Abstract
Background
In Louisiana, deaths related to COVID-19 have disproportionately occurred in Black persons. Granular data are needed to better understand inequities and develop prevention strategies to mitigate further impact on Black communities.
Methods
We conducted a retrospective study of patients admitted to an urban safety net hospital in New Orleans, Louisiana, with reactive SARS-CoV-2 testing from March 9 to 31, 2020. Clinical characteristics of Black and other racial/ethnic group patients were compared using Wilcoxon rank-sum test and Fisher exact tests. The relationship between race and outcome was assessed using day 14 status on an ordinal scale.
Results
This study included 249 patients. The median age was 59, 44% were male, and 86% were age ≥65 years or had ≥1 comorbidity. Overall, 87% were Black, relative to 55% Black patients typically hospitalized at our center. Black patients had longer symptom duration at presentation (6.41 vs 5.88 days; P = .05) and were more likely to have asthma (P = .008) but less likely to have dementia (P = .002). There were no racial differences in initial respiratory status or laboratory values except for higher lactate dehydrogenase in Black patients. Patient age and initial oxygen requirement, but not race (adjusted proportional odds ratio, 0.92; 95% CI, 0.70–1.20), were associated with worse day 14 outcomes.
Conclusions
Our results demonstrate minor racial differences in comorbidities or disease severity at presentation, and day 14 outcomes were not different between groups. However, Black patients were disproportionately represented in hospitalizations, suggesting that prevention efforts should include strategies to limit SARS-CoV-2 exposures and transmission in Black communities as one step toward reducing COVID-19-related racial inequities.
Keywords: COVID-19, hospitalizations, racial disparities, racial inequities, SARS-CoV-2
The United States now has more than 4 million reported cases of SARS-CoV-2, the novel coronavirus that causes the clinical syndrome known as COVID-19 [1]. Nationwide, COVID-19 has been shown to profoundly impact Black communities, with city and state public health data demonstrating disproportionately higher incidence and mortality rates among Black persons regardless of geographic region [2–6].
In Louisiana (LA), the first case of COVID-19 was diagnosed on March 9, 2020 [7], and in subsequent days the state earned the distinction of having the fastest-growing COVID-19 outbreak worldwide [8]. Since then, there have been more than 103 000 cases diagnosed in the state [8]. New Orleans, LA, emerged as an early epicenter of the epidemic, and in early March the city had one of the highest mortality rates globally [9]. Mortality rates were shown to be higher in Black Louisianans when Louisiana became one of the first states to release data by race/ethnicity. Most recent statistics from the Louisiana Department of Health show that Black persons represent 52% of deaths from COVID-19, while accounting for only 33% of the state’s population [9, 10]. In terms of hospitalizations, recently published data from a large integrated health system show that Louisiana mirrors other states that have experienced a dramatic overrepresentation of Black persons who require hospital admission for COVID-19 infection [11–13].
The objective of this study was to investigate trends in admission data as well as clinical characteristics and outcomes with respect to race among patients hospitalized with COVID-19 during the acceleration phase of the New Orleans pandemic. This review provides a single-center experience from University Medical Center (UMC), a tertiary care academic medical center that serves as the primary safety net hospital for the Greater New Orleans metropolitan area.
METHODS
We performed a retrospective review of patients hospitalized during the month of March 2020 who had screened positive for SARS-COV-2 on a reverse transcription polymerase chain reaction (PCR) nasopharyngeal swab. During the study period, our institution did not yet have in-house point-of-care testing for SARS-CoV-2. Test platforms varied during the month, with the majority of tests conducted by the Louisiana Office of Public Laboratory or private laboratory companies. When providers had suspicion for the virus, they would contact the state health department in order to have testing approved. In March 2020, testing through the State Public Health Lab was limited to patients meeting the following criteria: hospitalized with severe respiratory illness with no other known cause, suspected outbreak of COVID-19 among associated individuals with recent onset of fever and lower respiratory symptoms, recent fever and lower respiratory symptoms in a health care worker with direct contact to a laboratory-confirmed COVID-19 case, suspected COVID-19 in a patient associated with a high-risk exposure setting such as a long-term care facility or a correctional facility, suspected COVID-19 in a homeless patient. Patients who did not meet the state testing criteria could undergo testing through a commercial laboratory at their physician’s discretion.
