Abstract
Hypertension remains the most important cardiovascular risk factor in Poland. May Measurement Month is a global initiative organized by the International Society of Hypertension aimed at raising awareness of hypertension and the need for blood pressure (BP) screening and demonstrating the potential of the opportunistic BP measurements. An opportunistic cross-sectional survey of volunteers aged ≥18 was carried out in 146 sites in May 2018. Blood pressure was measured in 6450 subjects (mean age: 41 ± 15 years; 59% females). After multiple imputation, the age and sex standardized systolic and diastolic BP was 126.7/78.4 mmHg in the whole analysed group, 132.8/81.3 mmHg in subjects taking antihypertensive drugs, and 125.7/78.0 mmHg in those not taking any antihypertensive drugs. After multiple imputation, the proportions of subjects with high BP (systolic ≥140 mmHg or diastolic ≥90 mmHg or on treatment for raised BP) were 22.2% in the whole analysed group, 39.2% in subjects taking antihypertensive drugs, and 18.6% those not taking any antihypertensive drugs. Overall, hypertension was present in 32.8% of participants, among them 38.7% were not aware of the disease, 53.1% were taking antihypertensive drugs, and 32.3% had BP controlled to target (<140/90 mmHg). Blood pressure was increasing with increasing body mass index and alcohol intake. Smokers and project participants with diabetes had increased average BP. In conclusion, this project provides additional evidence for a considerable potential for further reduction of cardiovascular risk through improvement in detection and treatment of hypertension in Poland.
Keywords: Hypertension, Blood pressure, Screening, Treatment, Control, Disease awareness
Introduction
Although cardiovascular mortality has declined since 1991, cardiovascular diseases are the greatest threat to health of inhabitants of Poland. According to the latest available national statistics, cardiovascular diseases are responsible for 43% of all deaths.1 According the National Health Fund data, the registered number of patients with coronary artery disease is about 2.48 million (about 6.4 thousand per 100 000 inhabitants), whereas almost 750 000 patients have heart failure (about 1.4 thousand per 100 000 inhabitants). The estimated annual number of hospitalizations due to acute myocardial infarction is about 80 000.
Hypertension is considered the most important cardiovascular risk factor in developed countries.2 This is also true for Poland. This is a result of the close correlation between blood pressure (BP) values and mortality as well as the high prevalence of hypertension. Indeed, the last countrywide epidemiological study aiming to assess hypertension prevalence in the general population in Poland suggested 42.7% of adults (≥19 years of age) had hypertension.3 This would mean over 13 million Poles have hypertension. Although the control of hypertension has increased significantly during last 30 years in Poland, still it is low with only about 23% of hypertensives having their BP at goal.3
As the awareness of hypertension is still insufficient in Poland, the Polish Societies of Cardiology, Hypertension, Nephrology, Family Physicians, and Study on Lipids joined the May Measurement Month (MMM) project in 2017, a global initiative organized by the International Society of Hypertension aimed at raising awareness of high BP.4 Among the Polish participants of the MMM 17 project, 21% of subjects not taking any BP-lowering drugs and 49% of those treated for hypertension had high BP.5 The results suggested that opportunistic screening can identify a substantial number of subjects with raised BP. As the MMM project was also organized in 2018, the aim of the present analysis was to provide results of the Polish part of the project.
Methods
An opportunistic cross-sectional survey of volunteers aged ≥18 was carried out in 146 study sites in May 2018. The study sites were spread around the country. Subjects were recruited by the public health messages and endorsements, family physicians, non-public outpatient clinics, and pharmacies. The definition of hypertension, BP measurement, and statistical analysis followed the approved MMM18 protocol. Each participant had BP measured and received a questionnaire about demographic, lifestyle, and environmental factors. Weight and height were also measured. Three seated BP recordings were taken with 1-min intervals between readings. Automated Omron and Microlife healthcare electronic devices were used. Where either the second of third BP reading was missing, multiple imputation using the global data6 was performed to estimate the missing reading. Hypertension was defined as systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg (based on the mean of the second and third BP measurements) or taking antihypertensive medications, whereas high BP was defined as systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg. Blood pressure goal was defined as systolic BP below 140 mmHg and diastolic BP below 90 mmHg. Funding came from non-public chains of family physicians’ network, non-public outpatients’ clinics, and pharmaceutical companies. Data were collected via the MMM App and analysed centrally by the MMM project team. The project was approved by local ethics committee.
