Abstract
Objectives
We examined whether social isolation due to the COVID-19 shelter-in-place orders was associated with greater loneliness and depression for older adults, and, if so, whether declines in social engagement or relationship strength moderated that relationship.
Methods
Between April 21 and May 21, 2020, 93 older adults in the United States who had completed measures characterizing their personal social networks, subjective loneliness, and depression 6–9 months prior to the pandemic completed the same measures via phone interview, as well as questions about the impact of the pandemic on their social relationships.
Results
Older adults reported higher depression and greater loneliness following the onset of the pandemic. Loneliness positively predicted depression. Perceived relationship strength, but not social engagement, moderated this relationship such that loneliness only predicted depression for individuals who became closer to their networks during the pandemic. For those who felt less close, depression was higher irrespective of loneliness.
Discussion
The COVID-19 pandemic negatively affected older adults’ mental health and social well-being in the short term. Potential long-term impacts are considered.
Keywords: Aging, COVID-19, Depression, Loneliness
In response to the COVID-19 pandemic, more than 90% of U.S. residents were under shelter-in-place orders during April 2020 (Mervosh et al., 2020). One consequence of these orders was increased subjective isolation, generally referred to as loneliness (Killgore et al., 2020). Because loneliness negatively affects older adults’ mental and physical health (Cacioppo et al., 2010; Luo et al., 2012), the current study examined whether subjective isolation (loneliness) increased under the shelter-in-place orders and, if so, whether this predicted increased depression. We also explored the social network factors that might moderate this predicted relationship.
Loneliness is associated with myriad negative outcomes for older adults, including higher rates of depression and higher mortality (Luo et al., 2012). Longitudinal research suggests that loneliness predicts increased depression, but not the reverse (Cacioppo et al., 2010; for review, see Hawkley & Cacioppo, 2010). The relationship between loneliness and depression is moderated by a variety of social and lifestyle factors (Hawkley & Cacioppo, 2010; Segel-Karpas et al., 2018). Specifically, prior work suggests that greater social engagement (e.g., seeking social support) attenuates the relationship between depression and loneliness (Raut et al., 2014). However, another potential social factor that might moderate the association between loneliness and depression is relationship strength within individuals’ personal social networks (i.e., the group of family members and friends in which individuals are socially embedded). Indeed, closeness to the individuals in their network increases and predicts greater emotional well-being for older adults (English & Carstensen, 2014). Thus, greater closeness within an individual’s personal social network might attenuate the relationship between loneliness and depression. In the current investigation, we examine both social engagement and relationship strength as potential moderators between loneliness and depression.
An important theoretical limitation of extant research on loneliness for older adults is that it has typically focused on loneliness over a prolonged timeframe (e.g., over several years; Hawkley & Cacioppo, 2010). It thus remains unknown whether relatively brief periods of loneliness negatively affect older adults’ health. Social isolation imposed by shelter-in-place orders during the COVID-19 pandemic provided a natural experiment for examining the short-term effects of temporary social disruptions on older adults’ depression.
In the present study, we first assessed whether the shelter-in-place orders exacerbated loneliness for older adults, and, if so, whether that predicted increases in depression (Hypothesis 1). Subsequently, we explored social factors (social engagement and relationship strength) that might have moderated this predicted relationship. One possibility is that social engagement, notably spending less time with their personal social networks during the shelter-in-place orders, would exacerbate the relationship between loneliness and depression among older adults (Hypothesis 2a). Conversely, remaining virtually connected with their network members could attenuate that relationship (Hypothesis 2b). Indeed, social media use has been implicated in offsetting loneliness for some during the COVID-19 pandemic (for further discussion, see Galea et al., 2020). Alternatively, relationship strength might moderate the relationship between loneliness and depression such that older adults who felt less close to their network members during the shelter-in-place orders experienced an exacerbated relationship between loneliness and depression (Hypothesis 3). To account for potential individual differences in depression, we examined a population of older adults who had completed measures of their personal social networks, mental health, and loneliness 6–9 months prior to the COVID-19 pandemic and again during the pandemic.