An initial report was generated from our electronic health record that included all consecutive patients who underwent SARS-CoV-2 testing through March 31, 2020. Patient charts were then manually reviewed to determine whether SARS-CoV-2 was detected on testing. For those with positive/reactive SARS-CoV-2 testing, data abstraction into a REDCap database was conducted for the following elements: age, self-identified race and ethnicity, sex, body mass index (BMI), insurance type, days of symptoms at the time of hospitalization, presence of comorbidities, ZIP code, and laboratory and vital sign data from presentation and clinical outcomes. Race and ethnicity were documented according to patient self-identification at the time of hospital registration. Race categories are prespecified in the electronic health record and include American Indian or Alaskan Native, Asian, Black or African American, and White or Caucasian; ethnicity was categorized as Hispanic or non-Hispanic. Median income data were obtained for each participant’s five-digit ZIP code tabulation area (ZCTA) from the United States Census Bureau using the advanced search feature on the landing page at data.census.gov and the MABLE Geocorr tool. Analyses were run using R statistical software, version 3.6.2.
All charts were reviewed through April 14, 2020, to allow for a minimum of 2 weeks of follow-up for all patients. Patients were excluded if they had been transferred in from a hospital outside of our health system, as we would not have access to initial data points.
Patient Consent Statement
Before initiation of data collection, the study was approved by the LSU Institutional Review Board and University Medical Center Research Review Committee. The study was approved as medical chart review only, and the requirement for obtaining written informed consent was waived.
Analysis
Baseline Assessments
Patient demographics, comorbid conditions, and clinical characteristics at presentation were compared among Black and other racial/ethnic group patients. Because of relatively small numbers among other racial/ethnic group patients, all other races/ethnicities were grouped in analyses. Distributions of continuous variables were compared across racial groups using a Wilcoxon rank-sum test, and categorical variables were compared using a Fisher exact test. Charlson comorbidity index (CCI), which predicts 10-year survival in patients with multiple comorbidities, was calculated for each patient in the cohort and used as a measure of total comorbidity burden.
Outcomes
We examined outcomes that occurred during hospitalization including acute kidney injury, new dialysis requirement, requirement for invasive mechanical ventilation (IMV), and, in those who were extubated, any instance of reintubation. Two regression analyses were conducted. First, to determine the association between race and severity of illness at presentation, multivariable logistic regression was used to determine covariates associated with supplemental oxygen requirement on admission. Adjusted odds ratios (aORs) are reported for the logistic regression, along with 95% CIs, with confidence intervals >1 indicating an increased odds of oxygen need. To assess the association between patient race and hospital outcome, we examined day 14 patient outcomes according to an ordinal scale, using the following scoring system: death was assigned a score of 1, hospitalized and requiring invasive mechanical ventilation (IMV) were assigned a score of 2, hospitalized but not requiring IMV was assigned a score of 3, and discharged was assigned a score of 4. The adjusted proportional odds (aPOs) of better outcomes are reported for the cumulative logistic regression, along with 95% confidence intervals, with confidence intervals >1 indicating that that factor is associated with better outcomes in general. The analyses included the following covariates: CCI, age ≥65 years, BMI ≥40, smoking status (former or current), male sex, hypertension, asthma, income by ZCTA, and time (in days) since symptom onset. Asthma and hypertension were included separately, as they are not incorporated into the CCI. For predicting day 14 outcome, supplemental oxygen support was also included as a covariate. Covariates were standardized so that the magnitude of the confidence intervals would be directly comparable.
