In March 2018, Prime Minister Narendra Modi declared that India would achieve tuberculosis (TB) elimination by 2025, 5 years ahead of the global targets, which seemed unrealistic.1 Nonetheless, this gave an impetus to all sectors to escalate their efforts towards TB control.
In December 2019, in order to address the goal of TB elimination, a pilot project was started under the Mission TB Free Haryana,2,3 which is a unique public–private partnership (PPP) model led by a tertiary hospital funded by corporate social responsibility (CSR) funds of the hospital. The aim of this project was to develop a model of care to render a block TB free. The block is a contained unit with a few hundred thousand people, more amenable to an intervention to demonstrate robust methodology and impact and as a proof of concept rather than a district, which can be too large, heterogeneous and unwieldy. In this study, simultaneous house-to-house active case finding (ACF) and point-of-care (POC) mobile diagnostic services (digital chest X-ray [CXR] and cartridge-based nucleic acid amplification test [CBNAAT]) were offered to the entire population of the block to find all existing cases of TB in the community. In doing so, we intended to develop a scalable replicable TB Free model. All presumptive TB cases (cough ≥2 weeks) were offered digital CXR. Those with high clinicoradiological suspicion were tested with GeneXpert Edge (Cepheid, Sunnyvale, CA, USA) for microbiological confirmation and initiated on treatment on the same day, if found positive. This substantially reduced attrition. This initiative was supported by the Central TB Division and the state and district National TB Elimination Program (NTEP). The project ran from December 2019 through mid-March 2020.
On 22 March 2020, the country implemented a nationwide lockdown due to the coronavirus disease 2019 (COVID-19) pandemic. This social curfew has disrupted people's lives, most importantly routine healthcare services, apart from other economic and business activities. The pilot project also succumbed to the constrained healthcare system as a result of the pandemic and has been halted since then. It had a major impact on the TB control activities reflected in the TB case notifications prior to and after lockdown.
The TB Free block project was implemented in the Pataudi block (population of 342 000 living in 142 villages), District Gurgaon, a block that is partly urban and partly rural (agricultural). A total of 31 951 households were covered: 1302 were referred for diagnostic camps, 120 CXRs were suggestive of TB and 42 had a positive CBNAAT. The program had to stop abruptly when the lockdown in India started on 22 March. The program data for case notification of TB during the period November 2019–May 2020 were extracted and comparison was done during the same period in previous years (2017–18 and 2018–19). Another comparison was also done prior to (November 2019–February 2020) and after (March–May 2020) COVID-19 lockdown. Chi-square for trend has been reported. The data presented in this study came from the records routinely maintained by the TB control program and from the same block where the TB Free block project was implemented.
The project started in December 2019 and witnessed a sharp increase in TB case notification in the subsequent months of January and February 2020, significantly above (p<0.001) the figures during the same months in the previous 2 years. This was followed by a sharp decline (p for trend<0.001) during the period March–May 2020 (COVID-19 lockdown period), decreasing to 19 in May 2020. This decline is in sharp contrast to the number of TB notifications during the period March–May in the previous 2 years (Figure 1). The decline in notification started in March, even though the lockdown was implemented on 22 March, as by then there were already >350 cases of COVID-19 and several COVID-related deaths in the country. So even before the lockdown, the COVID-19 pandemic might have impacted on-field TB case finding activities.
Figure 1.
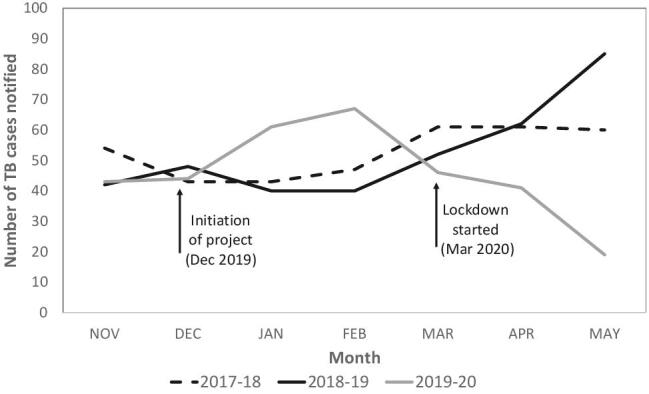
Comparison of the trends in TB case notifications in the Pataudi block, Haryana, from March to May during the period 2017–2020.
The TB Free model led to a significant increase in case notifications and demonstrated a scalable TB Free model in the fight towards eliminating TB. This PPP model provided access to digital CXR and POC microbiological confirmation in remote rural areas employing local human resources. As expansion of this model was being planned to other blocks, the COVID-19 pandemic halted the project.
The post-pandemic dip in TB case notifications is a major concern. This was due to the stoppage of active case finding under the project and a complete halt to the routine TB program activities in the block due to the lockdown. This means that we are missing a lot of TB cases, although it is reassuring that reduced social contacts during the pandemic reduces transmission of the disease. Despite social distancing measures, modelling exercises have predicted a surge in TB cases and deaths post-COVID-19 in India.4,5 We must ensure quick resumption of TB control services, even during the lockdown. Supplementary ‘catch-up’ TB case detection and treatment should be carried out. The Ministry of Health has directed all health facilities under the NTEP to provide uninterrupted TB screening, diagnostic and treatment services. However, it is very important to ensure adequate infection control measures, such as the use of masks and sanitizers, cough etiquette, safe disposal of sputum and daily disinfection of surfaces. The ministry has also recommended provision of anti-TB drugs for 1 month to all TB patients, treatment monitoring via telephone/video calls and screening for new-onset fever, cough or breathlessness. TB patients who do not turn up for TB treatment initiation/continuation due to the lockdown should be line listed. A treatment supervisor/supporter should contact the patient and initiate treatment, following adequate precautions. More importantly, we need to alleviate all apprehensions among healthcare workers regarding risks of contracting COVID-19 and their financial insecurity. The government has already ensured the timely release of salaries to all contractual program staff. This is a welcome move.
