Abstract
Organizational commitment to a structured professional advancement model (PAM) is critical for advanced practice provider (APP) development in order to promote and reward excellence, enhance job satisfaction and improve retention and recruitment. A PAM may also serve as a motivational tool for personal and professional growth by developing and promoting a professional, evidence-based collaborative practice environment. A voluntary PAM was implemented at a large Midwestern academic medical center to recognize experienced APPs including certified nurse practitioners, certified nurse-midwives and physician assistants. This manuscript describes the case for creating a PAM, implementation and evaluation.
Introduction
The advanced practice provider (APP) workforce has grown in recent years in response to the aging, increasingly insured United States population and a concurrent physician shortage.1, 2, 3 Additionally, since resident duty hour restrictions were implemented in 2003, academic medical centers have experienced increased demand for nurse practitioners (NPs) and physician assistants (PAs) to help meet critical patient care needs.4 All of these factors have resulted in our own large Midwestern academic medical center experiencing a 53% growth in APPs - including NPs, certified nurse-midwives (CNM) and PAs from 2014 to 2019. As our APP workforce increased and a reporting structure was created for APPs, our organization became more focused on methods to retain APPs and decrease turnover. One strategy was the creation of a professional advancement model (PAM). In this paper we describe the creation of our PAM and share early outcomes from the first three years of the program.
Background
Advanced practice providers manage a variety of primary care and specialty patient populations across the care continuum from ambulatory clinics to around the clock hospital coverage. Job performance of APPs has primarily been based on their ability to meet patient management needs. For the most part, however, they have not been incentivized to perform beyond these clinical responsibilities, including activities such as education, research, evidence-based practice projects or community wellness. Additionally, nurse practitioners have been found to be least satisfied with opportunities for professional growth5, 6 and opportunities to advance7. Recently reports are emerging on the interest for PAMs for APPs.7, 8, 9
Implementing advancement models is not a new concept within professional nursing, as clinical ladders for staff nurses have been in existence since the early 1970s to recognize and reward excellent registered nursing practice. Among staff nurses, clinical progression of nurses to expert has the ability to impact: 1) staff, patient and physician satisfaction, 2) professional development and 3) institution cost savings.10,11,12,13,14 Therefore, it is anticipated that implementing a PAM for APPs would yield similar benefits. At this time, reports on advancement programs for APPs are in the initial stages and more research is warranted to understand the impact of PAM programs on job satisfaction, retention and turnover of APPs.
Early Evidence to Support Professional Advancement Models for APPs
In 2012, the APP Council at Akron Children’s Hospital set out to create a PAM for APPs. In preparation, they reviewed the literature and developed a national survey to examine the importance of PAM variables. A nine-question survey was distributed to APPs at 15 hospitals throughout the country. Respondents (n=201) gave highest ratings to clinical practice and leadership as the most important factors on an advancement model. A repeat survey of 561 respondents at an APP leadership summit validated the initial survey findings. Based on the survey results, Akron Children’s Hospital implemented a three-tier PAM in the spring of 2013. Though no outcome data is reported, the authors suggested that a PAM could be used as an effective tool to measure institutional accomplishments and contributions to allow for role definition and ongoing growth.8 In a survey of NPs at New York University Hospitals Center, Paplanus and colleagues (2015) found support for the development of a three-level professional NP clinical ladder in order to support professional role development, provide financial compensation and enhanced job satisfaction. Similar to Stratton (2015), Paplanus et al., (2015) reported on the development and implementation of a model but did not provide a formal evaluation of their program.7, 8
University of Maryland Medical Center, Baltimore also developed a PAM based on survey data of 300 APPS (including NPs, certified registered nurse anesthetists, clinical nurse specialists, and PAs) demonstrating a lack of professional advancement opportunities9. Within 2 years of the survey the organization developed and implemented a four-tier PAM that included four domains: clinical expertise, leadership and policy, research/evidence-based practice and education. One year post-implementation, APPs were largely supportive of the PAM. Additionally, APP turnover decreased from year one to year three from 13.8% to 5%.9 Additionally, Paul and colleagues (2019) implemented a professional advancement model at Boston Children’s Hospital based on Benner and the American Association of Critical Care Nurses Synergy Model. The three-level advancement model implemented in 2017 identified practice domains (clinical practice and outcomes, impact and leadership) and required skills and competencies. Applicants were required to submit documentation through an advancement portfolio. About 12% of eligible APRNs were promoted to level II and received a 3% increase in their base salary. There was a positive impact on applicants seeking professional and leadership opportunities. The authors report successful implementation of the first phase and will be tracking outcomes related to recruitment and retention15.
