhage rather than ischemia—and among the LVO patients, 4 later developed intracranial hemorrhage—suggesting that COVID-19 might, in some cases, predispose to hemorrhagic complications. Although data are very limited, one study of COVID-19 patients reported 11 cases of ischemic strokes (5 LVOs), 1 CVST, and 1 cerebral hemorrhage—similar to the variety in our cohort—suggesting that COVID-19 may be associated with a spectrum of cerebrovascular pathology.7 The authors also reported an analogously high mortality rate among these 13 patients (38.5%).7 In another case series that included COVID-19 patients with 12 LVOs and 2 CVSTs, overall mortality was comparable (42.8%), and a similar proportion of patients developed hemorrhagic conversion requiring craniectomy.6
In addition to the initial neurological ictus, COVID-19 sequelae of other organ systems likely contributed to the high mortality. In particular, ARDS had a 88% case fatality rate in our series and was invariably fatal among LVO patients. However, although the overall mortality rate in our cohort was high, there appeared to be a dichotomous presentation and outcome—either a poor initial condition with fulminant disease (worse than expected from neurological event alone) or a favorable presentation followed by recovery. In effect, prognosis likely depends on the initial neurological condition and development of other COVID-19-related complications.
Cerebrovascular events in COVID-19 may be related to a coagulopathic, pro-inflammatory state that results in a cytokine release storm and thrombogenic, vascular endothelial dysfunction, as well as vasculitis,5,9-12 similar to phenomena observed in previous coronavirus outbreaks including Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome.4,13-15 It is possible that vascular endothelial injury, angiotensin-converting enzyme 2 (ACE2) receptor downregulation,16 and a systemic coagulopathic state may lead to a spectrum of neurovascular complications of COVID-19, including hemorrhage, ischemia, venous thrombosis, and arterial dissection (Figure 5). This may explain not only the observation of strokes (in otherwise healthy patients without risk factors for stroke), but also the high rate of hemorrhagic conversion, as well as hemorrhage from otherwise stable lesions (eg, aneurysm and pituitary adenoma). Notably, our finding of high D-dimer levels, previously reported among COVID-19 patients,9 may suggest a consumptive coagulopathy similar to Disseminated Intravascular Coagulation.12 Elevated D-dimer may also indicate greater disease severity,9 and might be a potential marker of prognosis, as levels were substantially higher among mortalities than survivors.
FIGURE 5.
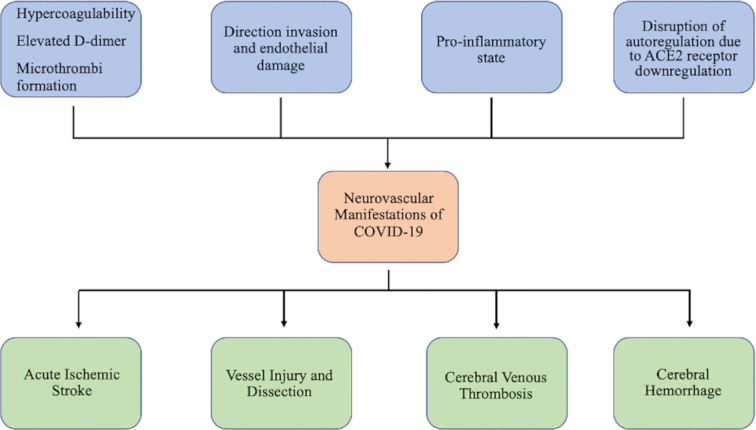
Flow chart showing factors that may lead to neurovascular pathology in COVID-19, including endothelial damage, inflammation, and ACE2 receptor downregulation. It is possible that cerebrovascular sequelae may include arterial ischemic and hemorrhagic events, dissection, and cerebral venous thrombosis.
