Background
As the pace of health sector transformation accelerates, the importance of leadership continues to grow across all health professions. Advances in a variety of disciplines can inform effective leadership development. However, at present, most health sector leadership competency models do not incorporate these advances and are instead developed using consensus-based methods within specific professions. An interprofessional approach to leadership competencies could help incorporate these advances and support better interdisciplinary leadership development.
Purpose
This study was pursued to revise and revalidate a widely used health sector leadership competency model and assess its potential for providing greater interoperability across the professions.
Methodology/Approach
Using the National Center for Healthcare Leadership’s interprofessional competency model Version 2.1 as the starting point, we developed a revised and revalidated model in four phases: (a) we completed a future scan using methods described in Garman et al. [Garman, A. N., Johnson, T. J., & Royer, T. (2011). The future of healthcare: Global trends worth watching. Chicago, IL: Health Administration Press.]; (b) we collected behavioral event interview data from pairs of leaders representing different organizational and performance levels, using methods developed by Boyatzis [Boyatzis, R. E. (1982). The competent manager: A model for effective performance. New York, NY: John Wiley & Sons.]; (c) we conducted a validity study via electronic survey of 145 working managers and calculated content validity ratios using methods described by Lawshe [Lawshe, C. H. (1975). A quantitative approach to content validity. Personnel Psychology, 38(4), 563–575.]; and (d) we used natural language processing to assess the extent to which existing leadership models in the health professions will crosswalk to the new model.
Findings
All competencies in the revised model successfully met criteria for validity. The revised model also successfully crosswalked against, on average, 85% of the competencies in the other five health professions leadership models.
Practice Implications
Based on the results of this research, we conclude the revised model can provide a “common language” framework in support of interdisciplinary leadership development. The availability of such a model may also assist human resource and development executives in better aligning learning resources with organizational goals.
Key words: interprofessional practice, leadership competencies, leadership development
In recent years, health delivery models in the United States have begun evolving at an unprecedented pace. Major changes at times seem almost too numerous to count but include rapid escalation of scale within traditional health systems through consolidation; cross-sector mergers bringing distinct business models together in novel ways, fundamentally changing the nature of the competitive landscape; advances in precision medicine, changing the ways in which diagnostics and care are delivered; and health systems taking greater leadership roles in the health and vitality of the communities they serve (Cabral, Garman, & Moscola, 2018; Garman, Lemak, & Standish, 2018; Society for Healthcare Strategy and Market Development, 2017). At the same time, community and governmental organizations are increasingly recognizing that successfully addressing complex systems challenges will require bridging the boundaries of professional disciplines (Acosta, Chandra, & Madrigano, 2017).
Within this context, increasing attention is being paid to leadership competencies across the health professions (Garman & Johnson, 2006). Ongoing leadership development is becoming more widely recognized as a critical activity for supporting strategic goals (Crowe et al., 2017; Li, Barth, Garman, Anderson, & Butler, 2017), and the role and expectations of higher education in preparing future leaders are also increasing. In particular, as concerns about cost-related access problems in higher education increase, emphasis has been growing on competency-based models of education, in which demonstrations of mastery are emphasized over course completion (Franklin & Lytle, 2015; Kelchen, 2015).
Despite this increased attention to leadership and competency-based approaches, there are clear gaps in the leadership development practices of many practice and higher education settings. On the practice side, Lucas, Goldman, Scott, and Dandar (2018) found that, although nearly all academic medical centers surveyed offered faculty leadership development programs, very rarely were these programs based on any specific leadership competency model. On the higher education side, a recent scoping review of leadership development programs in interprofessional education and practice found only 9% referenced theory, and only 3% provided a conceptual framework of any kind (Brewer, Flavell, Trede, & Smith, 2016). Even in higher education settings where competency-based approaches are prevalent, leadership development programs tend to use locally developed competency definitions, resulting in little or no standardization. In one recent review of 475 academic programs within 72 academic accrediting organizations, Seemiller and Murray (2013) tabulated a total of 244 distinct leadership competency definitions across 61 different domains.
In this article, we describe efforts in collaboration with the United States-based, nonprofit National Center for Healthcare Leadership (NCHL) to develop a science-informed and practice-friendly competency model to support leadership development in the health sector. The NCHL model was originally developed as a resource to help prepare people for progressively more responsible health care leadership roles. The most recent major revision of the model created Version 2.1 (Calhoun et al., 2008), containing 26 competencies, each with between three and six behaviorally defined levels of proficiency. In pursuing revision and revalidation for a Version 3.0, we sought to achieve three goals: (a) pursuing a more inclusive and participatory definition of the leadership role, (b) capitalizing on current and emerging research on leadership competencies, and (c) incorporating current and emerging challenges and opportunities anticipated for the health sector in the coming decade. The rationale for our third goal was explained in the introduction; we provide theoretical and conceptual underpinnings informing our first two goals in the next section.
