Since March 2020, lockdowns due to COVID-19 have confined around 3 billion people to their homes worldwide. Assessment of the potential psychological effects—post-traumatic stress symptoms, anxiety, depression, sleep disorders—is urgently needed, with a better understanding of the stressors promoting them [1].
Stressors may include quarantine duration (more than 2 months for COVID-19), infection fears, financial problems, and increased broadcast/internet media exposure (ME) [2]. Media, whose audience has drastically increased during the lockdown [3], relay official public-health recommendations to protect the population but also convey potentially traumatic content—dramatic, even frightening images and information. This unprecedented lockdown may make it difficult for vulnerable individuals to find activities—physical, work-related, social, cultural—to counterbalance the media’s pervasive influence. Good sleep is crucial for coping with stressful situations and strengthening immune defense against infections. We investigated whether media overexposure was associated with sleeping disorders during the lockdown.
When the lockdown began (March 17, 2020), we set up the COCONEL project (Appendix) to acquire weekly information about the French population’s reactions to it. Four weeks later, between April 15 and April 17, 2020, a cross-sectional online survey of 1,005 adults representative of the French population (aged 18+) asked about self-reported exposure to media and sleep problems. We investigated sleep problems using items of the French Health Barometer [4], we adapted partially to the COVID-19 period, with the following three items: Q1: Did you have sleep problems during the last 8 days: (a) not at all, (b) few, (c) a lot? If Q1 (b) or (c) Q2: Did they increase since the lockdown: (a) Yes, a lot; (b) Yes, a little; (c) not, really; (d) Not at all. If Q1 (b) or (c) Q3: Did these sleep problems and the resulted fatigue had an impact on your daily activities (work or leisure): (a) Not at all, (b) a little, (c) a lot? Q4: During the last 12 months, did you take sleeping pills or drugs for sleep: (a) yes, (b) no, (c) do not know? If Q4 (a) Q5: Was it before or after the lockdown? Q1 and Q3 are items of the French Health Barometer [4] that we used since two decades, and came from the Duke Health profile [5]. We added Q2 to assess whether sleep problems had worsened during the lockdown.
We also considered as a “severe” group, those who claimed of lot of sleep problems with daytime impairment and/or sleeping pills use increased since the lockdown.
We also built two scores to measure ME and fear due to media exposure FME.
The ME indicator was constructed by adding the response (Strongly agree-agree-disagree-strongly disagree) on the Likert scales to four items: range = 4–16, Cronbach alpha = 0.78: (i) I spend a lot of time watching TV every day to learn about the epidemic. (ii) Every day, to learn about the epidemic, I spend a lot of time reading press articles (on paper or on screen). (iii) Every day, to learn about the epidemic, I spend a lot of time listening to radio. (iv) Every day, I spend a lot of time watching videos on the internet to keep myself informed about the epidemic.
Regarding ME, overall, 39% of respondents agreed (or strongly agreed) spending “lots of time” watching TV (i), 33% reading articles (ii), 21% listening to radio (iii), and 20% watching videos (iv) to obtain information about COVID-19.
FME was built of the testimonies on the overall 68% who found the media content was often frightening (agree or strongly agree to “The images of the epidemic that we see in the media (saturated intensive care units, evacuation of patients by helicopter, improvised morgues, etc…) are often frightening.” And 71% felt (agreed or strongly agreed) that “the testimonies of caregivers and/or patients they see/read/hear in the media were often frightening.” The same method was applied the FME indicator: range = 4–16; Cronbach alpha = 0.766.
Overall, 73% of respondents reported poor sleep over the previous 8 days (25% a lot and 48% a little); 54% of these reported their sleep had worsened during the lockdown (19% a lot and 48% a little) and 68% that this had significantly affected their daily activities (12% a lot and 56% a little). Over the past year, 15% had taken sleeping pills, and more than half of them (8% of respondents) had done so since the lockdown began. Severe sleep problems concerned 26% of adults.
The ME score was higher among men than women, while the reverse was true for the FME score (p < .001).
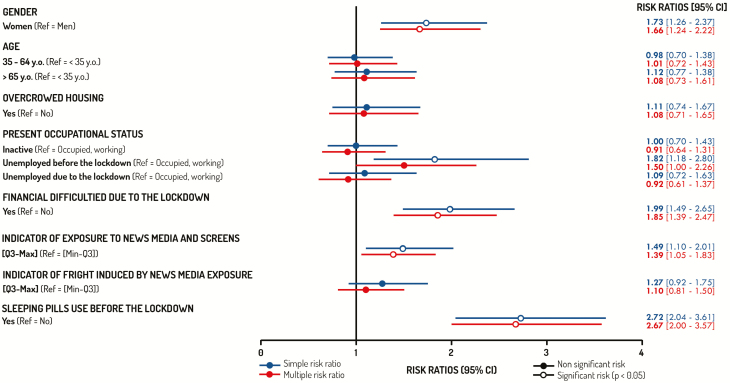
Multiple Poisson regressions found that aggravated and severe sleep problems with daytime impairment and/or sleeping pills use (26.2% of adults) during lockdown were strongly associated with the ME score. Compared with the overall sample representative of the general population, these problems were also significantly more frequent among women, people unemployed before the lockdown, and those with financial difficulties due to the lockdown (Figure 1).