The TB Free project is one of the largest and most robust CSR programs of any organization and definitely of any corporate hospital in the region, however, the future of the project is at risk. Due to the near stoppage of all non-pandemic healthcare activities during the lockdown and the blow to hospital revenue, the CSR fund is at risk and all programs linked to it stand abandoned. Worldwide, there is disruption to key national health programs. Similar disruptions of health services and declines in the utilisation of most programmes, including maternal and child health, TB, human immunodeficiency virus, immunization, malnutrition and non-communicable diseases, was observed during the Ebola outbreak in Africa.6 A significant decline in access to TB testing and diagnosis has also been reported during the fight against COVID-19 in Taiwan and South Africa.7,8
On the brighter side, there were some important lessons learned from this ACF activity under the TB Free block project that probably contributed to the increase in notifications. First, ACF typically carried out in daytime hours only captured women, as the men were out working and children were at school. The timing was changed and ACF was also carried out during evenings and Sundays. Second, low initial yield of spot sputum for GeneXpert increased significantly when early morning sputum was taken. While that would go against the principle of POC testing and diagnosis as envisioned in this project, health workers could track these patients, being in a defined area, and thus prevent any loss to follow-up. Third, presumptive TB patients referred on the same day for CXR reduced attrition.
A newer competing epidemic has impacted the existing TB epidemic in terms of funding, resource channelization and human resource allocation. The existing TB program and associated field activities should continue now that the process of unlocking has started. The program needs to find an integrated approach to address the needs of the competing threat rather than be submerged in the inevitable surge of a second epidemic, that of TB. With 16 COVID-19 cases in the block, can we afford to miss and neglect so many TB patients?
Acknowledgements
None.
Contributor Information
Bornali Datta, Department of Respiratory Medicine, Medanta the Medicity, Gurgaon, Haryana, India.
Anand Jaiswal, Department of Respiratory Medicine, Medanta the Medicity, Gurgaon, Haryana, India.
Pinky Goyal, Department of Respiratory Medicine, Medanta the Medicity, Gurgaon, Haryana, India.
Ashish Prakash, Department of Respiratory Medicine, Medanta the Medicity, Gurgaon, Haryana, India.
Jaya Prasad Tripathy, Department of Community Medicine, All India Institute of Medical Sciences, Nagpur, India.
Naresh Trehan, Medanta the Medicity, Gurgaon, Haryana, India.
Author's contributions
BD, AJ and NT were involved in conception of the idea, project planning and implementation, critical review of the manuscript and finalization of the manuscript. JPT was involved in conception of the idea, data collection and analysis, drafting of the manuscript and editing and finalization of the manuscript. PG and AP were involved in data collection, critical review of the manuscript and finalization of the manuscript. All the authors gave their approval to the final submitted version of the manuscript.
Funding
The study was funded by Medanta Hospital's Corporate Social Responsibility Fund. The funder had no role in the design of the study; collection, analysis and interpretation of data; or drafting the manuscript.
Competing interests
None declared.
Ethical approval
Ethical approval was obtained from the Ethics Review Committee of Medanta Hospital, Gurugram, Haryana. Administrative approval was obtained from the State TB Program, Haryana.
References
- 1. Revised National Tuberculosis Control Programme. National strategic plan for TB elimination in India (2017–2025) New Delhi: Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare;2017. [Google Scholar]
- 2. Datta B, Prakash A, Ford D et al.. Implementing upfront mobile digital chest x-ray for tuberculosis diagnosis in India–feasibility and benefits. Trans R Soc Trop Med Hyg. 2020;114(7):499–505. [DOI] [PubMed] [Google Scholar]
- 3. Ford D, Datta B, Prakash AK et al.. Fifth year of a public-private partnership to improve the case detection of tuberculosis in India: a role model for future action? Indian J Tuberc. 2019;66(4):480–6. [DOI] [PubMed] [Google Scholar]
- 4. Cilloni L, Fu H, Vesga JF et al.. The potential impact of the COVID-19 pandemic on tuberculosis: a modelling analysis. medRxiv. 2020; 10.1101/2020.05.16.20104075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McQuaid CF, McCreesh N, Read JM et al.. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur Respir J. 2020; 10.1183/13993003.01718-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Decroo T, Fitzpatrick G, Amone J. What was the effect of the West African Ebola outbreak on health programme performance, and did programmes recover? Public Health Action. 2017;7(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute for Communicable Diseases Impact of COVID-19 intervention on TB testing in South Africa. Johannesburg: National Institute for Communicable Diseases; 2020. [Google Scholar]
- 8. Lai C-C, Yu W-L.. The COVID-19 pandemic and tuberculosis in Taiwan. J Infect. 2020;81(2):e159–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