Theoretical and Conceptual Frameworks
Leadership in the Health Sector: An Inclusive Definition
As far back as 1974, David Stogdill, a pioneer of modern leadership behavioral research, noted that “there are almost as many different definitions of leadership as there are persons who have attempted to define the concept” (Stogdill, 1974, p. 7). Although leadership remains one of the most widely studied phenomena within the social sciences, efforts to establish a definition that is both precise and universal remain unsuccessful. As a result, most modern review articles define leadership implicitly (e.g., accepting author self-definitions; cf. Lord, Day, Zaccaro, Avolio, & Eagly, 2017) or informally (e.g., providing a general description; cf. Yukl, 2012). For our purposes, we adopted the informal definition provided by Yukl (2012), which describes the essence of organizational leadership as “influencing and facilitating individual and collective efforts to accomplish shared objectives.” The emphasis of this definition on “influencing” and “facilitating” includes the many ways individuals may attempt to affect the perspectives and actions of others as part of their day-to-day work, regardless of whether they are formally recognized as a leader by title. Defined in this way, leadership can be viewed as a role almost all individuals with interdependent responsibilities need to take periodically in order to accomplish their goals.
Leadership Competencies
Although leadership research has been ongoing for more than a century, much of the early work focused on identifying individual differences in potential (Lord et al., 2017). Efforts to define leadership in terms of a set of competencies originated with the work of psychologist David McClelland in the 1950s. In a seminal article in American Psychologist, McClelland (1973) argued that competencies—outcomes-relevant measures of knowledge, skill, abilities, and traits and/or motives—could provide a more useful approach to aptitude measurement than the intelligence- and personality-related assessments that were in widespread use at the time. In the following decades, several extended works were published documenting methods for robustly identifying competencies that could distinguish high-performing leaders. Among these works was the widely referenced source text The Competent Manager (Boyatzis, 1982).
In the 1990s, as the pace of technology-related advances accelerated, leadership roles also began evolving more rapidly. Organizations found they needed to define leadership roles more dynamically, providing greater flexibility for ongoing adaptation to changing organizational needs. Competency models, providing greater relative flexibility in comparison to traditional job analysis methods, began to flourish and evolve in new ways. In particular, organizational leaders began to recognize the value of defining learning and development needs not just around individual leaders but also around the “core competencies” of the organization as a whole (Prahalad & Hamel, 1990). Although competency practice was accelerating, the evidence base to inform it was not, and concerns began to grow about variations in the rigor of methods being used. The concerns eventually led the Society for Industrial and Organizational Psychology and the Society of Human Resource Management to commission task forces to publish professional practice guidelines (Campion et al., 2011; Schippman et al., 2000; Stetz & Chmielewski, 2015).
During the same period, although many academically based researchers continued developing new models of leadership, several scholars began making ambitious attempts to synthesize vast amounts of prior research into competency taxonomies (cf. Tett, Guterman, Bleier, & Murphy, 2000). By this time, three domains were already widely recognized as relevant across leadership models—one relating to structuring tasks, another relating to managing work relationships, and a third relating to managing change. More recently, a highly influential summary by Yukl (2012) identified a fourth domain, which is related to externally facing or “boundary spanning” work of leaders. Yukl also referenced a growing trend in studying the role of values in our understanding of leadership effectiveness and predicted this would become a more central component of future leadership models.
Leadership Competencies in the Health Professions
Although the health professions have a long history of recognizing the importance of their members taking leadership roles, formal definitions of clinical leadership roles and competencies have been more recent developments. So far, most of this work has taken place in the context of specific professions; however, there have been a few noteworthy exceptions. In the United States, the NCHL developed a competency model explicitly designed to transcend professions and career stages (Calhoun et al., 2008). In the United Kingdom, the National Health Service Leadership Academy (2011) developed the Clinical Leadership Competency Framework, which serves as a common point of reference for leadership development across the clinical professions. Across several subdisciplines of the health care management profession, the Healthcare Leadership Alliance, a U.S-based consortium of health care management professional associations, developed a five-domain model to be a high-level organizing framework aligning their associations’ health care management competency models (Stefl, 2008). In higher education, the Interprofessional Education Collaborative (2016) identified leadership as one of the subcompetencies in its Core Competencies for Interprofessional Collaborative Practice: 2016 Update.
Although these efforts each made important contributions in their own way, most were developed without regard to existing health care leadership models, let alone the evolving scientific literature on leadership and leadership development. Most also predated the advent of important legislative changes, such as the Affordable Care Act, and none reflected perspectives on emerging challenges the health sector may face in the decade to come. We attempted to address each of these limitations with our present work, using approaches we describe in the next section.
Methods
We pursued this work in four major phases, as described below. All phases of the research work involving human subjects were reviewed and approved by the institutional review board of the primary author.
Phase 1: Future Scan
Our first phase involved conducting an environmental scan of future scenarios across a breadth of macrolevel trends, using the year 2030 as our temporal anchor. We identified resources for review based on a series of Internet searches using the terms “scenario planning,” “future scan,” and the year 2030 and supplemented these with searches on the websites of organizations that we knew were involved with ongoing future scanning activity based on our prior work (e.g., the Foresight Unit of the Organization for Economic Cooperation and Development; Institute for Alternative Futures; Institute for the Future; Society for Healthcare Strategy and Market Development).
Once these resources were compiled, we analyzed content using methods described in Garman, Johnson, and Royer (2011). The approach involves first reviewing each document to identify dominant trends or “future facts.” Future facts that appear across multiple scenarios are then organized into broad themes. We then reviewed the themes with a focus group of chief executives and chief human resource officers from a diverse group leading U.S. health systems (e.g., an integrated delivery system, a community health system, a children’s hospital, and an international academic health system) to ensure credibility and relevance. The resulting themes provided a perspective on emerging needs that the model revision should address, in addition to what the present-state analyses suggest.
