Abstract
Objective
to assess the epidemiology and features of de novo surgical diseases in patients admitted with COVID-19, and their impact on patients and healthcare system.
Summary background data
Gastrointestinal involvement has been described in COVID-19; however, no clear figures of incidence, epidemiology and economic impact exist for de-novo surgical diseases in hospitalized patients.
Methods
This is a prospective study including all patients admitted with confirmed SARS-CoV-2 rT-PCR, between 1 March and 15 May 2020 at two Tertiary Hospitals. Patients with known surgical disease at admission were excluded. Sub-analyses were performed with a consecutive group of COVID-19 patients admitted during the study period, who did not require surgical consultation.
Results
Ten out of 3089 COVID-19 positive patients (0.32%) required surgical consultation. Among those admitted in intensive care unit (ICU) incidence was 1.9%. Mortality was 40% in patients requiring immediate surgery and 20% in those suitable for conservative management. The overall median length of stay (LOS) of patients admitted to ICU was longer in those requiring surgical consultation compared with those who did not (51.5 vs 25 days, p = 0.0042). Patients requiring surgical consultation and treatment for de-novo surgical disease had longer median ICU-LOS (31.5 vs 12 days, p = 0.0004). A median of two post-surgical complications were registered for each patient undergoing surgery. Complication-associated costs were as high as 38,962 USD per patient.
Conclusions
Incidence of de-novo surgical diseases is low in COVID-19, but it is associated with significant morbidity and mortality. Future studies should elucidate the mechanism underlying the condition and identify strategies to prevent the need for surgery.
Keywords: COVID-19, Complications, Costs, Surgical disease, SARS-CoV-2
Introduction
The outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-COV-2) was initially detected in Wuhan, capital of Hubei, province of China in December 20191, 2, 3 as pneumonia of unknown origin. On January 8th the novel Coronavirus was officially announced as the causative pathogen by the Chinese Centre for Disease Control and Prevention4 and it was named Coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) in February of 2020.5 On March 12th the WHO declared COVID-19 a pandemic.6 More than 26 million people have been infected, with over 864,000 deaths.7 Hospitalized patients requiring ICU admission are calculated around a 25%.8
In relation to surgery, poorer outcomes are associated after surgery in COVID-19-positive patients. Up to 44% of patients undergoing elective surgery during the COVID-19 incubation period might need postoperative Intensive Care Unit (ICU) care, with a mortality rate of 20.5%.9 Hence, most surgical societies recommend conservative management of COVID-19-positive patients presenting with some urgent surgical diseases.10 , 11 COVID-19 patients might develop de-novo surgical diseases during hospitalization, requiring surgical consultation and treatment.
Spain is currently the most affected country in Europe with 488,513 confirmed cases and 29,234 death by the 3rd September 2020.7 , 12 Recent reports suggest that, in Catalonia Region, the toll of deaths related to COVID-19 exceeded 12,954 cases, when fatalities based on data from funeral services are taken into account.13 Reporting on the Spanish experience could be useful at a time when some countries have not yet “flattened the curve” and new infection waves are predicted.
This study aims to assess the epidemiology, features, economic burden and outcome of late-onset surgical diseases in patients treated for COVID-19 in two Catalan hospitals, one of the most affected regions in Spain.
Methods
This is a prospective, STROBE-compliant, observational study performed at Vall d’Hebrón University Hospital and Bellvitge University Hospital. Ethical Committee approval was obtained.
Eligibility criteria
All hospital admitted patients, 18-years-old or older, with confirmed COVID-19 were prospectively assessed for inclusion (March 1–May 15). Patients who required surgical consultation/review during admission were identified. Patients who were admitted with a known surgical disease were not included, as well as patients without confirmed diagnosis of COVID-19.
Endpoint and outcome of interest
The primary endpoint was the incidence of late-onset surgical diseases in COVID-19 positive patients, the associated morbidity and outcome. All complications occurring after consultation and any therapies by the surgical team were used as outcome measures.
The secondary endpoints included mortality and the estimated costs associated with the complications.
Definitions
Collected data included demographics, underlying comorbidities and medications, date of hospitalization and discharge, testing pathway and date, length of stay, length of ICU stay, medical treatment received for COVID-19, date of surgical consultation, treatment received for the surgical condition, treatment results, surgical complications, mortality cause and date. In all patients included in the analysis who were admitted to ICU, ICU admission was due to COVID-19.
