Highlights
-
•
Swedish strategy is evidence-based and in close partnership between the government and the society.
-
•
No forced lockdown, but ‘soft measures’ built on trust with responsibility of the individual.
-
•
The Swedish way has also been noticed by the WHO and proposed as a future model.
-
•
Implemented measures have successfully flattened the curve.
-
•
Limited ability to implement protective measures in some elderly homes.
Keywords: COVID-19 pandemic, Sweden, Healthcare system, Health policy, Public policy, Public health surveillance
Abstract
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has challenged health care systems and put societies to the test in the world beyond expectations.
Objective
Our aim is to describe and analyze the Swedish approach in combating the pandemic.
Methods
We present and discuss data collated from various sources - published scientific studies, pre-print material, agency reports, media communication, public surveys, etc. - with specific focus on the approach itself, Covid-19 trends, healthcare system response, policy and measures overview, and implications.
Results
The main intervention to manage the curve has been the general recommendations to adhere to good hand hygiene, beware of physical distance to others, to refrain from large gatherings and restrain from non-essential travel. Persons with suspected Covid-19 infection were recommended to stay at home and avoid social contacts. Additionally, visits to the elderly care homes and meetings with more than 50 people were forbidden. As a result, the healthcare system in the country has so far, never been overwhelmed. However, the relatively high mortality among the elderly, together with the vulnerability of some migrants, points out the drawbacks.
Conclusions
Many countries have both marvelled and criticized the Swedish strategy that is formed in a close partnership between the government and the society based on a mutual trust giving the responsibility to individuals. It already highlights how much can be achieved with voluntary measures (recommendations) - something that was noticed and proposed as a future model by the World Health Organization.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has challenged healthcare systems of the world beyond expectations. The world has not seen such a fast progress of a virus with a huge impact on societies in all regions in modern times. It took only three months from the initial awareness report on 31st of December 2019 about a pneumonia, to the World Health Organization (WHO) declaring Covid-19 as a public health emergency of international concern on the 30th of January 2020, and for Covid-19 to finally be characterized as a pandemic on the 11th of March [1]. This coronavirus pandemic has put societies to the test: it is a test of political leadership, of national health systems, of social care services, of solidarity. In the face of this enormous challenge we risk deepening already stark health and social inequalities [2].
Two fundamental strategies to combat a pandemic are possible: (a) mitigation, which focuses on slowing but not necessarily stopping epidemic spread – reducing peak healthcare demand while protecting those most at risk of severe disease from infection, and (b) suppression, which aims to reverse epidemic growth, reducing case numbers to low levels and maintaining that situation indefinitely. Each policy has major challenges. As forecasted by Ferguson et al., effectiveness of any one intervention in isolation is likely to be limited, requiring multiple interventions to be combined in order to have a substantial impact on transmission [3]. The latter model, known as “Imperial”, has been already criticized in the community.
Many countries (and members of their press media) have marveled at Sweden's strategy in the face of the Covid-19 pandemic: primary schools and most workplaces have remained open, and police officers are not checking one's errands in the street. Severe critics have described it as Sweden sacrificing its (elderly) citizens to quickly reach herd immunity. The death toll has surpassed the closest neighbors, Denmark, Norway, and Finland, but the mortality remains lower than in the UK, Spain, and Belgium. It has become clear that a hard lockdown does not protect old and frail people living in care homes—a population the lockdown was designed to protect. Neither does it decrease mortality from Covid-19, which is evident when comparing the UK's experience with that of other European countries [4].
In this paper, we describe and analyze the case of Sweden, known to implement a different approach regarding the Covid-19 pandemic.
Country description
Country and health system overview
The Swedish healthcare system is governed on 3 levels (Fig. 1 ): i) the government is responsible at the national level to define policy and legislation including governance of the national agencies, such as the Public Health Agency of Sweden (PHA) and the National Board of Health and Welfare (NBHW), which are most significant in relation to the pandemic, ii) 21 regions with responsibility for healthcare, and iii) 290 municipalities providing care for the elderly and disabled.
Fig. 1.
The Swedish Healthcare Governance.
The government agencies are the most important tools to carry out the policy of the government. Ministerial rule is prohibited in Sweden, which prohibits ministers from intervening in day-to-day operations of the agencies [5]. The national agencies do not have enforcement of the regions and municipalities unless policies are mandated through a decision by parliament. Decision making in healthcare is either at the regional or municipality level with a high degree of autonomy, within the nationally defined legislation and policies. The PHA has been appointed to have an overall responsibility for communicable disease control including development of regulations as well as recommendations and guidance to ensure an effective management of communicable diseases, such as Covid-19 [6].
The Swedish healthcare is publicly financed, mainly through taxation (85%) but also through patient fees, with a 10.9 % of GDP spending placed on healthcare 2018 [7].
Swedish approach
Sweden is known to implement a different approach regarding the Covid-19 pandemic; however, the aspirations are similar to other countries: to reduce transmission and “flatten the curve”. The country's main overarching aims are outlined in the pandemic preparedness plan: a) to reduce the mortality and the morbidity in the population, and b) to minimise various negative consequences for individuals and society [8]. Thus, discussions in Sweden also focus on other objectives, such as providing opportunity for physical activity, maintaining important social functions and meeting children's needs. The ambition is to find implementation strategies that reduce the transmission of Covid-19 and reach other important health goals [9].
The strategy of the PHA first and foremost intends to protect people older than 70 years and avoid overwhelming the health system. On 1 April, PHA published regulations and general advice on everyone's responsibility to prevent the spread of Covid-19 (Fig. 2 ). These are strong recommendations related to hand hygiene, physical distancing, staying home when sick and avoiding unnecessary travel. The recommendations also outline what workplaces, public transportation, businesses, sports clubs, associations, as well as prison services and the migration board should do to combat Covid-19 [10].
Fig. 2.
How to protect oneself and others from infection, by the Public Health Agency of Sweden.
In numerous interviews, the representatives from PHA have been stressing that all the measures being implemented are only those that have established evidence to reduce the transmission, e.g., washing hands regularly and properly. In the light of this evidence-based strategy, many other measures undertaken by other countries, e.g., closing the borders [11], lack this power and can be questionable against their effectiveness. Thus, another unique feature of the Swedish approach is that the main responsibilities in the crisis management are in the hands of the experts, rather than politicians. The latter are entrusted to deal with the economic side (e.g., unemployment, support for the business sector, etc.) of the outbreak. It must be added that although claimed by foreign press and scientists inside and outside Sweden, pursuing herd immunity has been repeatedly denied by the officials to be a part of the strategy.
Hand hygiene - the basic measure
“Wash your hands frequently” - the first recommendation to everyone the PHA gives and repeats daily (Fig. 2). This basic measure is not only of utmost importance to every individual but amasses even more magnitude in health and social care. In a recent systematic review [12] regarding the cause of transmission and control measures of outbreaks in long-term facilities, the authors conclude that violation of basic infection control practices - defined as hand hygiene, disinfection and cleaning - could have a major role in the spread of infection. Hygiene routines are mandated [13] to all healthcare providers in Sweden, and there are annual surveillance audits to evaluate adherence. In healthcare under the responsibility of the regions, i.e. primary and hospital care, adherence to all aspects of hygiene routines has risen from below 60% (2010) to 82.7% (2020) [14] whereas adherence in the elderly care and assisted living, care provided by the municipalities, rose from below 40% (2010) to 59.2% (2020) [15]. Even though there has been a structured effort to improve the basic hygiene routines, the data demonstrates that it takes time to create an impact and that this was a significant risk factor at the start of the Covid-19 pandemic.