Phase 2: Leadership Role Analyses
The next phase of our work involved assessing leadership roles. The approach we took followed the Behavioral Event Interviewing (BEI) methodology, adapted from Boyatzis (1982). The BEI method is designed to help ensure that the results objectively reflect true behavioral differentiators of successful leadership performance, rather than opinions or attributions. The method involves first identifying matched pairs of leaders, one representing outstanding (top decile) performance and the other representing typical (median) performance. Each leader is then individually interviewed about their work using a structured process that results in behavioral descriptions of critical incidents in the workplace. Behaviors most frequently contrasting the two performance levels can then also be identified as “distinguishing competencies.”
For this study, pairs of leaders at the early-and mid-career levels were recruited with assistance from executives of health systems participating in one or more of NCHL’s member programs. Four early and midlevel pairs were recruited from organizations participating in the National Council on Administrative Fellowships, with pairings based on organization and approximate time fellowship completion (3–5 years prior to the study). Four separate midlevel pairs of physician leaders were recruited from organizations participating in NCHL’s Physician Leadership Development Council. To assess leadership at the senior-most levels, we also recruited from “c-suite” roles. However, given the unique nature of these roles, identifying pairs of performance levels within health systems was not practical. For this group, we instead identified three senior leaders as high-performing based on their prior recognition as recipients of NCHL’s peer-refereed national award for excellence in leadership and paired each with a senior executive currently working within another health system.
With the consent of the interviewees, all interviews were audio-recorded and then transcribed, yielding a total of 825 individually codable behavioral descriptions of leadership. Behavioral descriptions were then reviewed against the current version of the NCHL competency model (Version 2.1), and where possible, statement matches were coded according to current competencies and levels within competencies. Individual behavioral statements that could not be mapped uniquely to a single competency were given a secondary coding, yielding 1,042 pairings to the original model. Once the mappings were complete, the Version 2.1 model was examined to identify any competencies or levels within competencies, for which none of the new behavioral statements matched. This step resulted in the elimination of a proficiency level within two of the competencies, as well as the separation of one of the competencies (communication) into two separate competencies (writing and speaking/facilitating). Next, behavioral statements from the interviews were compared to the legacy model to identify needs and opportunities to update language within the behavioral statements.
Once this process was completed, we organized the revised competencies into a seven-domain framework. The source framework was developed with the goal of providing a widely adaptable resource for professional leadership development programs as informed by four streams of relevant science: (a) research on leadership theory and leadership competencies in applied settings (cf. Yukl, 2012); (b) reviews of the emerging knowledge base about neuropsychological correlates of leadership (cf. Boyatzis & Jack, 2018; Waldman, Balthazard, & Peterson, 2011); (c) theoretical and conceptual reviews of corporate social responsibility, including the role of the professions (cf. Groves & LaRocca, 2011; Susskind & Susskind, 2016); and (d) systematic reviews of leadership development in practice and higher education settings (cf. Day et al., 2014; Day & Dragoni, 2015; Slavich & Zimbardo, 2012). Adaptations to the framework were made based on feedback from practitioner reviewers to enhance the relevance of descriptions to the health sector.
Phase 3: Assessment of Generalizability
To help ensure that results would be generalizable to other health sector settings and leadership roles, the resulting model was then reviewed by two focus groups of practicing executives. The first review was provided by chief diversity officers from NCHL’s Diversity and Inclusion Council, as part of a face-to-face meeting in Detroit in August 2017. The second review was provided by the steering committee of NCHL’s membership programs, as part of a face-to-face meeting in Milwaukee in October 2017. Revisions from these two groups focused on ensuring that language and descriptions would be sensible within the applied settings participants represented, as well as appropriately inclusive of leaders from a breadth of backgrounds.
The final step in assessing generalizability involved coding the model into an electronic survey for distribution to a broader and more diverse group of health sector leaders. Participants in this final survey step were drawn from three sources: (a) directors and preceptors of postgraduate administrative fellowship programs recruited from the National Council on Administrative Fellowships (n = 38); (b) health system learning executives and chief diversity officers recruited from other NCHL membership programs (n = 21); and (c) graduate health care managers working in a variety of settings at early, middle, and late career stages recruited from the alumni associations of three graduate health care management programs in the Midwestern United States (n = 89). Collectively, these groups formed a survey pool of 148 total respondents. On the survey, respondents were asked first to identify the setting in which they worked as well as the level within their organization. Next, participants were asked to review each competency description individually and evaluate how essential they believed it was to successful performance in leadership positions they were most familiar with. Using methods described by Lawshe (1975), we calculated content validity ratios (CVRs) to determine the level of agreement among raters regarding the importance of each competency to each of the managerial levels. The CVR mathematically combines elements of both item reliability and absolute rated value; acceptable CVR scores are determined by a combination of sample size, interrater agreement, and actual ratings provided.