COVID-19 diagnosis was confirmed by SARS-CoV-2 reverse transcriptase-polymerase chain reaction (RT-PCR) testing with throat and nasal swab samples. In some patients, a chest CT was initially performed,14 with posterior RT-PCR confirmation.
Consultation and treatment for the following surgical diseases during hospitalization were included: bowel ischemia and/or perforation, bowel obstruction, appendicitis, cholecystitis, pancreatitis, peritonitis, and additional disease of surgical interest.
All surgical treatments were assessed, including watchful monitoring, medical therapy (e.g. antibiotics or any review/modification of current treatment by the surgical team), percutaneous drainage, and surgery. Surgical assessment of included patients always included imaging or surgery. Complications were graded according the Clavien-Dindo classification15 and the Comprehensive Complication Index (CCI) score.16
The complication costs were determined by CCI class for each procedure performed and patient age using the AssessSurgery tool (AssessSurgery.com).
Statistical analysis
Categorical data are presented as absolute numbers and percentages, whereas continuous variables are presented as median with ranges. A descriptive analysis was performed to report on the incidence and outcomes of de novo surgical diseases.
The overall incidence was computed by determining the rate of patients requiring surgical consultation among the entire number of patients who were admitted for COVID-19 at both Centers in the study period. Sub-analyses were performed to assess the LOS and outcomes in patients who needed ICU stay in the group who developed de-novo surgical disease during admission vs. a consecutive group of COVID-19 patients who did not require surgical consultation. For the control group, only patients with completely available data were considered.
The Fisher's exact test was used to compare categorical data, whereas the Mann–Whitney U test was used for continuous data. A p value < 0.05 was considered statistically significant.
Results
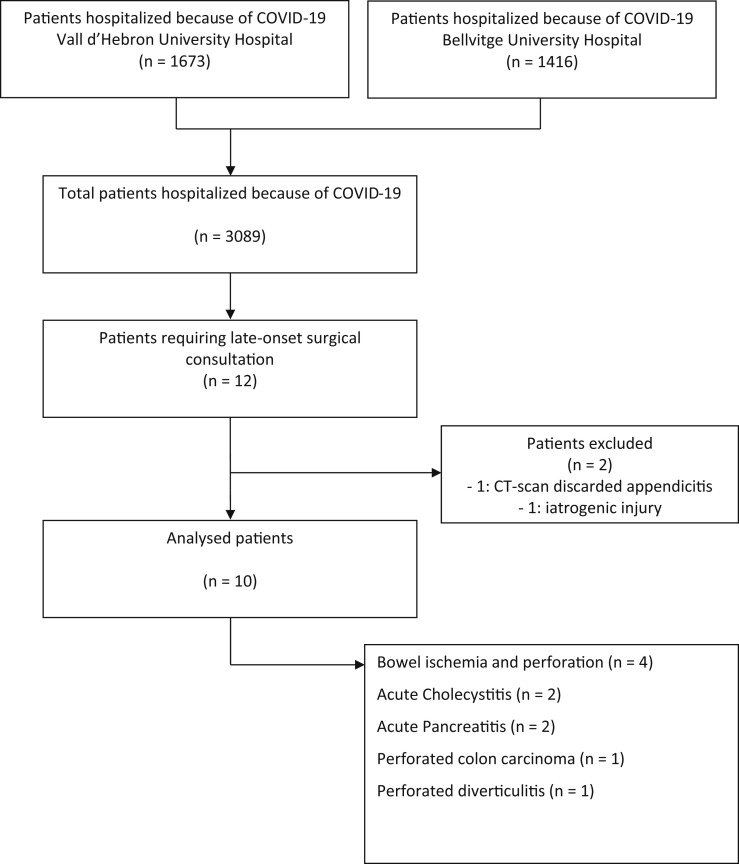
Between March the 1st and May the 15th 2020, 3089 patients were admitted with proven COVID-19 with no signs or symptoms of abdominal surgical diseases at both hospitals; of which 12 (0.39%) required surgical consultation. One patient was excluded from the final analysis because a CT scan ruled out appendicitis and another because surgical consultation was required because of an iatrogenic injury. Therefore, 10 patients required surgical consultation and treatment, accounting for 0.32% of admitted patients with COVID-19. When only patients already admitted to the ICU were considered, the incidence was 1.9% (8/409).