Soft measures fit for a “divergent” country
While most of the world is (or was) under some form of lockdown or “sheltering in place” order from their respective governments, Sweden employed “soft measures” in dealing with the pandemic, mainly relying on recommendations with very few legislative controls. The Swedish divergency culturally is related to its high value on secular-rational values and self-expression values where in 2006 it rated as the most individualistic of all 80 nations surveyed. Recent iterations of this study, now two waves from that 2006 report, have only shown that deviation to hold steady [16]. However, this is not the type of individuality that is often associated with the expression, as in a “rugged individualism” often describing other nations such as the US, rather Sweden's own brand which may be referred to as “Individualism with a social contract” [17]. The strategy has another important cultural characteristic to lean on for support. Being that the strategy has wide support of the public, most Swedes will follow out of a mixture of motivations, such as to avoid conflict with others, or avoid being called out as disturbing the social order. In a recent survey [18], 87% of the Swedish public have a “high level of confidence” for researchers and experts who speak publicly about the coronavirus, suggesting a high value on “expert power” for forming policies and strategies for managing the Covid-19 pandemic. Also, there has been a high level (varying though, 60-80%) of public trust with PHA and healthcare. For the most part, the population has been adherent to this guidance, and foreigners living in Sweden would frequently comment that this approach would not work in their respective countries. This approach fits what some may call the most divergent country in the world.
Covid-19 trends
Outline of data quality and sources
Sweden has a long history of national registries, which are a gold mine for research. It is possible to follow patients throughout their life via population-based registries compiled by government agencies or other organizations, or registries that are created for research purposes [19]. Sweden is also one of few countries with unique personal identity numbers [20], which make it possible to link data from different registries to a specific individual. A number of validation studies concluded that in general the registry data are valid and of good quality, e.g., Swedish death certificate data are fairly valid for use in epidemiological studies and mortality statistics [21,22], and the validity of The Swedish National Inpatient Register is high [23]. The specific Covid-19 data is collected in a registry for communicable diseases, including more than 50 diseases, where reporting is mandated by law. The registry has been operational since the late -90’s where the sensitivity, combining all diseases, of clinical and laboratory notifications was 91.6% and 95.9% respectively [24].
Overview of data and data availability
In Sweden these are the main data sources for Covid-19 status and trends:
-
1.
The Public Health Agency of Sweden (Folkhälsomyndigheten);
-
2.
The National Board of Health and Welfare of Sweden (Socialstyrelsen);
-
3.
The Swedish Intensive Care Register (Svenska Intensivvårdsregistret);
-
4.
Statistics Sweden (Statistiska centralbyrån).
Additionally, related information is also communicated by the Civil Protection and Preparedness Authority (Myndigheten för samhällsskydd och beredskap), via krisinformation.se (emergency information from Swedish authorities).
The Public Health Agency (PHA) collects and publicly reports various statistics on its webpage. The most commonly used indicators are presented on the dashboard (Fig. 3 ), which is updated daily at 14.00 CET. The information available publicly is summarised in the Table 1 .
Fig. 3.
The dashboard with the main indicators showing the status on 14 August 2020, by the Public Health Agency of Sweden.
Table 1.
Public data availability on Covid-19 in Sweden.
| Data source | Public Health Agency1,2 | National Board of Health and Welfare3 | Intensive Care Register4 |
|---|---|---|---|
| Dashboards, summary statistics |
|
|
|
| Raw data (available to download) |
|
|
|
| Reports |
|
|
|
| Notes |
|
|
All listed indicators are for the laboratory confirmed cases reported in accordance with the Infection Protection Act. The number of reported cases is constantly changing as people seek care and are examined for the virus. There is some delay in reporting data on new cases and deceased cases, so the most recent days’ report should be interpreted with caution (especially during holidays.) The statistics of deceased persons are based on data reported so far to the PHA, and show the number of people with confirmed Covid-19 who have died, regardless of the cause of death.
Laboratory-confirmed cases are an indicator for monitoring. Initially, people who were living in areas with known spread of Covid-19 were sampled. But since mid-March, people with symptoms consistent with Covid-19 infection who are in need of inpatient hospital care and/or elderly care, healthcare personnel, as well as people who are being tested in sentinel testing, are primarily being tested. This means that people with mild symptoms are not asked to contact the healthcare and therefore do not end up in the statistics of reported cases. The strategy to involve a broader testing has been developed and implemented since June.
The PHA also implements sentinel surveillance, which is commonly used for influenza and is generally based on reports made by sentinel general practitioners [25]. A sentinel surveillance system is used when high-quality data is needed about a particular disease that cannot be obtained through a passive system. Selected reporting units, with a high probability of seeing cases of the disease in question, good laboratory facilities and experienced well-qualified staff, identify and notify about certain diseases. Whereas most passive surveillance systems receive data from as many health workers or health facilities as possible, a sentinel system deliberately involves only a limited network of carefully selected reporting sites. Data collected in a well-designed sentinel system can be used to signal trends, identify outbreaks and monitor the burden of disease in a community, providing a rapid, economical alternative to other surveillance methods [26]. In connection with the spread of Covid-19 in Europe, PHA has decided to include analysis for Covid-19 in the sentinel samples. This is to get a better idea of the spread of influenza and Covid-19 as well as the risk groups and age groups affected.
Every day in spring at 14.00 CET (Monday to Friday) and twice weekly during the summer PHA has been arranging a press conference together with the representatives from NBHW and the Civil Protection and Preparedness Authority. The daily update briefly covers the situation in the World, in the country, recent trends in the incidence and mortality, as well as ICU capacity. This is often supplemented by more comprehensive analyses for specific issues, including measures being taken. The update is followed by the Q&A session, it is also being directly broadcasted to YouTube.
The National Board of Health and Welfare (NBHW) collects and reports statistics on Covid-19 that are summarised in Table 1. The statistics show deceased where the underlying cause of death was Covid-19, according to the cause of death certificates submitted to NBHW. The figures do not show the final number of deceased but are updated as more death certificates come in. Doctors send the certificates within three weeks and the final number will change as more death certificates are received. The NBHW information on deceased persons differs slightly from those presented by PHA on a daily basis. They depend on the origin of the statistics. The PHA reports only those deceased who have had a laboratory-verified Covid-19 and have died within 30 days. The NBHW reports all cases where the underlying cause of death was Covid-19, regardless of whether the diagnosis was laboratory confirmed or not.
The NBHW has produced several reports that include statistics related to Covid-19. The statistics are based on existing data available in the national registers. They estimate the number of people who are particularly vulnerable according to the assessment of PHA and are presented in more depth: by age and sex, with particular comorbidities, the number of comorbidities, and the vulnerable groups at risk in special living arrangements.
A particularly vulnerable group for more severe symptoms and infection of the coronavirus and Covid-19 is the older part of the population. The data shows how many people aged 70 and older live in special housing arrangements or have in-home services. In addition, the place of death is reported if the person has died in hospital, special accommodation or ordinary living place.
