Abstract
To raise awareness of hypertension in the general population, we have held an annual community-based nationwide campaign for blood pressure (BP) screening. The 2018 May Measurement Month (MMM) campaign in Taiwan followed a similar protocol as the 2017 MMM campaign. We recruited adults aged 20 years and older at about 800 community pharmacies across Taiwan. After a 10-min seated rest, volunteers—consisting of community pharmacists—took three BP readings using automated BP devices. The means of the 2nd and 3rd BP readings were used as the screening BP estimates. Hypertension was defined as current use of antihypertensive medications, or the screening BP of ≥140/90 mmHg. Of the 15 365 enrolled participants with a mean age of 56.8 ± 16.4 years, 53.3% were women. After imputation, we found 48.1% of the individuals had hypertension. Among participants with hypertension, 83.7% were aware, 55.0% had controlled BP, and 81.3% were medically treated, of whom 67.7% had controlled BP (<140/90 mmHg). In contrast to the global results, our results showed that the participants with diabetes mellitus, prior myocardial infarction, or stroke had higher BP than those without these comorbidities. The annual campaign experience enables us to establish a feasible approach to raising awareness and to assessing the management of hypertension in the general population. Whether the regular annual BP screening campaign makes a lasting effect on hypertension-related disease burden awaits verification.
Keywords: Hypertension, Blood pressure, Screening, Treatment, Control, Pharmacy
Introduction
The prevalence of hypertension in Taiwan has reached a plateau of ∼25% in the general population aged 18 years or over according to the reports of the 2013–15 and 2015–19 Nutrition and Health Surveys.1 Although the prevalence of hypertension is not declining in recent years, hypertension-related mortalities are decreasing. In Taiwan, cardiovascular diseases were the second leading cause of death in 2018 with a mortality rate of 165.8 per 100 000, consisting of a mortality rate of 48.8, 26.1, and 12.8 per 100 000 for heart diseases, cerebrovascular diseases, and hypertension, respectively.1 Compared with the 2017 statistics, the 2018 cardiovascular mortality rate increased by 4.5%; but decreased by 2.0% in cerebrovascular diseases, and by 1.6% in hypertension.
Raising the awareness of high blood pressure (BP) is a fundamental step in the management of hypertension. We, therefore, collaborated with the International Society of Hypertension to hold the 2017 May Month Measurement (MMM) campaign for a nationwide community-based BP screening.2 Based on the Taiwan results of the 2017 MMM campaign,3 the control rate was 64.3% in the medically treated population with hypertension and was 52.5% in the overall population with hypertension. To continue the effort on raising the awareness of hypertension and surveying the updated status of hypertension control in the general population, we launched the 2018 MMM campaign in Taiwan.
Methods
Similar to the 2017 MMM campaign,3 the 2018 MMM campaign in Taiwan was conducted by the Taiwan Hypertension Society, along with the Taiwan Health Promotion Administration and the Taiwan Pharmacist Association. After the campaign protocol was approved by the research ethics committee of the National Taiwan University Hospital, we started to recruit adults aged 20 years or more in May 2018 at about 800 community pharmacies across Taiwan, of which 43.2% were located at the northern Taiwan areas, 28.4% at the central ones, and 26.5% at the southern ones. Local ethical regulations limit adult surveys to ≥20 years.
After participants gave their informed consent, the medical history and lifestyle habits were procured using a structured questionnaire. Then, they were asked to sit in a quiet place for 10 min, and then community pharmacists used automated oscillometric sphygmomanometers to take three sitting BP readings, with each spaced 1 min apart, on the right or the left arm upheld on a table at the heart level. The means of the 2nd and the 3rd BP readings were used for the screening of BP estimates, and imputed if missing, using multiple imputation based on global data.4 Hypertension was defined as current use of antihypertensive medications, or with a screening BP of 140/90 mmHg or more. Uncontrolled BP was defined as a BP of 140/90 mmHg or more in medically treated participants. Body weight categories were defined as follows: underweight, if body mass index (BMI) was lower than 18.5 kg/m2; healthy weight, if BMI was between 18.5 and 24.9 kg/m2; overweight, if BMI was between 25.0 and 29.9 kg/m2; obese, if BMI was 30 kg/m2 and more. Data were analysed centrally by the MMM project team.
Results
A total of 15 365 Taiwanese participants with a mean age of 56.8 ± 16.4 years were enrolled into this analysis. Of them, 8183 (53.3%) were women. Before imputation, using the average of the 2nd and 3rd BP measurements, there were 6720 (63.5%) individuals with hypertension. After imputation, we found 7393 (48.1%) individuals with hypertension. Of 9357 participants not receiving antihypertensive medication, 1385 (14.8%) were hypertensive. Among the 7393 hypertensive participants, 6188 (83.7%) were aware of their high BP, and 6 008 (81.3%) were medically treated. Of the 6008 participants who were medically treated, 4066 (67.7%) had their BP controlled. Of all 7393 hypertensive patients, the control rate was 55.0%.
