Abstract
Objectives
Older adults may experience loneliness due to social distancing and isolation during the Coronavirus disease 2019 (COVID-19) pandemic. Loneliness may further catalyze numerous poor health outcomes including impaired sleep. This study aimed to assess COVID-19 related worries and resilience as potential moderators of the loneliness-sleep problems link.
Method
In the midst of the lock-down period of COVID-19, we collected data using a web-based public platform from 243 Israeli older adults (mean age = 69.76, SD = 6.69, age range = 60–92). Participants completed measures of COVID-19 related loneliness, sleep problems, COVID-related worries, and resilience.
Results
COVID-19 related loneliness was related to more sleep problems. The loneliness-sleep association was especially strong among those with more COVID-19 related worries or among those with lower resilience.
Conclusion
The relationship between COVID-19 related loneliness and sleep problems is not uniform across older adults. The subjective sleep quality of those with more COVID-19 related worries or less resilience (i.e., feeling less being able to adapt to the challenging circumstances) is more susceptible to feeling lonely. Considering these variables may facilitate detection of and intervention for older adults vulnerable to aversive results in the context of COVID-19.
Keywords: Loneliness, Sleep problems, Worries, Resilience, COVID-19
Highlights
-
•
COVID-19 loneliness positively associated with sleep problems among older adults.
-
•
Sleep problems associated with loneliness depended on worries and resilience.
-
•
The association was stronger for those with more COVID-19 related worries.
-
•
The association was stronger for older adults with low resilience.
1. Introduction
The Coronavirus disease 2019 (COVID-19) is highly linked with conditions that may impair sleep (Altena et al., 2020). This is especially true in older adults for two reasons. First, older adults may have poorer sleep. For example, a large meta-analysis showed that parameters indicative of good sleep such as sleep efficiency, slow wave sleep, and REM sleep diminish with age (Ohayon, Carskadon, Guilleminault, & Vitiello, 2004). Second, loneliness, which is relevant in the context of COVID-19 as described below, can impair sleep in older adults (Shankar, 2020).
Social distancing/confinement globally adopted as a countermeasure to the COVID-19 pandemic may be highly advantageous in reducing the spreading of the coronavirus. However, social isolation, i.e., an objective lack of interactions with others (Leigh-Hunt et al., 2017), can contribute to negative outcomes, such as loneliness. Loneliness refers to subjective distress resulting from a discrepancy between desired and perceived social relationships (e.g., Perlman & Peplau, 1981). Feeling of loneliness can be typically experienced when isolation is out of one's control (Cacioppo & Cacioppo, 2014). Loneliness has been found to link and even predict numerous adverse outcomes (Segel-Karpas, Ayalon, & Lachman, 2018) including reduced sleep quality (Cacioppo et al., 2002; Matthews et al., 2017; Shankar, 2020).
Lonely individuals experience more sleep fragmentation than people who report more connection to others (Kurina et al., 2011). These latter authors suggest that perceptions of a non-secure social surrounding, promotes an alert state, which hinders the possibility for a restful night's sleep. Recently, it was found that both objective and subjective social isolation are associated with sleep problems among older adults (Cho et al., 2019). Those authors concluded that older adults experience sleep problems because they feel socially isolated, not just because they are deprived of social networks.
Hitherto, we examined the loneliness – sleep link in older adults. Two potential moderators of this association are outlined below, namely worries and resilience. The COVID-19 threat may also be accompanied by worries, such as fear of contracting the coronavirus, which may further impair sleep. Indeed, worries at bedtime are related to decreased sleep efficiency and other changes in sleep architecture (Åkerstedt, Kecklund, & Axelsson, 2007). A meta-analysis of adolescents' sleep studies (Bartel, Gradisar, & Williamson, 2015) concluded that pre sleep worry is one of the factors that have a negative impact on sleep. Accordingly, sleep problems should be worse when both loneliness and COVID-19 worries are high.
In contrast to worries, resilience correlates positively with sleep quality. Among participants positive for HIV, those high on resilience had lower odds of reporting poor sleep quality or of using sleep medications during the previous month (Downing et al., 2016). Likewise, in healthy pregnant women resilience was related to sleep quality and mediated the relationship between pregnancy stress and sleep quality (Li et al., 2016). From these two studies it emerges that even in stressful situations resilience may be an important factor for sleep quality. Thus, we postulate that loneliness would be associated with sleep problems to a lower degree when resilience is high.
