Abstract
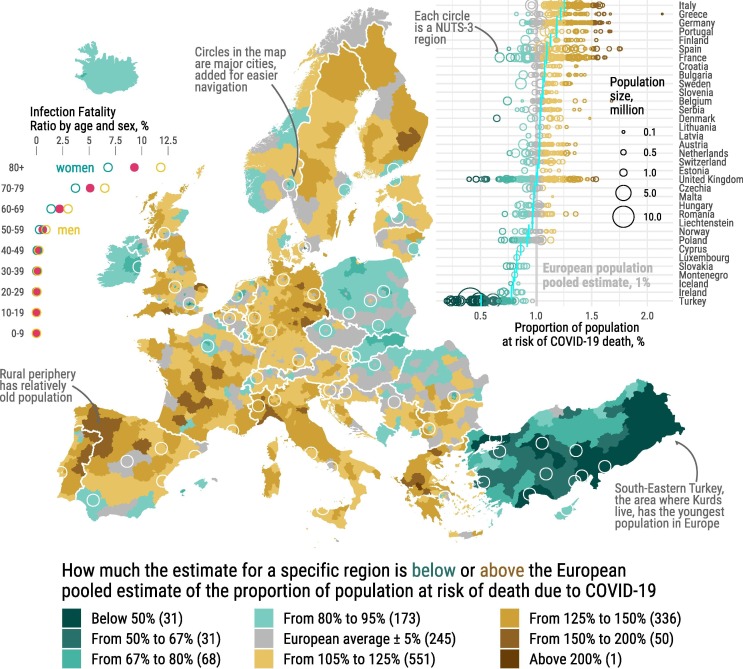
The map presented in this brief note summarizes regional differences in population age structures between the NUTS-3 regions of Europe in the context of unequal age- and sex-specific death risks associated with the spread of the COVID-19 pandemic. Since older people are exposed to much higher death risks, older populations are expected to face much more difficult challenges coping with the pandemic. The urban/rural dimension turns out to be very important as the remote rural areas are also the oldest. In the map NUTS-3 regions of Europe are colored according to the deviation from European pooled estimate of the proportion of population at risk of death due to COVID-19. We assume that 5/6 of the populations get infected and experience age-specific infection-fatality ratios (IFRs) modelled by the Imperial College COVID-19 Response Team. We adjust IFRs by sex ratios of age-specific case-fatality ratios observed in the European countries that are included in the COVerAGE-DB. Thus, we effectively introduce a summary measure of population age structures focused on the most vulnerable to the pandemic. Such an estimate for the total European population is 1%. The map reflects the unequal population age structures rather than the precise figures on COVID-19 fatality. It is a case-if scenario that highlights the possible effect of the population age structures, a demographic perspective. This analysis clearly shows the contribution of regional differences in population age structures to the magnitude of the pandemic – other things equal, we expect to see a four-fold variation in average regional infection-fatality ratios across Europe due only to differences in the population structures.
The COVID-19 pandemic is unequally claiming lives across age groups. Since death risks increase sharply with age for people infected by SARS-CoV-2 (Ferguson et al., 2020), the new coronavirus poses great challenges to populations with larger proportions of fragile people at older ages. Differences in population age compositions partly explain the spread and the crude fatality measures of the disease (Dowd et al., 2020). Looking at population age structures is therefore critically important to assess the potential impact of COVID-19 on mortality in Europe, the oldest part of the world with considerable variations in the degree of ageing (Kashnitsky and Schöley, 2018).
We explore differences in population age structures across European NUTS-3 regions1 (Eurostat., 2020) focusing on the crude estimate of the proportion of population expected to die due to COVID-19 (see Fig. 1 ). We assume that 5/6 of the populations get infected (Walker et al., 2020) and experience age-specific infection-fatality ratios (IFRs) modelled by the Imperial College COVID-19 Response Team (Ferguson et al., 2020). We adjust IFRs by sex ratios of age-specific case-fatality ratios observed for the pooled population of all the European countries in the COVerAGE database (Riffe and Acosta, 2020). Thus, we effectively introduce a summary measure of population age structures focused on the most vulnerable to the pandemic. The map in Fig. 1 summarizes regional differences in population age structures between the NUTS-3 regions of Europe in the context of unequal age- and sex-specific death risks associated with the spread of the COVID-19 pandemic.
Fig. 1.