RESULTS
A total of 249 patients hospitalized and PCR positive for SARS-CoV-2 at our institution between March 9, 2020, and March 31, 2020, were included in the analysis (Table 1). All patients included had symptoms consistent with COVID-19 infection at admission, with the exception of 2 patients who were admitted for other reasons and developed symptoms concerning for SARS-CoV-2 infection during their stay necessitating testing. Two patients were excluded due to missing racial information. Male patients constituted 44.2% of the cohort. Of the cohort, 87.1% self-identified as Black, 6.4% identified as White, 1.6% identified as Asian, 5.2% identified as other, and 1.1% of the cohort identified as Hispanic; 1.5% of patients selected multiple races. The mean age of the cohort was 59.6 years (Black patients 59.2 years, other racial/ethnic group patients 62.5 years). The majority of patients (86%) had at least 1 of the following conditions or comorbidities: age ≥65, hypertension, diabetes mellitus, cardiovascular disease, asthma, chronic lung disease, BMI ≥40, end-stage renal disease, cancer, or liver disease. The most common comorbidities were hypertension (79%), hyperlipidemia (52%), and diabetes mellitus (52%). At the time of presentation, 58.6% of patients were febrile (T ≥100.4°F).
Table 1. .
Demographics and Comorbidities by Race for Patients Hospitalized With COVID-19
| Variables | All Patients (n = 249) | Black Patients (n = 217) | Other Racial/Ethnic Group Patients (n = 32) | P Value |
|---|---|---|---|---|
| Age ≥65 y | 89 (36) | 73 (34) | 16 (50) | .078 |
| Male sex | 110 (44) | 100 (46) | 10 (31) | .130 |
| Insurance | .2885 | |||
| None | 21 (8) | 16 (8) | 5 (16) | |
| Public insurance | 196 (79) | 172 (79) | 24 (75) | |
| Private insurance | 32 (13) | 29 (13) | 3 (9) | |
| Any comorbidity | 232 (93) | 202 (93) | 30 (94) | 1.000 |
| BMI ≥40 kg/m2 | 58 (23) | 51 (24) | 7 (22) | 1.000 |
| Ever smoker | 95 (38) | 86 (40) | 9 (28) | .246 |
| Asthma | 49 (20) | 48 (22) | 1 (3) | .008 |
| Chronic pulmonary disease | 32 (13) | 31 (14) | 1 (3) | .092 |
| Hypertension | 198 (80) | 174 (80) | 24 (75) | .487 |
| Myocardial infarction | 27 (11) | 25 (12) | 2 (6) | .546 |
| Cardiovascular disease | 80 (32) | 67 (31) | 13 (41) | .312 |
| Dementia | 21 (8) | 13 (6) | 8 (25) | .002 |
| Liver disease | 12 (5) | 11 (5) | 1 (3) | 1.000 |
| Diabetes mellitus | 130 (52) | 118 (54) | 12 (38) | .089 |
| Mean HbA1ca (SD), % | 8.41 (2.56) | 8.49 (2.59) | 7.56 (2.15) | .238 |
| ESRD | 24 (10) | 21 (10) | 3 (9) | 1.000 |
| Malignancy | 30 (12) | 25 (12) | 5 (16) | .559 |
| HIV infection | 6 (2) | 5 (2) | 1 (3) | .566 |
| CCI, mean (SD) | 2.37 (2.31) | 2.38 (2.32) | 2.31 (2.32) | .939 |
| Median home income (SD), thousands of dollars | 38.83 (11.21) | 38.10 (9.79) | 43.78 (17.59) | .029 |
Data are presented as No. (%) unless otherwise indicated. Statistically significant results are in bold.
Abbreviations: BMI, body mass index; ESRD, end-stage renal disease; HbA1c, glycosylated hemoglobin.
