Abstract
Purpose
The current scenario of the COVID-19 pandemic has forced dentists to prepare themselves by updating their knowledge and receive training to face the present and after effects of COVID-19. The present survey was thus conducted to assess the knowledge, risk perception, attitude, and preparedness of the dentists in India about COVID-19.
Materials and Methods
A cross-sectional online survey was carried out among registered dentists in India. A self-administered, anonymous, questionnaire comprising of 25 close-ended questions was circulated to gather the relevant information. A total of 765 dentists submitted a response, out of which 646 complete responses were included in the statistical analysis. Pearson’s Chi-square test was used for inter-group statistical comparison.
Results
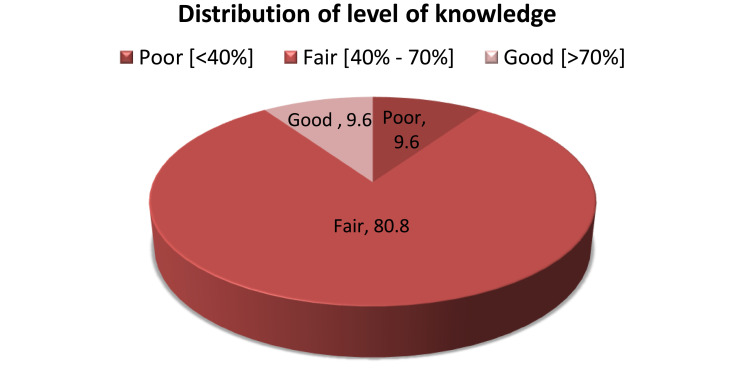
The majority (80.8%) of the dentists had a fair knowledge about the characteristics of COVID-19. Nearly 60.7% and 49.7% of the dentists had taken infection control training and special training for COVID-19, respectively. Nearly 50% of the dentists had the perception that COVID-19 is very dangerous. Only 41.8% of the dentists were willing to provide emergency services to patients. Most of the dentists had an opinion that there is a need to enhance personal protective measures. During the survey, it was found that varied technological advances are offered to dentists to ensure good clinical practice. They also concurred that there was a need to standardize the tools and measures available to carry out dental practices.
Conclusion
In the present study, Indian dentists have presented satisfactory knowledge with adequate preparedness as the majority of them had a fair level of knowledge with significantly higher knowledge among female respondents and those with post-graduation studies. Dentists should make judicious utilization of all the precautionary measures to safely practice dentistry. As we are going through an evolutionary phase where new advances are expected to evolve, dentists will definitely emerge successfully out from the crisis of the COVID-19 pandemic.
Keywords: corona virus, healthcare workers, dentistry, Asian, awareness
Introduction
In Wuhan city in the People's Republic of China, on December 30, 2019, multiple cases of pneumonia of unknown etiology were identified. WHO named it as COVID-19 and declared it as a public health emergency of international concern because of it’s highly infectious nature.1 COVID-19 is caused due to SARS-CoV-2 virus which is a single-stranded RNA with protein spike, envelope membrane, and nucleic capsid.2 In most of the cases, the average incubation period is of 4–14 days.3 The clinical symptoms are varied and manifest as fever, nasal congestion, headache, cough, sore throat, shortness of breath, nausea, vomiting, and diarrhea.4 COVID-19 is spread among humans through all kinds of droplet infection including through sneezing and coughing.5
COVID-19 has so far affected a large number of health professionals around the world.6 Since the dentist works in close proximity to body fluids such as saliva and blood in the oral cavity; they are at a high risk to get infected.7 The emergence of COVID-19 made us realize that even though we have been working in the field of dentistry and handling clinical cases with HIV, hepatitis, tuberculosis, and other infectious diseases, we were never prepared for a pandemic with such a high impact on community health.
Severe acute respiratory syndrome (SARS) in 2003 reported that no dental health worker or a patient had contracted the virus in a dental setting. It was unlikely that patients with SARS could visit a dental clinic in the acute phase because of high fever. The applications of universal precautionary measures were found to be adequate for infection control.8 However, COVID-19 is highly infectious as it is even spreading through asymptomatic contact. The presence of virus in saliva (91.7% of patients) makes the dentist extremely vulnerable to contract the disease.9
Dentists work in an environment of aerosol and splatter. The airborne material can spread at a distance of eighteen-inches from the operator site.10 To protect the dental community, the American Dental Association has issued guidelines to suspend elective or planned dental treatment and carry out only emergency procedures.11 To have minimal or no contact with patients, telemedicine or telephonic communication is being advised.12 Dentists are in a state of psychological distress and fear while working in such an unprecedented situation.13,14 Dentists, among various health professionals, fall at the highest risk of contracting an infection.15 Dentistry is undergoing a phase where there is a need to enhance and improvise the way of practice. This survey was conducted to assess the awareness and knowledge about COVID-19 among dental professionals. The present survey also assessed the preparedness of dental professionals towards managing and treating patients in the present crisis.
Materials and Methods
This prospective, cross-sectional study was carried out from June 1, 2020 to June 8, 2020. This study was conducted among dentists in India, including those doing post-graduation studies, general and specialist dentists working in government, private and other health sectors. A self-explanatory, online questionnaire comprised of 25 closed-ended questions was prepared using Google forms to assess knowledge, attitude, and preparedness of COVID-19 among Indian dentists.