Method
Participants
From June to October 2019, 120 older adults (MAge = 74.68 years, SD = 7.13; 64 female) from the Bloomington, Indiana community participated in a laboratory study on the impact of their social relationships on their overall well-being. Older adults were primarily white (96.7%) and well-educated (86.7% had a college degree or higher). None were cognitively impaired (as indicated by scoring >26 on the Mini-Mental State Examination; Folstein et al., 1975).
Starting in mid-April 2020, all 120 older adults were re-contacted and invited to participate in a phone interview related to the COVID-19 pandemic. A priori power analyses conducted in G*Power (Faul et al., 2007) using a small effect size (f2 = 0.15), α = 0.05, and power = 0.80, with three predictors indicated 77 participants would be sufficient to detect effects. The interviewers contacted and conducted interviews with 94 of the original participants (MAge = 75.20 years, SD = 6.86; 52 female). Of these, one female withdrew during the social network interview, and social network data from two others (1 male and 1 female) was lost due to experimenter error. Interviews took place between April 21 to May 21, 2020. The shelter-in-place order in Bloomington, Indiana was issued on March 24 and expired on May 16.
Materials and Procedures
In Time 1 (summer/fall 2019) and Time 2 (April/May 2020), older adults completed an expanded structured network interview adapted from the PhenX Toolkit Social Networks Battery (Hamilton et al., 2011; Perry & Pescosolido, 2010). The interview was the same in both waves. At Time 1 and Time 2, the interview elicited names of individuals in a respondent’s social network that were activated for discussions about “important matters,” as well as supportive ties, significant family members, neighbors, etc. (Perry et al., 2018). After the full list of names was elicited, respondents provided information about each person in the network, including tie strength (closeness between the respondent and each individual in the network). Social network data were then computed in STATA 16 using aggregation methods to generate average closeness in the network (tie strength) in the overall networks. An important benefit to using the social network interview instead of proxy questions (e.g., “How many good friends do you have?”) is that the latter may produce biased personal social network measures because such questions are cognitively demanding (Burt, 1987).
The social network interview was always completed first, but the order of the remaining measures was randomized across participants at Time 1 and Time 2. Directly relevant to the current study, these measures included the eight-item Patient Health Questionnaire (PHQ), a widely used measure of depression (Kroenke et al., 2009), and the three-item UCLA Loneliness Scale (Russell, 1996). We also collected measures related to anxiety and stress (see Supplementary Materials). Reliability on the PHQ was acceptable (α Time 1 = 0.75, α Time 2 = 0.67), and reliability on the loneliness measure was good at Time 1 and Time 2 (αs = 0.86 and 0.81, respectively). Test–retest reliability was high for all measures (rs > 0.60, ps < .001).
At Time 2 only, older adults also responded to questions about their COVID-related behaviors, including whether or not they were currently sheltering in place and, if so, how long they had been doing so (Table 1; Supplementary Table 1). Older adults also indicated whether their “social life has decreased/been negatively affected by COVID-19” (yes or no). Social engagement by asking whether they spent much more, somewhat more, just as much, somewhat less, or much less time during the pandemic reconnecting with others, spending time with others, and using social media to keep in touch. Respondents also provided an approximate amount of time (in minutes) that they spent “socializing virtually or over the phone each day,” and the number of times they had virtually contacted others in the past 2 weeks. See Supplementary Table 2 for correlations between measures.
Table 1.