The Case for a Professional Advancement Model
Estimates of APP turnover range from 12.6–2016 and the Advisory Board estimates that for each day an APP position is vacant it costs the healthcare organization $1,500.17 In 2014 our health system’s APP turnover rate was 22%. Additionally 40% of our NPs reported they were unsure about staying or did not intend to stay in their current position. They were least satisfied with intrapractice partnership/collegiality and professional growth, consistent with the APP literature.18,19,20 Together, this spurred our APP leadership to examine opportunities to improve APP retention. One such opportunity was a PAM, which supports the professional development and career advancement of APPs. We envisioned that a PAM would eliminate lost revenue from turnover and training, incentivize retention of more seasoned APPs, and offer a competitive edge for recruiting new and experienced APPs.
Program Development and Implementation
A PAM was proposed by our APP Shared Governance Council to reward high performing APPs for their clinical expertise, as well as their achievements in other professional development activities. Senior leadership collaborated with the APP Directors to develop an annual bonus structure that the APP would receive upon completion of an approved professional advancement plan. Concurrently, APP Shared Governance leaders reviewed the literature and contacted other institutions with PAMs to formulate the structure of our PAM.
Once the business plan was approved, a committee of APP leaders formed to operationalize the program, which was based on Benner’s adaptation of the Dreyfus Model of Skill Acquisition.21 Our model sought to promote professional practice by rewarding clinicians who excel in clinical practice, education, leadership, research/evidence-based practice, and community service. Based Benner’s novice to expert framework, we created three APP levels: Entry, Proficient and Expert (Table 1). The PAM is a voluntary program in which the APP demonstrates and maintains expertise in the following exemplar areas: 1) leadership, 2) clinical education 3) clinical practice, 4) research/evidence-based practice, and 5) community service and wellness. The PAM Committee envisioned the following goals of the PAM:
Table 1.
Professional Advancement Model levels
| APP Category | Description and Qualifications |
|---|---|
| APP (entry) |
|
| APP Proficient |
|
| APP Expert |
|
Note. APP = advanced practice provider - includes nurse practitioners (NP), certified nurse-midwives (CNM) and physician assistants (PA)
promoting excellence in the five PAM exemplar areas
enhancing job satisfaction, increasing APP retention and recruitment,
providing a motivational tool for professional APP growth,
promoting a professional, evidence-based, collaborative practice environment, and
providing a role development tool and mentorship process.
The committee outlined the qualifications for Proficient and Expert and created a timeline for submission. Applicants must be NP’s, PA’s, or CNM’s employed at least 60% for 12 months prior to the application and demonstrate professional specialty organization membership. The criteria for advancement (education, practice, leadership, EBP, etc) are major components of the clinical nurse specialist job description, and therefore they have their own advancement program under development at our institution. Applicants are required to submit an Intent to Advance form and an advancement goal and plan for each of the five category exemplars. The goal statements are to be written as SMART goals (specific, measurable, attainable, relevant and time-bound) with detailed action plans. Examples of Proficient and Expert goals can be found in Table 2.
Table 2.
