Abstract
Background
Low socioeconomic status (SES) is linked to failure to quit smoking. Health inequity models suggest that low SES smokers experience barriers to quitting in part due to greater exposure to pro-smoking social contexts.
Purpose
The current study examined longitudinal associations among socioeconomic status, pro-smoking social context factors (i.e., exposure to other smokers, places where smoking was allowed), cigarette availability, and smoking lapse during a quit attempt.
Methods
Ecological momentary assessments (EMA) were gathered from a multiethnic sample of 365 smokers engaged in a quit attempt. A multilevel structural equation model estimated a latent variable for SES indicated by income, education, health insurance, and employment, associations among EMAs for pro-smoking social contexts and cigarette availability, and indirect effects of SES through, pro-smoking social contexts and cigarette availability to subsequent smoking lapse.
Results
Lower SES scores were associated with a higher likelihood of smoking lapse. Decomposition of the path from SES to smoking lapse into indirect effects showed significant paths through exposure to places where smoking is allowed and cigarette availability. Additionally, significant serial indirect paths from SES through both exposure to other smokers and places where smoking was allowed, in turn, through cigarette availability, and, ultimately, to smoking lapse were noted.
Conclusions
Consistent with models positing that SES influences health behaviors via contextual factors, the current study demonstrated that low SES smokers attempting to quit experienced greater pro-smoking social contexts that affected subsequent risk for lapse.
Keywords: Tobacco inequities, Smoking cessation, Ecological momentary assessment, Social contexts
Lower SES smokers experienced greater exposure to pro-smoking social environments in daily life and, as a result, were more likely to lapse during a quit attempt.
Introduction
Cigarette smoking is the leading cause of morbidity and mortality in the USA, accounting for 30% of all cancers and approximately 90% of lung cancer [1, 2]. Recent estimates place the annual economic burden of smoking in the USA at US$170 billion in healthcare costs with an additional US$150 billion in lost worker productivity [2, 3]. As rates of cigarette smoking have declined dramatically over the past half century among the general population, smoking has become increasingly concentrated in low socioeconomic status (SES) groups [4, 5] with healthcare costs attributed to smoking increasingly covered by public funds [3]. Research suggests that SES-related smoking inequities are widening and that reduced rates of smoking cessation among low SES groups are central to explaining this gap [6]. Although only 6% of smokers in the general population are able to successfully quit each year [7], cessation rates are even lower among low SES groups as typically defined by education and income [6, 8].
A critical factor that may be inhibiting low SES smokers from successfully quitting is their social context [6, 9]. Health behavior theories suggest that the smoking-specific features of social contexts may play an important role in this process among low SES smokers [10–12]. For example, low SES individuals are hypothesized to spend more time in locations that allow smoking and more time around other smokers [9, 13]. These pro-smoking social contexts may have a direct impact on smoking lapse by activating brain circuits that respond to cues for smoking [14]. Furthermore, greater time spent in pro-smoking social contexts may also increase access to cigarettes for a smoker who is trying to quit and, in turn, increase the risk of smoking lapse [15]. To date, there are few empirical studies on the associations among SES, smoking-specific features of social contexts, and smoking behavior [9, 13]. One reason for this dearth of research is the inherent challenge in measuring the dynamic nature of social contexts. In the course of a given day, individuals are likely to encounter multiple social contexts—some pro-smoking and some antismoking. A recent qualitative study among Australian smokers reported that lower SES individuals described more exposure to pro-smoking social contexts, whereas higher SES individuals reported more exposure to antismoking contexts [16].