Because both loneliness and sleep problems are very relevant to the older adult population, we also thought to assess if older adults worry levels or resilience levels may moderate the loneliness-sleep link. In summary, the aim of the current study was to examine how worries or resilience may moderate the link of COVID-19 imposed loneliness with sleep problems. We hypothesized that COVID-19 related loneliness would be related to more sleep problems, especially among older adults who report more COVID-19 related worries. We further hypothesized that the loneliness-sleep problems link would be mitigated among older adults high in resilience.
2. Methods
2.1. Participants and procedure
Using the Qualtrics web-based public platform, we collected data across Israel in the midst of the lock-down period of COVID-19 (between March 16 to April 14, 2020). On the last day of data collection, 12,361 Israelis were tested positive for the coronavirus and 123 had died. The sample included 243 people between the ages of 60 and 92 (mean age = 69.76, SD = 6.69). Most of them were women (n = 168, 69.1%), married or cohabitating (n = 177, 72.8%), and most had academic degree (n = 179, 73.7%). Of the participants 101 (41.6%) reported to have been diagnosed with chronic medical condition known to be related to increased risk of death due to COVID-19 complications. The majority rated their health (n = 155, 63.8%) and economic status (n = 156, 64.2%) as good or very good.
The online questionnaire was disseminated across multiple social media resources and contact lists provided by organizations (e.g., continuing-care retirement communities, institutions hosting educational activities for older adults). All participants provided an informed consent. Ethical approval was received from the Institutional Review Board at the third author's University.
2.2. Measures
Participants completed background characteristics, including age, gender, marital status, and education (rated from 1 = without formal education to 6 = formal tertiary education). They noted whether they have been diagnosed with chronic medical conditions known to be related to increased risk of death due to COVID-19 complications (i.e., cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer), and rated their health and economic status on scales ranging from 1 (not good at all) to 5 (very good). Participants further reported their level of exposure to six COVID-19 pandemic related events (i.e., being tested positive for the coronavirus, being [or having been] in self-isolation, knowing family members, friends, or other people who were tested positive, knowing people in self-isolation; exposure score was the sum of events). Participants further reported whether they have changed 11 behaviors due to the COVID-19 pandemic (i.e., avoid shaking hands, avoiding hugs, keeping physical distance from others, avoiding social events, going out less frequently, avoid inviting or meeting with people, using a mask or gloves, avoid going to public places, washing hands more often, buying more food and water than usual, canceling/changing significant plans; behavioral change score was the sum of behaviors changed).
Participants completed the additional below measures while being asked to relate to their feelings and symptoms during the COVID-19 pandemic and due to it.
Loneliness was assessed with the 3-item version of the UCLA Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004). Items were rated on a 5-point scale ranging from 1 (not at all) to 5 (almost always). The loneliness score was the mean of ratings, and higher scores reflected higher loneliness. The Hebrew version of the scale was used in previous studies (Spitzer, Segel-Karpas, & Palgi, 2019). Internal reliability was good (α = 0.80).
COVID-19 related worries were assessed by four items developed for the current study regarding worrying about self/close people/relatives developing COVID-19, or infecting others in case of having COVID-19. Items were rated on a 5-point scale ranging from 1 (not at all) to 5 (almost always). The worries score was the mean of ratings, and higher scores reflected increased worries. Internal reliability was good (α = 0.78).
Resilience was assessed by the 10-item Connor–Davidson Resilience Scale (CD-RISC; Campbell-Sills & Stein, 2007), where items were rated on a 5-item scale ranged from 1 (strongly disagree) to 5 (strongly agree). The resilience score was the average of items, and high scores indicate higher resilience. The Hebrew version of the scale was used in previous studies (Hoffman, Cohen-Fridel, Bodner, Grossman, & Shrira, 2016). Internal reliability was good (α = 0.89).
