ABSTRACT
Background
Recently a severe form of COVID-19 infection has been described in a cluster of children presenting as multisystem inflammatory condition. One of the important spectrum of this condition is incomplete Kawasaki disease (KD).
Case report
A 5-month-old male child presented with high-spiking fever for 5 days with skin rash, bilateral non-purulent conjunctivitis and irritability. His C-reactive protein was markedly elevated (215.4 mg/l). Echocardiography revealed dilated left main coronary artery (3.0 mm, Z score +4.30) and left anterior descending artery (2.37 mm, Z score +3.76). Concomitantly Reverse Transcription- Polymerase Chain Reaction for COVID-19 was positive on fifth day sample. He was diagnosed as incomplete KD with COVID-19 infection and treated with intravenous immunoglobulin (IVIG) (2 g/kg), oral aspirin and azithromycin. Patient improved after 48 h and was discharged on oral aspirin.
Conclusion
Incomplete KD may co-exist with COVID-19 infection in infant. Early institution of IVIG may lead to better outcome.
Keywords: incomplete Kawasaki disease, infant, COVID-19 infection
INTRODUCTION
Kawasaki disease (KD) is a systemic vasculitis of childhood occurring predominantly under 5 years of age, in which the most feared complications are coronary artery abnormalities [1]. From the onset of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2 or COVID-19) pandemics though children appears to have largely a benign course, recently a severe form of this disease described in a cluster of children from Europe and North America with a multisystem inflammatory condition [2]. This condition defined by WHO as multisystem inflammatory disorder in children and adolescents has a wide spectrum of manifestations ranging from incomplete KD, Kawasaki shock syndrome, toxic shock syndrome to multiorgan failure [2]. We are presenting case report of a 5-month-old infant with incomplete KD and concomitant COVID-19 infection.
CASE REPORT
A previously healthy 5-month-old boy from a green zone for COVID-19, weighing 6.5 kg was referred to our center with unrelenting fever for 5 days (spiking up to 40°C), irritability for 2 days and non-pruritic maculopapular rash in upper limbs and trunk for 2 days. He was also noted to have non-purulent bulbar conjunctivitis from Day 4 of fever. However, no cracked lips, strawberry tongue, edema of limbs were noticed. There was no history of cough, running nose, ear discharge, vomiting, diarrhea, icterus, seizure, altered sensorium, joint swelling, urinary straining or respiratory distress. There was no history suggestive of influenza like illness or gastroenteritis in recent past. There was no history of contact with known COVID-19 patients at the time of admission. On examination heart rate was 120/min regular, respiratory rate was 26/min, BP 92/58 mmHg, saturation was 98% in room air and warm extremities. There was no hepatosplenomegaly, lymphadenopathy or edema. Patient was treated with IV cephalosporin and paracetamol but without clinical improvement. Initial investigations revealed mild anemia and normal total and differential count (Hb 9.9, TLC 12570, N 50, L 45). Platelet count was 4.25 l/mm3. Markedly elevated C-reactive protein (CRP) (215.4 mg/l) and raised Erythrocyte Sedimentation Rate (ESR) (78 mm/h) were noted. Other relevant investigations showed hyper-ferritinemia (ferritin 975 ng/ml), hypoalbuminemia (2.4 g/dl), hyponatremia (130 mEq/l), normal renal and liver function, coagulation profile and urine examination. Chest X-ray showed mild opacity in right middle lung zone. Echocardiography was done in suspicion of incomplete KD, which showed normal left ventricular function, with left main coronary artery of 3.0 mm (Z score +4.30) (Fig. 1) and left anterior descending (LAD) artery of 2.37 mm (Z score +3.76) with increase perivascular brightness and lack of tapering (Fig. 2) but proximal right coronary artery (RCA) of 1.8 mm (Z score +1.8). Serum NT-proBNP level (2025 pg/ml) was raised. Intravenous immunoglobulin (IVIG) (2 g/kg) over 24 h and oral aspirin (30 mg/kg) was started. Fever subsided after 48 h of finishing IVIG infusion, and the child became playful, CRP reduced to 93 mg/l. Aspirin dose was reduced to 3 mg/kg/day after 48 h. In between RT-PCR for COVID-19 was sent from nasopharyngeal swab in view of fever in pandemic situation which came as positive. Multiplex PCR of nasopharyngeal swab did not find any other respiratory pathogen. Subsequently, nasopharyngeal swab for COVID-19 of both asymptomatic parents was send and both came to be positive. Oral azithromycin (10 mg/kg/day) was started and continued for 5 days as the child was in moderate disease severity category and fever was continuing at low spikes up to 48 h of IVIG therapy. Serial echocardiography evaluation was performed, showing appearance of tapering and loss of perivascular brightness on Day 12. Repeat nasopharyngeal swab for COVID-19 was sent after 10 days, which came as negative. Patient was discharged on oral aspirin (3 mg/kg/day) and planned for clinical follow-up after 2 weeks. Consent for publication was obtained from parents.
Fig. 1.
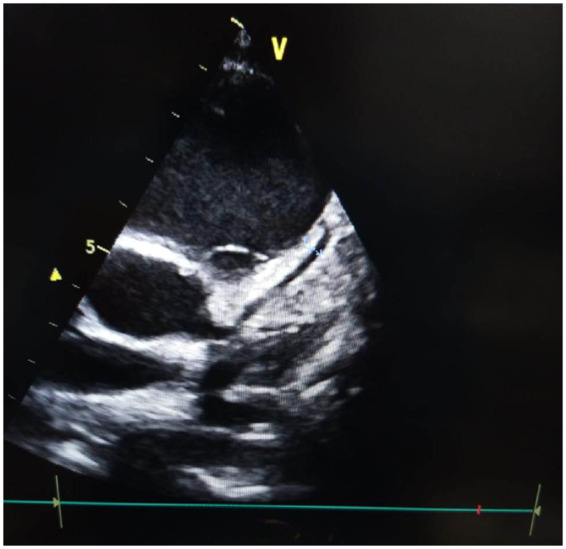
Image of echocardiography 2D mode showing left main coronary artery.