The Swedish Intensive Care Register receives data reported on cases of Covid-19 that end up in ICUs (Intensive Care Unit). The registry has existed for more than 15 years [27] and has a coverage of 95% of all ICU's in Sweden [28]. How quickly it receives data depends on local reporting procedures and local IT systems. This type of information is available publicly and updated daily as listed in Table 1.
Statistics Sweden collects and reports (see: https://www.scb.se/en/finding-statistics/coronavirus/) the preliminary number of deceased per day for the period of 2015-2020. The information is available by age group and sex, by region, by municipality, daily and weekly. According to preliminary statistics, mortality during the week 21 (18-24 May) was 14% above the 2015-2019 average, had declined since April (∼30%) and returned to normal level in June.
Covid-19 daily data and trends
The data described below is taken from the above-mentioned sources up to week 33 (9-15 August) 2020.
The main indicators
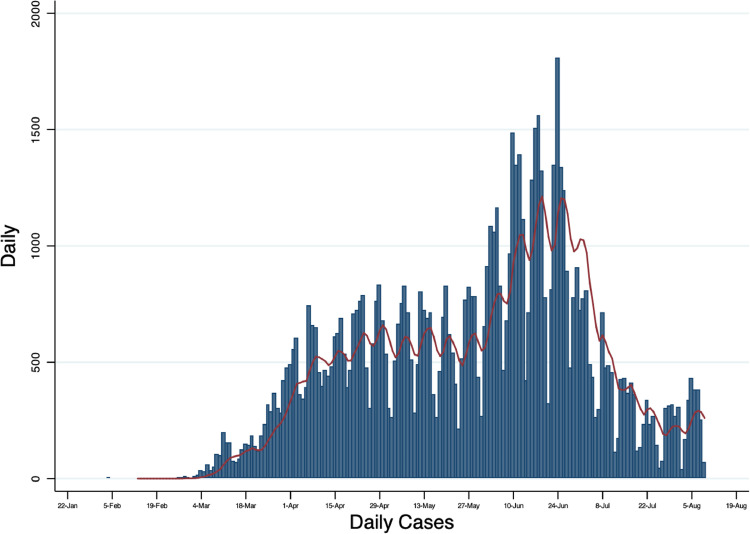
Until 13 August 2020 there were 83,852 cases in Sweden (830 per 100,000), 35,155 (42%) of them men and 48,697 women (58%). The number of new cases per day is shown in Fig. 4 . The peak was recorded towards end of June and it reflects the expansion of the testing strategy to include everyone with the symptoms of Covid-19, as well as testing to take place in cases of contact tracing or screening (even if there are no symptoms). In its weekly reports PHA presents a graph with mild and severe cases separated, with mild cases comprising the majority since the expansion of testing.
Fig. 4.
New cases per day.
The differences are apparent when looking to a regional distribution, e. g., Jonköping, 1326 cases per 100,000, Gävleborg, 1115 per 100,000, Stockholm, 1007 per 100,000 and Skåne, 294 per 100,000, Kalmar, 328 per 100,000, Blekinge 345 per 100,000. The distribution by age groups is shown in Fig. 5 . There has been no case with re-infection reported.
Fig. 5.
Total number of cases by age group.
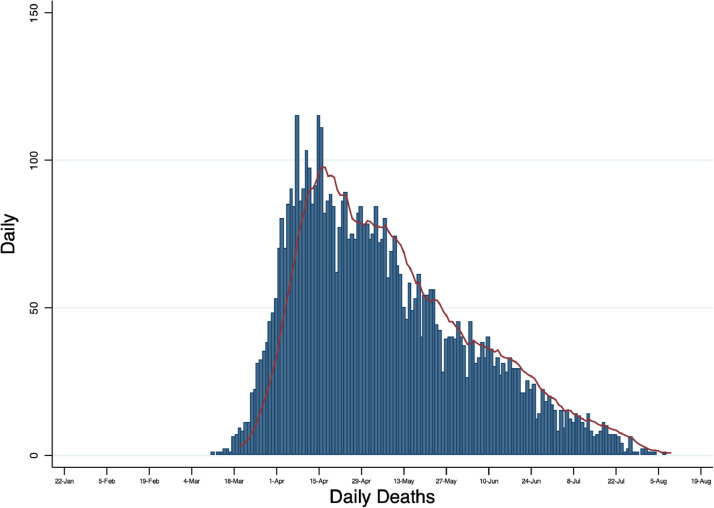
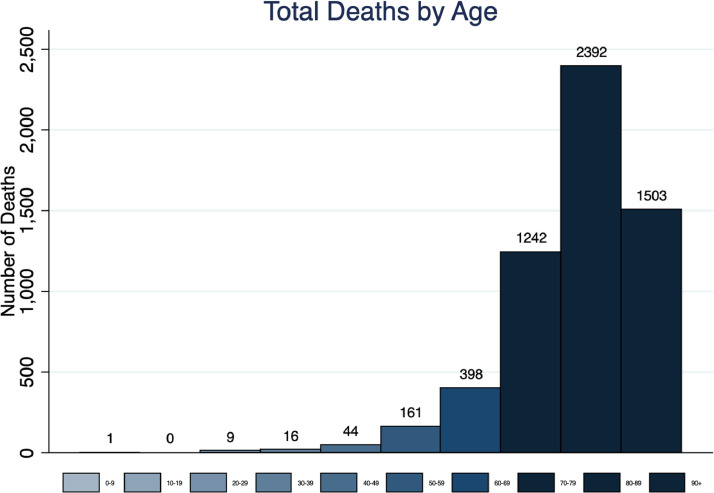
The number of deaths was 5776 (57.1 per 100,000). Of them, 3163 (55%) men and 2613 (45%) women. The number of deaths per day has been gradually declining since mid-April (Fig. 6 ), to at 1 per day recently. As shown in Fig. 7 , most of the deaths occurred in the 80-89 years old age group – 2392 (41.5%). 89.1% of those who died were 70 years or older; only 2.3% were less than 60 years old. As Sweden is a large country by area, regional differences are evident (Table 2 ). One of the examples that deserves mentioning is Skåne, a region in Southern Sweden, including Malmö (3rd largest city), where the number of cases, deaths and patients in ICU has been relatively low, more closely resembling Denmark, which has been pursuing a rather different strategy (in fact, mortality per 100.000 in May was 8.0 in Skåne vs. 16.9 in the Copenhagen capital region) [29].
Fig. 6.
Number of deaths per day.
Fig. 7.
Total number of deaths by age group.
Table 2.