Sleep problems were assessed with three items. Two items were adapted from the insomnia severity index (Bastien, Vallières, & Morin, 2001): “How satisfied are you with your current sleep?” and “How much have you been suffering from difficulties in falling asleep since entering isolation/social distancing?” A third item was adapted from the PHQ-9 depression questionnaire (Kroenke, Spitzer, & Williams, 2001): “To what extent did you experience, since the outbreak of the coronavirus crisis, a feeling of tiredness or low energy?” Items were rated on a 4-item scale ranged from 1 (no sleep problems) to 4 (significant sleep problems). The sleep problem score was the average of the three items, with high scores indicating more problems. The Hebrew version of the scales was used in previous studies (Grossman et al., 2016; Magnezi & Glasser, 2014). Internal reliability was acceptable (α = 0.75).
3. Data analysis
First, we calculated means and standard deviations, frequencies and percentages as basic descriptive statistics. Pearson and Spearman coefficients were used to describe the relationship between these variables. Second, two complementary hierarchical regressions were conducted for testing the study hypotheses. In each of the two analyses sleep problems were regressed on demographic variables (age, gender, education, marital status), subjective economic status, self-rated health status, COVID-19 related exposure, behavioral change, and medical conditions related to increased risk of death due to COVID-19 complications for Step 1. Step 2 included loneliness and worries or loneliness and resilience according to the tested hypothesis. The third step included the interaction between loneliness and worries or loneliness and resilience respectively. Interaction variables were calculated by multiplying loneliness × COVID-19 related worries and loneliness × resilience after mean centering the variables. PROCESS computation plugin (Hayes, 2013) Model 1 was applied to estimate simple slope tests for significant interactions.
4. Results
Few participants reported being tested positive for the coronavirus or being in self-isolation (n = 44, 18.1%), yet most knew someone who tested positive or was in self-isolation (n = 154, 63.4%). All respondents reported changing at least one behavior due to the pandemic (ranging from buying more food and water than usual: n = 81, 33.3%, to going out less frequently: n = 224, 92.2%).
Average scores for the study variables as well as correlations can be found in Table 1 . Reports of sleep problems correlated positively with loneliness and with COVID-19 related worries, and negatively with resilience.
Table 1.
Descriptive statistics of study variables.
| M (SD)/n (%) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sleep problems | 1.64 (0.69) | – | |||||||||||
| 2 | Loneliness (UCLA) | 2.39 (0.90) | 0.36⁎⁎⁎ | – | ||||||||||
| 3 | COVID-19 related worries | 2.99 (0.91) | 0.21⁎⁎⁎ | 0.11 | – | |||||||||
| 4 | Resilience (CD-RISC) | 3.83 (0.69) | −0.20⁎⁎⁎ | −0.17⁎⁎ | −0.12 | – | ||||||||
| 5 | Age | 69.76 (6.69) | −0.12 | −0.01 | −0.12 | −0.02 | – | |||||||
| 6 | Gendera | 168 (69.1) | 0.21⁎⁎⁎ | 0.05 | −0.05 | −0.13⁎ | −0.13⁎ | – | ||||||
| 7 | Marital statusb | 177 (72.8) | −0.06 | −0.09 | 0.06 | 0.00 | −0.08 | −0.25⁎⁎ | – | |||||
| 8 | Educationc | 179 (73.7) | −0.03 | −0.09 | −0.08 | −0.05 | −0.11 | 0.06 | 0.12⁎ | – | ||||
| 9 | Subjective economic statusd | 156 (64.2) | −0.14⁎ | −0.09 | −0.13⁎ | 0.03 | −0.10 | 0.05 | 0.18⁎ | 0.27⁎⁎ | – | |||
| 10 | Self-rated healthd | 155 (63.8) | −0.16⁎ | 0.01 | −0.20⁎⁎ | 0.08 | −0.19⁎⁎ | 0.22⁎⁎⁎ | −0.00 | 0.18⁎⁎⁎ | 0.44⁎⁎⁎ | – | ||
| 11 | Medical conditionse | 101 (41.6) | 0.01 | 0.10 | −0.01 | −0.05 | −0.23⁎⁎ | 0.24⁎⁎ | −0.03 | −0.08 | −0.20⁎⁎ | −0.53⁎⁎⁎ | – | |
| 12 | Behaviorsf | 8.38 (2.16) | 0.07 | 0.11 | 0.19⁎⁎ | 0.19 | −0.03 | −0.01 | 0.04 | 0.06 | 0.03 | −0.09 | 0.02 | – |
| 13 | Exposure to COVID-19g | 28 (11.6) | 0.01 | 0.09 | 0.00 | 0.06 | −0.03 | 0.03 | 0.03 | 0.06 | 0.08 | 0.12 | −0.04 | 0.05 |
N = 243. Correlation values for variables 1–5 & 12–13 are Pearson coefficients; values involving items 6–11 are Spearman coefficients.
p < .05.
p < .01.
p < .001.