The questionnaire was designed in the English language and was categorized into four parts: 1) demographics and general characteristics (8 items) of the participants; 2) knowledge (10 items) of the participants about COVID-19; 3) Risk perception and attitude (10 items) of the participants about COVID-19; and 4) Preparedness (5 items) of the participants against COVID-19. A pilot study was performed on 30 randomly selected dentists before starting the collection of actual data figures. The pilot samples were not included in the final sample size. The main purpose of the pilot survey was to ensure the validity and reliability of the questionnaire; to find out any hurdle while collecting the data; to evaluate time duration required in filling the form and obtaining suggestions from the participants to overcome the obstacles. The face and content validity of the questionnaire was thoroughly assessed and evaluated for readability, clarity and comprehensiveness of the questions by the subject and research experts. The questionnaire was modified according to the reviewer comments before the final approval. Cronbach’s alpha test was used to assess the reliability of the questionnaire. Cronbach’s alpha value for knowledge segment and attitude segment were 0.853 and 0.812, respectively, which indicated that the questionnaire was well-structured and suitable for the selected population. Knowledge score was calculated by awarding “1” point for each positive/correct response and “0” points for each negative/wrong response. The final scores were presented in the form of percentage by adding all the points of the respondents followed by calculating the percentage. The calculated knowledge score was divided into three categories based on percentage: poor knowledge (0–40%), fair knowledge (41<70%) and good knowledge (70% and above).16
The study proposal was addressed to the Institutional Ethics Committee (IEC) and ethical clearance (2020–3645) was obtained. The link of the questionnaire along with a consent form was forwarded to the contacts of the researchers using e-mails and various social media platforms. From all over India, 765 dentists were randomly selected for voluntary participation. The confidentiality of information was preserved during the process by keeping it anonymous and requesting the participants for honest answers. Data was collected in an organized manner from dentists working in various health sectors across different states in India.
The data on categorical variables are shown as n (% of respondents - prevalence) and the data on continuous variables is presented as mean and standard deviation (SD). The inter-group statistical comparison of the distribution of categorical variables was tested using Pearson’s Chi-square test. In the entire study, P-values less than 0.05 were considered to be statistically significant. The entire data was statistically analyzed using Statistical Package for Social Sciences (SPSS ver 22.0, IBM Corporation, USA) for MS Windows.
Results
Distribution of Demographic Parameters
A total of 765 respondents submitted the form, out of which 646 (84.4%) complete responses were included for the statistical analysis. Of the 646 respondents, 350 (54.2%) were male and 296 (45.8%) were female. The majority of the respondents, 303 (46.9%) had an age range of 30–39 years. While considering the duration of practice, only 100 (15.5%) had recorded experience of above 15 years. Most of the dentists (345, 53.4%) belonged to the west zone followed by north and central zone. The majority (378, 58.5%) of the respondents were from the private sector, 123 (19%) from the public sector and 145 (22.4%) were from university clinics. Most of the participants in the study held a BDS degree and a substantial amount held a MDS degree, with a distribution of 285 (44.1%) and 272 (42.1%) respectively (Table 1).
Table 1.
Distribution of Demographic Parameters of the Respondents Participating in the Study
| Parameter | Distribution of Respondents’ n (%) |
|---|---|
| Age group | |
| <30 years | 230 (35.6%) |
| 30–39 years | 303 (46.9%) |
| 40–49 years | 80 (12.4%) |
| >50 years | 33 (5.1%) |
| Gender | |
| Male | 350 (54.2%) |
| Female | 296 (45.8) |
| Duration of practice | |
| <5 years | 269 (41.6%) |
| 5–15 years | 277 (42.9%) |
| >15 years | 100 (15.5%) |
| Zone of practice | |
| Central | 98 (15.2%) |
| East | 48 (7.4%) |
| West | 345 (53.4%) |
| North | 103 (15.9%) |
| South | 52 (8.1%) |
| Organization | |
| Private sector | 378 (58.5%) |
| Public sector | 123 (19.0%) |
| University Clinics | 145 (22.4%) |
| Educational status | |
| BDS | 285 (44.1%) |
| MDS | 272 (42.1%) |
| Post-graduate students | 76 (11.7%) |
| Doctoral (PhD) | 13 (2.0%) |
| Training taken (Infection control) | |
| Yes | 392 (60.7%) |
| No | 254 (39.3%) |
| Training taken (COVID-19) | |
| Yes | 321 (49.7%) |
| No | 325 (50.3%) |
When the respondents were asked about their previous training or courses of infection control, out of 646 respondents, 392 (60.7%) revealed that they had previous training on infection control. Similarly, 321 (49.7%) respondents stated that they had training or informative lectures on COVID-19.
Distribution of Level of Knowledge
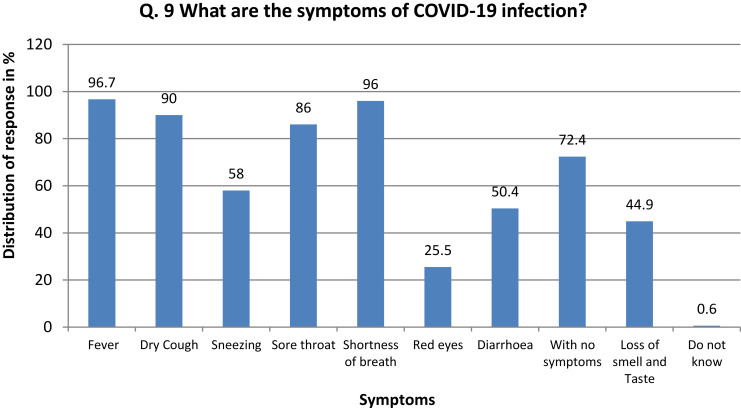
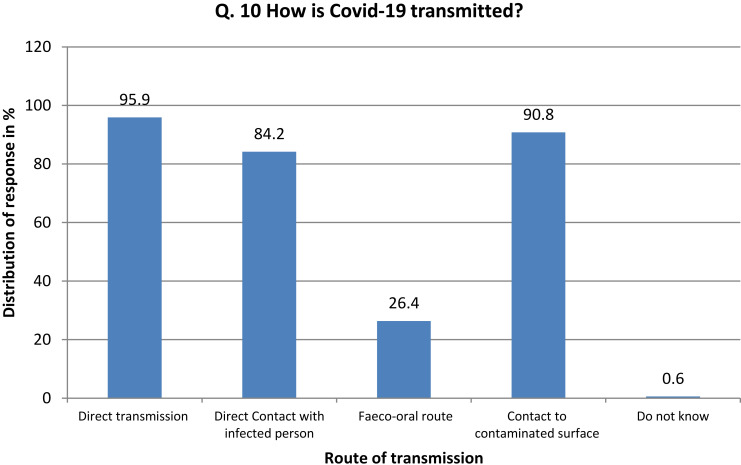
Table 2 represents the distribution of the number and frequency of respondents who had selected the correct answer related to knowledge and awareness (Figures 1 and 2). Distribution of overall knowledge among the 646 respondents in the study showed that 62 (9.6%) had a poor level of knowledge, 522 (80.8%) had a fair level of knowledge and 62 (9.6%) had a good level of knowledge (Figure 3).