Phase 4: Cross-Mapping to Other Health Sector Leadership Models
To assess the potential for the resulting model to also serve as a common platform across professions, we next identified comparison leadership models from the professions of medicine, nursing, social work, and health care management, as well as a general clinical leadership framework. These disciplines were chosen because they represent the four largest professions in the health sector by workforce size (World Health Organization, 2017). Models were identified through Internet searches using permutations of the search phrases “leadership competencies,” “leadership competency model,” and the names of the disciplines, which we supplemented with outreach to professional colleagues from these disciplines. For each category, we attempted to identify the model that appeared to have the most widespread application by virtue of the number and size of the professional associations and/or health sector organizations formally endorsing it. We also sought to have a mix of national and international models, as well as profession- and organization-focused models. Where more than one model met our criteria, we emphasized newer models. For medicine, we chose the leader role definition from the Royal College of Physicians and Surgeons of Canada (2018). For nursing, we selected the executive nurse model of the United States-based Association of Nurse Executives (2015). For social work, we used the management competency framework of the Network for Social Work Management (Hassan & Wimpfheimer, 2015). For health care management, we used the competency model adopted by the International Hospital Federation (2015). To help ensure relevance across health professions more broadly, we also included a general clinical leadership framework, the Clinical Leadership Competency Framework from the National Health Service Leadership Academy (2011).
Crosswalks between each of these models were conducted with the assistance of an internally developed natural language processing application (CrossBot, v1.2: Garman & Lindsey, 2017). The program calculates a statistical comparison (cosine similarity) between text passages using the open-source application Gensim (Rehurek & Sojka, 2010) and then flags the highest quality match for each competency in the model. Based on prior research assessing interrater concordance between natural language processing and human raters (Garman, Standish, & Kim, 2018), we set a minimum cutoff of 0.2 as representing an acceptable level of match. In cases where no competencies matched at that level, we considered the competency to be “unmatched.”
Results
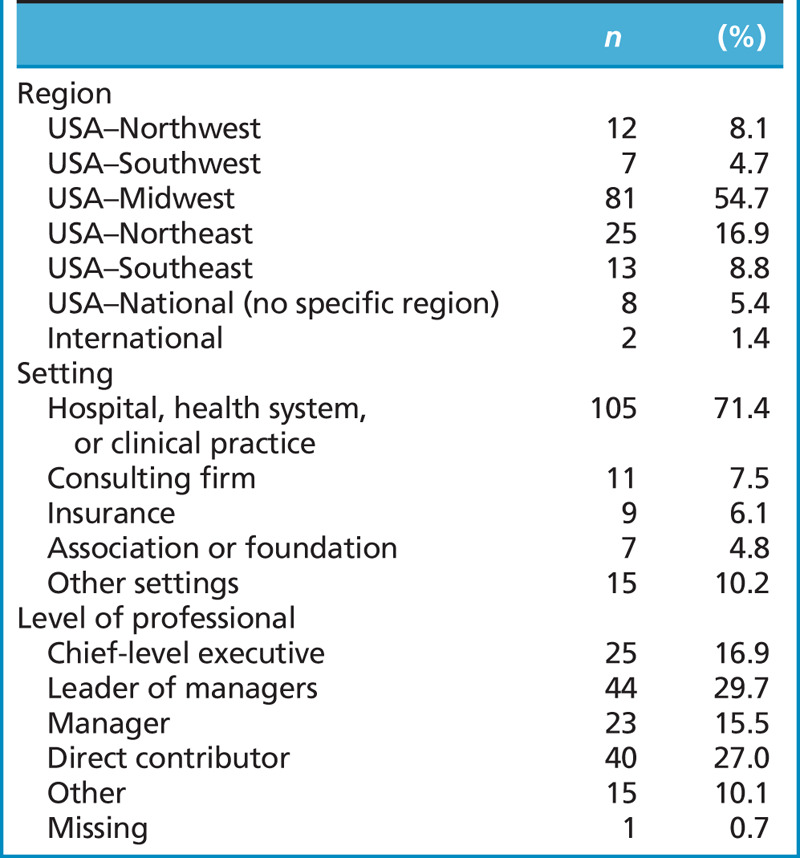
A demographic description of respondents to the content validation survey is provided in Table 1. Respondents represented all major regions of the United States, with the majority coming from the Midwest. Employment settings were primarily health systems and clinical practices; however, respondents also reported a variety of other employers, including consulting firms, insurance companies, associations, foundations, and other settings. Respondents were well distributed across organizational levels represented by survey respondents, with the majority self-identifying as manager level or above.
Table 1.
Demographics of survey respondents (n = 148)
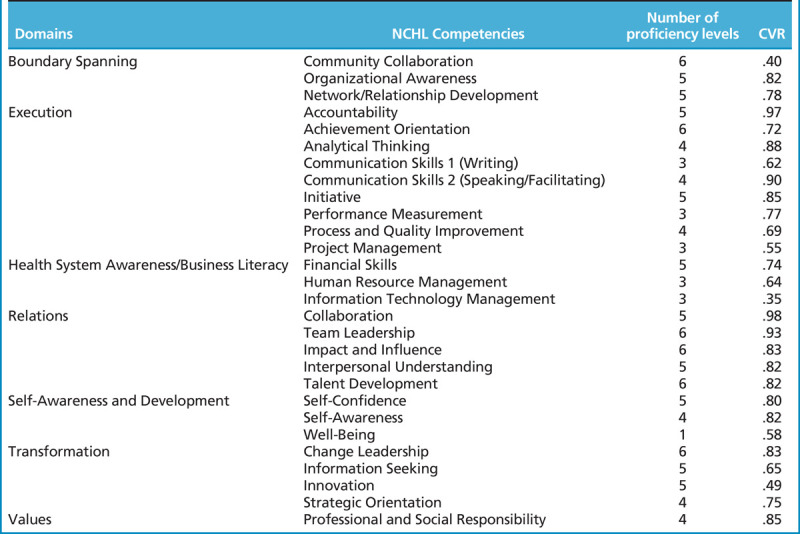
CVRs from the survey are reported in Table 2. Results indicated that all competencies exceeded the recommended cutoff values provided by Lawshe (1975). As such, all competencies that were tested at this stage were ultimately retained.