Out of 10 patients who required consultation, four (40%, 4/10) were diagnosed with bowel ischemia and perforation, two (20%, 2/10) with acute cholecystitis, two (20%, 2/10) with acute pancreatitis, one (10%, 1/10) with perforated colon carcinoma, and one (10%, 1/10) with perforated diverticulitis. Flowchart of patient selection is represented in Fig. 1 .
Fig. 1.
Flowchart.
Patient characteristics are detailed in Table 1 . A median of 18 (3–28) days passed between admission and surgical consultation.
Table 1.
Characteristic of patients who required surgical consultation during admission for COVID-19.
| Characteristics | Patients (n = 10) |
| Age, yr median | 63.5 (46–72) |
| Male | 6 (60%) |
| BMI, kg/m2 median (range) | 28.2 (23.9–49.4) |
| Comorbidities | |
| Peripheric vascular disease | 1 (10%) |
| Dementia | 1 (10%) |
| COPD | 1 (10%) |
| Diabetes mellitus | 1 (10%) |
| Peptic ulcer disease | 1 (10%) |
| Solid tumor | 1 (10%) |
| Charlson comorbidity index | |
| 2 | 6 (60%) |
| 3 | 2 (20%) |
| 4 | 1 (10%) |
| 6 | 1 (10%) |
| ASA score | |
| I | 4 (40%) |
| II | 4 (40%) |
| III | 2 (20%) |
| SARS-CoV-2 RT-PCR testing | 10 (100%) |
| Length of stay, days median (range) | 44.5 (11–108) |
| Length of ICU stay, days median (range) | 28.5 (0–104) |
| Length of stay before surgical consultation, days median (range) | 18 (3–28) |
BMI: Body Mass Index; COPD: Chronic Obstructive Pulmonary Disease; ASA: American Society of Anesthesiologists' score; ICU: Intensive Care Unit.
The reason for consultation is reported in Table 2 , along with therapeutic decisions and outcomes.
Table 2.
Reason for surgical consultation and outcome, including costs associated with complications.
| Pt | Age | Gender | BMI | Comorbidities | Charlson | ASA | LOS | ICU |
Surgical disease | Treatment | CD | CCI | Estimated costs for complications | COVID-19 complications | Mortality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LOS | |||||||||||||||
| 1 | 62 | F | 29.2 | None | 2 | 1 | 76 | 66 | Bowel ischemia – perforation | Right Hemicolectomy | 2 | 33.2 | 31,742 USD | ARDS, GBS, PTE | No |
| 2 | 72 | M | 28.6 | Diabetes mellitus | 4 | 2 | 54 | 47 | Perforated colon cancer | Right Hemicolectomy | 5 | 100 | 80,871 USD | ARDS, ARF, delirium, myopathy, | Yes |
| 3 | 57 | F | 25,9 | COPD | 2 | 3 | 18 | 18 | Bowel ischemia – perforation | Right Hemicolectomy | 5 | 100 | 80,871 USD | ARDS, ARF, CRS | Yes |
| 4 | 64 | M | 24.6 | None | 2 | 1 | 40 | 29 | Acute biliary Pancreatitis | Watchful monitoring | – | – | – | ARDS, PTE + PVT, Pneumothorax, | No |
| 5 | 62 | M | 49.4 | None | 2 | 2 | 21 | 18 | MAT + massive bowel ischemia | Symptom control/palliation | – | – | – | ARDS, PTE + PVT | Yes |
| 6 | 72 | M | 29.8 | Dementia, Hypophysis adenoma | 6 | 3 | 49 | 28 | Perforated Diverticulitis | Hartmann Procedure | 2 | 22.6 | 30,854 USD | ARDS | No |
| 7 | 60 | M | 27.8 | Peripheral Vascular Disease | 3 | 2 | 11 | 0 | Acute biliary Cholecystitis | Percutaneous Cholecystostomy | – | – | – | None | No |
| 8 | 69 | F | 23.9 | None | 2 | 2 | 108 | 104 | Bowel ischemia – perforation | Transverse Colectomy | 2 | 22.6 | 27,365 USD | ARDS, myopathy, BSI | No |
| 9 | 65 | M | 25.9 | None | 2 | 1 | 63 | 34 | Acute biliary Cholecystitis | Percutaneous Cholecystostomy | – | – | – | PTE, Ischemic colitis, BSI | No |
| 10 | 46 | F | 29.9 | PUD, Ulcerative Colitis | 1 | 1 | 14 | 0 | Non-biliary Acute Pancreatitis | Watchful monitoring | – | – | – | None | No |
BMI: Body Mass Index; LOS: Length of stay; ICU: Intensive care unit; CD: Clavien-Dindo classification; CCI: cumulative complication index; F: Female; M: Male; ARDS: Acute Respiratory Distress Syndrome; GBS: Guillain Barré Syndrome; PTE: Pulmonary thromboembolism; ARF: Acute Renal Failure; COPD: Chronic Obstructive Pulmonary Disease; CRS: Catheter-related sepsis; PVT: Peripheral Vascular Thrombosis; MAT: Mesenteric Arterial Thrombosis; BSI: Bacterial Superinfection; PUD: Peptic Ulcer Disease.