Summary of Time in Isolation for the 87 (of 93) Respondents Who Had Indicated That They Were Sheltering in Place at the Time of the Interview
| N and % of respondents | |
|---|---|
| In late January | 0 (0%) |
| In early February | 1 (1.1%) |
| In late February | 12 (13.8%) |
| In 2 weeks before the order | 17 (19.5%) |
| 1 week before the order | 17 (19.5%) |
| A few days before the order | 7 (8.0%) |
| When the order started | 35 (40.2%) |
Notes: Time is relative to the statewide shelter-in-place order, which began March 24, 2020, and is in response to the question “When do you begin sheltering-in-place.” Response options offered to the respondents are provided in the table. % of respondents is relative to 87.
Results
COVID-Related Behaviors
Of the 93 individuals surveyed, 93.5% (N = 87) were still sheltering in place at the time of the interview. Of those, 56% (N = 52) had begun sheltering in place before it was state-ordered (Table 1). Analyses are reported only for the 87 older adults who were still sheltering in place at the time of the interview, but significant results remain as such for the full sample.
The majority of older adults (79.3%; N = 69) said their social life had decreased/been negatively affected by COVID-19, and more than two thirds (69.0%; N = 60) reported spending somewhat or much less time with people they cared about. However, 60.9% (N = 53) reported spending somewhat or much more time reconnecting or catching up with people they cared about, and 78.2% (N = 68) were using some form of internet technology to keep in touch during the pandemic.
Older adults reported spending an average of 78.79 min (SD = 81.20) socializing virtually or over the phone daily. Older adults also reported that they had virtually contacted others over the past 2 weeks an average of 42.61 (SD = 47.86) times.
Hypothesis 1: Sheltering in Place Associated With Increased Depression and Loneliness
No gender effects emerged regarding depression or loneliness, so findings are reported across gender. Overall, older adults experienced more depression in Time 2 (MPHQ = 3.24, SD = 3.24) than Time 1 (MPHQ = 2.40, SD = 2.71), t(84) = 3.07, p = .003, 95% confidence interval [CI] 0.29–1.38 and greater loneliness in Time 2 (MLoneliness = 6.05, SD = 2.83) than Time 1 (MLoneliness = 5.14, SD = 2.49), t(83) = 3.48, p = .001, 95% CI 0.39–1.42. Even though, on average, depression and loneliness increased, this pattern was not present for all older adults.
Hypothesis 1 predicted that increased loneliness during the shelter-in-place orders would positively relate to increased depression. To test this, we created difference scores (Time 2 – Time 1) for each variable. Consistent with Hypothesis 1, greater loneliness between Time 2 and Time 1 (M∆Loneliness = 0.77, SD = 2.37) predicted greater increases in depression from Time 1 to Time 2 (M∆PHQ = 0.89, SD = 2.52), r(86) = 0.22, p = .045.
Hypothesis 2: Reduced Social Engagement Predicts Loneliness, Depression
Hypothesis 2a examined whether a reduction in social engagement (e.g., spending less time with others) moderated the relationship between changes in loneliness and depression. To examine this possibility, we conducted two regressions with changes in loneliness, the social engagement measure, and the interaction between the two as predictors. The first model tested spending time with people they cared about (more, less, the same) as a potential moderator, whereas the second model tested spending time reconnecting with others (more, less, the same) as a potential moderator. Neither model was significant, both Fs < 2.13, ps > .10.
We next examined whether virtually connecting with others moderated the relationship between loneliness and depression (Hypothesis 2b). We again tested two different moderators here: (a) time spent virtually connecting with people they care about (more, less, the same) and (b) the number of minutes per day they spent socializing virtually or over the phone. Again, neither model was significant, both Fs < 1.93, ps > .13.