Professional Advancement Model Proficient and Expert goal category examples
| Proficient | Expert |
|---|---|
| Leadership Exemplar | |
|
|
| Clinical Education Exemplar | |
|
|
| Clinical Practice Exemplar | |
|
|
| Research/Evidence-Base id Practice (EBP) Exemplar | |
|
|
| Community Service & Wellness Exemplar | |
|
|
Note. This is not an exhaustive list of goals. Each goal must be submitted in SMART format (specific, measurable, attainable, relevant and time-bound) and requires evidence of completion that can be submitted electronically
To manage and oversee the PAM process, a new APP Shared Governance committee was established. The Professional Advancement Program Committee consists of two directors of APPs, two co-chairs, and members at large. Committee members are recruited from program candidates who had successfully attained proficient or expert status. An initial review of each APP’s proposed plan is completed to determine if a revised plan is necessary by the Professional Advancement Program Committee. Mentors are made available to assist applicants in the process. In the first year of the program APP managers served as the mentors and subsequently, committee members have fulfilled this role. Final electronic submission of plan completion includes supporting evidence of how each exemplar was met and an abstract of 300 words or less that summarizes the process. Figure 1 displays the PAM timeline. Successful candidates are awarded a bonus at the end of the year, 5% of annual salary for Proficient and 7% for Expert. The PAM requires annual resubmission to maintain or advance the Proficient and Expert levels.
Figure 1.
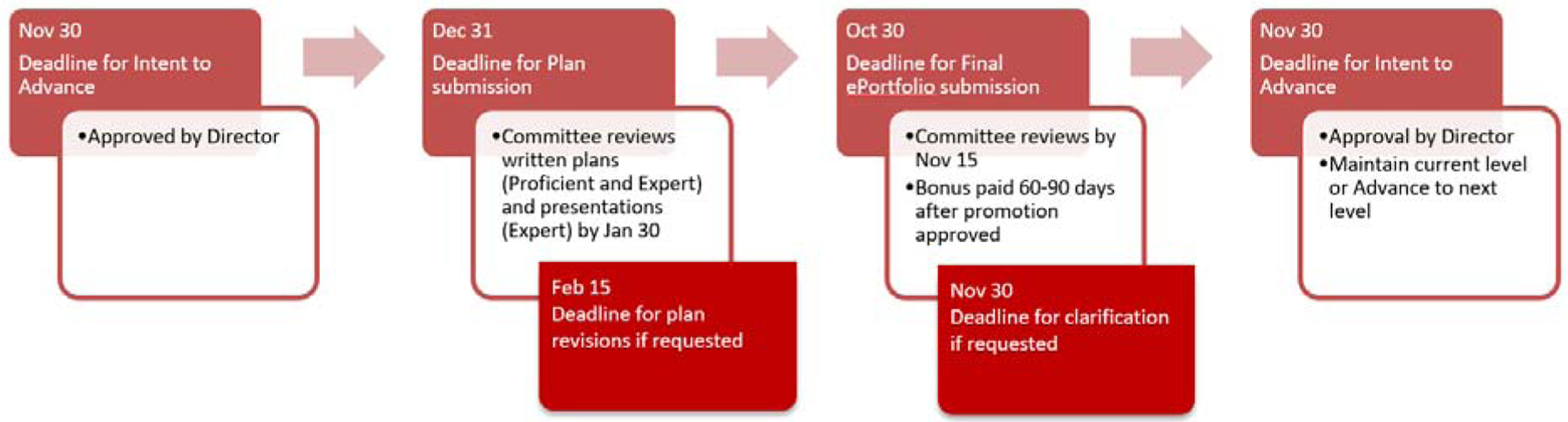
Professional Advancement Model timeline
Results and Evaluation
Our institution employed 406 APPs in year one, 460 APPs in year two, and 543 APPs in year three. Of eligible APPs, 150 (37%), 109 (24%), and 94 (17%) applied for advancement in years one two and three, respectively. Table 3 displays a summary of the program results for the first three years. Year two was the first time applicants could apply for Expert, and many APPs who initially applied for Expert completed the Proficient level instead due to the high expectations for Expert level. Program completion was attained by 71 (47%), 60 (55%), and 48 (51%) of applicants in each of the first three years, respectively. Reflecting our institution’s population of APPs, NP’s comprised the majority of those completing the program each year. Those completing the program included 62 NPs (87%), and 9 PAs (13%); 50 NPs (83%) and 10 PAs (17%); and 37 NPs (77%) and 11 PAs (23%) in each of the first three years, respectively. Common reasons for non-completion were that the applicant’s initial advancement plan did not meet the outlined criteria, or the applicant chose not to complete the program after initial plan acceptance. Less commonly applicants’ final program completion materials did not meet criteria for Proficient or Expert level.