Out of four patients with bowel ischemia, this occurred in the right colon/terminal ileum in two (50%, 2/4), and at the transverse colon in one (25%, 1/4), whereas one patient had massive small bowel ischemia due to mesenteric arterial thrombosis that could not be treated by interventional radiology. The latter patient was offered palliative treatment, whereas the other three were operated on. Overall, five patients had a bowel perforation, and all underwent open surgery with no anastomosis, because of clinical instability. One of them (20%, 1/5) died within 24 h from surgery because of multi-organic sepsis. One patient (20%, 1/5) with perforated colon cancer died after myocardial infarction, five weeks after surgery.
Two patients were diagnosed with acute cholecystitis and underwent cholecystostomy. Two patients were diagnosed with acute pancreatitis, one of them with a 16-cm collection. Watchful monitoring was decided, which proved successful, with clinical and radiological improvement in subsequent CT scans.
The pathology report of the patient with the perforated colon cancer was consistent with a G2, pT3N0 adenocarcinoma with a 30% mucinous component. Perforation and invasion of small vessels was found. In two of the three ischemic perforations, involvement of small and medium vessels was observed, and micro-thrombosis in one.
Thirteen complications occurred in the five patients who underwent surgery, with a median of two (range 1–4) complications per patient. These ranged from wound infection to multi-organ failure and death (Table 2). Each patient developed at least one complication.
The overall median LOS was 44.5 (range 11–108), the median LOS in ICU was 28.5 (0–104) days.
LOS and mortality of patients admitted to ICU who required surgical consultation were compared with a consecutive group of 272 patients who were admitted to ICU for COVID-19 and did not require surgical consultation. The overall median LOS of those admitted to ICU was longer in those who required surgical consultation, being 51.5 (range 18–108) vs 25 (range 2–72) days, surgical consultation group vs. controls (p = 0.0042). Patients who needed surgical consultation and treatment for de-novo surgical diseases had a median of 19.5 days longer LOS in ICU compared with controls (31.5 [range 18–104] vs. 12 [1–62] days, p = 0.0004).
Overall, mortality was 30% (3/10). Among those who needed immediate surgery, mortality was 40% (2/5) and 20% (1/5) in those suitable for conservative management. Mortality in patients who required surgical consultation during their ICU stay was 37.5% (3/8), which was higher but not statistically different from mortality in the control group of patients who did not require surgical consultation (20.22%, 55/272, p = 0.369).
Overall, the costs associated with the surgical complications were as high as 311,703 USD, with median costs of 38,962 (range 27,365–80,871) USD for each operated patient.
Discussion
In this study, the overall incidence of de-novo surgical disease in hospitalized patients for COVID-19 was 0.32% in two tertiary hospitals during the peak phase of the pandemic, which increased to 1.9% when only considering patients already admitted in ICU for COVID-19. Mortality in those who required surgery was twice as high as that previously reported in COVID-19 patients presenting with abdominal diseases. The onset of de-novo surgical diseases negatively impacts on hospital resources, increasing the overall LOS and stay in ICU, and postoperative complications, which are frequent in this group of patients. This significantly increases the care associated costs.
