Summary
Background
Under the unique Japanese policy to restrict reverse transcriptase–polymerase chain reaction (RT-PCR) testing against severe acute respiratory syndrome coronavirus 2, a nationwide number of its confirmed cases and mortality remains to be low. Yet the information is lacking on geographical differences of these measures and their associated factors.
Aim
Evaluation of prefecture-based geographical differences and associated predictors for the incidence and number of RT-PCR tests for coronavirus disease 2019 (COVID-19).
Design
Cross-sectional study using regression and correlation analysis.
Methods
We retrieved domestic laboratory-confirmed cases, deaths and the number of RT-PCR testing for COVID-19 from 15 January to 6 April 2020 in 47 prefectures in Japan, using publicly available data by the Ministry of Health, Labour and Welfare. We did descriptive analyses of these three measures and identified significant predictors for the incidence and RT-PCR testing through multiple regression analyses and correlates with the number of deaths through correlation analysis.
Results
The median prefectural-level incidence and number of RT-PCR testing per 100 000 population were 1.14 and 38.6, respectively. Multiple regression analyses revealed that significant predictors for the incidence were prefectural-level population (P < 0.001) and the number of RT-PCR testing (P = 0.03); and those for RT-PCR testing were the incidence (P = 0.025), available beds (P = 0.045) and cluster infections (P = 0.034).
Conclusion
Considering bidirectional association between the incidence and RT-PCR testing, there may have been an underdiagnosed population for the infection. The restraint policy for RT-PCR testing should be revisited to meet the increasing demand under the COVID-19 epidemic.
Introduction
Since the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China erupted in late-2019, infection with the causative virus of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has rapidly become a significant problem worldwide.1 During the last several months of the global response to COVID-19, it has been increasingly understood that SARS-CoV-2 has spread partly via mild symptoms and an asymptomatic population.2 Further, COVID-19 has a relatively long incubation period among symptomatic patients.3 This means that alongside rigorous social distancing, a liberal performance of RT-PCR testing is essential to prevent the SARS-CoV-2 from spreading, which has been gaining an increasing popularity for the response against COVID-19 globally.4 However, such liberal approach is not accepted and remains controversial in some countries including Japan, in which a restrictive performance of RT-PCR testing has been conducted mainly for severe patients with COVID-19.5
In this context, a case study of the Japanese response would provide significant insight toward a strategy for RT-PCR testing. In Japan, the first case was detected as early as mid-January 2020, but the epidemic curve was not steep compared with that of other countries, such as Italy, South Korea, the USA and Iran as of April 2020.6,7 It has been increasingly speculated that this has been caused by the Japanese central government’s policy to restrict the provision of RT-PCR testing for this SARS-CoV-2.8,9 Alternatively, Japan has focused on testing for cluster infections of SARS-CoV-2 as a proactive epidemiological investigation, and indeed the testing provision remains moderate (1000–2000 per day nationwide in late March 2020).10 In this strategy, upon request from attending clinicians, bureaucrats in a local governmental healthcare center give their decision to perform any test at their discretion based on the restrictive guidelines of the central government. However, it has been reported that such requests from clinicians frequently result in rejection, and thus it is reasonable to speculate that testing number would be small and differ among regions.
Japan is composed of 47 administrative districts (prefectures), covering an area of 377 900 km2 and a population of 126.8 million.10 Although the population density and human flow vary substantially in each prefecture, ranging from densely populated metropolis like Tokyo to depopulating rural areas, contributing factors related to geographical differences in the incidence and mortality of COVID-19 and the provision of RT-PCR testing in each prefecture remain unknown.
In this study, it was primarily aimed to evaluate geographical differences in incidences, number of deaths and RT-PCR testing with regard to the COVID-19. Additionally, the associated predictors were investigated for geographical differences through multiple regression analyses concerning the incidence and RT-PCR testing for COVID-19 and correlates with deaths through correlation analysis using the demographic and geographic data for each prefecture.
Methods
Study settings and data collection
Domestic laboratory-confirmed COVID-19 cases and the total numbers of RT-PCR testing conducted from 15 January 2020 (the day when the first case of COVID-19 in Japan was documented in the governmental report) to 6 April 2020, were collected in 47 prefectures in Japan, using publicly available data from the Ministry of Health, Labour and Welfare (MHLW). The MHLW initiated the RT-PCR testing using the prototype testing kit from 14 January 2020, and the development of RT-PCR testing was completed on 21 January 2020.10
In the publicly available data, the number of RT-PCR tests included both positive and negative cases, while the number of cases tested for a follow-up (e.g. confirmation of negativity for hospitalized patients before discharge) were not included. Domestically identified cases only were included, whereas, charter flights returnees from Wuhan, China and those quarantined on a cruise ship ‘Diamond Princess’ docked in Yokohama were excluded, as the aim was to focus solely on cross-prefecture comparisons.