Table 2.
Distribution of Level of Knowledge Recorded by Respondents According to Questions
| No. | Question | Correct Answer Respondents [n (%)] |
|---|---|---|
| 1. | Among these which is Coronavirus? a) Common cold, b) Middle East Respiratory Syndrome (MERS), c) Severe Acute Respiratory Syndrome (SARS), d) COVID-19, e) All, f) Do not know |
e) All 292 (45.20%) |
| 2. | Which is more deadly (High mortality)? a) SARS, b) MERS, c) COVID-19, d) Do not know |
b) MERS 65 (10%) |
| 3. | Which is more infectious? a) SARS, b) MERS, c) COVID-19, d) Do not know |
c) COVID-19 544 (84.2%) |
| 4. | COVID-19 is caused by virus a) SARS-CoV-2, b) SARS-CoV, c) MERS-CoV, d) Do not know |
a) SARS-CoV-2 546 (84.5%) |
| 5. | What is the incubation period of COVID-19 virus? a) 2–7 days, b) 2–14 days, c) 1–5 days, d) 1–21 days, e) Do not know |
b) 2–14 days 587 (90.8%) |
| 6. | What is the overall mortality rate of COVID-19 disease? a) 3.2%, b) 6.8%, c) 10.4%, d) 12.6%, e) Do not know |
b) 6.8% 78 (12%) |
| 7. | What is the basic reproduction number (R0-R naught) for COVID-19? a) 2.2, b) 5.3, c) 1.6, d) 4.2, e) Do not know |
a) 2.2 69 (10.6%) |
| 8. | What is the laboratory test available to diagnose COVID-19? a) rRT-PCR, b) ELISA, c) Western Blot, d) DNA hybridization, e) Do not now |
a) rRT-PCR 525 (81.2%) |
Figure 1.
Response of the participants in relation to Q.9.
Figure 2.
Response of the participants in relation to Q.10.
Figure 3.
Distribution of level of knowledge among the respondents participated in the study.
Distribution of level of knowledge did not differ significantly across the various age groups and the various groups based on the duration of practice (P-value >0.05). Distribution of level of knowledge (fair or good) was significantly higher among the female compared to male respondents (P-value <0.05) (Table 3). Distribution of level of knowledge (fair or good) differs significantly between various zones of practice with highest among the south zone compared to the rest of the zones (P-value <0.05) (Table 3).
Table 3.
Distribution of Level of Knowledge According to Various Demographic Characteristics of Respondents who Participated in the Study
| Characteristics | Level of Knowledge | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Poor (n=62) | Fair (n=522) | Good (n=62) | Total (n=646) | P-value | |||||
| n | % | n | % | n | % | n | % | ||
| Age group | |||||||||
| <30 years | 18 | 7.8 | 193 | 83.9 | 19 | 8.3 | 230 | 100.0 | |
| 30–39 years | 34 | 11.2 | 233 | 76.9 | 36 | 11.9 | 303 | 100.0 | 0.348NS |
| 40–49 years | 7 | 8.8 | 67 | 83.8 | 6 | 7.5 | 80 | 100.0 | |
| >50 years | 3 | 9.1 | 29 | 87.9 | 1 | 3.0 | 33 | 100.0 | |
| Gender | |||||||||
| Male | 45 | 12.9 | 267 | 76.3 | 38 | 10.9 | 350 | 100.0 | 0.003** |
| Female | 17 | 5.7 | 255 | 86.1 | 24 | 8.1 | 296 | 100.0 | |
| Duration of practice | |||||||||
| <5 years | 23 | 8.6 | 225 | 83.6 | 21 | 7.8 | 269 | 100.0 | |
| 5–15 years | 29 | 10.5 | 219 | 79.1 | 29 | 10.5 | 277 | 100.0 | 0.603NS |
| >15 years | 10 | 10.0 | 78 | 78.0 | 12 | 12.0 | 100 | 100.0 | |
| Zone of practice | |||||||||
| Central | 2 | 2.0 | 84 | 85.7 | 12 | 12.2 | 98 | 100.0 | |
| East | 5 | 10.4 | 41 | 85.4 | 2 | 4.2 | 48 | 100.0 | |
| West | 37 | 10.7 | 278 | 80.6 | 30 | 8.7 | 345 | 100.0 | 0.001*** |
| North | 14 | 13.6 | 84 | 81.6 | 5 | 4.9 | 103 | 100.0 | |
| South | 4 | 7.7 | 35 | 67.3 | 13 | 25.0 | 52 | 100.0 | |
| Organization | |||||||||
| Private sector | 39 | 10.3 | 314 | 83.1 | 25 | 6.6 | 378 | 100.0 | |
| Public sector | 10 | 9.3 | 86 | 72.2 | 27 | 18.5 | 123 | 100.0 | 0.001*** |
| University Clinics | 13 | 9.0 | 122 | 84.1 | 10 | 6.9 | 145 | 100.0 | |
| Educational status | |||||||||
| BDS | 29 | 10.2 | 242 | 84.9 | 14 | 4.9 | 285 | 100.0 | |
| MDS | 0 | 0.0 | 67 | 88.2 | 9 | 11.8 | 76 | 100.0 | 0.001*** |
| Post-graduate students | 32 | 11.8 | 202 | 74.3 | 38 | 14.0 | 272 | 100.0 | |
| PhD | 1 | 7.7 | 11 | 84.6 | 1 | 7.7 | 13 | 100.0 | |
| Training taken (Infection control) | |||||||||
| Yes | 2 | 6.1 | 323 | 82.4 | 45 | 11.5 | 392 | 100.0 | 0.001*** |
| No | 38 | 15.0 | 199 | 78.3 | 17 | 6.7 | 254 | 100.0 | |
| Training taken (COVID-19) | |||||||||
| Yes | 18 | 5.6 | 268 | 83.5 | 35 | 10.9 | 321 | 100.0 | 0.002** |
| No | 44 | 13.5 | 254 | 78.2 | 27 | 8.3 | 325 | 100.0 | |
Notes: P-value for Chi-square test. P-value <0.05 is considered to be statistically significant. **P-value <0.01, ***P-value<0.001, NS-statistically non-significant. Higher mean score indicates higher level of knowledge and vice-versa.