Table 2.
National Center for Healthcare Leadership competency model 3.0 domains, competencies, proficiency levels, and content validity ratios (CVRs) from the generalizability survey (n = 148)
Model Structure
The model resulting from this work contains 28 competencies, which are organized according to the seven domains depicted in Figure 1. The model identifies four “action” domains, representing leaders in the context of doing their work, as well as three “enabling” domains, representing leaders in the context of their preparation and/or development. Three of the action domains closely parallel domains from the original Version 2.1 model; the fourth, Boundary Spanning (“optimizing relationships between a leader’s span of control and the departments, organizations, communities and/or broader networks within which it operates”), is consistent with guidance from the Yukl (2012) research cited previously.
Figure 1.
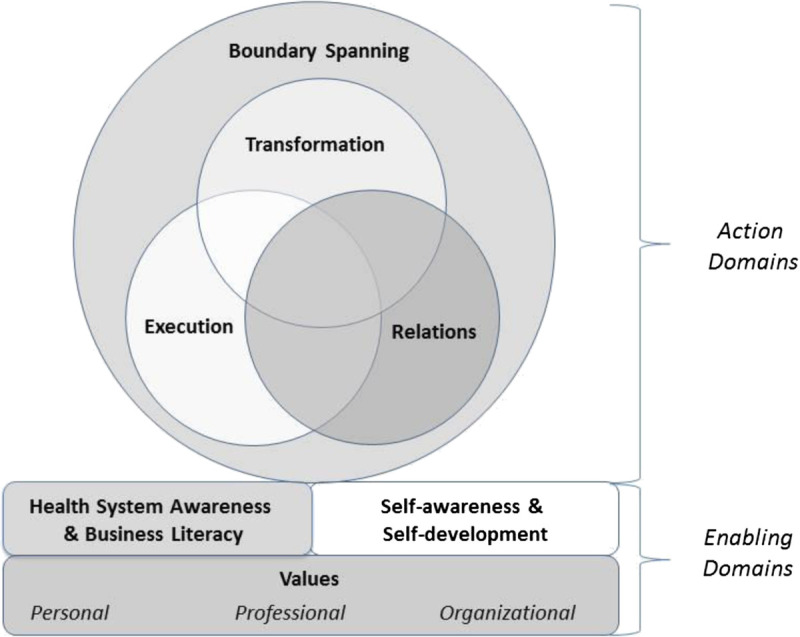
Transdisciplinary framework for leadership development in the health sector
The three “enabling” domains are also expansions from the Version 2.1 framework; however, in most cases, the changes reflect a more robust arrangement of competencies rather than the addition of new competencies. For example, Health System Awareness and Business Literacy, defined as “understanding the health system’s current business and operating frameworks as well as the dynamic context within which they operate (e.g., community, competitive, human resource, financial, legal, policy, and environmental),” is intended to be a flexible component that can house technical management competencies such as financial skills, human resource management, and information technology, as well as other management competencies that may be specific to an individual manager or organization. Self-Awareness and Development (“ongoing habits and actions taken to continuously improve self-knowledge, interpersonal effectiveness and well-being”) also houses two competencies evolved from the original model: Self-Awareness and Self-Confidence, as well as a new addition, Well-Being. The latter competency reflects an emerging recognition of the critical need to improve well-being within the health sector itself, as well as our growing understanding of the leader’s essential role in fostering a climate conducive to resilience (e.g., Shanafelt & Noseworthy, 2017). Lastly, Values was added as the third enabling domain. The Values domain houses the revised Professional and Social Responsibility competency and, as with the Health System Awareness domain, is also intended to flexibly house learning activities focused on the formation and clarification of professional and organizational values, which differ based on an individual’s professional background and setting. (Descriptions of the full model, including all competencies and levels within competencies, are available in the NCHL, 2018, publication or by contacting the primary author.)