Recent advances in mobile technology have allowed researchers to examine both social contexts and smoking behavior in near real time using ecological momentary assessment (EMA) data [17]. EMA studies generally gather data on participant perceptions and behaviors on multiple occasions over the course of a day for several weeks to produce highly detailed longitudinal data sets. Growing evidence has demonstrated that EMAs more accurately assess situational contexts and minimize recall biases and errors compared with standard survey instruments [17]. EMAs are particularly well-suited to examine the smoking-specific features of social contexts that are likely to change multiple times each day as individuals travel from home to work or other locations. To date, only one published study has utilized EMA data to examine SES-related differences in social contexts associated with cigarette smoking [13]. Jahnel and colleagues examined the impact of place-based smoking restrictions on smoking behavior over the course of 3 weeks among 194 daily and nondaily smokers. Results indicated that participants with lower education spent more time each day in locations where smoking was allowed and, in turn, smoked a greater number of cigarettes per day. The authors concluded that lower education was indirectly associated with smoking behavior through greater exposure to places where smoking was allowed. Interestingly, the authors did not find significant indirect effects when considering income alone as an indicator of SES [13]. Health behavior scholars have highlighted this potential for inconsistent findings across models employing single indicators of SES such as income and education [18]. As such, these scholars have urged researchers to consider multidimensional measures of SES that seek to account for both stable aspects of SES such as education and potentially variable aspects of SES such as annual income [18]. Although the work of Jahnel and colleagues highlights the influence of SES-related social context on daily smoking, participants in this study were not in the process of trying to quit. Building on this line of research to examine SES-related social contextual factors among smokers trying to quit could provide important information for smoking cessation programs and enhance efforts to reduce smoking-related health inequities among low SES populations.
The current study examined smoking-specific features of social contexts as factors linking SES to smoking lapse during a quit attempt [9, 11]. The current study expanded upon previous studies by considering the multidimensional nature of SES through use of a latent variable for SES indicated by income, educational attainment, health insurance status, and employment status [18], associations of SES with two interrelated dimensions of social context (i.e., exposure to other smokers and exposure to places where smoking is allowed), their association with cigarette availability and, in turn, the association of each of these factors with smoking lapse. To the best of our knowledge, no study to date has considered all of these elements using near real-time EMA data. Participants with lower SES scores were hypothesized to have an increased likelihood of subsequent lapse and to experience greater exposure to other smokers, places where smoking is allowed, and cigarette availability. Greater exposure to other smokers and places where smoking is allowed was hypothesized to increased cigarette availability, and all three were hypothesized to increase the likelihood of subsequent smoking lapse. Additionally, pro-smoking social contexts were hypothesized to increase the likelihood of smoking lapse indirectly through cigarette availability. Finally, lower SES scores were hypothesized to be indirectly associated with lapse through greater exposure to other smokers, places where smoking is allowed, and availability of cigarettes.
Methods
Participants
Data for the current study were drawn from a longitudinal cohort study designed to examine racial/ethnic differences in the processes of smoking cessation. Potential participants in the Houston, TX area were recruited from 2005 to 2007 via media advertisements to enroll in a smoking cessation study. Participants were required to be at least 21 years of age, have smoked an average of at least five cigarettes per day for the past year, have a home address and telephone number, demonstrate proficiency in English at a 6th grade level or higher, and be motivated to quit smoking in the next 30 days. Exclusion criteria included contraindication for a nicotine patch, use of tobacco products other than cigarettes, an active substance use disorder, use of nicotine replacement products other than the patch, participation in a cessation program in the past 90 days, or another household member enrolled currently in the study. The study was approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center.
Potential participants were screened over the phone to determine eligibility (N = 944). Those who met eligibility criteria (n = 837) were invited to in-person screening and orientation sessions where informed consent and baseline measures were collected. A total of 424 individuals met eligibility criteria and were enrolled in the study. Only participants with postquit EMAs were included in this study (n = 370). Five participants identifying as Asian American, Native American, or Pacific Islander were also excluded given insufficient group size to constitute a separate racial/ethnic category. Participants smoked an average of 21 cigarettes per day prior to the quit attempt. Additional sample details have been published elsewhere [19].