Table 3.
Professional Advancement Model numbers of applicants and completions in the first three years
| Applied | Successful Completion | |||||
|---|---|---|---|---|---|---|
| Proficient | Expert | Total | Proficient | Expert | Total | |
| Year 1 | 150 | * | 150 | 71 | * | 71 |
| Year 2 | 73 | 36 | 109 | 48 | 12 | 60 |
| Year 3 | 78 | 16 | 94 | 38 | 10 | 48 |
Note.
Applicants only eligible for Proficient year one
To assess barriers to PAM application and completion and to gather feedback for program evaluation and improvement, all APPs in the institution were asked to complete a survey approximately six months after each program year completion, regardless of whether they participated in the APP PAM. Annual survey response rates ranged from 30–60%. Results from survey respondents who also participated in the PAM are presented in Table 4.
Table 4.
Results of annual survey regarding APP perceptions of the Professional Advancement Model.
| Year 1 (n=78) | Year 2 (n=120) | Year 3 (n=66) | |
|---|---|---|---|
| Reason applied, n (%) | |||
| Compensation | 54 (76) | 80 (68) | 42 (76) |
| Already meeting level criteria | 42 (59) | 73 (62) | 44 (80) |
| Recognition | 35 (49) | 27 (23) | 22 (40) |
| Build resume | 34 (48) | 33 (28) | 23 (42) |
| Professional growth | -- | 66 (56) | 34 (62) |
| Most difficult part of the process, n (%) | |||
| Electronic submission | 29 (41) | 35 (32) | 13 (27) |
| Writing goal statement | 29 (41) | 31 (28) | 16 (33) |
| Coming up with plan | 21 (30) | 26 (24) | 9 (18) |
| Writing final abstracts | 19 (27) | 6 (5) | 16 (34) |
| Completing the plan/goals | 15 (21) | 9 (8) | 7 (14) |
| Conflicting feedback | -- | 58 (53) | 20 (41) |
| Finding time to complete goals | -- | 52 (47) | 30 (61) |
| Meeting program expectations | 17 (24) | 41 (37) | -- |
| Meeting the deadlines | -- | 14 (13) | 4 (8) |
| Finding a community service project | -- | 23 (21) | -- |
| Completing initial plan worksheetsa | -- | -- | 15 (31) |
| Most time-consuming aspect, n (%) b | |||
| Writing final abstract | 35 (49) | 33 (30) | |
| Writing goal statement | 28 (39) | 33 (30) | |
| Coming up with plan | 21 (30) | 20 (18) | |
| Electronic submission | 20 (28) | 25 (23) | |
| Completing the plan/goals | -- | 52 (47) | |
| Collecting evidence of completion | -- | 37 (34) | |
| Instructions were clear, n (%) c | 47 (66) | 80 (68) | 27 (49) |
| Compensation was worth the effort, n (%) c | 25 (48) | 51 (55) | 20 (67) |
| Would apply again c | 42 (59) | 63 (57) | 33 (67) |
Note. Totals do not equal 100% as these were multiple response items.
Due to missingness, percentages are calculated from the number of respondents who answered each item.
Worksheets intended to facilitate writing goal statements and plan activities was initiated in year 3 based on feedback from previous years
This question was omitted in year three
Percent of respondents who answered yes; non-multiple response items
Most APPs applied for advancement for the financial compensation and because they already met the criteria for advancement with their current work and projects. In the first two years, among the most difficult parts of the process were submitting the final evidence electronically and writing SMART goal statements. Additionally, APPs found completing the plan/goals also to be difficult, which might reflect the high level of performance expected for plan completion. Some applicants reported getting conflicting feedback, often between their assigned mentor and the plan reviewers.