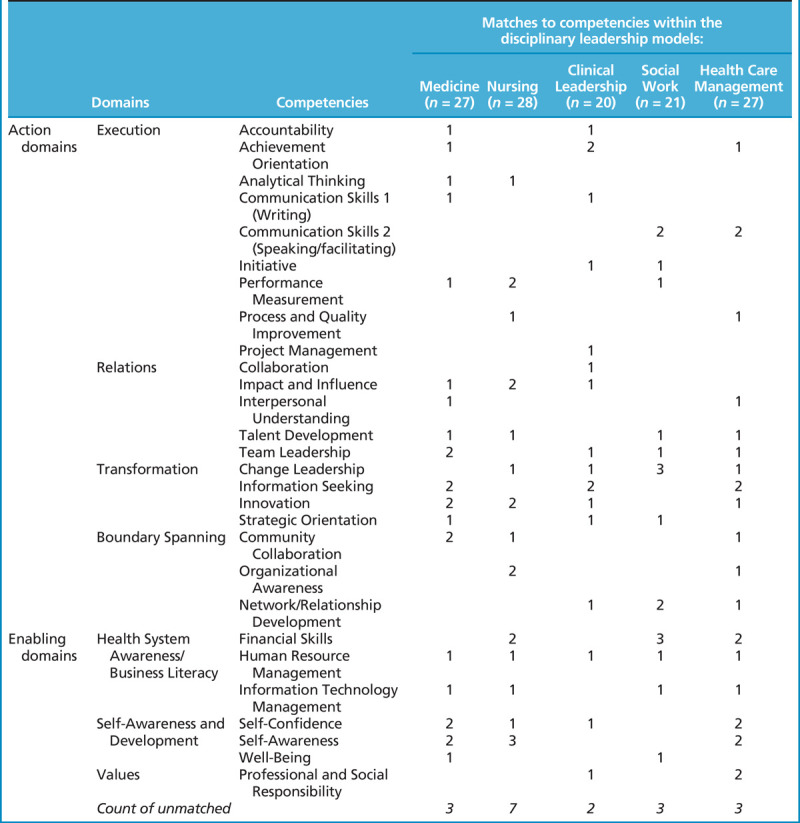
Assessment of Universality
Results of our crosswalk between the new NCHL model and the five health professions leadership models are summarized in Table 3. Using the cutoff of 0.2, we found that the NCHL model found matches for an average of 85% of the competencies across the five models. All five models also demonstrated matches across all four of the “action” domains as well as at least two of the three “enabling” domains (Health System Awareness and Business Literacy and Self-Awareness and Development). The third “enabling” domain, Values, did not match to three of the five models: medicine, nursing, and social work.
Table 3.
Count of competency matches (cosine similarities >0.2) between the transdisciplinary leadership model and leadership models from medicine, nursing, clinical leadership, and health care management
Discussion
Our results provide preliminary evidence that it is possible to map most of the content contained within many of the widely known health sector leadership competency models to a common framework. The framework we used, which was synthesized from the broader scientific literature on leadership competencies, provided a mapping for approximately 85% of the competencies we tested. Furthermore, many of the competencies that did not map did not technically meet our definition of “leadership,” typically because they related to the delivery of clinical care and not to activities among coworkers. Competencies from these models mapped broadly across the domains of the common framework, such that at least six of the seven domains mapped to multiple competencies from each model. The exception was the Values domain, which did not map to three of the models. This finding was unexpected, particularly given the central role values play in our understanding of the professions. In discussing these results with clinical leaders, the consensus interpretation was that clinical leadership models may reflect an underappreciation of the magnitude of differences between the values adopted as part of clinical training and the values that are associated with formal leadership roles. In particular, although clinically focused values tend to emphasize maximizing the outcomes of a given clinician’s patients, leadership values need to emphasize maximizing the stewardship of finite resources on behalf of a population of patients, consumers, or a community. The absence of values in these clinical leadership models may thus reflect a potential blind spot—a perspective that is consistent with recent writings about leadership in the health professions (cf. Begun, Butler, & Stefl, 2018; Frich & Spehar, 2018; Joseph & Huber, 2015).
Limitations and Future Studies
Although we believe we were able to follow current best practice guidelines closely throughout the competency modeling process, there are a number of limitations to the present work that are important to note. One relates to biases in our approaches to selecting of interviewees as well as survey participants. In terms of interviewees, the labor-intensive nature of the BEI process limited the number of interviews we were able to conduct, and there is a relatively greater degree of risk of sampling bias with a smaller pool of interviewees. There is even greater risk that differences within pairs of interviewees (i.e., “distinguishing competencies”) will not generalize reliably. In our executive sample, this limitation may have been further compounded by the approach we took to finding pairs for our outstanding performers, which was not standardized according to organization nor to third-party judgments of performance. In future work, we hope to add to the BEI data pool such that we will be able to report distinguishing competencies as part of future studies.
In terms of our survey participants, although our sample size may be large enough to provide a good assessment of content validity generally (Lawshe, 1975), generalizability remains a concern, especially given the overall heterogeneity of the health sector. Although we sought participation from a broad representation of health sector organizations, our demographics clearly reflected a bias toward health systems. To the extent that the broader health ecosystem reflects a diversity of leadership competencies, aspects of this diversity may not be fully reflected in our results. Lastly, to the extent that some participants may have had prior knowledge about the NCHL and/or other leadership competency models, this knowledge could conceivably have created a response set that affected their responses to the validation survey. Because we did not ask participants about this as part of the study process, this potential effect is not possible for us to determine retrospectively.
Practice Implications
The availability of a universally applicable framework for leadership development in health can provide several important benefits for practitioners. A universal model may be particularly helpful for framing learning programs involving multiple disciplines, such as the leadership development academies operated by many health systems, as well as programs of higher education. The domain-level approach can also provide a high-level starting point for prioritizing individual leadership development needs, which may provide a more manageable mental model to work with. For example, if leaders want to improve their capacity to meet operating goals, they might first prioritize the Execution domain and then prioritize competencies within that domain for future development. Alternatively, if future success will require stronger relationships with other departments or organizations, they might first prioritize the Boundary Spanning domain and then consider the competencies it contains.
A universal framework can also be a useful tool for consolidating leadership development activities in health systems that are seeking to centralize, consolidate, and/or strategically align existing leadership development programs. In health systems where leadership development has been delivered in profession-specific ways and/or within local departments or health systems, leaders and participants of these programs often feel a strong sense of “ownership” over these programs and may each believe that their model should prevail. In these contexts, a universal model can provide a helpful “neutral territory” in which legacy models can be more objectively integrated or at least interoperated.