Hypothesis 3: Relationship Strength Predicts Loneliness, Depression
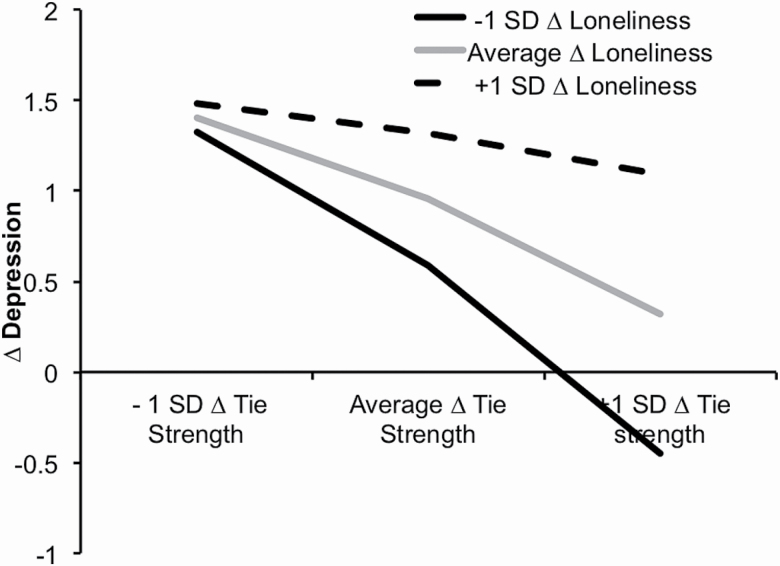
Finally, we examined whether changes in network closeness (tie strength) moderated the relationship between loneliness and depression for older adults (Hypothesis 3). Tie strength was an average based on how close the respondent was to each individual in his or her network (1 = not at all, 3 = very much). We created difference scores for tie strength (Time 2 – Time 1) to measure changes in network closeness during the pandemic (M∆Tie Strength = 0.04, SD = 19) and entered these into the regression. The overall model was significant, F(3,83) = 3.97, p = .011, and accounted for 13% of the variance in depression (see Table 2 for regression statistics). Results revealed that older adults who felt less close to their social network during the pandemic (vs. prior to it) experienced increased depression irrespective of their loneliness. However, for older adults who felt closer to their social networks during the pandemic (vs. prior to it), depression only increased markedly for those who experienced a large increase in loneliness. Notably, depression scores were reduced slightly during the pandemic for older adults whose network ties became stronger and who experienced decreases in loneliness during the pandemic (Figure 1; Supplementary Table 3).
Table 2.
Summary of Regression Predicting ∆Depression (Time 2 – Time 1) From ∆Loneliness (Time 2 – Time 1), ∆Network Tie Strength (Time 2 – Time 1), and Their Interaciton
| Variable | β | t | R | R 2 |
|---|---|---|---|---|
| ∆Loneliness | 0.15 | 1.33 | 0.36 | 0.13 |
| ∆Network tie strength | −0.35 | −2.75** | ||
| ∆Loneliness × ∆Network tie strength | 0.26 | 1.98* |
*p ≤ .05, **p < .001.
Figure 1.
Simple slopes of −1 SD and +1 SD ∆Tie strength (Time 2 – Time 1) predicting ∆Depression (Time 2 – Time 1) as a function of −1 SD and high +1 SD ∆Loneliness (Time 2 – Time 1). For both tie strength and loneliness, −1 SD reflects decreases, whereas +1 SD reflects increases.
Discussion
Several important findings emerged from this study. First, older adults’ mental health was negatively affected by the COVID-19 pandemic. They experienced greater depression and loneliness than they had prior to the pandemic. Second, relationship strength (perceived closeness to network members), but not social engagement, moderated the relationship between loneliness and depression. Specifically, loneliness was associated with higher levels of depression for older adults who felt closer to their social networks during the pandemic. Conversely, older adults who felt less close to their social networks experienced more depression, irrespective of their loneliness. Finally, older adults’ were relatively adaptable in staying connected during the pandemic. Specifically, although it did not offset their loneliness (for similar findings, see Aarts et al., 2015; Bell et al., 2013), older adults reported spending much more time using social media to reconnect with people they cared about.