Comparing 3 largest regions representing 53% of population.
| Skåne | Stockholm | Västra Götaland | |
|---|---|---|---|
| Population1 | 1 380 983 | 2 383 269 | 1 728 573 |
| Absolute diagnosed2 | 3 904 | 23 754 | 19 120 |
| Diagnosed / 100 000 | 283 | 997 | 1106 |
| Absolute mortality2 | 274 | 2 387 | 842 |
| Mortality /100 000 | 19,8 | 100,2 | 48,7 |
| Absolute number of patients in intensive care2 | 117 | 908 | 440 |
| Patients in intensive care / 100 000 | 8,5 | 38,1 | 25,5 |
| COVID-19 Community Mobility Report3 | |||
| Retail creation | 18% | -10% | 8% |
| Grocery & pharma | 6% | -6% | 5% |
| Parks | 336% | 144% | 442% |
| Transit stations | -22% | -36% | -23% |
| Workplaces | -48% | -58% | -51% |
| Residential | 7% | 9% | 8% |
The total number of patients that have been admitted to ICUs up until 13 August was 2538. Of them, 1851 (73%) men and 687 (27%) women. The number of the patients at ICUs on 13 August was 30 and the number of the patients at ICUs per day has been gradually decreasing since end of April (Fig. 8 ), as the number of newly admitted to ICUs (Fig. 9 ). It must be said, that the number of ICUs had increased substantially since the beginning and during the peak of the pandemic. The pre-pandemic level of critical care beds was 5.8 per 100,000, one of the lowest in Europe [30]. In May it was around 10 per 100,000, more precisely the number of ICUs available on 14 May was 1003, of them 423 (33%) being unused and ready for use if needed. Currently, on 13 August, the number of ICU beds decreased to pre-pandemic level, i. e., to 527, of them 321 occupied (39% being available if needed), of them 30 with Covid-19. It turned out that the healthcare system has never been overwhelmed and there has always been ICU availability for those in need.
Fig. 8.
Total number of patients at ICUs per day.
Fig. 9.
Number of newly admitted to ICUs per day.
Specific analyses
Monitoring risk groups with a presumed risk of serious illness or death from Covid-19 infection is important in order to be able to assist people with special needs for care. According to the NHBW data, among 5612 deceased with Covid-19, 2770 (49.4%) had an underlying cardiovascular disease, 4395 (78.3%) high blood pressure, 1553 (27.7%) diabetes, and 787 (14.0%) a respiratory disease. Of those, 3242 (57.8%) had two or more of those comorbidities, 1502 (26.8%) - one, and 868 (15.5%) - none of the above mentioned (Fig. 10 ).
Fig. 10.
Comorbidity distribution among deceased by sex.
Covid-19 is known to severely affect the nursing and in-home care services, and Sweden is not an exception. Among those who died with Covid-19, 2623 (46.7%) were living in special living arrangements (e.g., care homes), and 1417 (25.3%) were receiving in-home services (it is organized primarily by the municipalities and consists of assisting the individual with help in their own home so that the individual can continue to stay at home; it is usually run by staff employed by the municipality, but the services can also be purchased by private companies).
Telia Crowd Insights is a service that analyses anonymized and aggregated mobile network data that is adjusted to represent the entire population of Sweden. It is possible to look at behaviours and patterns of movement (see: https://www.telia.se/privat/aktuellt/hemma-i-folknatet/covid-19-mobilitetsanalys). When, as an example, traveling during week 19 (4-10 May) is compared to week 6 (3-9 February), before the spread of Covid-19 took off in Sweden, travel has decreased by 16%. When looked at three major regions, change in the number of daily trips reduced by 23% in Stockholm, 18% in Västra Götaland, and 14% in Skåne. Telia also shows the similar numbers for the neighbouring countries, which can be compared with Denmark (-13%), Norway (-12%), and Finland (-20%) during the week 19.
On 28 April Region Stockholm also announced statistics about the number of infected and deceased by municipality [31]. The highest cumulative number of cases per 10,000 was 74, recorded in the Rinkeby-Kista area, the second highest was 59, recorded in the Spånga-Tensta area, with the average for the region being 30. The above-mentioned areas had also the highest number of deaths: 12.9 and 10.4 per 10,000, respectively. These areas are well known for the high immigrant and persons with foreign background population proportions.
Predictions, modelling, and other studies
PHA regularly updates the estimation of the instantaneous reproduction number Rt (the reproduction number calculated at different time points during the epidemic, i.e. the average number of expected infected persons by a primary case if conditions remain the same) which was 0.87 (95%CI: 0.73-1.01) on 30 July 2020 (the last available) [32].
On 21 April, 2020 PHA published the report using a mathematical model to estimate the spread of Covid-19 in Stockholm County between February and April 2020. The results show that the day with the highest number of infectious persons Stockholm County occurred on April 8 with 70,500 contagious at the same time. According to the modelling, about 26% (616,655; 95%CI: 11.5%-50.7%) of the population in Stockholm County will be or have been infected with Covid-19 on the first of May. The model takes into account both reported cases that have been confirmed by the healthcare system to be infected with SARS-CoV-2 and unconfirmed cases [33].
A similar model, showing that the peak of infections appears in mid-April and infections start settling in May when 1/3 of the population in the region has been infected, was estimated by Tom Britton, Stockholm University [34].
A new mathematical modelling by Tom Britton et al., shows that herd immunity can be achieved already when 40 percent of the population has had Covid-19. The herd immunity levels are clearly lower than previously calculated, which means that fewer need to be infected before the immunity protection against further outbreaks and spread of infection is achieved. Herd immunity is achieved when a sufficient number of people in a population have been infected and become immune so that the spread of the disease clears and ceases, even after restrictions have been relieved. If herd immunity has not been achieved before lifting restrictions, a second wave of contagion can be expected. Earlier calculations have predicted that about 60% of the population needs to be immune for herd immunity to be achieved. This figure applies to the vaccine immunity, but not to disease immunity that is not evenly distributed. With the help of new mathematical modeling calculations, two research teams, independently of each other, have now concluded that this figure can be significantly lower [35].
Arguably, one of the most interesting report is on estimating the infection fatality rate that is 0.1 (95%CI, 0.1 - 0.2) for the age group under 70 years old, and, not surprisingly, a much higher estimate of 4.3 (95%CI, 2.7-7.7) for the older group [36]. To add, a report on the demographic factors [38] showed the median age of those deceased with Covid-19 to be 84 years. Given the life expectancy in Sweden is 82 years, it´s a well framed question on potential years of life lost for future research. The same report also revealed a higher incidence and mortality for the citizens born outside Sweden (e.g., the highest incident among those born in Turkey, 753 per 100.000 vs. Swedes, 189 per 100.000; the highest mortality among Finns, 145 per 100.000 vs. Swedes, 32 per 100.000). Additionally, taxi drivers were found to have 4.8 times higher risk for getting infected compared to other occupations; with the school staff having no higher risk than other occupations [39].
The PHA has analysed how school closures in Sweden would affect workplace absenteeism for caregivers in an epidemic. According to the report, the regions would find it very difficult to fulfil their mission during the pandemic. In relatively favourable conditions, the absence of a doctors and nurses amounts to 43,000 or a tenth of the personnel [40].
Almost 25 percent of the staff at Danderyd Hospital who had been in contact with Covid-19 patients had developed antibodies against SARS-CoV-2 early this summer [41]. In the light of media´s focus on antibody levels, it is worthy to remind that T-cells are actually specialised in recognising virus-infected cells and are an essential part of the immune system. According the preliminary results, many people with mild or asymptomatic Covid-19 demonstrate so-called T-cell-mediated immunity to the new coronavirus, even if they have not tested positively for antibodies [37].