aHbA1c only analyzed in patients with diagnosis of diabetes
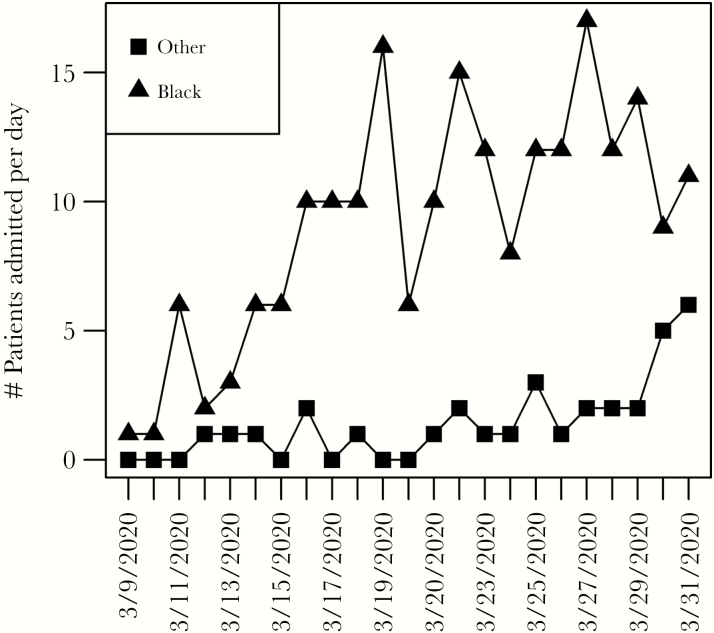
Black patients were more likely to have a diagnosis of asthma (P = .008) but less likely to have dementia (P = .002). There was no difference in the mean calculated CCI score between Black patients and other racial/ethnic group patients. Figure 1 displays the number of admissions over time and demonstrates the racially disproportionate rates of hospitalizations between Black and other racial/ethnic group patients in March 2020. Mean days from Louisiana’s first diagnosed case to time of presentation were different for Black and other racial/ethnic group patients (13.41 vs 16.19 days; P = .005) (Table 2). Mean symptom duration before presentation was 6.41 days for Black patients vs 5.88 days for other racial/ethnic group patients (P = .05). There were no racial differences in imaging findings or respiratory status, including respiratory rate and oxygen requirement, at the time of presentation. The only lab value that demonstrated a statistically significant difference was initial lactate dehydrogenase (LDH; P = .03), with higher values in Black patients compared with other racial/ethnic group patients.
Figure 1. .
Admissions over time by race.
Table 2. .
Clinical Characteristics at Presentation by Race for Patients Hospitalized With COVID-19, March 2020
| All Patients (n = 249) | Black Patients (n = 217) | Other Racial/Ethnic Group Patients (n = 32) | P Value | |
|---|---|---|---|---|
| Time since start of pandemic, mean (SD), d | 13.77 (5.66) | 13.41 (5.55) | 16.19 (5.91) | .005 |
| Symptom duration at presentation, mean (SD), d | 6.35 (8.21) | 6.41 (7.81) | 5.88 (10.69) | .050 |
| Abnormal chest x-ray | 222 (89) | 193 (89) | 29 (91) | 1.000 |
| Abnormal chest CT | 15 (6) | 13 (6) | 2 (6) | 1.000 |
| Initial O2 required | 137 (55) | 122 (56) | 15 (47) | .346 |
| D-dimer, mean (SD), ng/mL | 1816.09 (5661.56) | 1956.94 (6020.53) | 806.6 (1065.28) | .626 |
| GFR, mean (SD), mL/min | 65.69 (29.87) | 64.96 (29.98) | 70.41 (29.16) | .334 |
| Ferritin, mean (SD), ng/mL | 778.51 (1345.84) | 803.42 (1420.44) | 616.57 (682.33) | .520 |
| LDH, mean (SD), U/L | 375.79 (231.8) | 386.03 (241.29) | 298.35 (117.38) | .030 |
| CRP, mean (SD), mg/dL | 12.52 (10.81) | 12.46 (8.57) | 13 (21.11) | .089 |
| WBC, mean (SD), ×103/μL | 6.98 (3.35) | 7.03 (3.31) | 6.62 (3.59) | .173 |
| ALC, mean (SD), ×103/μL | 1.15 (1.5) | 1.17 (1.59) | 0.98 (0.57) | .453 |
| ANC, mean (SD), ×103/μL | 5.16 (2.88) | 5.18 (2.8) | 5.02 (3.43) | .265 |
| Fever at presentation (T ≥100.4°F) | 141 (56.6) | 128 (59.0) | 13 (40.6) | .575 |
| Respiratory rate, mean (SD), breaths/min | 22.77 (6.01) | 22.94 (6.13) | 21.66 (5.08) | .298 |
| Oxygen saturation on room air, mean (SD), % | 91.49 (8.93) | 91.21 (9.12) | 93.31 (7.48) | .136 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: CT, computed tomography; cGFR, glomerular filtration rate; dCRP, C-reactive protein; eWBC, white blood cell; fALC, absolute lymphocyte count; gANC, absolute neutrophil count.
