Abstract
Background
The first case of coronavirus 2019 (COVID-19) in Latin America was detected on February 26th, 2020, in Brazil. Later, in June, the World Health Organization announced that the focus of the outbreak had shifted to Latin America, where countries already had poor control of indicators of noncommunicable diseases (NCDs). Concerns about coronavirus infection led to a reduced number of visits and hospitalizations in patients with NCDs, such as cardiovascular disease, diabetes, and cancer. There is a need to determine the impact of the COVID-19 pandemic on patients who have cardiometabolic diseases but do not have clinical evidence of COVID-19 infection.
Methods
The CorCOVID LATAM is a cross-sectional survey of ambulatory cardiometabolic patients with no history or evidence of COVID-19 infection. The study will be conducted by the Interamerican Society of Cardiology. An online survey composed of 38 questions using Google Forms will be distributed to patients of 13 Latin American Spanish-speaking countries from June 15th to July 15th, 2020. Data will be analyzed by country and regions. Seven clusters of questions will be analyzed: demographics, socioeconomic and educational level, cardiometabolic profile, lifestyle and habits, body-weight perception, medical follow-up and treatments, and psychological symptoms.
Results
Final results will be available upon completion of the study.
Conclusions
The present study will provide answers regarding the impact of the COVID-19 pandemic on noninfected cardiometabolic patients. Data on this topic are scarce, as it is an unprecedented threat, without short-term solutions.
Résumé
Contexte
Le premier cas de maladie à coronavirus 2019 (COVID-19) en Amérique latine a été détecté le 26 février 2020 au Brésil. En juin, l’Organisation mondiale de la Santé a annoncé que le foyer de l’épidémie s’était déplacé en Amérique latine, où le suivi des indicateurs relatifs aux maladies non transmissibles est déjà déficient. Les préoccupations relatives à l’infection par le coronavirus ont entraîné une diminution du nombre de consultations et d’hospitalisations des patients atteints d’une maladie non transmissible, comme une ma-ladie cardiovasculaire, le diabète ou un cancer. Il est donc nécessaire d’évaluer l’incidence de la pandémie de COVID-19 chez les patients atteints d’une maladie cardiométabolique ne présentant aucun signe clinique d’une infection au virus de la COVID-19.
Méthodologie
L’étude CorCOVID LATAM est une enquête transversale menée auprès des patients ambulatoires atteints d’une maladie cardiométabolique n’ayant pas d’antécédents d’infection au virus de la COVID-19 et ne présentant aucun signe d’une telle infection. L’étude est réalisée par la Société interaméricaine de cardiologie. Du 15 juin au 15 juillet 2020, on a demandé aux patients de 13 pays hispanophones d’Amérique latine de répondre à un questionnaire en ligne de 38 questions dans Google Forms. Les données seront analysées par pays et par région. Les réponses aux questions seront examinées selon sept grands thèmes : caractéristiques démographiques, caractéristiques socioéconomiques et niveau de scolarité, profil cardiométabolique, mode de vie et habitudes, perception quant au poids corporel, suivi et traitements médicaux et symptômes psychologiques.
Résultats
Les résultats seront publiés à la fin de l’étude.
Conclusions
L’étude fournira des renseignements sur l’incidence de la pandémie de COVID-19 chez les patients atteints d’une maladie cardiométabolique non infectés. Les données sur cette question sont rares, puisqu’il s’agit d’une menace sans précédent, à laquelle il n’existe de surcroît pas de solution à court terme.