Results
A total of 6450 subjects were screened, of whom 3771 were females, 2668 were males, and 11 unclassified. The mean age was 41.1 ± 14.9 years and median age was 38.0 years (interquartile range: 20.0 years). Supplementary material online, Table S1 presents basic characteristics of the analysed group. Based on the participants’ declarations, 17.4% of them were taking antihypertensive drugs and 66.6% had their BP measured within previous 12 months. Most of the measurements were taken during working days (see Supplementary material online, Table S1). Mean age and sex standardized BP was 126.7/78.4 mmHg in the whole analysed group, 132.8/81.3 mmHg in subjects taking antihypertensive drugs, and 125.7/78.0 mmHg in those not taking any antihypertensive drugs. The proportions of subjects with high BP were 22.2% in the whole analysed group, 39.2% in subjects taking antihypertensive drugs, and 18.6% in those not taking any antihypertensive drugs.
Overall, hypertension was diagnosed in 32.8% of participants, among them 38.7% were not aware of the disease (Figure 1). 53.1% of all subjects with hypertension were taking antihypertensive drugs. Among those who were aware of their diagnosis, 86.6% were taking antihypertensive drugs. Among treated participants, 39.2% still had high BP, whereas among those not taking antihypertensive drugs, high BP was diagnosed in 18.6%. Overall, 32.3% of all subjects with hypertension had BP well controlled (Figure 1).
Figure 1.
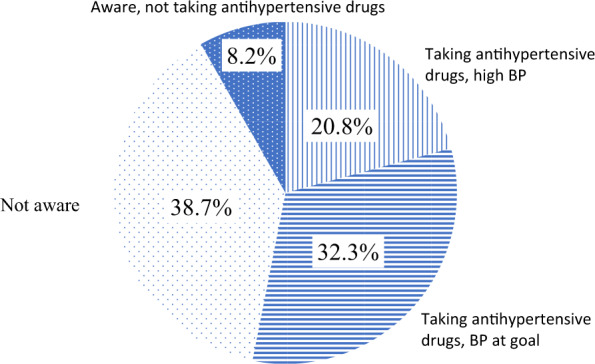
Awareness, treatment, and control of blood pressure among MMM 2018 project participants in Poland.
Both systolic and diastolic BP increased with body weight (Supplementary material online, Figure S1). Smokers had higher BP values compared with non-smokers, whereas alcohol consumers had higher systolic BP compared with participants not drinking alcohol (Supplementary material online, Figure S2). Participants with a history of myocardial infarction had higher both systolic and diastolic BP, whereas those with a history of diabetes only systolic BP. In contrast, history of stroke was not related to systolic BP, but there was a small decrease in diastolic BP (Supplementary material online, Figure S3). Patients whose BP values have been measured in outdoor public places had higher values of systolic [by 4.0 (2.1, 6.0) mmHg], but not diastolic BP [0.3 (-1.0, 1.6) mmHg] when compared with BP measurements in the hospital or clinic. Patients whose BP values have been measured in indoor public places had BP values not significantly different from patients whose BP values have been measured in the hospital or clinic [difference in systolic BP: -0.4 (-2.5, 1.7) mmHg; difference in diastolic BP: -1.3 (-2.6, 0.1) mmHg]. Patients having BP measured in pharmacy had lower systolic, but not diastolic BP when compared with BP measurements in the hospital or clinic [difference in systolic BP: -2.1 (-3.8, -0.4) mmHg; difference in diastolic BP: -0.8 (-1.9, 0.3) mmHg].
Discussion
Overall, 22.2% of the project participants in Poland had high BP, whereas 32.8% fulfilled criteria for hypertension. Importantly, only 61.3% of hypertensives were aware of their diagnosis, only 53.1% were taking any antihypertensive drugs, and only 32.3% had BP at goal. Another important finding is that almost one in five patients not taking antihypertensive drugs were found to have raised BP (18.6%).