Previous studies on non-COVID-19 patients reported that approximately 1–1.5% of patients in ICU develop an ICU-acquired abdominal sepsis.17 It has been suggested that late-onset abdominal sepsis accounts for 15% of all cases of abdominal sepsis in ICU.18 We found that the incidence of abdominal complications not present at the time of admission is overall negligible in confirmed COVID-19-patients; however, in the subgroup of patients admitted to ICU, the rate is higher. A study on 141 critically-ill COVID-19 patients, found that five needed surgery for abdominal conditions (3.5%), mainly represented by bowel ischemia19; when only cases with no signs/symptoms of abdominal disease at admission are evaluated, the rate might be lower. Gastrointestinal involvement is common in COVID-19 patients in ICU, and may be managed with conservative approach depending on the involved pathology and the diseases progression.19
Involvement of small vessels and viral entero-neuropathy has been suggested to occur in COVID-19 patients, and might be responsible for the relatively high number of patients with bowel ischemia and ileus.19 In our series, all patients with bowel perforation had involvement of small vessels at pathology, suggesting that the virus itself might be responsible for the condition rather than the treatments delivered. Even if the small sample size does not allow definitive conclusions, future studies should elucidate the pathophysiology of surgical diseases in patients with COVID-19.
The overall number of COVID-19 patients who need surgical consultation for de-novo surgical disease is low, but there are aspects that need to be carefully considered and might be relevant.
Complications are common in patients who undergo surgery during COVID-19 infection, and all patients in this series developed at least one complication. Postoperative mortality has been reported to occur in almost 24% of COVID-19-positive patients.19 Even in patients undergoing elective surgery with known diagnosis of COVID-19 death rate is non-negligible (9.1%).20 Figures might be higher when de-novo surgical diseases occur, with up to 37.5% mortality in ICU patients with COVID-19. Differently from the usual causes of death reported in COVID-19 patients, mainly pulmonary complications,8 , 20 in this series, most patients died as a consequence of systemic sepsis. Compared with COVID-19 patients in ICU who did not require surgical consultation, mortality was almost doubled in those who required input from the surgical team, but the small sample size should be taken into account (p=0.369).
Discussing care-associated cost might be useful, given the resource shortage that has been reported during the mitigation phase, and the backlog of procedures that need to be performed in the upcoming months.21 It has been estimated that COVID-19 will cause 654.0 USD billion in direct costs in the US over the course of the pandemic should 8% of the population be infected.22
Early predictions in Spain suggested that 1800 billion Euros would be required to face the pandemic.23 Mechanical ventilation is associated with incremented costs, which are already high in COVID-19 patients. The first two days are usually the most expensive as mechanical ventilation is often needed, whereas costs become more stable from day 3 of ICU stay (mechanical ventilation, 3968 USD; no mechanical ventilation, 3184 USD).24 In our series, the LOS in ICU was in median almost 3 weeks longer in patients with de novo surgical disease compared with patients who did not need surgical consultation (p = 0.0004). This generate much higher costs than can be predicted, since – after surgery – patients may need prolonged use of ventilators.
Postoperative complications add to the aforementioned costs. A median of two complications per patient occurred in the patients who underwent surgery, meaning that the costs for each patient increased by approximately 38,962 USD.
Study limitations
The relatively small sample size requires that findings are interpreted with caution. The cost estimates were approximated and might have been higher in the context of the pandemic.
However, this study was conducted prospectively on patients from two of the larger tertiary centres in Spain, with high volume of COVID-19 patients treated. Incidence could be reliably estimated, and the morbidity and complication-associated costs might be useful in managing patients with such presentation.
The incidence of de-novo surgical disease is low in COVID-19, similar to non-COVID-19 critically ill patients. However, clinical symptoms should be detected and surgical review obtained, due to unacceptably high associated morbidity and mortality. Surgical treatment prolongs admission in ICU and increases costs of care. Conservative treatment is a safe option, when possible.
Future studies should elucidate the mechanism underlying the condition, e.g. hypercoagulability and thrombo-inflammation in COVID-19 patients,25, 26, 27 and identify strategies to prevent the need for surgery.