Our finding that older adults experienced increased depression during the COVID-19 pandemic is consistent with emerging work with young and middle-aged adults during the pandemic (Killgore et al., 2020; Wang et al., 2020). Because we were able to compare changes in mental health over time, we were uniquely positioned to capture an important shift in older adults’ mental health that might have otherwise gone unnoticed. An important caveat to our finding, however, is that although PHQ scores increased during the pandemic, the mean score at Time 2 was still relatively low (M = 3.24), which is below the cutoff for a clinical diagnosis of mild symptoms (Dhingra et al., 2011). Future research should monitor whether these symptoms continue to increase. Although we did not find gender differences in the current study (Barber & Kim, 2020), this could be because we measured increases in depression over time within our older adult sample. However, it is important to note that recent work found gender differences specific to COVID-related worries (Barber & Kim, 2020).
Our results also suggest that perceived closeness to social network ties during the pandemic exacerbated the relationship between loneliness and depression, but only for older adults who felt closer to their networks during the pandemic. Put another way, among older adults who became closer to their networks during the pandemic, those experiencing decreased loneliness were slightly less depressed during the pandemic than before it, while those with large increases in loneliness experienced significant increases in depression. Although older adults who felt less close to their networks during the pandemic showed the greatest increases in depression, this occurred irrespective of their loneliness. Together, these findings suggest that perceived relationship strength might have served a protective function for older adults in combination with low loneliness during the pandemic. However, for those who felt increasingly lonely, even stronger network ties did not attenuate effects on depression.
Albeit speculative, one possibility as to why some older adults felt lonelier during the pandemic while also feeling closer to their networks could pertain to their perceived value to the network. Specifically, older adults who felt less important to their networks during the pandemic (e.g., because they could not provide as much support to others as they had previously) might have felt lonelier, in spite of feeling closer to their network. Indeed, providing support to one’s network is even more beneficial to older adults’ mental well-being than receiving it (Thomas, 2010). Moreover, our data showed that loneliness was associated with lower perceived support-giving within the network (Supplementary Table 2). Future research should examine this relationship further.
There are several limitations to the current study. First, because there is not a young adult comparison, we cannot identify the extent to which these results are unique to older adults. However, because loneliness is two to three times more prevalent among older than young adults (Hawkley & Cacioppo, 2010), our results are particularly relevant to older adults. Moreover, because older adults had the highest fatality rate from COVID-19 (Wu & McGoogan, 2020), shelter-in-place orders in most states were longer and more critical for this population and may have thus been perceived as particularly isolating. Second, respondents in this sample were homogeneous (e.g., white and well educated), which limits the overall generalizability of these results. Relatedly, potential racial differences in older adults’ mental health outcomes also cannot be assessed. This is an important additional avenue for future research because COVID-19 disproportionately affects non-white populations (Centers for Diseases Control and Prevention, 2020). Third, because we did not collect data on household composition, we cannot determine whether sheltering in place had the most deleterious mental health outcomes for individuals living alone. Finally, we cannot rule out the possibility that self-reported time in isolation (as reported in Table 1) was inflated by memory errors because we did not collect data relevant to this point (e.g., confidence ratings).
Together, our findings suggest that the pandemic had immediate negative impacts on older adults’ mental health and social well-being. At the same time, they reinforce the adaptability of this population in maintaining their social relationships and the importance of perceived loneliness and social integration. Nevertheless, an important avenue of future research will be to evaluate how these negative impacts and adaptability unfold over time.
Supplementary Material
Acknowledgments
The authors thank Jenny Zhao, Anthony Morales, and Andrew Stewart for assistance with data collection. This study was not preregistered, but data, analytic methods, and study materials will be made available to other researchers upon request.
Funding
This publication [or project] was supported by a Project Development Team within the Indiana Center for Translational Science Institute NIH/NCRR grant number UL1TR001108.
Conflict of Interest
None declared.