COVID-19 in unequally ageing European regions. NUTS-3 regions of Europe are colored according to the deviation from the European pooled estimate of the proportion of population at risk of death due to COVID-19 – 1%. The inset plot on left shows the infection-fatality ratios by sex and age. The inset plot on the right shows the esimated proportions of people at risk of death due to COVID-19 for all the regions grouped by countries; the vertical blue marks represent country-specific population-weighted averages; the vertical grey line marks the weighted average estimate for the whole Europe. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
This approach requires careful consideration of the assumptions and limitations and the lack of high-quality data on the unfolding pandemic. The proportions of population at risk of death can predict the pandemic tolls only if (1) the age-specific profile of IFRs stays as modelled and (2) 5/6 of the population get infected (3) uniformly across regions. This is unlikely to hold true by the end of the pandemic as multiple non-pharmaceutical interventions have been put in place and others have been suggested (Block et al., 2020). Estimates of IFRs move upwards as more outcomes of the infection are known and downwards as more mild cases are registered (Russell et al., 2020). The final proportion of the population infected is difficult to predict and depends on the interventions taken that vary across countries and regions (Flaxman et al., 2020). Finally, other dimensions of structural differences in the populations may play an important role in the way the pandemic spreads. i.e. health inequalities (Nepomuceno et al., 2020) or the compositional structure of the households (Esteve, Permanyer, Boertien, & Vaupel, 2020).
Despite the limitations, the regional differences in age structures shown here are relevant for the story of the unfolding pandemic and can inform potential scenarios in Europe, as long as the relative differences in fatality between age groups stay proportional. Unlike the data on COVID-19, data on European population age structures are of great quality and shed light on the possible hotspots of the ongoing pandemic, which is highly relevant for planning public health interventions. The map reflects the unequal population age structures rather than the precise figures on COVID-19 fatality. Within Europe, population age structure differences alone can cause four-fold differences in the exposure to COVID-19 death risks.
The map highlights that if the spread of the disease is not mitigated, the most affected regions are likely to be the remote periphery with relatively old populations, which in some countries are also less likely to have enough access to healthcare (Verhagen et al., 2020). The first months of fighting the pandemic in Europe showed that the unprecedented interventions were mostly successful (Flaxman et al., 2020) but we are nowhere close to herd immunity even in the most affected areas (Vollmer et al., 2020), and the possibility of the second wave cannot be excluded.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
NUTS stands for Nomenclature of Territorial Units for Statistics. This hierarchical system of territorial division is an attempt to unify geographical levels across Europe and facilitate cross-country comparisons. NUTS-3 level usually correspond to the unit size of county, like in Sweden, or departments in France.
References
- Block P., Hoffman M., Raabe I.J., Dowd J.B., Rahal C., Kashyap R., Mills M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nature Human Behaviour. 2020;4(6):588–596. doi: 10.1038/s41562-020-0898-6. [DOI] [PubMed] [Google Scholar]
- Dowd J.B., Andriano L., Brazel D.M., Rotondi V., Block P., Ding X., Liu Y., Mills M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences. 2020 doi: 10.1073/pnas.2004911117. 10/ggsd5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve A., Permanyer I., Boertien D., Vaupel J.W. National age and coresidence patterns shape COVID-19 vulnerability. Proceedings of the National Academy of Sciences. 2020 doi: 10.1073/pnas.2008764117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashnitsky, I., Schöley, J. (2018). Regional population structures at a glance. The Lancet, 392, 10143, 209–210. https://doi.org/10/dfnv. [DOI] [PubMed]
- Eurostat. (2020). Population on 1 January by age, sex and NUTS 3 region. https://ec.europa.eu/eurostat/web/regions/data/database.
- Riffe, T., Acosta, E. (2020). COVerAGE-DB: A database of COVID-19 cases and deaths by age. 10.17605/OSF.IO/MPWJQ. [DOI]
- Ferguson, N., Laydon, D., Nedjati Gilani, G., Imai, N., Ainslie, K., Baguelin, M., … Ghani, A. (2020). Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. https://doi.org/10/ggqtdx.
- Flaxman, S., Mishra, S., Gandy, A., Unwin, H., Coupland, H., Mellan, T., … Bhatt, S. (2020). Report 13: Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. https://doi.org/10/ggrbmf.
- Nepomuceno M.R., Acosta E., Alburez-Gutierrez D., Aburto J.M., Gagnon A., Turra C.M. Besides population age structure, health and other demographic factors can contribute to understanding the COVID-19 burden. Proceedings of the National Academy of Sciences. 2020;117(25):13881–13883. doi: 10.1073/pnas.2008760117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell T.W., Hellewell J., Jarvis C.I., Zandvoortvan K., Abbott S., Ratnayake R.…Kucharski A.J. Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020. Eurosurveillance. 2020;25(12):2000256. doi: 10.2807/1560-7917.es.2020.25.12.2000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen M.D., Brazel D.M., Dowd J.B., Kashnitsky I., Mills M.C. Forecasting spatial, socioeconomic and demographic variation in COVID-19 health care demand in England and Wales. BMC Medicine. 2020;18(1):203. doi: 10.1186/s12916-020-01646-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer M., Mishra S., Unwin H., Gandy A., Melan T., Bradley V.…Bhatt S. [DOI]
- Walker P.G.T., Whittaker C., Watson O.J., Baguelin M., Winskill P., Hamlet A., Ghani A.C. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science. 2020;369(6502):413–422. doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]