According to the primary investigation by The Swedish Palliative Register, it is many times safer and calmer for the elderly and often multi-sick person who lives in a special place to stay in their habitual environment instead of being moved. The register has so far received data on over 700 people who have died as a result for Covid-19 and the register shows that the final days for these elderlies was calmer for those who died in special housing compared to those who died in the hospital [42] .
This article is not meant to discuss in details other modelling studies and possible miscalculations that have been circulating, e.g., estimating median mortality of 96,000 by May – a far departure from the actual [43].
Policy roadmap
Policy and measures: overview and development
The policy interventions are grouped by the primary objective of the intervention, the organization responsible for the measure and when implemented (Fig. 11 ; also, in Supplementary material). The measures to manage the curve include only a few legislative measures including international travel restrictions, size of public gatherings and additional requirements for restaurants, bars, cafes, schools dining rooms, catering activities, and the restriction of visits to elderly homes. The main intervention to manage the curve has been the general recommendations by the PHA to adhere to good hand hygiene (wash with soap), beware of physical distance to others (outdoors and indoors, when using public transportation), to refrain from large gatherings (parties, funerals, christenings, weddings etc.) and restrain from non-essential travel. Persons with suspected Covid-19 infection were recommended to stay at home and avoid social contacts. Contact tracing was implemented intensively in the early start of the pandemic, but once the transmission in the community was stated, it was abandoned as not feasible anymore. Currently, PHA recommends to carry forward contact tracing by patients themselves.
Fig. 11.
Timeline of policy interventions.
The measures implemented can also be characterized as sustainable and bearable for longer time, however they might be reviewed in response from the public. As there are more talks on the second wave, there might be also more local focus to the outbreaks, also various sectors (e.g., education, transport) are currently revising their practices together with PHA that recently published the modelling scenarios for the autumn as support for the planning and preparation [44].
An important measure to prevent the spread has been the temporary modification to sick-leave compensation, removing the financial impact on the company and/or the employee while choosing to be at home when in doubt of disease. In addition, protection of the old and vulnerable beyond the restriction from visiting elderly homes, includes specific recommendations to individuals above 70 years old and persons with other underlying risk factors. These recommendations include limiting social contacts, avoiding public transportation and shopping for groceries, at pharmacies, or being at crowded places. Recognizing the limitations to full adherence of the hygiene routines [15] in elderly care, the recommendation has been not to use personal protective equipment (PPE) since this may lead to a false sense of safety which risks having a negative impact on the basic hygiene routines which are more important. In settings where the basic hygiene routines are well established, PPE may be added as an additional measure. The healthcare and capacity and performance, which is the responsibility of the regions, includes a few national policies to manage the extra-ordinary situation. In order to increase ICU capacity, the government instructed the NBHW to function as a national coordinator to ensure expansion to meet needs [45]. The NBHW was further designated to coordinate material supply to the healthcare among the regions, in order to ensure optimal use of the critical supply. On 17th of April PHA presented a national strategy to increase testing from 50,000 per week to 150,000 per week. Even though a recommendation was given to close municipal adult education and vocational adult schools, secondary schools and universities, the decision was to keep preschools and primary schools open with the objective to keep the healthcare professionals available, with this also being an essential measure for the broader economy. To sustain the economy, the total investment is valued to be 3.8 % of GDP [46], including an array of activities, e.g., support to business as well as specific sectors such as media, culture and sports. In order to minimize the effect on companies who had a temporary drop in business, a solution for temporary unemployment payment was introduced which allows the companies to make the employees temporarily redundant during the drop where the company only has to carry approximately 30% of the cost of the employee while the government will cover the remaining cost, with limited impact on the income of the employee.
Policy reach in ethnic groups
Sweden has emerged from being a homogenous country to becoming a multicultural and multiethnic society with more than 19.6% of its population born or having affiliation from another country [47]. There are a plethora of studies indicating that migrants in Sweden tend to have poor health in comparison with Swedish born, as indicated by overrepresentation in statistics of health issues such as mental health, obesity, stress, poor dental health, certain forms of cancer, low participation in physical activities [48], [49], [50].
Furthermore, there are studies that have shown that migrants encounter a multitude of challenges in the process of accessing healthcare services. These studies point out an array of factors that impacts the health of migrants in Sweden and they include a lack of culturally sensitive information on how the healthcare system functions in Sweden and information on the management of illnesses, health and disease. Additionally, unsatisfactory encounters with healthcare professionals have been demonstrated to constitute a major reason as to why migrants refrain from seeking healthcare services. Poor command of the Swedish language, alongside migrants' own cultural norms and beliefs also influence the ways in which they relate with the healthcare system and how they care for their health [51], [52], [53], [54].
From a cultural perspective, Swedes in general hold a very high value in being self-sufficient and taking responsibility, and therefore, approach their health concerns from a place of personal responsibility, not wanting to be a burden either for those close to them nor to the healthcare system. This cultural trait is somewhat divergent from many other cultures including a large sector of the migrant community where healthcare workers from outside the community are not trusted for their expert knowledge, rather may be regarded as “suspect.” A large proportion of the migrant community in Sweden come from cultures that are more communitarian in nature where trust is extended mainly to those inside the community and all members of the community take responsibility for each other, including with health concerns [17,[55], [56], [57], [58], [59]].
One lesson to take away during these unprecedented Covid-19 times in Sweden is the way the government and decision makers have had to rely on migrant community leaders, representatives of migrant associations, religious leaders and other influencers to reach out with culturally sensitive information. It is important to note that the high rate of deaths among migrants cannot solely be explained by the lack of information on Covid-19, but also by other underlying factors such as housing congestion, poor health conditions and the living conditions of some migrant groups [60], [61], [62].
Elderly homes
Due to the reported problems with excess mortality in some elderly homes, the Health and Social Care Inspectorate, carried out an evaluation of 1045 elderly housing units, where it was detected that approximately 10% had severe deficiencies in relation to how they handle the pandemic [63,64]. Table 3 provides a summary of the factors that influence the outcomes. In addition to issues related to operations of the elderly homes, challenges in collaboration between the municipalities and the regions have been suggested as an important factor contributing to problems within the elderly homes [65]. Personnel at the municipalities decide when a doctor should be contacted for assessment of individuals in the homes and most of the assessments at these assisted living/elderly care facilities are usually done telephonically. During this pandemic, the authors describe cases in which initiation to test asymptomatic individuals by medical doctors was opposed by municipalities [65]. In a press conference on 27th of May the director general of IVO announced that when it comes to the elderly in assisted living facilities, it may be that proper assessment of patients by a doctor were not performed. Being that this assessment is the first step toward admission to hospital if needed, a higher risk factor is inevitable if these assessments are not performed for those who may be in need of hospitalization.
Table 3.
Audit summary from 1045 elderly care units, factors influencing the COVID-19 outcomes
| Positive impact 1 | Negative impact 1 |
|---|---|
|
|
Economic and financial fluctuation
The preliminary results of the Swedish GDP indicate a drop 0.3% compared to previous quarter [46]. Comparing unemployment in March to April 2020 with the same period in 2019 shows that the number of unemployed who received a job decreased by 19.7% and the additional unemployment increased by 52.9% resulting in a total unemployment 10.0% higher compared to the same period last year. In addition, there were 420,000 people on temporary leave, representing an additional 65.1% increase of temporary unemployed, with compensation from the government to support businesses which have temporary problems due to Covid-19. This group is anticipated to increase to 550 000, at a total cost of 95 billion SEK.