Distribution of the level of knowledge was significantly higher among the group of respondents with a post-graduation degree compared to respondents having only a graduation degree (P-value <0.05). A significantly higher level of knowledge was reported among respondents who had training of infection control compared to those who did not attend any such program in the recent past (P-value <0.05). However, a significantly higher level of knowledge was recorded among respondents who had training or informative lectures on COVID-19 (P-value<0.05) (Table 3).
Distribution of Risk Perception and Attitude
In the present survey, half (n=329) of the total numbers of respondents had the perception that COVID-19 is highly contagious followed by 301 (46.6%) respondents who believed it to be moderately contagious. Of the total respondents, 319 (49.4%) were aware of the fact that 80% of COVID-19-positive patients present with mild symptoms. The majority of the respondents (562, 87%) believed that dentists fall in the very high risk exposure category (Table 4).
Table 4.
Distribution of Risk Perception and Attitude of the Respondents who Participated in the Study
| Risk Perception | Response | n | % | |
|---|---|---|---|---|
| Perception about COVID-19 | Highly contagious | 329 | 50.9 | |
| Moderately contagious | 301 | 46.6 | ||
| Non contagious | 16 | 2.5 | ||
| % COVID-19 +ve patients shows mild symptoms | 80% | 319 | 49.4 | |
| 60% | 165 | 25.5 | ||
| 40% | 98 | 15.2 | ||
| Do not know | 64 | 9.9 | ||
| Under which category do dentists fall in the risk of exposure? | Very high exposure risk job | 562 | 87.0 | |
| High exposure risk job | 80 | 12.4 | ||
| Low exposure risk job | 4 | 0.6 | ||
| Which mask should generally be used by dentists? | A1 | 323 | 50.0 | |
| A1 + A2 | 133 | 20.6 | ||
| A2 | 92 | 14.2 | ||
| A1+A2=A3 | 34 | 5.3 | ||
| A1 +A3 | 24 | 3.7 | ||
| Other | 36 | 5.6 | ||
| Do not know | 4 | 0.6 | ||
| Which of the following needs to be checked before wearing N95? | B1 | 231 | 35.8 | |
| B1+B2+B3 | 178 | 27.6 | ||
| B1+B2 | 104 | 16.1 | ||
| B2 | 37 | 5.7 | ||
| B1+B3 | 29 | 4.5 | ||
| Other non-relevant combination | 26 | 4.0 | ||
| Do not know | 41 | 6.3 | ||
| What would you do for a dental problem of a confirmed/suspect COVID-19 patient? | C1 | 299 | 46.3 | |
| C1+C2 | 199 | 30.8 | ||
| C2 | 143 | 22.1 | ||
| C3 | 5 | 0.8 | ||
| What dental procedures carry the maximum risk of virus transmission while treating a COVID-19-positive patient? | D1+D2 | 476 | 73.7 | |
| D2 | 32 | 5.0 | ||
| D1+D2+D3 | 57 | 8.8 | ||
| D1+D2+D4 | 26 | 4.0 | ||
| D1 | 20 | 3.1 | ||
| D1+D2+D5 | 25 | 3.9 | ||
| Other non-relevant combination | 8 | 1.2 | ||
| Do not know | 2 | 0.3 | ||
| Are the personal protective equipments useful in protecting from confirmed/suspected COVID-19 patients? | Agree | 508 | 78.6 | |
| Disagree | 76 | 11.8 | ||
| Do not know | 62 | 9.6 | ||
| Will you provide emergency dental treatment to a COVID-19-positive patient? | Yes | 270 | 41.8 | |
| No | 264 | 40.9 | ||
| Do not know | 112 | 17.3 | ||
| Will you provide dental treatment to a previous COVID-19-positive patient? | Yes | 536 | 83.0 | |
| No | 81 | 12.4 | ||
| Do not Know | 29 | 4.6 | ||
| Key elaboration for Table 4 | ||||
| A1 | Surgical N95 (Medical respirator) | B1 | Fit test for proper seal | |
| A2 | Standard N95 (Unvalved) | B2 | User should have prior training | |
| A3 | Surgical Mask | B3 | Certain medical condition | |
| C1 | Use teleconference and if the dental treatment can be delayed give advice about pharmaceuticals | D1 | Ultrasonic scaling | |
| D2 | Use of high speed headpiece | |||
| C2 | Refer the patient directly to the higher center | D3 | Dental procedures under rubber dam | |
| C3 | Examine the patient directly in your dental office to check the severity of the dental condition | D4 | Crown cementation | |
| D5 | Use of lasers | |||
In response to the question “Which mask should generally be used by Dentists?” almost 50% (n=323) of the respondents selected Surgical N95 (Medical respirator) as an option, followed by 133 (20.6%) respondents who opted for a combination of Surgical N95 (Medical respirator) and Standard N95 (Unvalved) as protective gear. Whereas, 91 (14.2%) respondents believed that only Standard N95 (Unvalved) should be used during the dental procedure. The next question was in relation to the basic requirements to be checked before wearing the N95 mask. Of the total 646 respondents, 231 (35.8%) believed that only the fit test for proper seal should be checked before use, whereas 178 (27.6%) respondents selected all three options (fit test for a proper seal, plus user should have prior training and certain medical condition) (Table 4).