Smoking cessation treatment was based on the Treating Tobacco Use and Dependence Clinical Practice Guideline [20] and all participants received identical treatment. Beginning on quit day, participants were directed to use nicotine patch therapy for 6 weeks. Participants were also provided with six brief smoking cessation counseling sessions (five in-person sessions and one telephone session). Counseling sessions were conducted 1 week prior to quit day, on quit day, and at 1, 2, 3, and 4 weeks postquit) and completed five assessments during in-person visits. Participants received a US$30 gift card for each completed in-person assessment and were eligible to receive up to US$50 per week for EMA completion.
Measures
EMA data were collected via palmtop personal computer from 1 week prior to quit day to 28 days after quit day. During normal waking hours, participants were scheduled to receive four random EMA prompts per day. Waking hours were separated into 4 hr blocks, one EMA prompt was audibly and visually cued by the palmtop within each 4 hr block, and consecutive prompts were separated by at least 30 min. Over the 28 days of postquit monitoring, participants completed 31,800 random EMAs (77% of randomly issued prompts) for an average of 87 EMAs per person and approximately 3 EMAs per person per day. An additional 25,065 nonrandom, event-based EMAs were completed in the postquit period. Participants were instructed to self-initiate a nonrandom EMA when they experienced a smoking lapse or an urge to smoke. Data from nonrandom EMAs were used only to assess smoking lapses that occurred between two random EMAs. Measures of exposure to other smokers, places where smoking is allowed, and cigarette availability were drawn from random EMAs only to capture the most ecologically valid reports. The average interval between two completed random EMAs was 6 hr.
Smoking lapse was measured by both random and nonrandom EMAs. Participants were randomly asked to respond to a single item asking if they had smoked any cigarettes that they had not already recorded in the computer. If lapse was indicated, participants responded to an additional item “How long ago did you smoke the most recent cigarette that you did not record?” For nonrandom EMAs, participants responded to two items “How many cigarettes did you smoke during this slip?” and “How long ago did you smoke your last cigarette?” Random and nonrandom smoking lapse items assessed the time that a smoking lapse occurred with seven response options ranging from “0–15 minutes” to “8 hours or more.” Time of lapse was measured by midpoint of the response option interval (e.g., 0–15 min = 7.5 min) subtracted from the time of EMA. Lapse times of 8 hr or more were set to missing given that the specific time of lapse could not be identified. Intervals between two random EMAs that included one or more lapse were coded as 1. Intervals between two random EMAs that indicated no smoking lapse were coded as zero. Responses occurring simultaneously with a random EMA were coded as occurring in the prior interval.
Other smokers
At each random EMA, participants responded to one question if they were around other people. If yes, they were asked an additional question if any of those people were currently smoking a cigarette. Responses were coded such that 1 indicated exposure to another smoker and 0 indicated alone or around others who were not smoking.
Smoking allowed
At each random EMA, participants responded to single question regarding whether smoking was allowed in the current context. Response options from 1 to 3 indicated smoking was forbidden, smoking was discouraged, or smoking was allowed.
Cigarette availability
At each random EMA, participants rated if cigarettes were available to them at that moment on a 5-point scale from 1 = Not at all to 5 = Easily.
Socioeconomic status
At baseline, participants responded to four questions that were used to construct a multidimensional measure of SES. Annual family income was indicated by 11 categories ranging from less than US$10,000 to greater than US$100,000 broken into US$10,000 increments. The average income was approximately US$30,000 to US$39,999 (M = 3.8). Twenty eight per cent of participants reported an income of less than US$10,000, 24% reported US$10,000 to US$29,999, 19% reported US$30,000 to US$59,999 income, and 19% reported greater than US$60,000. Education was indicated by 1 = college degree and 0 = less than college degree. Health insurance status was indicated by 1 = privately insured and 0 = not privately insured. Employment status was indicated by 1= currently employed in regular full or part-time work and 0 = currently unemployed.