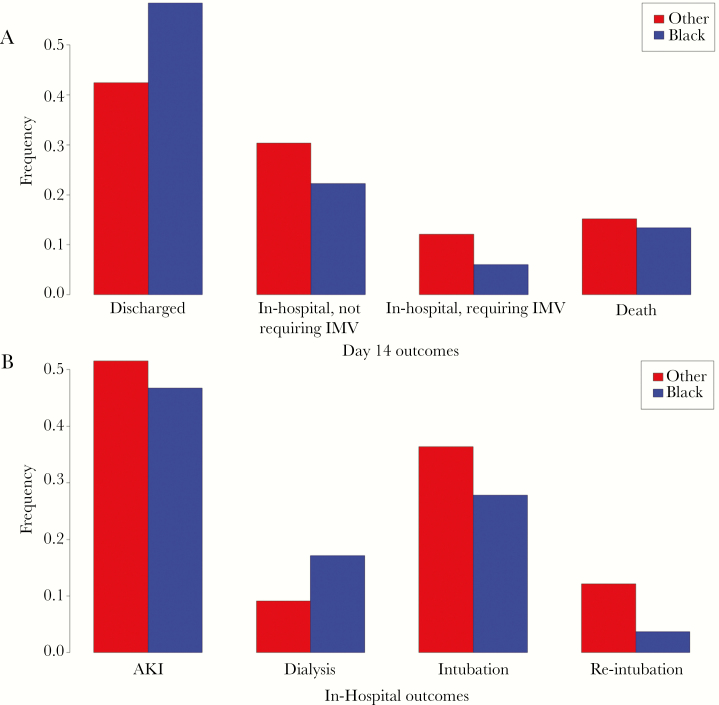
When we examined in-hospital outcomes (for all durations of follow-up), we found that Black patients had higher rates of acute kidney injury (AKI; 48.8% vs 37.5%) and requirement for dialysis (16.6% vs 12.5%) and intubation (30.0% vs 21.9%), although these rates were not statistically significant (Figure 2A). When we looked specifically at outcomes at day 14 of hospital follow-up, we found that Black patients more often were still hospitalized and less often had been discharged or had died; these rates also were not statistically significant.
Figure 2. .
A, Hospital outcomes by race over the follow-up period. B, Day 14 outcomes by race. Abbreviations: AKI, acute kidney injury; IMV, invasive mechanical ventilation.
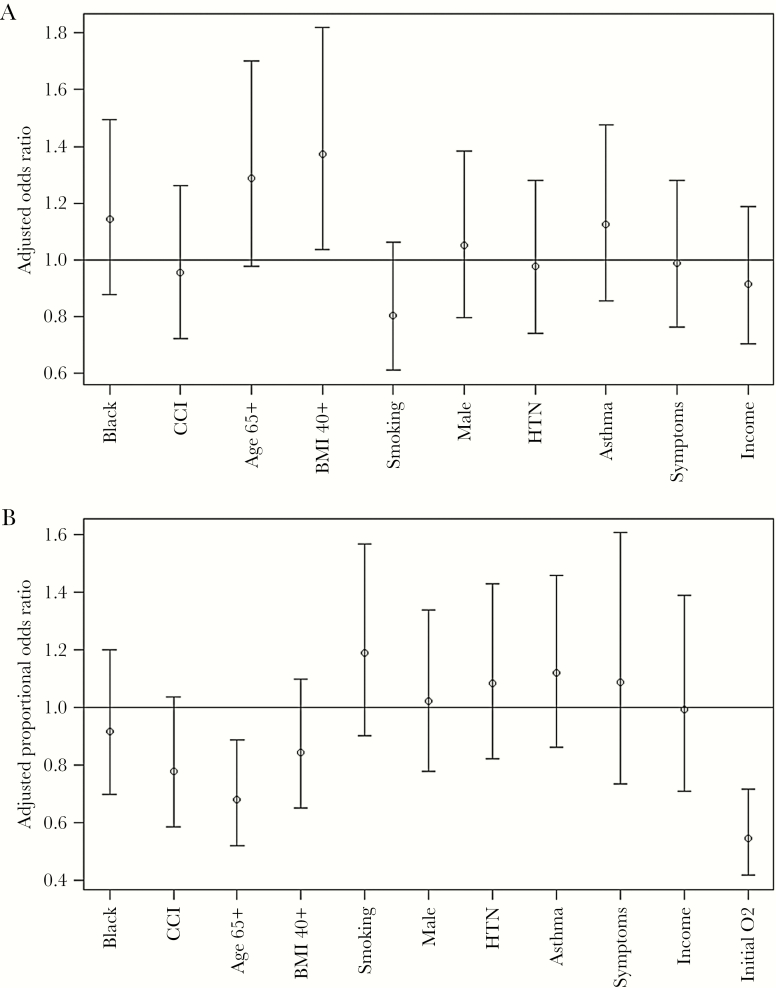
For the adjusted regression analyses, the only factor associated with increased likelihood of requiring supplemental oxygen at presentation was BMI ≥40 mg/kg2 (aOR, 1.37; 95% CI, 1.04–1.82) (Figure 3A). Race was not associated with oxygen requirement on admission (aOR, 1.15; 95% CI, 0.88–1.49). Only patient age ≥65 and initial supplemental oxygen requirement were associated with a significant shift in day 14 patient outcome scores, with both increasing the probability of poor outcomes (Figure 3B). Race was not independently associated with day 14 outcome (aPO, 0.91; 95% CI, 0.70–1.20).
Figure 3. .
A, Logistic regression for initial oxygen requirement. B, Cumulative logistic regression for ordinal day 14 outcomes. Abbreviations: BMI, body mass index; CCI, Charlson comorbidity index; HTN, hypertension .
Discussion
Our study represents the experience of an urban safety net hospital in New Orleans during a time when Louisiana was experiencing the fastest initial increase of COVID-19 cases in the world [8]. We examined all COVID-19 cases admitted to our hospital during the month of March—the 3 weeks following Louisiana’s first case—and demonstrate a rapid uptick in hospitalizations among Black patients. As compared with other racial/ethnic group patients, Black patients presented closer to the time of the first diagnosed case, and as Figure 1 demonstrates, the upward trend in the number of daily cases in other racial/ethnic group patients did not begin until the end of the month. We found that ultimately Black patients accounted for 87% of COVID-19 hospitalizations