Using the population of each prefecture as of 2018 published by Japan’s Statistics Bureau,11 the number of physicians, nurses, COVID-19 patients and the number of RT-PCR testing per population were calculated in each prefecture. In addition, the number of available beds was obtained for specific infectious diseases, including COVID-19, which are legally categorized as Type 2 in the Japanese classification, in each prefecture from the MHLW data as of 6 April. Based on the data published by prefectural governments, the number of deaths due to COVID-19 for each prefecture was obtained as of 6 April. Further, the number of cluster infections were obtained, defined in the MHLW report as of 31 March 2020, in each prefecture.
In addition, to take into account the influence of foreign visitors, Chinese visitors and US military facilities were accounted; the number of Chinese visitors in each prefecture using the data published by the Ministry of Land, Infrastructure, Transport and Tourism; the numbers of US Force Japan facilities using publicly available information released by the Defense Agency in each prefecture.
Data analysis
Data were first screened for outliers, which were identified using the outlier labeling rule,12 then winsorized.13 All variables were not normally distributed (Shapiro–Wilk’s test, P < 0.05); thus, the data were square-root-transformed to satisfy the assumption of normality.14 Multiple regression analyses were conducted to identify significant predictors for the number of patients as the outcome variable.
Firstly, none of the variables were significant predictors for the number of patients when all seven variables were considered; including the number of deaths, population, the number of patients, available beds, the number of clusters, Chinese visitors and US Force Japan facilities. After excluding variables that were less relevant, four predictor variables were used in the final model; including population, the number of available beds, the number of RT-PCR tests and the number of clusters. Multicollinearity was of no concern Variance Inflation Factors (VIFs < 10).
Second, the contributing factors to the number of RT-PCR tests were analyzed. We hypothesized that five predictor variables for the number of RT-PCR tests were the outcome variables, including the number of deaths, population, number of patients, available beds and clusters. Multicollinearity was of no concern (VIFs < 10). Tests were done to assess whether the number of doctors, nurses, Chinese visitors and US Force Japan facilities would predict the number of RT-PCR tests, although none of these variables did not predict the outcome significantly.
Lastly, Pearson’s correlation was used to identify correlates with deaths. Five predictors were considered to explore relationships with deaths: population, the number of patients, the number of RT-PCR tests, the number of available beds and the number of clusters.
Results
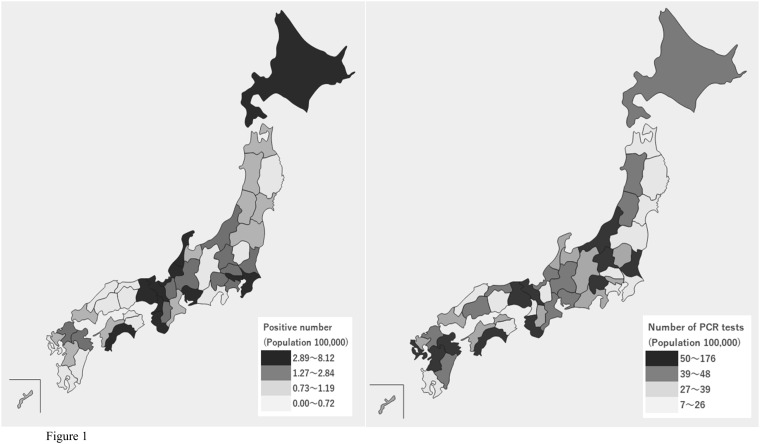
During the study period, a total of 3817 test positive COVID-19 cases were reported, with an incidence of 3.0 per 100 000 population throughout Japan (median, 1.138; interquartile range [IQR] 0.70–2.82). Similarly, the total number of RT-PCR tests was 48 357, and the median number of RT-PCR testing per 100 000 population was 38.6 (IQR 25.4–48.1). Figure 1 shows the number of cases of COVID-19 and RT-PCR testing per 100 000 population in each prefecture. The incidence of COVID-19 tended to be higher in prefectures with large cities (e.g. Tokyo and Osaka). There was no apparent association between the size of cities and the number of RT-PCR tests per population. Details of the numbers of each variable in each prefecture are available in Supplementary Tables S1 and S2.
Figure 1.
Number of COVID-19 patients and RT-PCR testing per 100 000 population in each prefecture.
Table 1 shows multiple regressions predicting the number of patients in each prefecture. The four predictor variables accounted for 80% (adjusted R2) of the variance for the number of patients, indicating a large effect size.15 Population (P < 0.001) and the number of RT-PCR tests (P = 0.03) were significant positive predictors for the number of patients. The number of clusters was not significant (P = 0.054). Table 2 shows multiple regression analysis predicting the number of RT-PCR tests in each prefecture. The five predictor variables accounted for 74% (adjusted R2) of the variance for the number of RT-PCR tests, indicating a large effect size.15 The number of patients (P = 0.025), clusters (P = 0.034) and available beds (P = 0.045) were significant positive predictors.