The evolution of knowledge about severe acute respiratory syndrome coronavirus-2 and cardiac involvement, such as the entry pathway by angiotensin-converting enzyme 2, prognostic cardiovascular (CV) risk factors, and early diagnosis of myocardial injury in critically ill patients, have built a strong connection between this new disease and cardiometabolic patients.1, 2, 3
Since the first case of coronavirus disease 2019 (COVID-19) was identified in Wuhan, China on December 31st, 2019, almost all the countries of the world have adopted prevention measures such as hand hygiene and social distancing, use of masks, and partial or total quarantines. A never-before-seen disruption of the world economy and healthcare systems occurred as a consequence of these actions.4, 5, 6
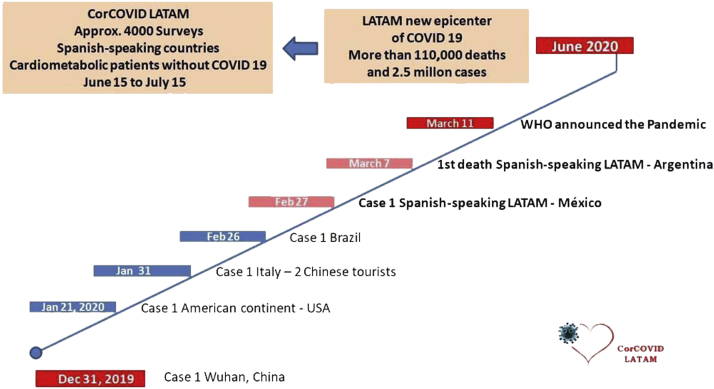
The first case detected in Latin America was on February 26th, 2020, in a 61-year-old individual from Brazil. The first death occurred in Argentina on March 7th, and 4 days later, the World Health Organization declared a pandemic.7,8 Finally, in June 2020, the World Health Organization declared that the focus of the outbreak (epicenter) had shifted to Latin America (Fig. 1).
Figure 1.
Evolution of coronavirus disease 2019 (COVID-19) pandemic in the world, and its further impact in Latin America. WHO, World Health Organization.
CV diseases are now the leading cause of morbidity and mortality worldwide, and current global health policy goals include a 25% reduction in premature mortality from noncommunicable diseases (NCDs) by 2025.9 However, data from the Prospective Urban and Rural Epidemiological study showed that in Latin American countries, secondary prevention drugs may be unavailable and/or unaffordable for a large proportion of communities and households.10
Concerns about coronavirus infection in the community, as occurred in Europe and the United States, led to a reduced number of visits and hospitalizations in patients with chronic NCDs, such as CV diseases, diabetes, and cancer.11,12
A decrease in acute coronary syndromes and vascular hospitalizations was reported, as well as an increased incidence of community cardiac arrests, stress cardiomyopathies (Takotsubo), and mortality due to acute myocardial infarction, compared with non-pandemic periods (the “excess mortality rate”).13, 14, 15
In this context, the question of how the COVID-19 pandemic has affected the life of noninfected cardiometabolic patients arises.16 The current pandemic has raised important concerns in many aspects of the healthcare system, given the presumption that in parallel to the COVID-19 contagion curve there was another upward curve that was not being measured: the one related to CV events in non-COVID patients who were not properly attended to in the population considered at risk.17
The aim of this survey is to collect information about the impact of the COVID-19 pandemic on the life of ambulatory noninfected cardiometabolic patients. No previous data from this field of study are available because this is an unprecedented scenario full of challenges and without immediate short-term solutions. This information could be of help for healthcare decision makers to prepare the appropriate policies to improve the care of these populations in health-threatening situations.
Methods and Design
Study population
The study population will include ambulatory adult patients with cardiometabolic diseases during regular cardiology follow-up in Spanish-speaking Latin American countries.
Inclusion criteria
Patients with prior CV (arterial hypertension, coronary artery disease, cardiomyopathies, valvular disease, or pericardial disease) or metabolic (metabolic syndrome, obesity, dyslipidemia, diabetes) history with no evidence or history of COVID-19; who voluntarily agree to participate in the study.
Exclusion criteria
The patient exclusion criteria are as follows: (i) age <18 years; (ii) history, symptoms, signs, or suspicion of COVID-19 or absence of cardiometabolic disease; (iii) inability to provide consent.
Informed consent
Patients will be informed about the objective of the survey and the anonymity of their responses. No identifiable personal data will be collected. Ethics approval was obtained from the Interamerican Society of Cardiology (IASC) Research Ethics Board.
Study design
A cross-sectional online survey consisting of 38 questions will be developed using Google Forms (Mountain View, CA). Research staff will administer the questionnaire to patients and then enter data online. In accordance with government measures to limit population mobilization in some countries, the survey will be conducted either by face-to-face visits or by phone or video chat, in which case provision of informed consent will be verbal.
