Latin America has become an epicentre of coronavirus disease 2019 (COVID-19) pandemic and Brazil is the most affected country by the novel coronavirus currently. In Brazil, the first case of COVID-19 was confirmed on 26 February 2020, in the São Paulo metropolis, in a Brazilian man who traveled from 9 to 20 February 2020, to Lombardy, Northern Italy, where a significant outbreak was ongoing.1 COVID-19 spread rapidly across Brazilian states2 and now >2 million cases and 85 000 deaths has been registered.
Brazil is a country of continental dimensions that presents regional social inequalities with millions of people living in highly dense communities, with precarious housing conditions and poor sanitation. Additionally, it is estimated that one in five Brazilian adults has two or more morbidities,3 which may increase the susceptibility to COVID-19 mortality, especially among poor people.4 As the association between COVID-19 and poverty is still poorly described, it is necessary to assess the impact of social inequalities on severity and mortality due to COVID-19.5
In this ecological study, we investigated the association between social inequality and COVID-19 fatality rate in Aracaju municipality, Sergipe state, Northeast Brazil. Aracaju has an area of 182.2 km2 and an estimated population of 657 053 inhabitants. The proportion of literacy rate and the average number of residents per household obtained from Instituto Brasileiro de Geografia e Estatística 2010 (Brazilian Institute of Geography and Statistics, in English language) are 93.7 and 3.37, respectively. In addition, the proportion of low-income households is 42.9% and the Human Development Index is 0.770. Currently, the municipality is divided into 42 neighbourhoods that are organized in four urban zones (North, South, East and West).
Data on COVID-19 and population data were obtained from information systems and they were used to calculate the rates of incidence and case fatality due to COVID-19 for each neighbourhood of Aracaju. Case fatality rate (CFR) has been used to assess the severity and healthcare capacity in response to the COVID-19 outbreak and it was estimated dividing the number of confirmed deaths from COVID-19 by the number of registered cases for each neighbourhood. Data were retrieved from accurate databases up to 14 July 2020.
Social inequality was evaluated for each neighbourhood based on the Living Conditions Index (LCI) proposed by Carvalho et al.6 LCI is an aggregate score that summarizes three components of living conditions including education (proportion of households headed by illiterate people), income (proportion of households earning less than one-fourth of the minimum wage per capita) and housing (proportion of households in subnormal agglomerates including slums, villages, irregular lots, shacks and stilt houses). The score index ranges from 3 to 90 and higher values indicate worse living conditions. Neighbourhoods were grouped into LCI quartiles: high (3–24), intermediate (25–44), low (45–60) and very low (62–90).
Cochran–Armitage test was used to evaluate the trend of the incidence rate and CFR by LCI stratum. The significance level was set at 5%. Analyses were performed by using JASP software version 0.13 (JASP Team, Amsterdam, the Netherlands).
On 14 March 2020, the first case of COVID-19 in Aracaju was identified in a female patient with recent travel to Spain, whereas on 2 April 2020, the first death from disease was officially confirmed. At the time of writing this study, SARS-CoV-2 has infected 21 207 patients and resulted in 429 deaths. Most deaths occurred among males (n = 248; 57.8%) and in people aged > 60 years (n = 297; 69.2%). The median time from onset of symptoms to death was 14 days (Q1 = 8; Q3 = 23).
The incidence rate of COVID-19 was 322.8 cases per 10 000 population and the CFR was 2.0%. Although the highest incidence rates were recorded in the neighbourhoods with better living conditions (P < 0.001), there was an increasing trend in the mortality rate in neighbourhoods with higher social inequality (P < 0.001). The COVID-19 CFR was 2-fold higher for neighbourhoods with very-low LCI compared with neighbourhoods with high LCI (Table 1). Geographically, the highest mortality estimates have been observed in the North and West zones, which have a large number of socio-economically deprived neighbourhoods in Aracaju. Approximately, 57% of neighbourhoods (12 of 21) in these zones had CFR >1.5% (Figure 1).
Table 1.
Incidence rate and COVID-19 fatality rate according to the LCI
| LCI | Neighbourhoods | Urban zones | COVID-19 estimates | ||||||
|---|---|---|---|---|---|---|---|---|---|
| East | West | South | North | Incidence ratea (per 103 inhabitants) | P value | CFRa (%) | P value | ||
| High | 10 | 8 (80.0%) | 1 (10.0%) | 1 (10.0%) | 0 | 398.4 | <0.001 | 0.8 | <0.001 |
| Intermediate | 10 | 3 (30.0%) | 2 (20.0%) | 4 (40.0%) | 1 (10.0%) | 295.0 | 1.2 | ||
| Low | 10 | 0 | 3 (30.0%) | 2 (20.0%) | 5 (50.0%) | 248.2 | 1.7 | ||
| Very-low | 12 | 0 | 2 (16.7%) | 3 (25.0%) | 7 (58.3%) | 193.4 | 2.0 | ||
aMissing data for cases and deaths according to the neighbourhood’s distribution were counted to 2763 and 184, respectively.