Demographics
At baseline, participants answered questions providing demographic data on age, gender, and race/ethnicity.
Analytic Approach
Researchers have noted the importance of disaggregating within person, momentary estimates and between person, and average estimates to better understand person-level processes in repeated measure data [21, 22]. Multilevel structural equation models (MSEMs) offer one method to disaggregate within- and between-person estimates derived from these types of data. In this approach, within-person measures are person mean–centered to allow for the examination of momentary deviations from average experiences during the study period. For example, within-person measures of exposure to other smokers, exposure to places where smoking was allowed, and cigarette availability were coded to reflect deviations from each participant’s average score on these measures during the quit attempt. The general advantages of MSEMs relative to other approaches have been described in detail elsewhere [23–25]. MSEMs were estimated with Mplus 8.1 [26] using the Bayes estimator and probit link to evaluate the effects of covariates on the continuous latent response underlying a binary measure of smoking lapse [27]. At the within-person level, the effect of person mean–centered measures of each covariate is evaluated in terms of the likelihood of smoking lapse in the subsequent moment; at the between-person level, the effect of average levels of each covariate is evaluated on the likelihood of smoking lapse at any given moment across the study period. MSEMs employing the Bayes estimator with noninformative priors often provide similar estimates to a maximum likelihood estimator, but offer two important advantages. The Bayesian approach (a) produces asymmetric credibility intervals (CI) and (b) reduces computational complexity of MSEMs that require many dimensions of numerical integration. The latter reduces convergence issues and substantially hastens model estimation. Models were estimated with a minimum of 20,000 iterations. To determine significance, the 95% highest probability density interval (HPD) was calculated from the posterior distribution of the model and CIs that did not include zero were considered statistically different from zero [27]. The Bayes estimator in Mplus is a full information estimator and handled missing data [26]. Data were missing for less than 1% of data points and missingness was largely a result of left censoring for prior interval smoking lapse at the start of the study period and subsequent interval smoking lapse information being unavailable at the end of the study period.
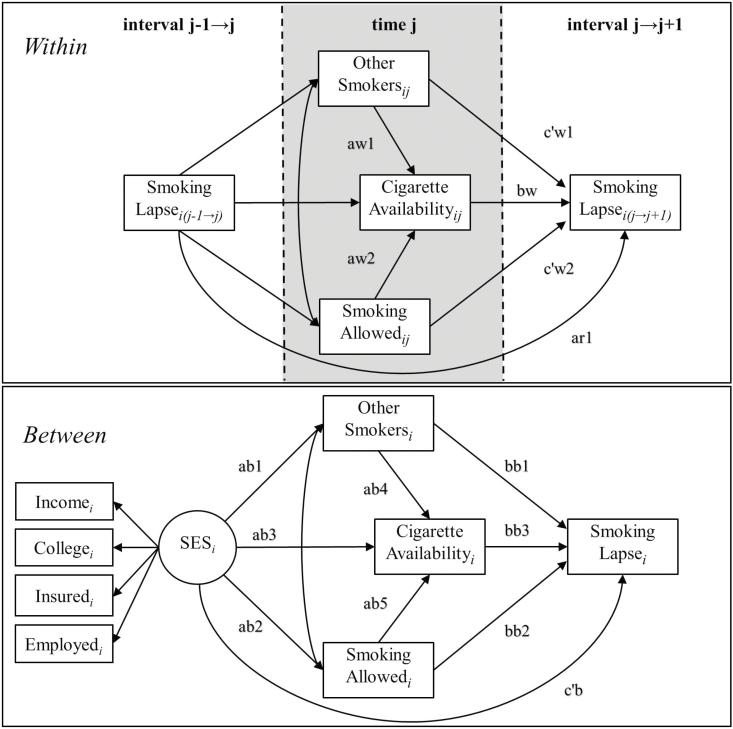
Figure 1 presents a graphic of the model for ease of interpretation. MSEMs, unlike standard regression approaches also allow for the shared variance among multiple interrelated variables to be summarized as a single latent variable. Health scholars have consistently recognized that typical indicators of SES such as income or education may fail to capture the multidimensional nature of SES [18]. Latent variables offer an established method of accounting for this multidimensional nature of SES by modeling the shared variance among income, education, insurance status, and employment status [26]. A preliminary structural equation model estimating a latent variable for SES (M = 0, SD = 1) that predicted smoking lapse after controlling for age, gender, and race/ethnicity was estimated at the between-person level only. Results showed that lower scores on the latent variable for SES were significantly associated with increased likelihood of lapse during the quit attempt (Est. = −.080, SD = .027, p = .003, 95% CI [−.133, −.028]) and confirmed adequate fit for the latent variable (χ 2 = 46.24, df = 17, p = .000; RMSEA = .007; CFI = .93). Indirect estimates presented in Table 3 represent the decomposition of this total effect of SES on lapse.