The survey will be divided into 2 parts: (i) questions that examine a patients demographic profile; (ii) questions that examine a patient's behavior during the preceding 30 days
Questions include both dichotomous and multiple-option response possibilities. Responses will not be forced, and respondents are permitted to select multiple response choices depending on the question content.
Study distribution
The IASC made a call for cardiologists of Spanish-speaking Latin American countries to join a team of collaborators for the CorCOVID Study on June 1st, 2020. Among the 21 countries in the Americas that have Spanish as their official language, cardiologists from 13 countries registered to participate. Countries will be divided according to a prespecified geographic distribution (Fig. 2) as follows:
-
•
North, Central, and Caribbean region (NCC): Mexico, Guatemala, El Salvador, Costa Rica, Cuba, and the Dominican Republic;
-
•
Andean region (AR): Venezuela, Colombia, Ecuador, and Peru;
-
•
Southern cone region (SCR): Paraguay, Chile, and Argentina.
Figure 2.
Spanish-speaking Latin American countries divided into 3 regions according to a prespecified geographic distribution.
The total population within these 13 countries is approximately 375 million. A minimum of 1000 surveys was established as a goal for each region to have representativeness and allow subsequent comparative analysis.
Survey
The survey platform will be opened from June 15th until July 15th, 2020 for enrolling patients. Reminders will be emailed daily to maximize response rates, along with information about the progression of surveys by country. The survey has 7 clusters of questions, as detailed in the following sections.
Population demographics
It is crucial to determine factors that may affect behavior, such as age and gender. Equally important is to characterize the country in which patients live, as diet, physical activity, and climate can differ substantially. It is well known that environmental factors have an important influence on psychological distresses such as depression and stress.18,19 In terms of environmental and cultural factors, the differences among the 3 regions are substantial. Also, some countries have received migratory flows, especially from Europe, that have created ethnic differences, in contrast to other countries with larger native populations.
Socioeconomic status and education level
The Prospective Urban and Rural Epidemiological study showed that socioeconomic status is associated with differences in risk factors for CV disease incidence and outcomes, including mortality.20 According to this study, people with a lower level of education in low- and middle-income countries, such as the Latin American community, have a higher incidence of and mortality rate from CV diseases.20 Factors such as access to health services, treatments, and vaccination against influenza and pneumonia are essential to understanding the true situation for patients with cardiometabolic diseases during the COVID-19 pandemic.
Cardiometabolic profile
Patients will be characterized by their cardiometabolic history and the time of their last hospitalization due to CV events. It is well known that survivors of myocardial infarction or ischemic stroke, particularly diabetic patients, are at high risk for subsequent CV events, and they need aggressive intervention for secondary prevention and comorbidity management.21
An observational study performed in Mexico showed that more than 70% of the adult population living in areas with high social marginality present with diabetes, hypertension, and obesity.22 An analysis of different CV profiles and how the COVID-19 pandemic affected their care will help in developing support strategies to keep these patients within the healthcare system.
Lifestyle and habits
Primary and secondary prevention guidelines highlight the importance of a healthy lifestyle to avoid CV events.23 However, we have no evidence regarding the impact of quarantines on physical activity level or abrupt changes in diet, particularly among countries that adopted confinement measures of differing intensities, yet data related to toxic habits are of utmost importance. The coronavirus pandemic has raised concerns that people who smoke may be at a greater risk of harm from infection, given the impact of smoking on respiratory and immune function.24 For this reason, healthcare teams have an unexpected and unprecedented opportunity to identify many patients who are in the Prochaska contemplative stage.25 This transtheoretical model of behavior change is a theory of therapy that assesses an individual's readiness to act on new and healthier behavior and provides strategies of change to guide an individual.26 The model is made up of constructions such as stages of change, self-efficacy, and decisional equilibrium.26 The contemplative stage, at which time the individual analyzes the possibility of generating change, is essential for the healthcare team to begin developing a smoking cessation intervention with the expectation of success.26 This group of questions includes one specifically aimed at determining whether a patient has considered quitting tobacco use because of concern about getting COVID-19 infection.