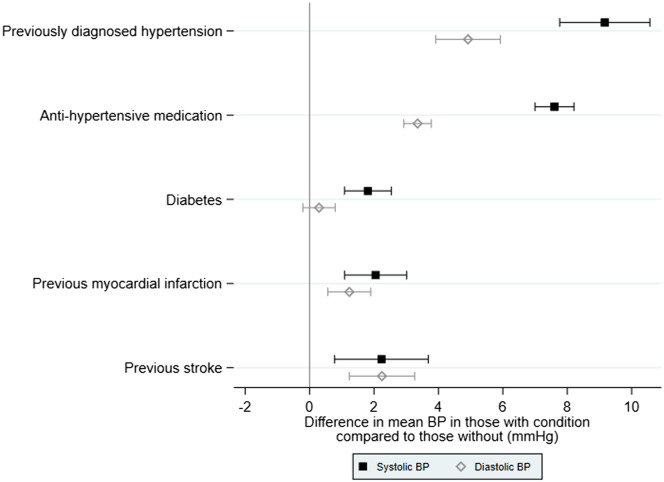
Of note, our results regarding the relationships between BP and comorbidities did not entirely concur with the 2018 MMM global results.4 As revealed in Figure 1, we found that, among participants with prior hypertension diagnosis and those treated with antihypertensive medications, BP was raised by 9.2 [95% confidence interval (CI): 7.8–10.6)/4.9 (95% CI 3.9–5.9)] mmHg and 7.6 (95% CI 7.0–8.2)/3.4 (95% CI 2.9–3.8) mmHg, respectively. In contrast, our participants with diabetes mellitus, prior myocardial infarction, or stroke, were more likely to have higher systolic BP than those without those comorbidities, whereas the global results showed the opposite relationships between BP and these comorbidities.
Figure 1.
Differences in mean blood pressures in participants with each comorbidity/risk factor compared to those without from linear regression models adjusted for age, sex, and antihypertensive medication (antihypertensive medication adjusted for age and sex alone).
There was a positive association between BP and increasing BMI. As compared with participants with healthy weight, the BP decreased by 3.0 (95% CI −4.3 to −1.7)/1.6 (95% CI −2.6 to −0.7) mmHg in underweight participants; while BP increased by 3.5 (95% CI 2.9–4.1)/2.8 (95% CI 2.4–3.2) mmHg in overweight participants, and by 5.7 (95% CI 4.6–6.8)/4.3 (95% CI 3.6–5.1) mmHg in obese participants, after adjusting for sex and age (with an interaction) and the use of antihypertensive medication.
Discussion
Among the more than 15 000 Taiwanese participants recruited in the 2018 MMM campaign, 48.1% were hypertensive. Of those with hypertension, 83.7% were aware of their hypertensive status and 81.3% were on antihypertensive medication. As for the control of hypertension, 67.7% of medically treated patients and 55.0% of the overall hypertensive patients had their screening BP controlled below 140/90 mmHg. Overall, the hypertensive population in Taiwan had higher awareness, medical treatment, and control rates than hypertensive patients worldwide, and even those in high-income countries. While our results largely concurred with the 2018 MMM global results,4 the finding that our participants with diabetes mellitus, prior myocardial infarction, or stroke had higher systolic BP than those without the comorbidities might indicate that more attention is needed to achieve optimal control of BP in hypertensive patients with the comorbidities.
Though inherently confounded by self-referral bias, our findings of this campaign could be, at least, generalized to the population with high health consciousness. Given the cumulative evidence indicating that pharmacist-based interventions could improve the management of hypertension and that the pharmacist-measured BP could be less affected by white-coat effect than office BP,5 our campaign model for BP screening in community pharmacies demonstrated an effective approach to identify hypertensive patients who are unaware, undertreated, or poorly controlled. Whether the nationwide annual BP screening campaign would improve the management status of hypertension and hypertension-related diseases in Taiwan and the rest of the world awaits verification in studies with more complex designs.
Acknowledgements
The authors sincerely thank the Taiwan Health Promotion Administration, Ministry of Health and Welfare, the Taiwan Pharmacist Association, and the pharmacists voluntarily participating this campaign for the logistic support.
Funding
The campaign was funded by the Taiwan Hypertension Society and the Taiwan Pharmacist Association.
Conflict of interest: none declared.
References
- 1. Cheng HM, Lin HJ, Wang TD, Chen CH.. Asian management of hypertension: current status, home blood pressure, and specific concerns in Taiwan. J Clin Hypertens 2019;doi:10.1111/jch13747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beaney T, Schutte AE, Tomaszewski M, Ariti C, Burrell LM, Castillo RR, Charchar FJ, Damasceno A, Kruger R, Lackland DT, Nilsson PM, Prabhakaran D, Ramirez AJ, Schlaich MP, Wang J, Weber MA, Poulter NR; May Measurement Month Investigators. May Measurement Month 2017: an analysis of blood pressure screening results worldwide. Lancet Glob Health 2018; 6:He736–He743. [DOI] [PubMed] [Google Scholar]
- 3. Lin HJ, Pan HY, Kobeissi E, Beaney T, Poulter NR, Chen WJ, Wang TD.. May Measurement Month 2017: results from Taiwan-East Asia. Eur Heart J Suppl 2019;21(Suppl D):HD115–HD117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, Kruger R, Nilsson PM, Prabhakaran D, Ramirez AJ, Schlaich MP, Schutte AE, Tomaszewski M, Touyz R, Wang J-G, Weber MA, Poulter NR; May Measurement Month Investigators. May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J 2019;40:H2006–H2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, Urbina EM, Viera AJ, White WB, Wright JT Jr.. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019;73:He35–He66. [DOI] [PMC free article] [PubMed] [Google Scholar]