References
- Aarts S, Peek S T, & Wouters E J (2015). The relation between social network site usage and loneliness and mental health in community-dwelling older adults. International Journal of Geriatric Psychiatry, 30(9), 942–949. doi: 10.1002/gps.4241 [DOI] [PubMed] [Google Scholar]
- Barber S J, & Kim H (2020). COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e17–e23. doi: 10.1093/geronb/gbaa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell C, Fausset C, Farmer S, Nguyen J, Harley L, & Fain W B (2013). Examining social media use among older adults. In Proceedings of the 24th ACM conference on hypertext and social media (pp. 158–163), Paris, France. doi: 10.1145/2481492.2481509 [DOI]
- Burt R S. (1987). Social contagion and innovation: Cohesion versus structural equivalence. American Journal of Sociology, 92(6), 1287–1335. doi: 10.1086/228667 [DOI] [Google Scholar]
- Cacioppo J T, Hawkley L C, & Thisted R A (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. doi: 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Diseases Control and Prevention (2020). COVID-19 in racial and ethnic minority groups. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
- Dhingra S S, Kroenke K, Zack M M, Strine T W, & Balluz L S (2011). PHQ-8 days: A measurement option for DSM-5 Major Depressive Disorder (MDD) severity. Population Health Metrics, 9, 11. doi: 10.1186/1478-7954-9-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English T, & Carstensen L L (2014). Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. International Journal of Behavioral Development, 38(2), 195–202. doi: 10.1177/0165025413515404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. doi: 10.3758/bf03193146 [DOI] [PubMed] [Google Scholar]
- Folstein M F, Folstein S E, & McHugh P R (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Galea S, Merchant R M, & Lurie N (2020). The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine, 180(6), 817–818. doi: 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- Hamilton C M, Strader L C, Pratt J G, Maiese D, Hendershot T, Kwok R K, Hammond, J. A., Huggins, W., Jackman, D., Pan, H., & Nettles, D. S. (2011). The PhenX Toolkit: Get the most from your measures. American Journal of Epidemiology, 174(3), 253–260. doi: 10.1093/aje/kwr193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L C, & Cacioppo J T (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W D, Cloonen S A, Taylor E C, & Dailey N S (2020). Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Research, 290, 113117. doi: 10.1016/j.psychres.2020.113117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine T W, Spitzer R L, Williams J B, Berry J T, & Mokdad A H (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- Luo Y, Hawkley L C, Waite L J, & Cacioppo J T (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine (1982), 74(6), 907–914. doi: 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh S, Lu D, & Swales V (2020, April 20). See which states and cities have told residents to stay at home. New York Times Retrieved from https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html
- Perry B L, & Pescosolido B A (2010). Functional specificity in discussion networks: The influence of general and problem-specific networks on health outcomes. Social Networks, 32(4), 345–357. doi: 10.1016/j.socnet.2010.06.005 [DOI] [Google Scholar]
- Perry B L, Pescosolido B A, & Borgatti S P (2018). Egocentric network analysis: Foundations, methods, and models (Vol. 44). Cambridge University Press. [Google Scholar]
- Raut N B, Singh S, Subramanyam A A, Pinto C, Kamath R M, & Shanker S (2014). Study of loneliness, depression and coping mechanisms in elderly. Journal of Geriatric Mental Health, 1(1), 20. doi: 10.4103/2348-9995.141920 [DOI] [Google Scholar]
- Russell D W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. doi: 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Segel-Karpas D, Ayalon L, & Lachman M E (2018). Loneliness and depressive symptoms: The moderating role of the transition into retirement. Aging & Mental Health, 22(1), 135–140. doi: 10.1080/13607863.2016.1226770 [DOI] [PubMed] [Google Scholar]
- Thomas P A. (2010). Is it better to give or to receive? Social support and the well-being of older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65(3), 351–357. doi: 10.1093/geronb/gbp113 [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho C S, & Ho R C (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, & McGoogan J M (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Journal of the American Medical Association, 323(13), 1239–1242. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.