Table 1.
Multiple regression predicting the number of COVID-19 patients in each prefecture
| Predictor variables | B | SEB | β | CI for B (lower, upper) |
|---|---|---|---|---|
| Population | 1.47* | 0.30 | 0.69 | 0.86, 2.08 |
| Number of available beds | −0.60 | 0.34 | −0.24 | −1.28, 0.07 |
| Number of RT-PCR testing | 0.09** | 0.04 | 0.29 | 0.01, 0.17 |
| Number of clusters | 1.22 | 0.62 | 0.20 | −0.02, 2.46 |
| Adjusted R2 | 0.80 | |||
B, unstandardized regression coefficient; SEB, standard error of the coefficient, β standardized coefficient; CI, confidence interval.
P < 0.01.
P < 0.05.
Table 2.
Multiple regression predicting the RT-PCR testing of patients in each prefecture
| Predictor variables | B | SEB | β | CI for B (lower, upper) |
|---|---|---|---|---|
| Deaths | −1.51 | 2.28 | −0.09 | −6.11, 3.09 |
| Population | 0.48 | 1.42 | 0.07 | −2.39, 3.35 |
| Number of patients | 1.39* | 0.60 | 0.42 | 0.19, 2.60 |
| Number of available beds | 2.61* | 1.26 | 0.31 | 0.06, 5.16 |
| Number of clusters | 5.20* | 2.37 | 0.26 | 0.42, 9.99 |
| Adjusted R2 | 0.74 | |||
B, unstandardized regression coefficient; SEB, standard error of the coefficient, β standardized coefficient; CI, confidence interval.
P < 0.05.
Table 3 shows correlation analysis identifying significant correlates with deaths; all variables were significant including, population, number of patients, tests, available beds and clusters (P < 0.01). Among them, the number of patients (r = 0.80), population (r = 0.73) and number of clusters (r = 0.70) were strongly associated with the number of deaths.
Table 3.
Correlation analysis with regards to deaths.
| Deaths | |
|---|---|
| Population | 0.73* |
| Number of patients | 0.80* |
| Number of RT-PCR testing | 0.69* |
| Number of available beds | 0.67* |
| Number of clusters | 0.70* |
P < 0.01.
Discussion
As new data about COVID-19 are being released day by day, we aimed to give a timely report for COVID-19 by analyzing publicly available data with regard to COVID-19 throughout Japan, which will help better understand the regional differences in the COVID-19 situation. As of 6 April 2020, population and number of RT-PCR tests were significantly associated with the increased incidence of COVID-19 in 47 prefectures. In addition, the deaths due to COVID-19 were significantly associated with various analyzed factors, including the population and the number of clusters, alongside the incidence and RT-PCR tests. Given that Japan has adopted a unique policy to restrict the number of RT-PCR testing, these findings would provide important lessons to a strategy to counteract the spread of emerging infectious diseases, including and beyond the case of the COVID-19.
These results are reasonable because residents in densely populated prefectures, such as Tokyo and Osaka, would have numerous opportunities to contract COVID-19 due to limited social distancing, and an increased number of patients would lead to an increased number of deaths. Of note, the fact that the increased number of RT-PCR tests led to more detection suggests the presence of numerous underdiagnosed patients under Japan’s constrained policy for RT-PCR testing.
The number of RT-PCR was, in fact, lower in Japan than in other countries; as of April 6, the number of RT-PCR testing per 100 000 in Italy, Korea, and the USA was more than 1200, 900 and 500, respectively, while, that of Japan was as low as 38 as shown in this study.16 RT-PCR testing has not been sufficiently provided to citizens in need under the policy of prioritizing RT-PCR testing to severe cases, leading to a significant concern that Japan’s official statistics underestimate the actual case number of COVID-19.
It was found that there were wide differences in the number of RT-PCR tests among prefectures, and it was significantly associated with the number of COVID-19 patients, clusters and available beds. This would reflect a unique policy that the Japanese government has prioritized to perform RT-PCR testing for finding clusters of COVID-19 patients and related individuals who had close contact with the patients by the special projects team of the government. Although the number of available beds predicted the number of RT-PCR, given that medical institutions with such beds tend to be present in large cities, there may be confounding factors affecting the finding.
Of note, among the 47 prefectures, Wakayama prefecture had the highest number of RT-PCR testing per population (175.6 testing per 100 000), possibly because the local governor adopted a liberal and aggressive RT-PCR testing policy contrary to the central government, and it has succeeded in containment as of early April 2020. On the other hand, the prefectures with dense cities such as Tokyo and Osaka (32.0 and 19.9 testing per 100 000, respectively) were not able to implement such an aggressive policy for RT-PCR testing, and subsequently, the number of patients is rapidly increasing, although other factors may also explain the phenomenon.