At the interorganizational level, a universal model can provide greater efficiency in developing new learning programs and resources. In particular, there are often more similarities than differences in the leadership development challenges faced by health systems within a given country or region. When health systems adopt similar nomenclatures to describe these challenges, they are in a better position to pursue common solutions, which can be more efficient and more effective than working separately on similar challenges. The many existing learning collaboratives and professional forums within health care can provide ready platforms for such work.
Conclusion
As the roles of health systems grow more complex and the pace of change continues to increase, health sector organizations must efficiently and effectively attend to the leadership development needs of a broad and inclusive complement of staff. In the work described in this article, we sought to develop a model that had not only strong empirical underpinnings but also an accessible resource for interprofessional leadership work. We hope that this revision contributes to more robust and inclusive approaches to leadership development in health sector organizations, empowering a much broader range of professionals to lead.
Footnotes
This study was supported by departmental funding from Rush University.
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
References
- Acosta J. Chandra A., & Madrigano J. (2017). An agenda to advance integrative resilience research and practice: Key themes from a resilience roundtable. RAND Health Quarterly, 7, 5. [PMC free article] [PubMed] [Google Scholar]
- Association of Nurse Executives. (2015). Nurse executive competencies. Retrieved from http://www.aone.org/resources/nec.pdf
- Begun J. W. Butler P. W., & Stefl M. E. (2018). Competencies to what end? Affirming the purpose of healthcare management. Journal of Health Administration Education, 35, 133–155. [Google Scholar]
- Boyatzis R. E. (1982). The competent manager: A model for effective performance. New York, NY: John Wiley & Sons. [Google Scholar]
- Boyatzis R. E., & Jack A. I. (2018). The neuroscience of coaching. Consulting Psychology Journal: Practice & Research, 70(1), 11–27. [Google Scholar]
- Brewer M. L. Flavell H. L. Trede F., & Smith M. (2016). A scoping review to understand “leadership” in interprofessional education and practice. Journal of Interprofessional Care, 30(4), 408–415. [DOI] [PubMed] [Google Scholar]
- Cabral J. Garman A. N., & Moscola J. (2018, March). Preparing healthcare leaders for the decade to come: Long-term trends and their associated development implications. Presentation at the Annual Congress of the American College of Healthcare Executives, Chicago, IL.
- Calhoun J. G. Dollett L. Sinioris M. E. Wainio J. A. Butler P. W. Griffith J. R., & Warden G. L. (2008). Development of an interprofessional competency model for healthcare leadership. Journal of Healthcare Management, 53(6), 375–389. [PubMed] [Google Scholar]
- Campion M. A. Fink A. A. Ruggeberg B. J. Carr L. Phillips G. M., & Odman R. B. (2011). Doing competencies well: Best practices in competency modeling. Personnel Psychology, 64, 225–262. [Google Scholar]
- Crowe D. Garman A. N. Li C. C. Helton J. Anderson M. M., & Butler P. (2017). Leadership development practices and hospital financial outcomes. Health Services Management Research, 30(3), 140–147. [DOI] [PubMed] [Google Scholar]
- Day D. V., & Dragoni L. (2015). Leadership development: An outcome-oriented review based on time and levels of analyses. Annual Review of Organizational Psychology and Organizational Behavior, 2(1), 133–156. [Google Scholar]
- Day D. V. Fleenor J. W. Atwater L. E. Sturm R. E., & McKee R. A. (2014). Advances in leader and leadership development: A review of 25 years of research and theory. The Leadership Quarterly, 25(1), 63–82. [Google Scholar]
- Franklin C., & Lytle R. (2015). Employer perspectives on competency-based education. Burlington, MA: Center on Higher Education Reform, American Enterprise Institute. [Google Scholar]
- Frich J. C., & Spehar I. (2018). Physician leadership development: Towards multidisciplinary programs? BMJ Leader, 2, 91–94. [Google Scholar]
- Garman A. N., & Johnson M. P. (2006). Leadership competencies: An introduction. Journal of Healthcare Management, 51(1), 13–17. [PubMed] [Google Scholar]
- Garman A. N. Johnson T. J., & Royer T. (2011). The future of healthcare: Global trends worth watching. Chicago, IL: Health Administration Press. [Google Scholar]
- Garman A. N. Lemak C. H., & Standish M. P. (2018). Future trends: Implications for leadership. In Rubino L. G. Esparza S. J., & Chassaikos Y. (Eds.), New leadership for today’s health care professionals (2nd ed.). Burlington, MA: Jones & Bartlett. [Google Scholar]
- Garman A. N., & Lindsey Z. (2017). CrossBot v1.2—A Gensim-enabled Python program to automate competency crosswalks (Working paper). Burlington, MA: Rush University HSM Leadership Center. [Google Scholar]
- Garman A. N. Standish M. P., & Kim D. H. (2018). Enhancing efficiency, reliability and rigor in competency model analysis using natural language processing. Journal of Competency-Based Education, e01164. doi: 10.1002/cbe2.1164 [DOI] [Google Scholar]