Informed consent
Informed oral consent was obtained from all individual participants included in the study, following the recommendations of our ethical committees due to the pandemic.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020 doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D.S., Azhar I.E., Madani T.A., Ntoumi F., Kock R., Dar O. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health: the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gao Y., Shi C., Chen Y., Shi P., Liu J., Xiao Y. A cluster of the Corona Virus Disease 2019 caused by incubation period transmission in Wuxi, China. J Infect. 2020;80(6):666–670. doi: 10.1016/j.jinf.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation . WHO; Geneva: 2020. WHO director general's opening remarks at the media briefing on COVID-19–11 March 2020. [Google Scholar]
- 7.Center for Systems Science and Engineering (CSSE), Johns Hopkins University The COVID-19 Dashboard. https://coronavirus.jhu.edu/map.html Available at: [accessed 03.09.2020]
- 8.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. Published 2020 Apr 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aranda-Narváez J.M., Tallón-Aguilar L., Pareja-Ciuró F., Martín-Martín G., González-Sánchez A.J., Rey-Simó I. Emergency surgery and trauma care during COVID-19 pandemic. Recommendations of the Spanish Association of Surgeons. Cirugia Espanola. 2020 Apr doi: 10.1016/j.ciresp.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS. Royal College of Surgeons of England. The Royal College of Surgeons of Edinburgh . 16 March 2020. Clinical guide for the management of surgical patients during the coronavirus pandemic.https://www.england.nhs.uk/coronavirus/wpcontent/uploads/sites/52/2020/03/specialty-guide-surgery-and-coronavirus-v1.pdf [Google Scholar]
- 12.Instituto de Salud Carlos III. Ministerio de Sanidad. Gobierno de España Situación de COVID-19 en España. https://covid19.isciii.es/ [accessed 03.09.2020]. Available at:
- 13.El periódico Coronavirus en Catalunya: última hora del número de casos. https://www.elperiodico.com/es/sociedad/20200518/coronavirus-catalunya-ultima-hora-casos-7949013 03 September 2020.
- 14.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;40(4):E8–E15. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slankamenac K., Graf R., Barkun J., Puhan M.A., Clavien P.A. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258(1):1–7. doi: 10.1097/SLA.0b013e318296c732. [DOI] [PubMed] [Google Scholar]
- 17.Sakr Y., Jaschinski U., Wittebole X., Szakmany T., Lipman J., Ñamendys-Silva S.A. Sepsis in intensive care unit patients: worldwide data from the intensive care over nations audit. Open Forum Infect Dis. 2018;5:ofy313. doi: 10.1093/ofid/ofy313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blot S., Antonelli M., Arvaniti K., Blot K., Creagh-Brown B., de Lange D. Epidemiology of intra-abdominal infection and sepsis in critically ill patients: “AbSeS”, a multinational observational cohort study and ESICM Trials Group Project. Intens Care Med. 2019;45(12):1703–1717. doi: 10.1007/s00134-019-05819-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaafarani H.M.A., Moheb M.E., Hwabejire J.O., Naar L., Christensen M., Breen K. Gastrointestinal complications in critically ill patients with COVID-19. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004004. [published online ahead of print, 2020 May 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 396, 10243, 27-38 doi: 10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed]
- 21.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, 2020 May 12] Br J Surg. 2020 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bartsch S.M., Ferguson M.C., McKinnell J.A., O’Shea K.J., Wedlock P.T., Siegmund S.S. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood) 2020;39(6) doi: 10.1377/hlthaff.2020.00426. [published online ahead of print, 2020 Apr 23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.País El. La Generalitat cifra en 1.800 millones el coste sanitario del coronavirus. https://elpais.com/espana/catalunya/2020-03-31/la-generalitat-cifra-en-1800-millones-el-coste-sanitario-dela-covid-19.html 31 March 2020.
- 24.Dasta J.F., McLaughlin T.P., Mody S.H., Piech C.T. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266–1271. doi: 10.1097/01.ccm.0000164543.14619.00. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y., Xiao M., Zhang S., Xia P., Cao W., Jiang W. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382(17) doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Connors J.M., Levy J.H. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020;18(7):1559–1561. doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 Apr 10;191 doi: 10.1016/j.thromres.2020.04.013. 145-14, pii: S0049-3848(20)30120-30121. [DOI] [PMC free article] [PubMed] [Google Scholar]