Fig. 2.

Image of echocardiography 2D mode showing left anterior descending artery with increase perivascular brightness with lack of tapering.
DISCUSSION
Severity of illness in infants and children with COVID-19 is far less catastrophic than that of adults. Children younger than 18 years have made up only 1.7% of national cases in the USA, and 2.0% of a large observational cohort in the UK [3, 4]. Recently, attention has now shifted to the vulnerability of children to hyper-inflammatory state which is defined by WHO as Multisystem inflammatory disorder of children and adolescents 0–19 years of age with fever > 3 days and two of the following: (i) rash or bilateral non-purulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet); (ii) hypotension or shock; (iii) features of myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities (including ECHO findings or elevated Troponin/NT-proBNP); (iv) evidence of coagulopathy (by PT, PTT, elevated d-Dimers); (v) acute gastrointestinal problems (diarrhea, vomiting or abdominal pain); and elevated markers of inflammation such as ESR, CRP or procalcitonin; and no other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes; and evidence of COVID-19 (RT-PCR, antigen test or serology positive), or likely contact with patients with COVID-19 [2].
Our patient had fever for 5 days with rash, bilateral non-purulent conjunctivitis and abnormal coronaries in echocardiography. Laboratory parameters showed elevated CRP and ESR; and COVID-19 was detected by RT-PCR. So, condition of the child was fulfilling multisystem inflammatory disorder with features similar to those of incomplete KD.
Kawasaki disease-like illness is sporadically reported in association with COVID-19 from few pediatric centers around the world though [5–7]. Children with persistent fever (≥ 5 days) with 2–3 principle criteria of typical KD should be evaluated for incomplete KD and presence of positive echocardiogram (Z score of LAD coronary artery or RCA ≥2.5 or coronary artery aneurysm) confirms diagnosis [8]. Patients with incomplete KD, particularly those <6 months of age may experience significant delays in diagnosis [9]. Early management with high-dose IVIG can avoid majority of complications. We have not observed any surge of KD in our center during this pandemic. This was the solitary case. Our patient improved partially within first 48 h of IVIG therapy. Azithromycin was added in the treatment as RT-PCR for COVID-19 was positive. No definite data are available on use of hydroxychloroquine and other antiviral therapy in infants suffering from COVID-19 infection.
Riphagen et al. [10] reported series of eight patients with hyperinflammatory shock syndrome. Median age was 8.9 years old (4–14 years) and predominant presentations were shock and gastrointestinal symptoms (7/8). One striking feature in imaging was echo-bright coronary vessels which progressed to giant coronary aneurysm in one patient. COVID-19 was positive in only two patients. Initial presentation may be severe with some patients but majority recover rapidly with IVIG and steroids [5, 10, 11]. During COVID-19 pandemic period in case of non-resolution/delayed resolution of fever in KD after IVIG therapy, co-association of COVID-19 to be suspected and tested. Incomplete KD as a presentation of COVID-19 in Indian infant is rarely reported to the best of our knowledge.
CONCLUSION
Incomplete KD as a spectrum of multisystem inflammatory disorder may co-exist with COVID-19 infection in infant. These need a high index of suspicion.
INFORMED CONSENT
Consent for publication was obtained from parents.
REFERENCES
- 1. Hang F-Y, Hwang B, Chen S-J, et al. Characteristics of Kawasaki disease in infants younger than six months of age. Pediatr Infect Dis J 2006;25:241–4. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Multisystem Inflammatory Disorder in Children and Adolescents. 15 May 2020 Statement. Geneva: World Health Organization. http://www.WHO/2019-nCoV/Sci_Brief/Multisystem_Syndro me_Children/2020.1 (28 May 2020, date last accessed).
- 3. Coronavirus Disease 2019 in children—United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep 2020;69:422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Docherty AB, Harrison EM, Green CA, et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. medRxiv 2020; published online April 28. doi: 10.1101/2020.04.23.20076042(preprint). [DOI]
- 5. Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 2020;395:1771–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Toubiana J, Poirault C, Corsia A, et al. Outbreak of Kawasaki disease in children during COVID-19 pandemic: a prospective observational study in Paris, France. medRxiv. 2020 May 14; doi:2020.05.10.20097394. [DOI] [PMC free article] [PubMed]
- 7. Jones V G Mills M Suarez D, et al. . COVID-19 and Kawasaki Disease: Novel Virus and Novel Case. Hospital Pediatrics 2020;10:537–40. [DOI] [PubMed] [Google Scholar]
- 8. McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 2017;135:e927–99. [DOI] [PubMed] [Google Scholar]
- 9. Minich LL, Sleeper LA, Atz AM, et al. ; Pediatric Heart Network Investigators. Delayed diagnosis of Kawasaki disease: what are the risk factors? Pediatrics 2007;120:e1434–40. [DOI] [PubMed] [Google Scholar]
- 10. Riphagen S Gomez X Gonzalez-Martinez C, et al. . Hyperinflammatory shock in children during COVID-19 pandemic. Lancet (London, England) . Lancet 2020;395:1607–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DAIC. Kawasaki-like inflammatory disease affects children with COVID-19 [Internet]. 2020. https://www.dicardiology.com/article/kawasaki-inflammatory-disease-affects-children-covid-19%C2%A0 (26 May 2020, date last accessed).