Women.
Married or cohabitating.
Tertiary education.
Good or very good.
Diagnosed with chronic medical condition known to be related to increased risk of death due to COVID-19 complications.
No. of self-behaviors changed since outbreak of COVID-19.
Exposed to at least three items on the exposure scale.
Table 2 presents the results of the main regression analyses predicting sleep problems. Across regressions, being female and having lower health levels linked with higher sleep problem levels. After controlling for the effect of Step 1 variables, loneliness, but not resilience or COVID-19 related worries, was related to higher sleep problem levels. In each model, as predicted, both interactions, i.e., the Loneliness × COVID-19 related worries interaction, and the Loneliness × Resilience interaction, were significant.
Table 2.
Regression analyses of loneliness, COVID-19 related worries/resilience on sleep problems.
| Loneliness × COVID-19 worries | ΔR2 | B | β | Loneliness × Resilience | ΔR2 | B | β | ||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | 0.09⁎⁎ | Step 1 | 0.09⁎⁎ | ||||||
| Age | −0.01 | −0.12 | Age | −0.01 | −0.12 | ||||
| Gender (woman) | 0.23 | 0.16⁎ | Gender | 0.23 | 0.15⁎ | ||||
| Marital status (with partner) | 0.00 | 0.00 | Marital status (with partner) | 0.00 | 0.00 | ||||
| Education | −0.02 | −0.01 | Education | −0.22 | −0.01 | ||||
| Subjective economic status | −0.09 | −0.12 | Subjective economic status | −0.09 | −0.12 | ||||
| Self-rated health | −0.15 | −0.20⁎ | Self-rated health | −0.15 | −0.20⁎ | ||||
| Medical conditions | −0.04 | −0.03 | Medical conditions | −0.04 | −0.03 | ||||
| Behaviors | 0.02 | 0.05 | Behaviors | 0.02 | 0.05 | ||||
| Exposure to COVID-19 events | −0.00 | −0.00 | Exposure to COVID-19 events | −0.00 | −0.00 | ||||
| Step 2 | 0.13⁎⁎⁎ | Step 2 | 0.13⁎⁎⁎ | ||||||
| Loneliness | 0.26 | 0.35⁎⁎⁎ | Loneliness | 0.25 | 0.33⁎⁎⁎ | ||||
| COVID-19 related worries | 0.08 | 0.11 | Resilience | −0.11 | −0.10 | ||||
| Step 3 | 0.02⁎ | Step 3 | 0.02⁎ | ||||||
| Loneliness × Worries | 0.11 | 0.15⁎ | Loneliness × Resilience | −0.14 | −0.13⁎ |
p < .05.
p < .01.
p < .001.
The interactions were probed using the PROCESS plugin (Model 1, Hayes, 2013) to estimate the effect of loneliness on sleep at different levels (±1SD from the mean) of worries (Analysis 1) and different levels (±1SD from the mean) of resilience (Analysis 2). When levels of COVID-19 worries were at +1 SD above the mean (i.e., high worries level), the relationship between loneliness and sleep problems was strong (B = 0.35, t (219) = 6.00, p < .001). However, for those with low levels of COVID-19 worries (−1 SD below the average) the loneliness-sleep problems association was weaker (B = 0.15, t (219) = 2.39, p = .018). In essence the slope depicting the loneliness-sleep association was significantly steeper when worries were higher. When looking at the moderating effect of resilience, at resilience levels of −1 SD below the mean, loneliness and sleep problems were strongly associated (B = 0.34, t (218) = 5.34, p < .001). However, for those with high levels of resilience (+1 SD), the association between loneliness and sleep problems was weaker (B = 0.15, t (218) = 2.31, p < .02). The slope reflecting the loneliness-sleep link was steeper when resilience was low.