In April 2020, the number of COVID-19 patients has continued to increase in Japan, but it is not clear whether the infection has been spreading or it is just because the government has gradually changed the policy to increase the number of RT-PCR testing to find more undiagnosed cases. Actually, some institutions have started screening of individuals without definite symptoms related to COVID-19 using RT-PCR or serological testing and found 3–6% of them could have already been exposed to SARS-CoV-2, suggesting the presence of much higher number of undiagnosed populations.17 Given that extensive RT-PCR testing for a wider population has gradually become a consensus in containing the disease worldwide, the restricting policy for testing in Japan can be considered suboptimal.
Limitations
Several limitations are present in this study. There were other factors that could not be evaluated in the multiple regression analysis, such as access to medical care, therapeutic drugs, other diseases like influenza, detailed situations of human flow domestically and internationally, ventilators and intensive care unit beds. In addition, as there were only 80 deaths associated with COVID-19 at the time of our analysis, these findings should be interpreted with caution.
Conclusion
In this study, it was primarily shown that the prefectural-level incidence and RT-PCR testing were low, and the large geographical differences in the incidence and deaths of COVID-19 and the provision of RT-PCR testing with their predictive factors in Japan. Although the incidence of COVID-19 remained low, it should be interpreted with caution since the prefectural-level number of RT-PCR testing was much smaller than that of other countries facing similar situations. The bidirectional association between the number of patients and RT-PCR may have suggested the presence of underdiagnosed patients, and it is necessary to increase the capacity of the RT-PCR testing to meet its growing demand in the country.
Supplementary material
Supplementary material is available at QJMED online.
Supplementary Material
Acknowledgments
We would like to thank Ms. Erika Yamashita and Dr. Masahiro Kami for their constructive opinions. We would like to thank Editage (www.editage.com) for English language editing.
Funding
None declared.
Conflict of interest. A.O. and T.T. receive personal fees from Medical Network Systems (MNES) Inc., outside the submitted work. The other authors have no conflict of interest to declare.
References
- 1.Coronavirus disease (COVID-19) outbreak. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (30 April 2020, date last accessed).
- 2. Aguilar JB, Faust JS, Westafer LM, Gutierrez JB. Investigating the impact of asymptomatic carriers on COVID-19 transmission. medRxiv 2020. 10.1101/2020.03.18.20037994 (30 April 2020, date last accessed). [DOI]
- 3. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med2020; 172(9):577–582. [DOI] [PMC free article] [PubMed]
- 4.WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–16 March 2020 Geneve: World Health Organization, 2020.
- 5.Testing for COVID-19: A Way to Lift Confinement Restrictions—28 April 2020. Paris: Organization for Economic Co-Operation and Development, 2020. https://read.oecd-ilibrary.org/view/?ref=129_129658-l62d7lr66u&title=Testing-for-COVID-19-A-way-to-lift-confinement-restrictions (30 April 2020, date last accessed).
- 6. Osumi M. Will Japan’s Virus Testing Policy be Enough to Flatten the Curve? Tokyo: Japan Times, 2020.
- 7. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD.. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020; 395:931–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dooley B, Rich M, Inoue M.. In Graying Japan, Many Are Vulnerable But Few Are Being Tested Tokyo: New York Times, 2020.
- 9. Normile D. Did Japan miss its chance to keep the coronavirus in check? Science2020. https://www.sciencemag.org/news/2020/04/did-japan-miss-its-chance-keep-coronavirus-check (30 April 2020, date last accessed).
- 10.About Novel Coronavirus Infection (In Japanese). 2020. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00001.html (22 April 2020, date last accessed).
- 11.Statistics of Japan. https://www.e-stat.go.jp/en (30 April 2020, date last accessed).
- 12. Hoaglin DC, Iglewicz B.. Fine-tuning some resistant rules for outlier labeling. J Am Stat Assoc 1987; 82:1147–9. [Google Scholar]
- 13. Tukey JW. The future of data analysis. Ann Math Stat 1962; 33:1–67. [Google Scholar]
- 14. Field A. Discovering Statistics Using IBM SPSS Statistics, 5th edn London, UK: Sage, 2018. [Google Scholar]
- 15. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 16.Total Tests for COVID-19 per 1,000 People. https://ourworldindata.org/grapher/full-list-cumulative-total-tests-per-thousand (30 April 2020, date last accessed).
- 17. Takita M Matsumura T Yamamoto K Yamashita E Hosoda K Hamaki T,. et al. Challenges of community point-of-care antibody testing for COVID-19 herd-immunity in Japan. QJM. 2020; https://doi.org/10.1093/qjmed/hcaa182 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.