Regarding alcohol intake, the survey will focus on the amount of current consumption and on the relation between consumption during a home-confinement period compared with prior stages.27 There are concerns about increased consumption in some populations due to increased psychological stress triggered by the interaction of financial difficulties, social isolation, and uncertainty about the future.28
Body-weight perception
Misperception of weight has repeatedly been documented among overweight and obese adults, and it has been hypothesized that in overweight and obese individuals, this attitude may preclude the adoption of healthful attitudes and behaviors, perhaps as a result of lower weight-loss motivation.29
As in the case of toxic habits, a major question is how psychological stress and depression will influence appetite and diet disorders.30 The imbalance between food intake and physical activity, added to the poor perception of body weight, can lead to a change in the metabolic profile of overweight and obese patients in a relatively short period of time.
Medical controls and treatments
Suboptimal adherence to medications taken chronically for secondary prevention of CV and metabolic diseases continues to burden the healthcare system, despite the well-established prevention benefits of adherence.31 The number of pills per day, the access to healthcare systems, and the availability of drugs and medical prescriptions are some potential barriers to appropriate adherence.32 Given this scenario, it is extremely valuable to evaluate the percentage of the population receiving treatment according to medical indications. We are also interested in evaluating adherence to recommended immunization against influenza and pneumonia, as vaccines are particularly indicated in this group of patients.33
Psychological symptoms
The COVID-19 pandemic has brought not only the risk of death from infection but also unbearable psychological pressure.34,35 In the absence of antecedents of a global crisis of this magnitude in the current times, it is unknown what the real impact is in terms of stress and depression in our patients. Early detection of symptoms, and proper action to provide tools for a better life during the pandemic, may decrease post-pandemic long-term effects.36
Statistical analysis
Data will be collected in Google Forms. All statistical analyses will be performed using Stata v. 13.1 (Stata Corp, College Station, TX). Data will be described using means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. Independent sample t tests will be used to compare the normally distributed continuous variables; the Mann-Whitney U statistic will be used for non-normally distributed continuous variables; and the Pearson χ2 test (or the Fisher’s Exact test as appropriate) will be used for categorical variables. A P value of <0.05 will be considered statistically significant. Multiple logistic regression models will be constructed for comparisons, and odds ratios and 95% confidence intervals will be provided.
Conclusions
An unprecedented worldwide challenge that started about 6 months ago has transformed the world as we knew it. Healthcare systems have been particularly hard hit with this new condition that affects our patients both physically and mentally. The impact on patients with NCDs is extremely important, and learning from their experiences during the pandemic may help us deliver better care in the post-pandemic era. In particular, Latin American countries, as well as all low- and middle-income countries, have the major additional challenge of controlling NCD indicators.
The hope is that the CorCOVID LATAM Study will provide answers about the impact of the COVID-19 pandemic on cardiometabolic patients who do not have signs of infection.
Acknowledgements
Authors takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: Ethics approval was obtained from the Interamerican Society of Cardiology (IASC) Research Ethics Board.
See page 676 for disclosure information.
References
- 1.Zhang H., Menninger J.M., Li Y., Hong N., Slushy A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexander B., Baranchuk A. COVID-19 and myocardial injury CMAJ. 2020;192:E812–E813. doi: 10.1503/cmaj.201230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacIntyre C.R., Wang Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet. 2020;395:1950–1951. doi: 10.1016/S0140-6736(20)31183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauch C.T., Anand M. COVID-19: when should quarantine be enforced? Lancet Infect Dis. 2020;20:994–995. doi: 10.1016/S1473-3099(20)30428-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P. COVID-19 in Latin America: the implications of the first confirmed case in Brazil. Travel Med Infect Dis. 2020;35:101613. doi: 10.1016/j.tmaid.2020.101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Novel coronavirus (2019-nCoV) https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn Available at: Accessed October 12, 2020.
- 9.Joseph P., Leong D., McKee M. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. 2017;121:677–694. doi: 10.1161/CIRCRESAHA.117.308903. [DOI] [PubMed] [Google Scholar]
- 10.Khatib R., McKee M., Shannon H. Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet. 2016;387:61–69. doi: 10.1016/S0140-6736(15)00469-9. [DOI] [PubMed] [Google Scholar]
- 11.Lange S.J., Ritchey M.D., Goodman A.B. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions. MMWR. 2020;69:25. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Society of Cardiology ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance Available at: Accessed October 12, 2020.