About 299 (46.3%) respondents decided to use teleconferences to see if the dental treatment could be delayed by prescribing medications to solve the dental problem of a confirmed/suspect COVID-19 patient, followed by 143 (22.1%) respondents who selected that they will refer the patient directly to the higher center (Hospital setup). Very few respondents 5 (0.8%) had an opinion that they will examine the patient directly in their dental office to check the severity of the complaint. Most of the respondents (476, 737%) were aware of the fact that ultrasonic scaling and use of high-speed headpiece carries the maximum risk of virus transmission while treating a COVID-19-positive patient (Table 4).
Most of the respondents (508, 78.6%) recorded their agreement when asked that “Are personal protective equipment useful in protecting from confirmed/suspected COVID-19 patients? Very few respondents (76, 11.8%) recorded disagreement with the above statement. Of the 646 respondents, 270 (41.8%) recorded a positive attitude towards providing emergency dental treatment to COVID-19-positive patients, whereas 264 (20.9%) refrained from providing emergency dental treatment. Most of the respondents (536, 83%) showed a positive attitude towards providing dental treatment for the previous COVID-19-positive patients (Table 4).
Distribution of Preparedness
Distribution of Level of Preparedness According to Training Taken (Infection Control)
Distribution of level of preparedness in terms of training to be provided to the staff, precautions to be taken during treatment and preparation of the body to prevent COVID-19 did not differ significantly among respondents with and without training of infection control (P-value >0.05). However, distribution of level of preparedness in terms of contacting the appropriate organization if they had an unprotected exposure to a known or suspected COVID-19 patient and if having signs or symptoms of COVID-19 infection differed significantly between the groups (P-value <0.05) (Table 5).
Table 5.
Distribution of Level of Preparedness According to Training Taken (Infection Control/COVID-19) Among the Respondents who Participated in the Study
| Training Taken (Infection Control) | Training Taken (COVID-19) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No (n=254) | Yes (n=392) | P-value | No (n=325) | Yes (n=321) | P-value | ||||||
| Level of Preparedness | Response | n | % | n | % | n | % | n | % | ||
| Dentist should provide adequate training to their staff to promote many levels of screening and preventive measures. | Agree | 248 | 97.6 | 390 | 99.5 | 0.081NS | 315 | 97.0 | 321 | 100 | 0.018* |
| Disagree | 2 | 0.8 | 0 | 0.0 | 3 | 1.0 | 0 | 0.0 | |||
| Do not know | 4 | 1.6 | 2 | 0.5 | 7 | 2.0 | 0 | 0.0 | |||
| What precautions should the dental practitioners take when treating COVID-19-positive patients? | E1 | 190 | 74.8 | 307 | 78.3 | 0.070NS | 230 | 71.2 | 260 | 79.7 | 0.026* |
| E2 | 15 | 5.9 | 18 | 4.6 | 24 | 7.4 | 8 | 2.4 | |||
| E3 | 14 | 5.5 | 6 | 1.5 | 15 | 2.8 | 9 | 2.8 | |||
| E4 | 17 | 6.7 | 24 | 6.1 | 22 | 6.8 | 15 | 5.3 | |||
| E5 | 6 | 2.4 | 9 | 2.3 | 16 | 1.8 | 9 | 2.8 | |||
| E6 | 12 | 4.7 | 28 | 7.1 | 18 | 5.5 | 19 | 6.2 | |||
| How to prepare your body to prevent and avoid getting COVID-19 infection? | F1 | 191 | 75.2 | 306 | 78.1 | 0.242NS | 250 | 76.9 | 247 | 76.9 | 0.001*** |
| F2 | 28 | 11.0 | 39 | 9.9 | 36 | 11.1 | 31 | 9.7 | |||
| F3 | 14 | 5.5 | 27 | 6.9 | 17 | 5.2 | 24 | 7.5 | |||
| F4 | 11 | 4.3 | 5 | 1.3 | 14 | 4.3 | 2 | 0.6 | |||
| F5 | 4 | 1.6 | 7 | 1.8 | 0 | 0.0 | 11 | 3.4 | |||
| F6 | 6 | 2.4 | 8 | 2.0 | 8 | 2.8 | 6 | 1.9 | |||
| Do you know whom to contact if you have an unprotected exposure to a known or suspected COVID-19 patient? | Yes | 206 | 81.1 | 362 | 92.3 | 0.001*** | 270 | 83.1 | 298 | 92.8 | 0.001*** |
| No | 48 | 18.9 | 30 | 7.7 | 55 | 16.9 | 23 | 7.2 | |||
| Do you know what to do if you have signs or symptoms suspected of COVID-19 infection? | Yes | 234 | 92.1 | 387 | 98.7 | 0.001*** | 305 | 93.8 | 316 | 98.4 | 0.002** |
| No | 20 | 7.9 | 5 | 1.3 | 20 | 6.2 | 5 | 1.6 | |||
| Key elaboration for Table 5 | |||||||||||
| E1 | AIIRs should be reserved for patients, Air from these rooms should be exttacted directly by high-efficiency particulate air (HEPA) filter, Pre-procedural mouth rinse with 0.2% povidone-iodine, Extra-oral imaging should be preferred to intra-oral imaging | ||||||||||
| E2 | AIIRs should be reserved for patients, Air from these rooms should be extracted directly by high-efficiency particulate air (HEPA) filter, Pre-procedural mouth rinse with 0.2% povidone-iodine, Rubber dam should be used to minimize splatter generation | ||||||||||
| E3 | AIIRs should be reserved for patients, Air from these rooms should be exhausted directly by high-efficiency particulate air (HEPA) filter, Pre-procedural mouth rinse with 0.2% povidone-iodine, Extra-oral imaging should be preferred, Rubber dam should be used. Minimize the use of ultrasonic instruments, high-speed headpieces, and 3-way syringes. | ||||||||||
| E4 | AIIRs should be reserved for patients | ||||||||||
| E5 | AIIRs should be reserved for patients, Air from these rooms should be extracted directly by high-efficiency particulate air (HEPA) filter. | ||||||||||
| E6 | Other | ||||||||||
| F1 | Take proper rest and sleep, Daily intake of vitamin C in the form of citrus fruits, Drinking warm water and doing gargles with warm water mixed with povidone-iodine, salt etc, Exercise routinely to keep the body fit, Avoiding panic and psychological negative effects of the disease | ||||||||||
| F2 | Daily intake of vitamin C in the form of citrus fruits, Drinking warm water and doing gargles with warm water mixed with povidone-iodine, salt etc, Avoiding panic and psychological negative effects of the disease | ||||||||||
| F3 | Drinking warm water and doing gargles with warm water mixed with povidone-iodine, salt etc | ||||||||||
| F4 | Take proper rest and sleep, Drinking warm water and doing gargles with warm water mixed with povidone-iodine, salt etc, Exercise routinely to keep the body fit, Avoiding panic and psychological negative effects of the disease | ||||||||||
| F5 | Take proper rest and sleep | ||||||||||
| F6 | Other | ||||||||||
Notes: P-value for Chi-square test. P-value <0.05 is considered to be statistically significant. *P-value <0.05, **P-value <0.01, ***P-value <0.001, NS-statistically non-significant. Higher mean score indicates higher level of knowledge and vice-versa.