Fig. 1, Fig. 2 present the two-way interaction effects. As can be seen in Fig. 1, Fig. 2, loneliness was related to higher sleep problem levels. However, the loneliness-sleep problems association appears to be strongest among older people with more COVID-19 related worries and among older people with low resilience.
Fig. 1.
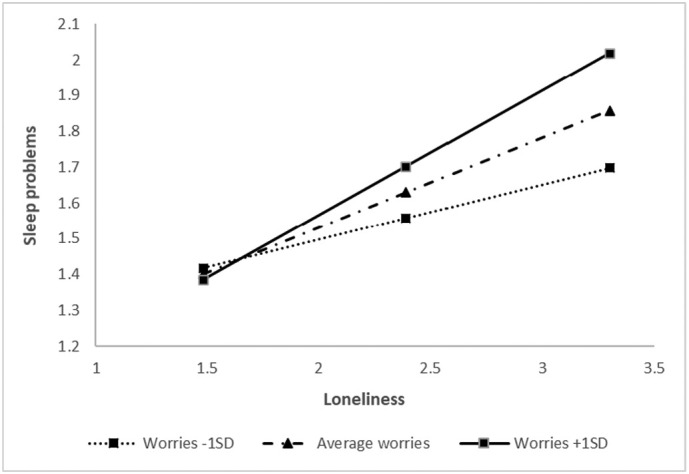
The interaction between COVID-19 related loneliness and COVID-19 related worries on sleep problems.
Fig. 2.
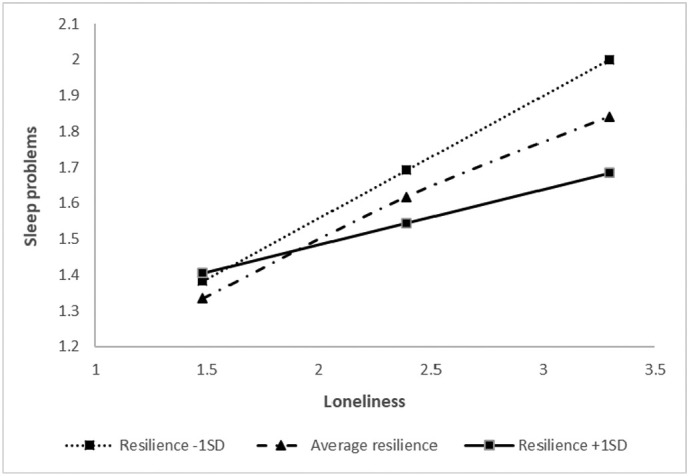
The interaction between COVID-19 related loneliness and resilience on sleep problems.
5. Discussion
This study found that higher level of COVID-19 related loneliness is associate with higher levels of sleep problems among older adults. Previous studies found similar results of relationship between social isolation and dissatisfaction with sleep both in general population surveys (Ohayon, Caulet, & Guilleminault, 1997) and in response to isolation following a large-scale disaster (Matsumoto et al., 2014). The association between loneliness and sleep problems was also found among older adults (Shankar, 2020).
Interactions further corroborated our hypotheses, indicating that among older adults, the rate of sleep problems associated with loneliness depended on COVID-19 related worries, and inversely on resilience. The loneliness-sleep problems association was much stronger for those with more COVID-19 related worries compared to those with less worries. Similarly, the loneliness-sleep problems association was much stronger for those with low resilience compared to those with high levels of resilience. Thus, both interactions indicate that the sensitivity of older people to the effects of loneliness on sleep depends on these psychological factors of worries and resilience.
When older adults feel worried, particularly about COVID-19, the effects of loneliness on their sleep can be detrimental. Inversely, a sense of being able to successfully adapt to challenging experiences (resilience), emerges as a potential buffering factor against encountering sleep problems (Downing et al., 2016). This finding is in line with a previous study (Liu et al., 2016), which found in a survey of community-dwelling adults, that both perceived stress and resilience predict sleep disturbance in an interactive manner. Thus, although our study related to loneliness while Liu et al. (2016) measured perceived stress, the current interaction resembles their results, whereby, sleep disturbances are more frequent when high perceived stress is coupled with low resilience in comparison to high resilience.