- 13.Jabri A., Kalra A., Kumar A. Incidence of stress cardiomyopathy during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14780. e2014780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metzler B., Siostrzonek P., Binder R. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. EHJ. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. JACC. 2020;25:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brook R.D., Levy P., Rajagopalan S. Cardiometabolic risk factor control during times of crises and beyond. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006815. e006815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chalasani M., Nasir K., Gupta M.D., Kalra A. The covid-19 pandemic and India's cardiovascular disease burden: finding the right balance [e-pub ahead of print]. Indian J Med Ethics. https://doi.org/10.20529/IJME.2020.059 Accessed October 12, 2020. [DOI] [PubMed]
- 18.Kolossa-Gehring M., Becker K., Conrad A. Environmental surveys, specimen bank and health related environmental monitoring in Germany. Int J Hyg Environ Health. 2012;215:120–126. doi: 10.1016/j.ijheh.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 19.Mirzakhani L., Poursafa P. The association between depression and climatic conditions in the Iran way to preventive of depression [sic] Int J Prev Med. 2014;5:947–951. [PMC free article] [PubMed] [Google Scholar]
- 20.Rosengren A., Smyth A., Rangarajan S. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–e760. doi: 10.1016/S2214-109X(19)30045-2. [DOI] [PubMed] [Google Scholar]
- 21.Li S., Peng Y., Wang X. Cardiovascular events and death after myocardial infarction or ischemic stroke in an older Medicare population. Clin Cardiol. 2019;42:391–399. doi: 10.1002/clc.23160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alcalde-Rabanal J.E., Orozco-Nuñez E., Espinosa-Henao O.E., Arredondo-Lopez A., Alcayde-Barranco L. The complex scenario of obesity, diabetes and hypertension in the area of influence of primary healthcare facilities in Mexico. PLoS One. 2018:13. doi: 10.1371/journal.pone.0187028. e0187028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mok Y., Sang Y., Ballew S.H. American Heart Association’s life’s simple 7 at middle age and prognosis after myocardial infarction in later life. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.007658. e007658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Majmundar A., Allem J.P., Cruz T.B., Unger J.B. Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob Res. 2020 doi: 10.1093/ntr/ntaa064. ntaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klemperer E.M., West J.C., Peasley-Miklus C., Villanti A.C. Change in tobacco and electronic cigarette use and motivation to quit in response to COVID-19. Nicotine Tob Res. 2020;22:1662–1663. doi: 10.1093/ntr/ntaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prochaska J.O., Velicer W.F. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 27.Rehm J., Kilian C., Ferreira-Borges C. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020;39:301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Goeij M.C., Suhrcke M., Toffolutti V. How economic crises affect alcohol consumption and alcohol-related health problems: a realist systematic review. Soc Sci Med. 2015;131:131–146. doi: 10.1016/j.socscimed.2015.02.025. [DOI] [PubMed] [Google Scholar]
- 29.Duncan D.T., Wolin K.Y., Scharoun-Lee M. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011;22:8–20. doi: 10.1186/1479-5868-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finch L.E., Tomiyama A.J. Comfort eating, psychological stress, and depressive symptoms in young adult women. Appetite. 2015;95:239–244. doi: 10.1016/j.appet.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 31.Osterberg L., Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 32.Tamargo J., Castellano J.M., Fuster V. The Fuster-CNIC-Ferrer cardiovascular polypill: a polypill for secondary cardiovascular prevention. Int J Cardiol. 2015;201:S15–S22. doi: 10.1016/S0167-5273(15)31028-7. [DOI] [PubMed] [Google Scholar]
- 33.Modin D., Claggett B., Køber L. Influenza vaccination is associated with reduced cardiovascular mortality in adults with diabetes: a nationwide cohort study [e-pub ahead of print]. Diabetes Care. https://doi.org/10.2337/dc20-0229 Accessed October 12, 2020. [DOI] [PubMed]
- 34.Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chew N.W., Lee G.K., Tan B.Y. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siu A.L., US Preventive Services Task Force. Bibbins-Domingo K., Grossman D.C. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:380–387. doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]