Figure 1.
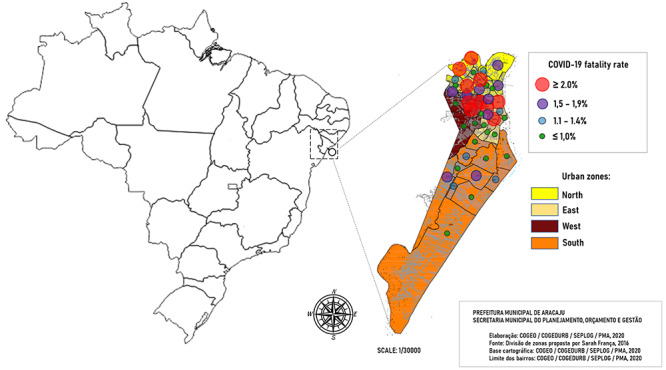
Mapping COVID-19 fatality rates according to the neighbourhoods in Aracaju municipality, Sergipe, Brazil.
Differences in COVID-19 infection and mortality rates are emerging as a result of the co-occurring non-communicable diseases and the existing poor social conditions.5 The most vulnerable populations have been disproportionately impacted by COVID-19, where areas with the greatest inequities are those most affected.7–9 Reduced geographic access to SARS-CoV-2 testing sites is associated with socio-demographic factors that are linked to poor structural access to care and health outcomes.10 In Aracaju, COVID-19 pandemic has exposed historical inequalities and poor communities have shown limited testing resources and higher fatality rates from COVID-19 compared with communities with better living conditions.
People living in socio-economically disadvantaged communities are substantially less likely to have education, adequate sanitation, access to clean water to wash hands, opportunity to work from home office and healthcare access. Furthermore, poor people are more likely to live in crowed homes and present underlying medical conditions including hypertension and diabetes that are considered risk factors for severe COVID-19. In addition, the difficulty to maintain social distancing in subnormal agglomerates contributes to SARS-CoV-2 spread and mortality in vulnerable populations.
This study has some limitations. The data were obtained from surveillance information systems and therefore cases are likely to be underreported. However, our findings showed that the poorest neighbourhoods have lower records of COVID-19, but higher fatality rates compared with neighbourhoods with better living conditions. These findings may reflect important implications of health and social inequalities and showed differences in testing resources and mortality estimates among urban communities. This scenario calls to urgent strategies to reduce the spread and mortality from COVID-19 in high-deprivation communities.
Authors’ Contributions
All authors contributed equally to the manuscript.
Acknowledgments
We dedicate this article to all the doctors, frontline health workers and other staff who are facing COVID-19. This study is part of the EpiSERGIPE project.
Conflict of interest
None declared.
References
- 1. Rodriguez-Morales AJ, Gallego V, Escalera-Antezana JP et al. . COVID-19 in Latin America: the implications of the first confirmed case in Brazil. Travel Med Infect Dis 2020; 35:101613 https://linkinghub.elsevier.com/retrieve/pii/S1477893920300806(15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Candido DDS, Watts A, Abade L et al. . Routes for COVID-19 importation in Brazil. J Travel Med 2020; 27 https://academic.oup.com/jtm/article/doi/10.1093/jtm/taaa042/5809508 (20 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nunes BP, Chiavegatto Filho ADP, Pati S et al. . Contextual and individual inequalities of multimorbidity in Brazilian adults: a cross-sectional national-based study. BMJ Open 2017; 7:e015885 http://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2017-015885 (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patel JA, Nielsen FBH, Badiani AA et al. . Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health 2020; 183:110–1. http://www.ncbi.nlm.nih.gov/pubmed/32502699 (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020. http://www.ncbi.nlm.nih.gov/pubmed/32535550 (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carvalho RA da S, Santos VS, de MCM, Gurgel RQ, Oliveira CC da C. Inequalities in health: living conditions and infant mortality in Northeastern Brazil. Rev Saude Publica 2015; 49 http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102015000100202&lng=en&tlng=en (16 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020; 8:659–61. https://linkinghub.elsevier.com/retrieve/pii/S2213260020302344(16 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finch WH, Hernández Finch ME. Poverty and Covid-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Sociol 2020; 5 https://www.frontiersin.org/article/10.3389/fsoc.2020.00047/full (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baqui P, Bica I, Marra V, Ercole A, Schaar M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Heal 2020. https://linkinghub.elsevier.com/retrieve/pii/S2214109X20302850 (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rader B, Astley CM, Sy KTL et al. . Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates. J Travel Med 2020. https://academic.oup.com/jtm/advance-article/doi/10.1093/jtm/taaa076/5837479 (15 July 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]