Our findings should be assessed in light of the study's limitations. First, the online sampling may have biased the sample towards populations with an access to or literacy in digital resources, and those who may be more socially connected, at least virtually, and thus may experience less loneliness and sleep problems. Second, the cross-sectional design does not allow to infer directionality. This issue of directionality may be particularly important when examining sleep problems in the context of resilience, because earlier studies suggested that the quality of REM sleep contributes to a resilient reaction in the face of traumatic exposure (Cowdin, Kobayashi, & Mellman, 2014). Future studies may be able to clarify this issue. Third, sleep problems were assessed by self-report and with three items. As we needed to obtain high response rates in a very narrow time window of full social closure, we opted for a very short sleep measure (3 items). In the future, it may be possible to collect more detailed measures in order to receive more accurate data. Additionally, the absence of reports of sleep problems from the period before the outbreak of the COVID-19 crisis precludes a comparison of the obtained data with pre-pandemic measures. Based on the current results and in line with earlier studies, sleep problems due to the COVID-19 crisis may further impair health (Christiansen, Larsen, & Lasgaard, 2016), especially when they become chronic (Grossman, Shrira, & Bodner, 2017). Finally, by using a general measure of worries we could have a view of the impact of worries on the loneliness and sleep relation. However, as the COVID-19 pandemic is a unique experience we assessed worries by items highly relevant to this situation.
Bearing the study limitations in mind, the current results of escalating vulnerability to sleep problems when feeling loneliness in conjunction with high level of worries/low level of resilience, suggest it wise to track and monitor the vulnerability of older adults to this aversive context of COVID-19. Our findings allude to the possibility that improvement in sleep quality may be obtained by promoting mental healthcare in order to enhance resilience, to counter COVID-19 related worries, or by engaging in programs to decrease loneliness. In addition, as the current COVID-19 crisis can be seen as an example of a lasting stressful situation, these results may attest to the importance of psychological responses or coping strategies in the face of stress. This is especially true as our results were obtained from high functioning individuals.
CRediT authorship contribution statement
Prof. Y. Palgi led the conceptualization and formation of the questionnaire and data acquisition. He reviewed and approved the last draft as well. Dr. E. Grossman, Dr. Y. Hoffman, and Prof. A. Shrira were responsible of data analysis, drafting, writing, and editing the manuscript.
Funding details
This work was not supported by any grant.
Consent
All participants indicated their consent to participate in the study prior to answering the questionnaire. All participants were fully anonymized.
Declaration of competing interest
The authors report no conflict of interest.
Acknowledgments
The authors wish to express many thanks to Mrs. Lia Ring for her work and great contribution in collecting the data for this survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.paid.2020.110371.
Appendix A. Supplementary data
Supplementary material
References
- Åkerstedt T., Kecklund G., Axelsson J. Impaired sleep after bedtime stress and worries. Biological Psychology. 2007;76:170–173. doi: 10.1016/j.biopsycho.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. Journal of Sleep Research. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Bartel K.A., Gradisar M., Williamson P. Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Medicine Reviews. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Cacioppo S. Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass. 2014;8:58–72. doi: 10.1111/spc3.12087. https://doi-org.mgs.ariel.ac.il/10.1111/spc3.12087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C., Berntson G.G., Ernst J.M., Gibbs A.C., Stickgold R., Hobson J.A. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13:384–387. doi: 10.1111/j.0956-7976.2002.00469.x. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress. 2007;20:1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Cho J.H.J., Olmstead R., Choi H., Carrillo C., Seeman T.E., Irwin M.R. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging & Mental Health. 2019;23:1130–1138. doi: 10.1080/13607863.2018.1481928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen J., Larsen F.B., Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Social Science & Medicine. 2016;152:80–86. doi: 10.1016/j.socscimed.2016.01.020. [DOI] [PubMed] [Google Scholar]