Figure 1.
Factors associated with important sleep problems associated with impairment in daily activities and/or sleeping drug use, during lockdown (26%).
The prevalence of sleep problems during the lockdown was notably higher than that reported among the general population in France in 2017 (49%) [6]. Physicians usually recommend coping with sleep disorders by exercising, going outside, avoiding screen time, and having a regular schedule—all recommendations difficult to apply during lockdown. Being forced to stay home and the ensuing boredom and loneliness may have led to increased ME, especially among disadvantaged people and overexposure to media COVID-19 content may have contributed to fright and emotional distress. Sleep disorders may result from this imbalance, as sleep is sensitive to both environmental and psychological factors [7]. The bright blue light of screens and the noise of radio and TV have well-known adverse effects on sleep, and exposure to repetitive and continuous stressful information may provoke anxiety and emotional distress.
Media have undoubtedly played an important role during the COVID-19 epidemic in informing people about recommended prevention behaviors. Trying to influence or regulate their content is probably not feasible or effective. Research is needed to develop effective interventions that help people in varied housing conditions to limit media use in these exceptional circumstances and to adopt healthy sleep behaviors. Moreover, suffering from sleep problems may have increased media use at night, and thus increased stress and/or psychological distress and reinforced sleeping problems.
Funding
The COCONEL survey has been funded by the French and National Agency for Research (ANR), the Fondation de France (Grant # ANR-20-COVI-0035-01) and the National Research Institute for Sustainable Development (IRD).
Acknowledgments
The authors are indebted to the IFOP (Institut Français d’Opinion Publique) which launched the survey, to Jo-Ann Cahn who revised the English wording and to Keyne Charlot who designed the figure.
Appendix
The COCONEL survey was based on a permanent panel of 750,000 French individuals, authorized by the French National Agency for Data Protection (CNIL). To limit coverage bias, random sampling to match official French census statistics for age, gender, and geographical area, size of municipality, household income, education level, and occupation. We applied a Quota sampling method to achieve a sample of 1,000 respondents, representative for the French adult population in terms of age, gender, occupation, and population in the area of residence. To limit selection bias, the subject of the survey (the sleeping issue) was not precisely announced prior to the survey. Moreover, panelists with low response rates (i.e. panelists aged between 18 and 24 years old, workers, and intermediate occupations) were oversampled relative to others. Finally, 1,005 panelists had answered the survey out of the 25,800 invitations mailed out between April 15 and April 17, 2020, to achieve a French representative sample.
The COCONEL Group includes: Patrick Peretti-Watel1,2 (scientific coordinator), Valérie Seror1, Sébastien Cortaredona1, Lisa Fressard1, Odile Launay3, Jocelyn Raude4, Pierre Verger2 (research consortium), François Beck5, Stéphane Legleye5, Olivier L’Haridon6, Jeremy Ward1–7, Damien Léger8,9 (Steering Committee).
1Aix Marseille Université, IRD, AP-HM, SSA, VITROME, Marseille.
2Southeastern Health Regional Observatory (ORS Paca), Marseille.
3Inserm CIC 1417; Univ Paris, Faculté de médecine Paris Descartes; AP-HP, hôpital Cochin; Paris.
4 EHESP School of Public Health, Rennes.
5CESP, Univ Paris Sud, Faculté de médecine UVSQ, Inserm, Univ Paris-Saclay, Villejuif.
6Univ Rennes, CNRS, CREM UMR 6211, Rennes
7GEMASS, CNRS, Université Paris Sorbonne, Paris
8Université de Paris, EA 7330 VIFASOM (Vigilance Fatigue Sommeil et Santé Publique), Paris, France
9APHP, Hôtel-Dieu, Centre du Sommeil et de la Vigilance, Consultation de pathologie professionnelle Sommeil Vigilance et Travail, Paris, France.
Contributor Information
COCONEL Group:
Patrick Peretti-Watel, Valérie Seror, Sébastien Cortaredona, Lisa Fressard, Odile Launay, Jocelyn Raude, Pierre Verger, François Beck, Stéphane Legleye, Olivier L’Haridon, Jeremy Ward, and Damien Léger
References
- 1. Brooks SK, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dong M, et al. Letter to the editor: Headline stress disorder caused by Netnews during the outbreak of COVID-19. Health Expect. 2020;23(2):259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Koeze E, et al. The virus changed the way we internet. New York Times. April 7, 2020. https://www.nytimes.com/interactive/2020/04/07/technology/coronavirus-internet-use.html. Accessed April 7, 2020. [Google Scholar]
- 4. Beck F, et al. [Insomnia and total sleep time in France: prevalence and associated socio-demographic factors in a general population survey]. Rev Neurol (Paris). 2013;169(12):956–964. [DOI] [PubMed] [Google Scholar]
- 5. Parkerson GR Jr, et al. Development of the 17-item Duke Health profile. Fam Pract. 1991;8(4):396–401. [DOI] [PubMed] [Google Scholar]
- 6. Beck F, et al. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. [published online ahead of print June 28, 2020]. J Sleep Res. doi: 10.1111/jsr.13119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leger D, et al. Environmental open-source data sets and sleep-wake rhythms of populations: an overview. Sleep Med. 2020;69:88–97. [DOI] [PubMed] [Google Scholar]