Discussion and policy implications
In a situation where the perspective of the pandemic is shaped by media and politics, it is important to take a step back to reflect upon the perceived objectives and what may be more relevant objectives to evaluate the policy measures against (Fig. 12 ). Firstly, who are the most vulnerable, secondly, who, due to their essential function (e.g., healthcare workers), need protection but also can serve as ‘shielders’ [66], and finally what the prospect is for the broader population. That would be followed by what drives the rationale for the chosen strategy to manage the curve - is it to match demand and capacity, to delay or to somehow prevent the effect until there is a permanent solution in place with vaccines or drugs? This should be balanced against the impact on the economy, general wellbeing of citizens and other aspects of health. The protection of the old and vulnerable primarily require different actions than those to manage the curve and may lose attention unless clearly articulated. The severity and vulnerability of those who inevitably will be infected will determine the appropriate treatment strategy, where the recognition of ability of the patient to withstand the more demanding ICU-treatment may lead to a decision that it may be more beneficial for the patient to receive palliative care.
Fig. 12.
Covid-19 policy discussion framework.
If to return to an issue of media reporting, a recent publication by Irwin [67] clearly depicts the biases and misinformation towards Sweden and Covid-19, particularly, when it comes to such popular narratives as [1] Life is normal in Sweden, [2] Sweden has a herd immunity strategy, [3] Sweden is not following expert advice, [4] Sweden is not following WHO recommendations [5] the Swedish approach is failing.
Managing the curve
The self-reported adherence to the ‘soft’ guidelines is regularly assessed by surveys, which demonstrate a high degree of compliance to the measures such as hygiene, keeping physical distance and to a somewhat lesser degree in relation to avoiding social gatherings outside the home. From the perspective of managing the curve in order not to burden the healthcare system the measures in Sweden have been effective, with the ICU-capacity never becoming exhausted. When different regions in Sweden are compared, Stockholm, which had the initial peak and was therefore caught off guard, differs from the other regions which had an advantage of having a few weeks to prepare before their peak. While the same policy has been applied across Sweden the outcomes are different, where Stockholm has more than a five-fold mortality then Skåne (Table 2). Even though some of this can be explained by the less aggressive start of the pandemic in Skåne, it would also suggest that there are other underlying factors that are more significant. Skåne and Västra Götaland both have higher mobility according to 5 out of 6 categories.
To add, in a recent systematic review [68] of the role of children in the transmission of the disease, the authors conclude that this population group is not the driver of the pandemic, thus opening up schools and kindergartens is unlikely to impact the mortality rates in older people. Recently, the European Centre for Disease Prevention and Control published a report, highlighting Swedish experience and urging to reopen schools as soon as possible [69]. Swedish perspective may offer invaluable insights into reopening education facilities worldwide. To add, The Statistics Norway analysis [70] suggests that the daily cost of closing their schools and kindergartens to be 1.7 billion NOK.
Protecting the old and vulnerable
There were known limitations in elderly care such as the adherence to hygiene routines, organizational challenges in the collaboration between municipalities and regions as well as other aspects which came to light in the pandemic. Even though more could have been done in some instances, this mainly represents structural challenges which require significant work and time to address and as such not likely addressed in time for the pandemic. The question is how these deficiencies will be addressed moving forward.
In addition to the above, multigenerational households with poor socioeconomic status have been left in a vulnerable situation, where the younger generation may be working in an environment such as taxi driving where the risk of infection is high with no option to shield the old and vulnerable in the same household.
Failing to reach ethnic groups
The strategy and approach relied on a response specific to the Swedish culture and thus failed to reach many ethnic groups. This challenge has previously been recognized and methods developed for how to overcome this, yet these methods was not deployed. We hope the painful insights from this, will lead to a more pro-active management of this in the future.
Managing the infected
Patients with severe Covid-19 can be extremely exhausted post hospitalization, especially those who required respirator treatment in ICUs, and neurological and psychiatric disorders have been observed in some of these patient categories. What this entails for the individual as well as for the society (cost) is still too early to say. In depth analysis will be required to assess decision making regarding the level of treatment (home, hospital, ICU) and for individuals in elderly homes at onset of palliation. Based on studies showing that most individuals who contract Covid-19 have mild symptoms, it is probable that those with mild to moderate severity in Sweden self-isolated after being in touch with the Swedish Healthcare Guide 1177 (online or telephone). Moreover, incoming Swedish data show that only a small proportion of hospitalized patients actually require ICU care and that mortality is higher in those patients compared to those who only received care in hospital wards.
Conclusions
Sweden's strategy to combat the pandemic can be characterized as evidence-based and in close partnership between the government and the society, built on mutual trust and giving the responsibility to the individual. It already highlights that much can be achieved with voluntary measures (recommendations). The Swedish way has also been noticed by the WHO and proposed as a future model.
The healthcare system in the country has never been overwhelmed and thus it is possible to conclude that “flattening the curve” has been successful. However, relatively high mortality among the elderly when compared to other Nordic countries has been much debated and discussed. Whether success of a strategy depends on the level of restrictions, is yet to be answered, but it is already evident that this correlation is not coherent; the sporadic association between repressive measures and mortality is yet confounded - a typical epidemiological phenomena - and many other factors, e.g., population density, healthcare and social care organization, household size, the proportion of vulnerable population groups and the elderly, lifestyle (e.g., smoking) and environmental (e.g., air pollution) risk factors, tourism and travelling patterns, even capability to reorganize working practices (remote work), will need to be taken into account to get a fuller picture.
Inevitably, more and more analyses are on their way to elucidate both health and social care related questions regarding the pandemic impact in terms of incidence, hospitalization, rehabilitation, mortality, excess mortality, life expectancy and causality (dying with vs. dying from). However there are other factors to consider when designing and evaluating the strategies, including the disruption of healthcare and education in countries with lockdowns in place (which have had relatively smaller consequences in Sweden) including mental health risks, violence, crime and violation of human rights, as well as broader analyses on the impact on unemployment, businesses and other sectors.
Acknowledgments
We would like to acknowledge Naomi Moy from the University of Bologna (Bologna, Italy), for helping with data visualisation, and Kia Wärn for helping with data extraction of policy initiatives.
Author Statements
Funding
None
Declaration of Competing Interest
None declared
Ethical approval
Not required
Footnotes
Competing interests: AK is also employed by Takeda Pharma AB. PO and IL declare no conflict of interest. JM is an independent consultant. MK is a CEO of Synergus RWE AB.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.hlpt.2020.08.009.