Although the opportunistic nature of the project is related to a number of obvious limitations, the relatively high number of participants allowed a cautious comparison of data obtained in 2017 and 2018. The basic characteristics of those who participated in the 2017 and 2018 session were very similar (e.g. mean age 42.0 vs. 41.1 years, proportion of females 57.4% vs. 58.6%). Mean BP was almost identical (126.8/78.7 mmHg in 2017 vs. 126.7/78.4 mmHg in 2018) whereas the proportion of subjects with high BP among those not taking antihypertensive drugs was a bit lower in 2018 (20.6% in 2017 and 18.6% in 2018). Similarly, the proportion of participants fulfilling criteria for diagnosis of hypertension was lower in 2018 (35.3% in 2017 and 32.8% in 2018).
In the most recent (yet unpublished) Polish study LIPIDOGRAM 2015, hypertension prevalence was 40.1% in general primary care adult population. According to the most recent countrywide epidemiological study aiming at assessment of hypertension prevalence in the general population of Poland, the age-standardized prevalence, awareness, treatment, and control of hypertension were 42.7%, 59.3%, 46.1%, and 23%, respectively.3 Although the prevalence of hypertension in the MMM 18 population was significantly lower, the proportions of participants aware, treated, and those with BP at goal were very similar. About 39% of the present study participants who were taking antihypertensive drugs had high BP. Similar findings were obtained in the general population studies as well as among patients with coronary artery disease.3,7
Conclusion
This project provides additional evidence for a considerable potential for further reduction of cardiovascular risk through improvement in detection and treatment of hypertension in Poland.
Supplementary Material
Acknowledgements
We would like to thank CHDE, Microlife, Servier, Medicover, ALAB Laboratoria, CenterMed, Super-Pharm, Medycyna Praktyczna, Edra Urban & Partner, IFMSA, and PTSF for the non-financial support for MMM18. In addition, we thank all volunteer MMM18 staff and participants in Poland.
Funding
International Society of Hypertension—fee for the opinion of the Bioethics Committee.
Conflict of interest: none declared.
References
- 1. Rozkrut D, Adach-Stankiewicz E, Bielak R, Weglowska M. Statistical Year Book of the Republic of Poland 2018. Warsaw: Statistics Poland; 2018. [Google Scholar]
- 2.GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:H1736–H1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Niklas A, Flotyńska A, Puch-Walczak A, Polakowska M, Topór-Madry R, Polak M, Piotrowski W, Kwaśniewska M, Nadrowski P, Pająk A, Bielecki W, Kozakiewicz K, Drygas W, Zdrojewski T, Tykarski A; WOBASZ II investigators. Prevalence, awareness, treatment and control of hypertension in the adult Polish population—Multi-center National Population Health Examination Surveys—WOBASZ studies. Arch Med Sci 2018;14:H951–H961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poulter NR, Lackland DT.. May Measurement Month: a global blood pressure screening campaign. Lancet 2017;389:H1678–H1680. [DOI] [PubMed] [Google Scholar]
- 5. Małyszko J, Mastej M, Banach M, Tykarski A, Narkiewicz K, Hoffman P, Jankowski P, Nowicki MP, Tomasik T, Windak A, Olszanecka A, Motyl A, Nowak D, Skowron Ł, Tomaszewski M, Beaney T, Xia X, Nillson P, Poulter NR, Jóźwiak J.. Do we know more about hypertension in Poland after the May Measurement Month 2017?—Europe. Eur Heart J Suppl 2019;21:HD97–HD100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, Kruger R, Nilsson PM, Prabhakaran D, Ramirez AJ, Schlaich MP, Schutte AE, Tomaszewski M, Touyz R, Wang J-G, Weber MA, Poulter NR; MMM Investigators. May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J 2019;40:H2006–H2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jankowski P, Czarnecka D, Badacz L, Bogacki P, Dubiel JS, Grodecki J, Grodzicki T, Maciejewicz J, Mirek-Bryniarska E, Nessler J, Piotrowski W, Podolec P, Śmielak-Korombel W, Tracz W, Kawecka-Jaszcz K, Pająk A. Practice setting and secondary prevention of coronary artery disease. Arch Med Sci 2018;14:H979–H987. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