Survey respondents offered several areas of constructive feedback. Some found the timing of the program difficult with the initial plan submission due date of December 31. Others found the process of evaluation subjective. The need for community service was also of concern with regards to the value of it as professional advancement and difficulty finding opportunities. Some did not agree with the compensation amount and felt the program activities had to be completed outside of regular work hours. However, despite this feedback, over half of APPs responded that they would apply again, and this percentage has increased each year to 67% at the end of year 3.
Outcomes of the PAM
Despite initial challenges with implementing the PAM, our organization has seen some immediate gains, such as increased APP visibility within the organization as well as externally. More APPs are presenting at APP Grand Rounds, they are publishing more in peer-reviewed journals, and presenting at conferences locally and nationally. For example, we saw a doubling in abstract submission to our regional APP conference from 20 in year one to 45 in year three of the PAM. Our APPs represent us locally, nationally, and internationally serving on committees, boards, and dissemination of their clinical and scholarly work. While the professional advancement program is likely not the sole contributor, there has been a decreasing turnover rate in APPs from 22% before implementation of the PAM to a current turnover rate of 5%. This decrease in turnover has had a significant positive financial impact for our institution, which supports the cost of the APP PAM.
Future Directions
We continue to survey PAM participants annually to evaluate and improve upon the program. When we saw a decline in the number of applicants after year three, we implemented several changes. Starting in year four, the Committee and APP leadership moved the maintenance process to align with the annual professional review process, created a goal/plan worksheet to improve submission quality, and revised standardized scoring system to make the process more objective. This increased the APP success rate from 47% in year 1 to 69% in year 4. We plan to replicate the 2013 survey to examine APP job satisfaction and intent to stay.20 These survey findings will be used to evaluate the PAM program and aspects of the APP workforce at our institution.
Conclusion
Implementing a PAM for APPs recognizes their multi-faceted contributions to professional practice, rewards expertise and adds value to the organization. Improved APP job satisfaction and retention has the ability to positively impact the quality and safety of patient care. Proficient and Expert APPs contribute to successful hospital Magnet and Beacon accreditations - both indications of high-quality patient care. As healthcare systems increasingly rely on APPs to deliver high-quality care, they should consider the mechanisms that support them to advance, such as PAMs, as a means for improved patient and APP workforce outcomes.
Highlights.
Traditionally, advanced practice providers (APPs) have been recognized and rewarded based solely on patient care activities
Professional advancement models provide a formal way to elevate the role of APPs and reward professional development
In implementing professional advancement models, organizations have the opportunity to improve APP job satisfaction and decrease turnover
Funding source:
This research was supported by the National Institute of Nursing Research (T32-NR0714, L. Aiken, Principal Investigator).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hooker RS, Cawley JF, & Everett CM (2011). Predictive modeling the physician assistant supply: 2010–2025. Public Health Reports 126(5), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auerbach DI (2012). Will the NP workforce grow in the future? Medical Care, 50(7), 606–610. [DOI] [PubMed] [Google Scholar]