CONCLUSION
In conclusion, we present a case series of a spectrum of major neurovascular events encountered among COVID-19 patients, including those with ischemic and hemorrhagic pathology. Although prognosis appears overall poor, higher initial GCS and lower D-dimer levels may indicate more favorable outcomes, a hypothesis that should be evaluated in future studies. Although causality has yet to be proven, future, population-based studies should also determine whether COVID-19 indeed influences the risk of a variety of cerebrovascular events. Such data would greatly influence management, such as deciding whether to anticoagulate, prescribe antiplatelet agents, or perform a mechanical thrombectomy or hemicraniectomy.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Contributor Information
Blake E S Taylor, Email: bt258@njms.rutgers.edu, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey.
Priyank Khandelwal, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey.
Michael S Rallo, Robert Wood Johnson Medical School, New Brunswick, New Jersey.
Purvee Patel, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey.
Lindsey Smith, Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey; Community Medical Center, a Robert Wood Johnson-Barnabas Health Facility.
Hai Sun, Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Robert Wood Johnson Medical School, New Brunswick, New Jersey.
Anil Nanda, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey; Robert Wood Johnson Medical School, New Brunswick, New Jersey; Department of Neurology, Division of Stroke and Neurocritical Care, Robert Wood Johnson University Hospital New Brunswick, New Jersey.
Amit Singla, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey.
Sudipta Roychowdhury, Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey; Robert Wood Johnson Medical School, New Brunswick, New Jersey.
Roger C Cheng, Department of Neurology, Division of Stroke and Neurocritical Care, Robert Wood Johnson University Hospital New Brunswick, New Jersey.
Kiwon Lee, Department of Neurology, Division of Stroke and Neurocritical Care, Robert Wood Johnson University Hospital New Brunswick, New Jersey.
Gaurav Gupta, Department of Neurosurgery, Rutgers New Jersey Medical School, Newark, New Jersey; Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey; Robert Wood Johnson Medical School, New Brunswick, New Jersey.
Stephen A Johnson, Department of Neurosurgery, Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Rutgers Neurosurgery Health Outcomes, Policy, and Economics (H.O.P.E.) Center, New Brunswick, New Jersey; Robert Wood Johnson Medical School, New Brunswick, New Jersey.
REFERENCES
- 1. Oxley TJ, Mocco J, Majidi S et al. . Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382(20):e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mao L, Jin H, Wang M et al. . Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Avula A, Nalleballe K, Narula N et al. . COVID-19 presenting as stroke. Brain Behav Immun. 2020;87;115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bikdeli B, Madhavan MV, Jimenez D et al. . COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75(23):2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Klok FA, Kruip M, van der Meer NJM et al. . Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sweid A, Hammoud B, Weinberg JH et al. . Letter: Thrombotic neurovascular disease in COVID-19 patients. Neurosurgery. published online: 2020(doi: 10.1093/neuros/nyaa254). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li Y, Wang M, Zhou Y et al. . Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Lancet. published online: 2020(doi: 10.2139/ssrn.3550025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Katsanos AH, Malhotra K, Goyal N et al. . Mortality risk in acute ischemic stroke patients with large vessel occlusion treated with mechanical thrombectomy. J Am Heart Assoc. 2019;8(21):e014425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lippi G, Favaloro EJ. D-dimer is associated with severity of coronavirus disease 2019: A pooled analysis. Thromb Haemost. 2020;120(5):876-878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473-474. [DOI] [PubMed] [Google Scholar]
- 11. Varga Z, Flammer AJ, Steiger P et al. . Endothelial cell infection and endotheliitis in COVID-19. Lancet North Am Ed. 2020;395(10234):1417-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. published online: 2020(doi: 10.1111/jth.14849). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chong PY, Chui P, Ling AE et al. . Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128(2):195-204. [DOI] [PubMed] [Google Scholar]
- 14. Umapathi T, Kor AC, Venketasubramanian N et al. . Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol. 2004;251(10):1227-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Who Mers-Cov Research G. State of knowledge and data gaps of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in humans. PLoS Currents. 2013;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586-590. [DOI] [PMC free article] [PubMed] [Google Scholar]