at our institution during the month of March. Similar to findings from recent publications, this was a significant overrepresentation of Black persons hospitalized at our center relative to the overall population [11, 13]. Typically, our hospital’s census is 55% Black patients [14]. Our region is represented by Orleans and Jefferson Parishes, of which Black residents comprise 60% and 28% of the population, respectively [9].
We found a statistically significant difference in the duration of symptoms before hospital presentation between Black and other racial/ethnic groups, suggesting potential barriers in access to care for Black patients. Similarly, 1 recently published study from California and another from Louisiana show that the majority of Black patients have been tested for SARS-CoV-2 in the hospital (either in the emergency department or once hospitalized) vs in primary care or urgent care clinics, which is consistent with known literature demonstrating barriers for Black patients in accessing primary care [12, 13, 15]. While Louisiana is a Medicaid Expansion state, having insurance does not mean all Louisianans have unrestricted access to primary care or unbiased care providers.
In this study, Black and other racial/ethnic group patients hospitalized with COVID-19 had few differences in comorbidities or baseline clinical status at the time of presentation to the hospital. The only racial differences in comorbidities included higher rates of asthma in Black patients and a higher rate of dementia in other racial/ethnic group patients. There was no difference in initial respiratory rate, oxygen saturation level, fever, or proportion of those with abnormal radiographic findings on chest imaging. Markers of inflammation were not significantly more elevated in Black patients relative to other racial/ethnic group patients except for venous LDH. Controlling for covariates, there was no race difference in oxygen requirement at presentation, suggesting that Black patients were not sicker or further along in their disease course at the time of presentation. We included a cumulative logistic regression for day 14 outcome, with an ordinal scale of death, requirement of mechanical ventilation, persistent hospitalization, and discharge. In this adjusted analysis, there were no proportional odds differences between Black and other racial/ethnic group patients.