Appendix. Supplementary materials
References
- 1.Coronavirus Disease (COVID-19) - events as they happen [Internet]. [cited 2020 Apr 9]. Available from:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- 2.The Lancet Public Health COVID-19 puts societies to the test. Lancet Public Health. May 2020;5(5):e235. doi: 10.1016/S2468-2667(20)30097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferguson N, Laydon D, Nedjati Gilani G, Imai N, Ainslie K, Baguelin M. Imperial College London; Mar 2020. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand [Internet]http://spiral.imperial.ac.uk/handle/10044/1/77482 [cited 2020 May 16]. Available from: [Google Scholar]
- 4.Giesecke J. The invisible pandemic. The Lancet [Internet] 2020 doi: 10.1016/S0140-6736(20)31035-7. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31035-7/abstract May 5 [cited 2020 May 16];0(0). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government Offices in Sweden . 2015. Public agencies and how they are governed [Internet]https://www.government.se/how-sweden-is-governed/public-agencies-and-how-they-are-governed/ [cited 2020 May 27]. Available from: [Google Scholar]
- 6.Our mission - The public health agency of Sweden [Internet]. [cited 2020 May 27]. Available from:http://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/about-us/our-mission/
- 7.Hälso- ochsjukvårdens andel av BNP var 10,9 procent 2018 [Internet]. Statistiska Centralbyrån. [cited 2020 May 27]. Available from:http://www.scb.se/hitta-statistik/statistik-efter-amne/nationalrakenskaper/nationalrakenskaper/halsorakenskaper/pong/statistiknyhet/halsorakenskaper-2018/
- 8.Pandemiberedskap, hur vi förbereder oss.:62.
- 9.IGGBerlin V.An insight into COVID-19 in Sweden [Internet]. Institut für Globale Gesundheit Berlin. 2020[cited 2020 May 16]. Available from:https://institut-fuer-globale-gesundheit.de/?p=2471
- 10.Gemensamma författningssamlingen avseende hälso- och sjukvård, socialtjänst, läkemedel, folkhälsa m.m. Folkhälsomyndighetens föreskrifter och allmänna råd om allas ansvar att förhindra smitta av covid-19 m.m.; [Internet]. [cited 2020 May 16]. Available from:https://www.folkhalsomyndigheten.se/contentassets/a1350246356042fb9ff3c515129e8baf/hslf-fs-2020-12-allmanna-rad-om-allas-ansvar-covid-19-tf.pdf
- 11.Updated WHO recommendations for international traffic in relation to COVID-19 outbreak [Internet]. [cited 2020 Aug 16]. Available from: https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbreak
- 12.Lee MH, Lee GA, Lee SH, Park Y-H. A systematic review on the causes of the transmission and control measures of outbreaks in long-term care facilities: Back to basics of infection control. PLOS ONE. 2020 Mar 10;15(3) doi: 10.1371/journal.pone.0229911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basal hygien i vård och omsorg. SOSFS 2015:10 [Internet]. [cited 2020 May 21]. Available from:https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/foreskrifter-och-allmanna-rad/2015-5-10.pdf
- 14.Carl R. Punktprevalensmätning av följsamhet till basala hygienrutiner och klädregler. Regionernas resultat. 2018 2020;17. [Google Scholar]
- 15.Einar S. Punktprevalensmätning av följsamhet till basala hygienrutiner och klädregler. kommunernas resultat. 2018 2020;17. [Google Scholar]
- 16.World Values Survey wave 5 (2005-2008) [Internet]. [cited 2020 May 18]. Available from: http://www.worldvaluessurvey.org/WVSDocumentationWV5.jsp
- 17.Berggren H, Trädgård L. Är Svensken Människa: Gemenskap och Oberoende i Det Moderna Sverige. Nordstedts. 2006 [Google Scholar]
- 18.Coronavirus in the Swedish media study - high public confidence in researchers and healthcare professionals [Internet]. [cited 2020 May 18]. Available from: https://www.alphagalileo.org/en-gb/Item-Display/ItemId/190972?returnOther=https://www.alphagalileo.org/en-gb/Item-Display/ItemId/190972
- 19.Emilsson L, Lindahl B, Köster M, Lambe M, Ludvigsson JF. Review of 103 Swedish healthcare quality registries. J Intern Med. 2015;277(1):94–136. doi: 10.1111/joim.12303. [DOI] [PubMed] [Google Scholar]
- 20.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. Nov 2009;24(11):659–667. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Faire U, L Friberg, Lorich U, Lundman T. A validation of cause-of-death certification in 1 156 Deaths. Acta Med Scand. 1976;200(1–6):223–228. doi: 10.1111/j.0954-6820.1976.tb08223.x. [DOI] [PubMed] [Google Scholar]
- 22.Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765–773. doi: 10.1007/s10654-017-0316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011 Jun 9;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jansson A, Arneborn M, Ekdahl K. Sensitivity of the Swedish statutory surveillance system for communicable diseases 1998-2002, assessed by the capture-recapture method. Epidemiol Infect. Jun 2005;133(3):401–407. doi: 10.1017/s0950268804003632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sentinel surveillance [Internet]. European centre for disease prevention and control. [cited 2020 May 19]. Available from:https://www.ecdc.europa.eu/en/seasonal-influenza/surveillance-and-disease-data/facts-sentinel-surveillance
- 26.WHO | Sentinel surveillance [Internet]. WHO. World Health Organization; [cited 2020 May 19]. Available from:https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/sentinel/en/
- 27.Sjöberg F, Walther S. Intensive care registries and the evolution of the concept of ‘quality of care’ – reflections from the 10-year anniversary symposium of the Swedish intensive care registry. Acta Anaesthesiol Scand. 2012;56(9):1073–1077. doi: 10.1111/j.1399-6576.2012.02757.x. [DOI] [PubMed] [Google Scholar]
- 28.Svenska Intensivvårdsregistret, 2018, Årsrapport. Sammanfattning, analys och reflektion [Internet]. [cited 2020 May 16]. Available from:https://www.icuregswe.org/globalassets/arsrapporter/analyserande_arsrapport_2018.pdf
- 29.Wessman J.Covid-19: allt färre i intensivvård i Danmark men hittills fler dödsfall på Själland än i Skåne [Internet]. [cited 2020 May 31]. Available from:https://www.newsoresund.se/covid-19-oresund/
- 30.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012 Oct 1;38(10):1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 31.28 april: Antal smittade och avlidna med covid-19 per kommun och stadsdel [Internet]. [cited 2020 May 19]. Available from:https://www.sll.se/verksamhet/halsa-och-vard/nyheter-halsa-och-vard/2020/04/28-april-antal-smittade-och-avlidna-med-covid-19-per-kommun-och-stadsdel/
- 32.Riket skattning av det momentana reproduktionstalet 2020-08-03.:5.
- 33.Skattning av peakdag och antal infekterade i covid-19-utbrottet i Stockholms län februari-april 2020.:26.
- 34.Britton T. Basic estimation-prediction techniques for Covid-19, and a prediction for Stockholm. medRxiv. 2020 May 14 2020.04.15.20066050. [Google Scholar]
- 35.Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020 Aug 14;369(6505):846–849. doi: 10.1126/science.abc6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The infection fatality rate of COVID-19 in Stockholm – Technical report.:30.
- 37.Robust Tcell immunity in convalescent individuals with asymptomatic or mild COVID-19 | bioRxiv [Internet]. [cited 2020 Aug 16]. Available from:https://www.biorxiv.org/content/10.1101/2020.06.29.174888v1 [DOI] [PMC free article] [PubMed]
- 38.Covid-19. Demografisk beskrivning av bekräftade covid-19 fall.:15.
- 39.Förekomst av covid-19 i olika yrkesgrupper.:11.