- Cowdin N., Kobayashi I., Mellman T.A. Theta frequency activity during rapid eye movement (REM) sleep is greater in people with resilience versus PTSD. Experimental Brain Research. 2014;232:1479–1485. doi: 10.1007/s00221-014-3857-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing M.J., Jr., Houang S.T., Scheinmann R., Yoon I.S., Chiasson M.A., Hirshfield S. Engagement in care, psychological distress, and resilience are associated with sleep quality among HIV-positive gay, bisexual, and other men who have sex with men. Sleep Health. 2016;2:322–329. doi: 10.1016/j.sleh.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman E.S., Hoffman Y., Bodner E., Palgi Y., Gottlieb M., Mesika O., Shrira A. Psychological effects following the Iran nuclear deal: Iranian nuclear threat salience moderates the relationship between PTSD symptoms and sleep problems. Psychiatry Research. 2016;243:292–294. doi: 10.1016/j.psychres.2016.06.032. [DOI] [PubMed] [Google Scholar]
- Grossman E.S., Shrira A., Bodner E. Enduring sleep complaints predict health problems: A six-year follow-up of the survey of health and retirement in Europe. Aging & Mental Health. 2017;21:1155–1163. doi: 10.1080/13607863.2016.1209735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Publications; New York: 2013. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hoffman Y., Cohen-Fridel S., Bodner E., Grossman E., Shrira A. Confidence in the ‘Iron Dome’ missile defense system combined with sense of resilience relate to lower posttraumatic stress disorder symptoms following missile attacks. Journal of Clinical Psychiatry. 2016;77:407–408. doi: 10.4088/JCP.15l10024. [DOI] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurina L.M., Knutson K.L., Hawkley L.C., Cacioppo J.T., Lauderdale D.S., Ober C. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011;34:1519–1526. doi: 10.5665/sleep.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Li G., Kong L., Zhou H., Kang X., Fang Y., Li P. Relationship between prenatal maternal stress and sleep quality in Chinese pregnant women: The mediation effect of resilience. Sleep Medicine. 2016;25:8–12. doi: 10.1016/j.sleep.2016.02.015. [DOI] [PubMed] [Google Scholar]
- Liu X., Liu C., Tian X., Zou G., Li G., Kong L., Li P. Associations of perceived stress, resilience and social support with sleep disturbance among community-dwelling adults. Stress and Health. 2016;32:578–586. doi: 10.1002/smi.2664. [DOI] [PubMed] [Google Scholar]
- Magnezi R., Glasser S. Psychometric properties of the Hebrew translation of the patient activation measure (PAM-13) PLoS One. 2014;9 doi: 10.1371/journal.pone.0113391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto S., Yamaoka K., Inoue M., Muto S., Teikyo Ishinomaki Research Group and Health and Life Revival Council in the Ishinomaki district (RCI) Social ties may play a critical role in mitigating sleep difficulties in disaster-affected communities: A cross-sectional study in the Ishinomaki Area, Japan. Sleep. 2014;37:137–145. doi: 10.5665/sleep.3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews T., Danese A., Gregory A.M., Caspi A., Moffitt T.E., Arseneault L. Sleeping with one eye open: Loneliness and sleep quality in young adults. Psychological Medicine. 2017;47:2177–2186. doi: 10.1017/S0033291717000629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon M.M., Carskadon M.A., Guilleminault C., Vitiello M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- Ohayon M.M., Caulet M., Guilleminault C. How a general population perceives its sleep and how this relates to the complaint of insomnia. Sleep. 1997;20:715–723. doi: 10.1093/sleep/20.9.715. [DOI] [PubMed] [Google Scholar]
- Perlman D., Peplau L.A. Toward a social psychology of loneliness. In: Gilmour R., Duck S., editors. Personal relationships: 3. Relationships in disorder. Academic Press; London: 1981. pp. 31–56. [Google Scholar]
- Segel-Karpas D., Ayalon L., Lachman M.E. Loneliness and depressive symptoms: The moderating role of the transition into retirement. Aging & Mental Health. 2018;22:135–140. doi: 10.1080/13607863.2016.1226770. [DOI] [PubMed] [Google Scholar]
- Shankar A. Loneliness and sleep in older adults. Social Psychiatry and Psychiatric Epidemiology. 2020;55:269–272. doi: 10.1007/s00127-019-01805-8. [DOI] [PubMed] [Google Scholar]
- Spitzer N., Segel-Karpas D., Palgi Y. Close social relationships and loneliness: The role of subjective age. International Psychogeriatrics. Advanced online publication. 2019 doi: 10.1017/S1041610219001790. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material