Fig. 1.
Multilevel structural equation model of socioeconomic status (SES), exposure to other smokers (OS), exposure to places where smoking is allowed (SA), cigarette availability (CA), and smoking lapse (SMK) across 28 days of a quit attempt. SES is represented as a latent variable. Subscript i indexes individuals (N = 365) and subscript j indexes ecological momentary assessments (N = 31,800).
Table 3.
Indirect estimates from a multilevel structural equation model of socioeconomic status (SES), exposure to other smokers (OS), exposure to places where smoking is allowed (SA), cigarette availability (CA), and smoking lapse (SMK)
| Indirect | (path) | Est. | SD | p a | [95% CI]b |
|---|---|---|---|---|---|
| Within | |||||
| OSij → CAij → SMKi(j → j+1) | (aw1 x bw) | .097 | .008 | .000 | [.083, .113]* |
| SAij → CAij → SMKi(j → j+1) | (aw2 x bw) | .104 | .005 | .000 | [.095, .115]* |
| Between | |||||
| SESi → OSi → SMKi | (ab1 x bb1) | .001 | .008 | .431 | [−.014, .016] |
| SESi → SAi → SMKi | (ab2 x bb2) | −.024 | .011 | .017 | [−.045, −.002]* |
| SESi → CAi → SMKi | (ab3 x bb3) | −.012 | .007 | .006 | [−.026, −.001]* |
| SESi → OSi→ CAi→ SMKi | (ab1 x ab4 x bb3) | −.008 | .004 | .000 | [−.016, −.001]* |
| SESi → SAi→ CAi→ SMKi | (ab2 x ab5 x bb3) | −.011 | .005 | .001 | [−.023, −.003]* |
i indexes participants (N = 365) and j indexes EMAs (N = 31,800); Est. = estimate; p = Bayesian one-tailed p-value; a = for positive values, the one-tailed p-value is the proportion of posterior distribution above 0; b = the 2.5 and 97.5 percentiles in the asymmetric posterior distribution, credibility intervals (CI) that do not include 0 noted with an asterisk (*).
The Model Constraint command was used to calculate indirect estimates at the within and between levels. Two serial indirect effects were computed for SES on smoking lapse through (a) exposure to other smokers and, in turn, cigarette availability and (b) exposure to places where smoking is allowed and, in turn, cigarette availability (see Fig. 1) [28]. To account for the possibility that participants who have recently lapsed had higher cigarette availability or had traveled to locations where other smokers were present and smoking was allowed, exposure to other smokers, exposure to places where smoking is allowed, and cigarette availability at time j was regressed on smoking lapse in the interval j → j − 1. All within-level paths controlled for the passage of time and the paths predicting smoking lapse controlled for the width of intervals. Between-level paths controlled for age, gender, and race/ethnicity. Additionally, we estimated the model presented in Fig. 1 with random slopes for all within-person paths of interest and computing indirect effects following procedures detailed by Preacher and colleagues [23, 24]. Results of this model were substantively identical to results from the fixed slopes model that are presented in Tables 2 and 3.