Abbreviation: AIIRs, airborne infection isolation rooms
Distribution of Level of Preparedness According to Training Taken (COVID-19)
A significantly higher level of preparedness in all aspects was recorded among respondents in the group who received training about COVID-19 compared to the group who never had training related to the COVID-19 infection.
Discussion
COVID-19 has emerged as a major healthcare concern around the world. Presently in India, private and public dental clinics are attending only emergency cases. However, practicing dentistry during such a pandemic is a first time experience for most dentists. The possible transmission routes in the dental clinic include direct contact by face-to-face communication, exposure to saliva, blood and other body fluids. Indirect contact can be due to contaminated instruments and the clinic environment.17 Considering the highly infectious nature of COVID-19, adequate training is required to carry out safe practice to prevent the spread to the working staff. These measures include wearing PPE, sterilized gloves, and respirators.18 The regulatory bodies are providing online training for diseases and their precautionary measures.19 The present survey was therefore undertaken among dentists in India to assess the knowledge and preparedness about COVID-19.
The majority (80.8%) of the respondents had a fair level (40–70%) of knowledge, which was significantly more among female respondents and those with post-graduation studies. This percentage is less when compared to the study conducted by Kamate et al19 in which 92.7% had a fair level of knowledge which could be due to the fact that it was a multinational study including developed countries like America and Australia.19 However this was in contrast to a study by Putrino et al20 in which males were more aware of the disease as compared to female participants.20 It was similar to a study by Quadri et al21 in which specialists had higher knowledge compared to auxiliaries and interns.21 Distribution of level of knowledge did not differ significantly across various age groups and duration of practice but was highest among those in the south zone. Most of the respondents were familiar with the wide variety of the symptoms that the patient can present at the clinic which is of utmost importance for the early diagnosis of the suspected positive patients. On the other hand, the asymptomatic carriers can pose the real problem as they have no or very mild symptoms which can be overlapping with other viral infections like common cold and flu. This requires that the dentists should consider each patient in the clinic to be a COVID-19 positive and take all the necessary precautions as such patients could sometimes be misjudged as normal patients (without COVID-19). Regarding the mode of transmission, nearly all respondents had a fair knowledge which means the dentist knows how to prevent the community spread of the current pandemic. This is very crucial especially to save the lives of the vulnerable patients who are more than 60 years old and suffering from pre-existing chronic illnesses. Regarding the level of training, the distribution of knowledge was significantly more among those having some training in infection control or those who had followed an informative lecture or training session on COVID-19. It also underlies the importance of keeping updated as the virus is continuously evolving and there might be changes in the protocols as more scientific evidence is gained.
Only 45% of the respondents knew about all the different types of coronavirus and only 10% knew that MERS has the highest mortality rate among all types of coronavirus. On a positive note 84.2% of them were conscious that COVID-19 is more infectious than the others which states the inquisitiveness that has been created by the new virus. Despite this, 84.5% of the respondents knew that COVID-19 is caused by SARS-CoV-2 but only 6.6% had an idea about the basic reproduction number (R0-R naught) of the virus which is reported as 2.2. This number can be defined as the average number of secondary cases attributable to infection by an index case after that case is introduced into a susceptible population. This number might increase with more well-defined studies which means the infectivity of the virus might be more than what we currently think and all the healthcare professionals need to have the updated information. Similarly, 90.8% of respondents knew about the incubation period of the virus (2–14 days) yet only 12% perceived the overall mortality rate by it. This may be partly due to the previous studies which stated a mortality rate of 3.4%.22,23 But according to the currently available data, the mortality rate is as high as 6.8%.24 A greater number (81.2%) of the participants agreed that the rRT-PCR laboratory test can help in the diagnosis of the suspected and asymptomatic cases. This real-time RT-PCR test works by the qualitative revelation of the nucleic acid of the SARS-CoV-2 in upper and lower respiratory specimens.25 Though a positive result is suggestive of progressive infection with SARS-CoV-2 but it does not rule out other bacterial and viral infections. Also, the negative results cannot rule out the absence of COVID-19, so proper decisions should be made following the patient’s symptoms, travel history, and geographical location.
Nearly 50% of the respondents perceived COVID-19 as very dangerous. This can be correlated to the fact that nearly the same number of participants feel that almost 80% of the patients can present with mild or no symptoms.4,26 Such patients pose the highest risk as these almost asymptomatic ones can not only act as carriers of infection to others but also can be the reservoirs of the disease causing reinfection unintentionally. This is in accordance with the study by De Stefani et al27 where the dentists recognized COVID-19 to be a highly dangerous viral infection.27 This made 87% of the dentists believe that their job falls under very high risk category of exposure. It is in accordance with a study by Cagetti et al28 where the majority of the respondents believe that the risk of infection transmission is high in the dental practice.28 Treating such patients can act like starting a chain reaction of spreading the infection to subsequent patients as the containment of the virus has not yet been fully understood.29 Nearly 85% of the dentists were well versed with the type of mask and were ready to use the N95 mask especially when dealing with COVID-19 patients. A surgical N95 respirator also called as a medical respirator is to be used by healthcare professionals that specifically need protection from airborne and fluid splashes. If there is a shortage of surgical N95 respirators then standard N95 respirators can be used with a face shield. For all other healthcare professionals, a standard N95 respirator can be used. Though most of the respondents agreed with wearing a N95 respirator, 35.8% felt that only a fit test should be done to check the seal and only 27.6% knew that they should be medically evaluated and properly trained to make sure that it feels comfortable donning the respirator and also know how to carry on a user seal check. This signifies the importance of the following the complete protocol when using N95 respirators.