- Groves K. S., & LaRocca M. A. (2011). An empirical study of leader ethical values, transformational and transactional leadership, and follower attitudes toward corporate social responsibility. Journal of Business Ethics, 103(4), 511–528. [Google Scholar]
- Hassan A., & Wimpfheimer R. (2015). Human services management competencies. Retrieved from https://socialworkmanager.org/wp-content/uploads/2016/01/Competency-Brochure-4-19-15-With-Forms.pdf
- International Hospital Federation. (2015). Leadership Competencies for Healthcare Services Managers. Retrieved from https://www.ihf-fih.org/resources/pdf/Leadership_Competencies_for_Healthcare_Services_Managers.pdf
- Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 Update. Retrieved from https://www.ipecollaborative.org/resources.html
- Joseph M. L., & Huber D. L. (2015). Clinical leadership development and education for nurses: Prospects and opportunities. Journal of Healthcare Leadership, 7, 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelchen R. (2015). The landscape of competency-based education: Enrollments, demographics, and affordability. Burlington, MA: Center on Higher Education Reform, American Enterprise Institute. [Google Scholar]
- Lawshe C. H. (1975). A quantitative approach to content validity. Personnel Psychology, 38(4), 563–575. [Google Scholar]
- Li C. Barth P. Garman A. N. Anderson M. A., & Butler P. (2017). Leadership development practices and patient satisfaction: A study of U.S. academic medical centers. Patient Experience Journal, 4(1), 97–102. [Google Scholar]
- Lord R. G. Day D. V. Zaccaro S. J. Avolio B. J., & Eagly A. H. (2017). Leadership in applied psychology: Three waves of theory and research. Journal of Applied Psychology, 102(3), 434–451. [DOI] [PubMed] [Google Scholar]
- Lucas R. Goldman E. F. Scott A. R., & Dandar V. (2018). Leadership development programs at academic health centers: Results of a national survey. Academic Medicine, 93(2), 229–236. [DOI] [PubMed] [Google Scholar]
- McClelland D. C. (1973). Testing for competence rather than for “intelligence.”. American Psychologist, 28(1), 1–14. [DOI] [PubMed] [Google Scholar]
- National Center for Healthcare Leadership. (2018). Health leadership competency model 3.0. Retrieved from http://www.nchl.org
- National Health Service Leadership Academy. (2011). Clinical Leadership Competency Framework. Retrieved from https://www.leadershipacademy.nhs.uk/
- Prahalad G. K., & Hamel G. (1990). The core competence of the corporation. Harvard Business Review, 68(3), 79–91. [Google Scholar]
- Rehurek R., & Sojka P. (2010). In Software framework for topic modeling with large corpora (Ed.), Proceedings of the LREC workshop new challenges for NLP frameworks. Valletta, Malta: University of Malta. [Google Scholar]
- Royal College of Physicians and Surgeons of Canada. (2018). “Leader.”. Retrieved from http://www.royalcollege.ca/rcsite/canmeds/framework/canmeds-role-leader-e
- Schippman J. S. Ash R. A. Battista M. Garr L. Eyde L. D. Hesketh B., … Sanchez I. (2000). The practice of competency modeling. Personnel Psychology, 53(3), 703–740. [Google Scholar]
- Seemiller C., & Murray T. (2013). The common language of leadership. Journal of Leadership Studies, 7(1), 33–45. [Google Scholar]
- Shanafelt T. D., & Noseworthy J. H. (2017). Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clinic Proceedings, 92(1), 129–146. [DOI] [PubMed] [Google Scholar]
- Slavich G. M., & Zimbardo P. G. (2012). Transformational teaching: Theoretical underpinnings, basic principles, and core methods. Educational Psychology Review, 24(4), 569–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Society for Healthcare Strategy and Market Development (2017). Futurescan 2018–2023: Healthcare trends and implications. Chicago, IL: Health Administration Press. [Google Scholar]
- Stefl M. E. (2008). Common competencies for all healthcare managers: The Healthcare Leadership Alliance model. Journal of Healthcare Management, 53, 360–373. [PubMed] [Google Scholar]
- Stetz T. A., & Chmielewski T. L. (2015). In Competency modeling documentation (Ed.), SHRM-SIOP White Paper Series. Retrieved from https://www.shrm.org/hr-today/trends-and-forecasting/special-reports-and-expert-views/Documents/SHRM-SIOP%20Competency%20Modeling%20Documentation.pdf
- Stogdill R. M. (1974). Handbook of leadership: A survey of theory and research. New York, NY: The Free Press. [Google Scholar]
- Susskind R., & Susskind D. (2016). The future of the professions: How technology will transform the work of human experts. Oxford University Press. [Google Scholar]
- Tett R. P. Guterman H. A. Bleier A., & Murphy P. J. (2000). Development and content validation of a “hyperdimensional” taxonomy of managerial competence. Human Performance, 13(3), 205–251. [Google Scholar]
- Waldman D. A. Balthazard P. A., & Peterson S. J. (2011). Leadership and neuroscience: Can we revolutionize the way that inspirational leaders are identified and developed? Academy of Management Perspectives, 25(1), 60–74. [Google Scholar]
- World Health Organization. (2017). Global health workforce statistics: 2017 Update. Retrieved from http://www.who.int/hrh/statistics/hwfstats/
- Yukl G. (2012). Effective leadership behavior: What we know and what questions need more attention. Academy of Management Perspectives, 26(4), 66–85. [Google Scholar]