The relative similarities in comorbidities and other clinical characteristics across race may inform our finding that Black patients were not more likely to have poor outcomes, despite our overall state-level data showing that Black persons are experiencing grave inequities in COVID-19 mortality. Our study demonstrates that Black patients have a greater likelihood of being exposed to SARS-CoV-2 and/or requiring hospitalization but are not at increased risk of decompensating once hospitalized. This finding amplifies findings from other recent reports of racial inequities in COVID-19, that is, disproportionate hospitalization rates but no increases in mortality once hospitalized. The increased likelihood of viral exposure and subsequent infection among Black persons observed in our study align with previous work from the H1N1 influenza pandemic; in 1 prior study, people of color were more likely to have difficulty avoiding public transportation, staying home from work, and accessing childcare separate from other children [16].
The stark reality in present-day New Orleans, LA, is that people of color are less able to implement social distancing measures due to the essential nature of their occupations on the front lines, for example, in service or health care industries [17]. Furthermore, challenges exist with respect to quarantining because of shared households and increased housing density [18]. In recent months, our team has observed many cases of COVID-19 in family members hospitalized simultaneously. These challenges can in part be attributed to residential segregation, a foundation of structural and institutional racism [16]. As a community loses its ability to secure housing, impact on future generations is felt with inequities in educational opportunities and future employment options. These inequities are at the forefront of the COVID-19 outbreak in Orleans and Jefferson Parishes and highlight the need for further exploration of the health burden of residential segregation [16].
Direct efforts to decrease exposure among Black persons in Louisiana may alleviate the inequities currently observed with COVID-19. Louisiana has implemented a COVID-19 Health Equity Task Force to better understand and interpret public health data, improve access to testing and quality care for all communities, and ensure that reopening of the state occurs in a way that does not exacerbate health disparities [19]. Crucial to this effort will be integrating resource coordination and social support measures with contact tracing efforts. Members of marginalized communities face considerable barriers in their ability to safely and practically isolate or quarantine at home. Direct food or grocery assistance, income replacement, and childcare assistance can reasonably increase one’s likelihood of successful isolation or quarantine periods. In other circumstances, individuals may require alternative temporary housing to avoid undue exposure to family members. Investments in such social supportive measures will serve to decrease community spread of virus and limit the undue impact of this outbreak on individuals and families at risk for continued disparate burden of disease in this pandemic. In addition to public health initiatives to counter structural and institutional racism, multisector partnerships and a community-driven effort are also needed [20].
This study has several limitations. First, this was a retrospective analysis subject to the shortcomings of chart review; however, 1 advantage is collection of information with a greater degree of detail (eg, days since symptom onset) that is not available with electronic abstraction of structured data elements. Second, although this study reveals our hospital’s unique experience as a large, urban, safety net hospital, this is a single-center study that does not represent the entire New Orleans or Louisiana experience of COVID-19 hospitalizations. Third, while we do have 14 days of follow-up on all patients, we were only able to access data for readmissions within our hospital system, so the results may not truly reflect hospital outcomes if patients were readmitted outside of our health care network. Fourth, we used income by ZIP code, as we did not have individual patient income, which would have been more accurate. Finally, the comparator group is not ideal in combining multiple races and ethnicities but was relatively small, a direct reflection of COVID-19 epidemiology in New Orleans, in which Black patients were disproportionately affected.
Conclusions
We present the data of hospitalized patients in March 2020 who tested positive for SARS-CoV-2 at a tertiary care academic medical center located in New Orleans and an analysis of clinical characteristics and outcomes by race. Our results indicate that, among patients hospitalized at the beginning of the COVID-19 outbreak in New Orleans, LA, there were minimal racial differences in rates of comorbidities or severity of disease at the time of presentation. Similarly, and unique to our analysis, day 14 overall outcomes were not different for Black and other racial/ethnic group patients. However, Black patients were disproportionately represented in hospitalizations, a similar finding to data recently emerging from other Southern cohorts. Our findings suggest that Black patients have a greater likelihood of being infected with SARS-CoV-2, and we propose that mitigating inequities with respect to race should start with limiting viral exposure and transmission in this population.