Nearly all the dentists thought that it is not a good idea to examine the patient directly in the dental office as about 46.3% respondents agreed for teleconferencing with the patients and delaying any treatment if the problem can be resolved by advising medications. Additionally, 30.8% also felt that any patient requiring a visit to the dental office for treating the dental problem that cannot be managed with medications should be referred directly to better equipped higher centers which can facilitate such cases in a better way. The majority (73.7%) of the dentists were aware that the dental procedures involving the use of ultrasonic scalers and high-speed handpieces carry the maximum risk of transmission of the virus along with aerosol particles. The virus can sustain on inanimate surfaces for almost 3 days making rigorous disinfection protocol a must for every dental office.30 The majority (78.6%) of the dentists agreed that wearing personal protective equipment like gloves, mask and goggles can be effective in preventing transmission of COVID-19 which was in accordance with the study by Khader et al31 where 92.9% of respondents felt the same. Nearly 42% of the respondents were willing to provide emergency treatment to patients having COVID-19. It is in contrast to the study by Khader et al in which 82.6% of the dentists preferred to avoid treating a suspected COVID-19 patient as the majority of these patients will have no or mild symptoms during the incubation periods but can be very effective in transmitting the disease.31 There are some dental emergencies especially Orofacial fractures and space infections which require surgical intervention and cannot be treated alone by medications. Treating COVID-19 patients requires the dentist to follow and keep updated with the recent guidelines mentioned by the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) very precisely.32–35 On the contrary, 83% of the respondents of the current study were ready to treat the patients who had contracted the disease previously but are disease free now.
To evaluate the preparedness in the current study, most of the dentists agreed to provide adequate training to their staff. According to the recommendation by the Occupational Safety and Health Administration (OSHA), a dental professional should keep their staff up to date and educated consistently to keep a healthy and protected dental office. Most of the dentists in the current survey were aware of the precautionary measures to be taken while treating COVID-19 positive patients, irrespective of their training status. These results are in agreement with the results published in the study conducted by Ahmed et al.14 The pre-procedural rinsing should be done with 0.2% povidone-iodine or 0.5–1% hydrogen peroxide as an antimicrobial mouth rinse can reduce the load of virus in the oral cavity.17,36,37 Airborne Infection Isolation Rooms (AIIRs) should be reserved for patients.38 Air from these rooms should be extracted directly to the outside or be filtered through a high-efficiency particulate air (HEPA) filter. Often the disposable devices should be used and extra-oral imaging should be preferred to intra-oral imaging to avoid stimulation of saliva and cough. Rubber dam use should be maximized and the use of ultrasonic instruments, high-speed handpieces, and 3-way syringes should be reduced to avoid aerosol generation. Cleaning and disinfection of the surfaces should be done at least once daily first with regular soap or detergent and then with 0.1% sodium hypochlorite (ie, equivalent to 1000 ppm).
The majority of the respondents have recorded good awareness about the preparedness of the body to prevent getting COVID-19 infection. The obvious reason for this high level of awareness is the continuous circulation of messages from the health department and educational videos and posts on social media during the current pandemic. About 80–90% of the respondents were aware of whom to contact if they have unprotected exposure to a known or suspected COVID-19 patient. In the current study higher awareness level was recorded in the respondents who had past training about infection control and COVID-19. This finding was in contrast to the study conducted by Khader et al, which revealed that only half of the dentists (58.2%) were aware of whom to contact in such a situation.31 The Centers for Disease Control and Prevention (CDC) has divided the exposures into high risk, medium risk and low risk depending upon the type of contact with COVID-19 patients. Almost all the respondents who had past training about the infection control and COVID-19 were aware about their plan of action if they develop signs or symptoms suspected of COVID-19 infection. In contrast, 75.8% of Jordanian dentists reported that they knew what to do if they developed signs or symptoms of a suspected COVID-19 infection.31
Limitations
Despite implementing all the possible measures to reduce bias, the study was still prone to some limitations. The major limitation was short time duration for data collection assuming the rapid effect this pandemic is currently having on dental health professionals, which could have resulted in a smaller than expected sample. The data collection was done only on social media so it could have resulted in the exclusion of the practitioners who were not using social media or those who were busy taking care of personal affairs. Some states or regions across the country were more affected than others which may influence the administration and healthcare preventive measures implemented by a particular region that could also influence the result of a study. Therefore, the findings of the current survey should be interpreted cautiously and should not be generalized. Based on the available study design (cross-sectional) we are not in a position to conclude a cause-effect association.