- 3.Maier CB, Barnes H, Aiken LH & Busse R (2016). Descriptive, cross-country analysis of the nurse practitioner workforce in six countries: Size, growth, physician substitution potential. BMJ Open, 6(9), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moote M, Krsek C, Kleinpell R, & Todd B (2011). Physician assistant and nurse practitioner utilization in academic medical centers. American Journal of Medical Quality, 26(6), 452–460. [DOI] [PubMed] [Google Scholar]
- 5.Misener T & Cox DL (2001). Development of the Misener nurse practitioner job satisfaction scale. Journal of Nursing Measurement, 9, 91–108. [PubMed] [Google Scholar]
- 6.DeMilt DG, Fitzpatrick JJ, & McNulty SR (2011). Nurse practitioners’ job satisfaction and intent to leave current positions, the nursing profession, and the nurse practitioner role as a direct care provider. Journal of the American Academy of Nurse Practitioners, 23, 42–50. [DOI] [PubMed] [Google Scholar]
- 7.Paplanus LM, Bratley-Daniele P & Mitra KS (2014) Knowledge translation: A nurse practitioner clinical ladder advancement program in a university-affiliated integrated medical center. Journal of the American Association of Nurse Practitioners, 26, 424–437. [DOI] [PubMed] [Google Scholar]
- 8.Stratton A, Breedlove K Kulasa-Luke D, Tsirambidis K & Brandon G (2015) Creating a model for professional advancement, Advance Healthcare Network NPs & PAs http://nurse-practitioners-and-physician Accessed January 29, 2019. [Google Scholar]
- 9.McComiskey C, Simone S, Schofield D et al. (2018). Professional advancement of advanced practice clinicians. The Journal for Nurse Practitioners, 14(1), 12–17. [Google Scholar]
- 10.Zimmer MJ (1972). Rationale for a ladder for clinical advancement. Journal of Nursing Administration, 2(6), 18–24. [DOI] [PubMed] [Google Scholar]
- 11.Shapiro M (1998). A career ladder based on Benner’s model an analysis of expected outcomes. The Journal of Nursing Administration, 28(3), 13–19. [DOI] [PubMed] [Google Scholar]
- 12.Drenkard K & Swartwout E (2005). Effectiveness of a clinical ladder program. Journal of Nursing Administration, 35(11), 502–506. [DOI] [PubMed] [Google Scholar]
- 13.Warman GA, Williams F, Herrero A et al. (2016). The design and redesign of a clinical ladder program: Thinking big and overcoming challenges. Journal for Nurses in Professional Development, 32(6), E1–E7. [DOI] [PubMed] [Google Scholar]
- 14.Moore A, Meucci J & McGrath J (2019). Attributes of a successful clinical ladder program for nurses: An integrative review. World Views on Evidence-Based Nursing, 16(4), 263–270. [DOI] [PubMed] [Google Scholar]
- 15.Paul F, Abecassis L, Freiberger D, et al. (2019). Competency-based professional advancement model for advanced practice RNs. JONA, 49(2), 66–72. [DOI] [PubMed] [Google Scholar]
- 16.Anderson C Managing doctor, nurse practitioner turnover rates key to collaborative care. Healthcare Finance. HIMSS Media Publications. Accessed from https://www.healthcarefinancenews.com/news/managing-doctor-nurse-practitioner-turnover-rates-key-delivery-collaborative-care-model on 2/24/2020. [Google Scholar]
- 17.Hostetter S and Campbell E Want to reduce APP turnover? Give them a voice in your medical group. Advisory Board. https://www.advisory.com/research/medical-group-strategy-council/practice-notes/2019/07/app-leadership accessed 2/24/2020. [Google Scholar]
- 18.Faris JA, Douglas MK, Maples DC, Berg LR, & Thrailkill A (2010). Job satisfaction of advanced practice nurses in the Veterans Health Administration. Journal of the American Association of Nurse Practitioners, 22, 35–44. [DOI] [PubMed] [Google Scholar]
- 19.DeMilt DG, Fitzpatrick JJ, & McNulty SR. (2011). Nurse practitioners’ job satisfaction and intent to leave current positions, the nursing profession, and the nurse practitioner role as a direct care provider. Journal of the American Academy of Nurse Practitioners, 23, 42–50. [DOI] [PubMed] [Google Scholar]
- 20.Brom HM, Melnyk BM, Szlacha LA, & Graham M (2016). Nurse practitioners’ role perception, stress, satisfaction and intent to stay at a Midwestern academic medical center. Journal of the American Association of Nurse Practitioners, 28, 269–276. [DOI] [PubMed] [Google Scholar]
- 21.Benner P (1984). From novice to expert: Excellence and power in clinical nursing practice. Menlo Park: Addison-Wesley, pp. 13–34. [Google Scholar]