Acknowledgments
The authors would like to acknowledge Dr. Benjamin Springgate, MD, MPH, for his guidance and input.
Financial support. This work was supported by the National Institutes of Allergy and Infectious Diseases (K23AI137121 to M.E.C.).
Potential conflicts of interest. M.E.C. reports the following financial disclosures: research grants to institution: Janssen; consultancy fees: FHI360. None of the other authors have conflicts to declare. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Centers for Disease Control and Prevention. Cases in the U.S. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed 5 June 2020.
- 2.Department of Health, State of Louisiana. Louisiana coronavirus COVID-19. Available at: http://ldh.la.gov/coronavirus/. Accessed 5 June 2020.
- 3.Georgia Department of Public Health. COVID-19 status report. Available at: https://dph.georgia.gov/covid-19-daily-status-report. Accessed 5 June 2020.
- 4. Millett GA, Jones AT, Benkeser D, et al. . Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020; 47:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johns Hopkins Coronavirus Resource Center. Maps & trends. Available at: https://coronavirus.jhu.edu/data. Accessed 5 June 2020.
- 6.Office of Governor John Bel Edwards. Gov. Edwards confirms Louisiana’s first presumptive positive case of COVID-19. Available at: https://gov.louisiana.gov/index.cfm/newsroom/detail/2392. Accessed 5 June 2020.
- 7.Department of Health, State of Louisiana. Coronavirus COVID-19 resources. Available at: http://ldh.la.gov/index.cfm/page/3878. Accessed 5 June 2020.
- 8.Centers for Disease Control and Prevention. Provisional death counts for coronavirus disease (COVID-19). Published 5 June 2020. Available at: https://www.cdc.gov/nchs/nvss/vsrr/covid19/index.htm. Accessed 5 June 2020.
- 9.US Census Bureau. US Census Bureau QuickFacts: Louisiana; United States. Available at: https://www.census.gov/quickfacts/fact/table/LA,US/PST045219. Accessed 5 June 2020.
- 10. Gold JAW, Wong KK, Szablewski CM, et al. . Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep 2020; 69:545–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Azar KMJ, Shen Z, Romanelli RJ, et al. . Disparities in outcomes among COVID-19 patients in a large health care system in California: study examines disparities in access and outcomes for COVID-19 patients who are members of racial and ethnic minorities and socioeconomically disadvantaged groups. Health Aff (Millwood). 2020; 39(7):1253–62. [DOI] [PubMed] [Google Scholar]
- 12. Massachusetts Medical Society. COVID-19. Available at: http://www.massmed.org/covid-19/#.Xtq1V2g3nMU. Accessed 5 June 2020.
- 13. Jyotsna Fuloria MD. Available at: https://www.umcno.org/physician-directory/jyotsna-fuloria-md/. Accessed 5 June 2020.
- 14. Quinn SC, Kumar S, Freimuth VS, et al. . Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health 2011; 101:285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wisniewski JM, Walker B. Association of simulated patient race/ethnicity with scheduling of primary care appointments. JAMA Netw Open 2020; 3:e1920010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bailey ZD, Krieger N, Agénor M, et al. . Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017; 389:1453–63. [DOI] [PubMed] [Google Scholar]
- 17.The Data Center. Who are the essential workers keeping the New Orleans region going? Available at: https://www.datacenterresearch.org/reports_analysis/who-are-the-essential-workers-keeping-the-new-orleans-region-going/. Accessed 7 June 2020.
- 18.The Data Center. Demographics of New Orleans and early COVID-19 hot spots in the U.S. Available at: https://www.datacenterresearch.org/covid-19-data-and-information/demographic-data/. Accessed 7 June 2020.
- 19.Office of Governor John Bel Edwards. Gov. Edwards announces creation of COVID-19 Health Equity Task Force. Available at: https://gov.louisiana.gov/index.cfm/newsroom/detail/2457. Accessed 5 June 2020.
- 20. Reskin B. The race discrimination system. Annu Rev Sociol 2012; 38:17–35. [Google Scholar]