- 40.Vårdpersonalens frånvaro vid skolstängning.:13.
- 41.Var femte anställd på Danderyds sjukhus har haft smittan [Internet]. DN.SE. 2020 [cited 2020 May 16]. Available from:https://www.dn.se/sthlm/var-femte-anstalld-pa-danderyds-sjukhus-har-haft-smittan/
- 42.Ahlgren K. Ny studie från Kalmar: Så är sista tiden för äldre som dör i corona. SVT Nyheter [Internet]. 2020 May 10[cited 2020 May 16]; Available from:https://www.svt.se/nyheter/lokalt/smaland/sss-11
- 43.Gardner JM, Willem L, Wijngaart W van der, Kamerlin SCL, Brusselaers N, Kasson P. Intervention strategies against COVID-19 and their estimated impact on Swedish healthcare capacity. medRxiv. 2020 Apr 15;2020.04.11.20062133.
- 44.Scenarier. Tre smittspridningsscenarier inom regeringsuppdraget.:35.
- 45.Regeringskansliet R och Work in the areas of public health, medical care, social care and social insurance with regard to the COVID-19 virus [Internet] Regeringskansliet. Regeringen och Regeringskansliet. 2020 https://www.government.se/articles/2020/03/s-work-in-the-areas-of-public-health-medical-care-social-care-and-social-insurance-with-regard-to-the-covid-19-virus/ [cited 2020 May 18]. Available from: [Google Scholar]
- 46.Andersson FM. Läget i ekonomin och uppföljning av regeringens åtgärder.:25.
- 47.Utrikes födda i Sverige [Internet]. Statistiska Centralbyrån. [cited 2020 May 20]. Available from:http://www.scb.se/hitta-statistik/sverige-i-siffror/manniskorna-i-sverige/utrikes-fodda/
- 48.Tinghög P. Migration, Stress and mental ill health : post-migration factors and experiences in the Swedish context. 2009[cited 2020 May 20]; Available from:http://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-18216
- 49.Akhavan S.The health and working conditions of female immigrants in Sweden [Internet]. Institutionen för folkhälsovetenskap / Department of Public Health Sciences; 2006[cited 2020 May 20]. Available from: http://openarchive.ki.se/xmlui/handle/10616/37871
- 50.Björngren Cuadra C, Cattacin S. Malmö University; MalmöIMER: 2007. Migration and health: difference sensitivity from an organisational perspective. editors. [Google Scholar]
- 51.Sundbeck M . Studentlitteratur; Lund: 2010. Omvårdnad i mångkulturella rum - frågor om kultur, etik och reflektion. ISBN 978-91-44-05307-3. [Google Scholar]
- 52.Nyampame I. Invandrade Kvinnors Hälsa i Sverige, - Om Genus Och Etnicitet. Socialmedicinskt tidskrift, Vol. 85, No. 3, 2008. Available from: https://socialmedicinsktidskrift.se/index.php/smt/issue/view/23.
- 53.Wamala S, Merlo J, Boström G, Hogstedt C. Perceived discrimination, socioeconomic disadvantage and refraining from seeking medical treatment in Sweden. J Epidemiol Community Health. 2007 May 1;61(5):409–415. doi: 10.1136/jech.2006.049999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Groglopo A. Stockholm; Fritze;: 2006. Hälsa, vård och strukturell diskriminering: rapport. editor. 232 p. (SOU) [Google Scholar]
- 55.Daun Å. Raben & Sjögren; Stockholm: 1989. Svensk mentalitet : ett jämförande perspektiv. [Google Scholar]
- 56.Daun Å. En Stuga På Sjätte Våningen: Svensk Mentalitet i En Mångkulturell Värld. Brutus Östlings Bokförlag Symposium. 2005 [Google Scholar]
- 57.Trompenaars F, Hampden-Turner. Riding the waves of culture: understanding diversity in global business 3/E (9780071773089):, [Internet]. Charles: Books; [cited 2020 May 20]. Available from:https://www.amazon.com/Riding-Waves-Culture-Understanding-Diversity/dp/0071773088
- 58.Fukuyama F. Free Press Paperback, Simon & Schuster; 1995. Trust: the social virtues and the creation of prosperity. [Google Scholar]
- 59.LeBaron M, Pillay V. 1st edition. Nicholas Brealey; Boston: 2006. Conflict across cultures: a unique experience of bridging differences; p. 240. [Google Scholar]
- 60.Lecerof SS, Stafström M. Lunds universitet; 2011. Olika Villkor - Olika Hälsa - En Osynlig Intervention. Malmö högskola, Uppsala universitet. [Google Scholar]
- 61.Baker U, Allebeck P.Hälsokommunikatörer i Stockholms Län - En Utvärdering Av Projektverksamheten 2010-2011. [Internet]. [cited 2020 May 20]. Available from:http://dok.slso.sll.se/CES/FHG/Jamlik_halsa/Rapporter/halsokommunikatorer-i-stockholms-lan_utvardering-2010-2011.2012.pdf
- 62.Kända rappare sprider coronainformation till svensk-somalier [Internet]. DN.SE. 2020 [cited 2020 May 25]. Available from:https://www.dn.se/kultur-noje/kanda-rappare-sprider-coronainformation-till-svensk-somalier/
- 63.IVO.se. Tillsyn av vård och behandling på landets samtliga särskilda boenden för äldre [Internet]. IVO.se. [cited 2020 May 28]. Available from: https://www.ivo.se/publicerat-material/nyheter/2020/tillsyn-av-vard-och-behandling-pa-landets-samtliga-sarskilda-boenden-for-aldre/
- 64.IVO.se. IVO:s tillsyn av äldreomsorgen under COVID-pandemin [Internet]. IVO.se.[cited 2020 May 28]. Available from:https://www.ivo.se/tillsyn/ivos-granskning-av-aldreomsorgen-under-covid-pandemin/
- 65.Hammarström A, Läkare L, vd Kwiatkowska vårdföretaget, geriatriker MHM, Nyman BFL. Felaktig organisation grund till tragedin inom äldrevården [Internet] Läkartidningen. 2020 https://lakartidningen.se/opinion/debatt/2020/05/felaktig-organisation-grund-till-tragedin-inom-aldrevarden/ [cited 2020 May 28]. Available from: [Google Scholar]
- 66.Smith GD, Spiegelhalter D. Shielding from COVID-19 should be stratified by risk. BMJ. 2020 May 28 doi: 10.1136/bmj.m2063. m2063. [DOI] [PubMed] [Google Scholar]
- 67.Irwin RE. Misinformation and de-contextualization: international media reporting on Sweden and COVID-19. Glob. Health. 2020 Jul 13;16(1):62. doi: 10.1186/s12992-020-00588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ludvigsson JF. Children are unlikely to be the main drivers of the COVID-19 pandemic - a systematic review. Acta Paediatr Oslo Nor. 1992 doi: 10.1111/apa.15371. 2020 May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.COVID-19 in children and the role of school settings in COVID-19 transmission [Internet]. [cited 2020 Aug 16]. Available from:https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf
- 70.Andresen ME.Hva koster det å stenge utdanningssektoren? Beregning av kostnader av smittevernstiltak mot COVID-19 for humankapital, studieprogresjon og produktivitet.:26.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.