Conclusion
In the present study, Indian dentists have revealed satisfactory knowledge about the COVID-19 etiology, symptoms, diagnosis and mode of transmission as the majority of them had a fair level of knowledge with significantly higher knowledge among female respondents and those with post-graduation studies. The respondents have recorded a good judgement about the risk perception as they know they fall in the very high risk exposure category and showed a positive attitude towards performing dental treatment in the current COVID-19 crisis. Despite having a satisfactory level of knowledge and risk perception, dental practitioners around the country were in a state of anxiety and stress about working in their respective fields. The dentists were also recommended to pursue the CDC and WHO guidelines in their clinics, so as to fight the pandemic in a more sophisticated way. Finally, all the dental professionals should attend the COVID-19 training program to improve their knowledge and to be well aware of the best practices and recommended approaches for infection control.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. The Research Ethic’s Committee, Indian Dental Association (Bathinda) approved the research with the approval number: 2020-3645
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Huang X, Wei F, Hu L, Wen L, Chen K. Epidemiology and clinical characteristics of COVID-19. Arch Iran Med. 2020;23(5):268–271. doi: 10.34172/aim.2020.09 [DOI] [PubMed] [Google Scholar]
- 2.Chen Y, Liu O, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Backer JA, Klinkenberf D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCov) infections among travellers from Wuhan, China. Eurosurveillance. 2020;25:20–28. doi: 10.2807/1560-7917.ES.2020.25.5.2000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Z, Liu S, Xianf M, et al. Protecting healthcare personnel from 2019-nCov infection risks: lessons and suggestions. Front Med. 2020;1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cleveland JL, Gray SK, Harte JA, et al. Transmission of blood borne pathogens in US dental health care settings. J Am Dent Assoc. 2016;147:729–738. doi: 10.1016/j.adaj.2016.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.To KK, Tsang OT, Chik-Yand Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;149:1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samaranayke LP, Peiris M. Severe acute respiratory syndrome and dentistry. A retrospective view. J Am Dent Assoc. 2004;135(9):1292–1302. doi: 10.14219/jada.archive.2004.0405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrel SK, Molinau J. Aerosols and splatter in dentistry: a brief review of literature and infection control implications. J Am Dent Assoc. 2004;135:429–437. doi: 10.14219/jada.archive.2004.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halepas S, Femini EM. A punch of prevention is a worth pound of cure. Proactive dentist in the wake of COVID-19. J Oral Maxillofac Surg. 2020;78(6):860–861. doi: 10.1016/j.joms.2020.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hau YS, Kim JK, Hur J, Chang MC. How about actively using telemedicine during the COVID-19 pandemic. J Med Syst. 2020;44(6):108. doi: 10.1007/s10916-020-01580-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shancham M, Raz H, Kolerman R, Mijiritsky O, Ben-Ezra M, Mijiritsky E. COVID 19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int J Environ Res Public Health. 2020;17(8):2900. doi: 10.3390/ijerph17082900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):17082821. doi: 10.3390/ijerph17082821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gamio L The worker who face the greatest corona risk. Available from: http://www.nytimes.com/interactive/2020. Accessed June1, 2020.
- 16.Al-Shawi MM, Darwish MA, Wahab A, Al-Shamlan NA. Misconceptions of parents about antibiotic use in upper respiratory tract infections: a survey in primary schools of the Eastern Province, KSA. J Fam Community Med. 2018;25:5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meng L, Hua F, Bia Z. Coronavirus disease 2019. COVID-19 Emerging future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamate S, Sharma S, Thakar S, et al. Assessing knowledge, attitudes and practices of dental practitioners regarding the COVID-19 pandemic: a multinational study. Dent Med Problem. 2020;57(1):11–17. doi: 10.17219/dmp/119743 [DOI] [PubMed] [Google Scholar]
- 20.Putrino A, Raso M, Magazzino C, et al. Coronavirus (COVID-19) in Italy: knowledge, management of patients and clinical experience of Italian dentists during the spread of contagion. BMC Oral Health. 2020;20(1):200. doi: 10.1186/s12903-020-01187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quadri MFA, Jafer MA, Alqahtani AS, et al. Novel corona virus disease (COVID-19) awareness among the dental interns, dental auxiliaries and dental specialists in Saudi Arabia: a nationwide study. J Infect Public Health. 2020;13(6):856–864. doi: 10.1016/j.jiph.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO director-general’s opening remarks at the media briefing on COVID-19-3 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-3-march-2020. Accessed June1, 2020.
- 24.Roser M, Ritchie H, Ortiz-Ospina E, et al. Mortality risk of COVID-19; 2020. Available from: https://ourworldindata.org/mortality-risk-covid. Accessed June1, 2020.
- 25.Tahamtan A, Ardebili A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev Mol Diagn. 2020;20(5):453‐454. doi: 10.1080/14737159.2020.1757437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Stefani A, Bruno G, Mutinelli S, Gracco A. COVID-19 outbreak perception in Italian dentists. Int J Environ Res Public Health. 2020;17:3867. doi: 10.3390/ijerph17113867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cagetti MG, Cairoli JL, Senna A, Campus G. COVID-19 outbreak in North Italy: an overview on dentistry. A questionnaire survey. Int J Environ Res Public Health. 2020;17(11):3835. doi: 10.3390/ijerph17113835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Occupational Safety and Health Administration’s Guidance on Preparing Workplaces for COVID-19. Available from: OSHA3990-03 2020. Accessed June1, 2020.
- 30.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khader Y, Al Nsour M, Al-Batayneh OB, et al. Dentists’ awareness, perception, and attitude regarding COVID-19 and infection control: A cross- sectional study among Jordanian dentists. JMIR Public Health Surveill. 2020;6(2):e18798. doi: 10.2196/18798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Infection control: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Available from: https://www.cdc.gov/coronavirus/2019-ncov/infection-control/controlrecommendations.html. Accessed June1, 2020.
- 33.Centers for Disease Control and Prevention. Dental settings: interim infection prevention and control guidance for dental settings during the COVID-19 response. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html. Accessed June1, 2020.
- 34.Centers for Disease Control and Prevention: interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html#take_precautions. Accessed June1, 2020.
- 35.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance; 2020a. Available from: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed June1, 2020.
- 36.Marui VC, Souto MLS, Rovai ES, Romito GA, Chambrone L, Pannuti CM. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: a systematic review. J Am Dent Assoc. 2019;150(12):1015–1026. doi: 10.1016/j.adaj.2019.06.024 [DOI] [PubMed] [Google Scholar]
- 37.Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther. 2018;7:249–259. doi: 10.1007/s40121-018-0200-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention: infection control basics, Transmission Based Precautions. Available from: https://www.cdc.gov/infectioncontrol/basics/transmission-basedprecautions.html#anchor_1564058235. Accessed June1, 2020.