Table 2.
Within and between estimates from a multilevel structural equation model of socioeconomic status (SES), exposure to other smokers (OS), exposure to places where smoking is allowed (SA), cigarette availability (CA), and smoking lapse (SMK)
| Variables | (path) | Est. | SD | p a | [95% CI]b | ||
|---|---|---|---|---|---|---|---|
| Within | |||||||
| OSij | → | CAij | (aw1) | .244 | .017 | .000 | [.210, .277]* |
| SMKi(j → j + 1) | (c'w1) | .101 | .029 | .000 | [.039, .153]* | ||
| SAij | → | CAij | (aw2) | .264 | .010 | .000 | [.245, .283]* |
| SMKi(j → j+1) | (c'w2) | .087 | .017 | .000 | [.056, .118]* | ||
| CAij | → | SMKi(j → j+1) | (bw) | .396 | .013 | .000 | [.372, .423]* |
| SMKi(j-1 → j) | → | SMKi(j → j+1) | (ar1) | .344 | .019 | .000 | [.307, .375]* |
| OSij | .032 | .002 | .000 | [.028, .035]* | |||
| SAij | .102 | .005 | .000 | [.092, .110]* | |||
| CAij | .360 | .006 | .000 | [.350, .371]* | |||
| OSij | with | SAij | .040 | .001 | .000 | [.038, .042]* | |
| Between | |||||||
| SESi | → | OSi | (ab1) | −.027 | .006 | .000 | [−.039, −.015]* |
| SAi | (ab2) | −.046 | .017 | .001 | [−.084, −.016]* | ||
| CAi | (ab3) | −.085 | .039 | .017 | [−.155, −.007]* | ||
| SMKi | (c'b) | −.064 | .033 | .025 | [−.127, .001] | ||
| OSi | → | CAi | (ab4) | 1.126 | .353 | .000 | [.457, 1.849]* |
| SMKi | (bb1) | −.048 | .286 | .431 | [−.597, .514] | ||
| SAi | → | CAi | (ab5) | .900 | .122 | .000 | [.688, 1.160]* |
| SMKi | (bb2) | .267 | .107 | .005 | [.058, .460]* | ||
| CAi | → | SMKi | (bb3) | .287 | .043 | .000 | [.201, .370]* |
| OSi | with | SAi | .024 | .006 | .000 | [.012, .034]* | |
| Latent Variablec | |||||||
| SESi | → | Incomei | 1.000 | .000 | .000 | [1.000, 1.000] | |
| Collegei | .374 | .075 | .000 | [.233, .531]* | |||
| Insuredi | .817 | .314 | .000 | [.487, 1.552]* | |||
| Employedi | .466 | .085 | .000 | [.303, .641]* |
i indexes participants (N = 365) and j indexes EMAs (N = 31,800); Est. = undstandardized estimate (probit); SD = posterior standard deviation; p = Bayesian one-tailed p-value; a = for positive values, the one-tailed p-value is the proportion of posterior distribution above 0; b = the 2.5 and 97.5 percentiles in the asymmetric posterior distribution, credibility intervals (CI) that do not include 0 noted with an asterisk (*); c = continuous latent variable for SES (M = 0, SD = 1).
Results
Table 1 provides descriptive statistics and correlations. Participants were 42 years of age on average and 56% were female (N = 203). For race/ethnicity, 34% (n = 124) identified as White, non-Hispanic, 33% (n = 122) identified as African American/Black, non-Hispanic, and 33% (n = 119) identified as Hispanic/Latino. Among indicators of SES, participants averaged US$30,000 in annual income, 15% had achieved a college degree, 42% reported private health insurance, and 57% were currently employed.
Table 1.
Descriptive statistics and correlations for time-varying and time-fixed variables
| Variable | M (%) | SD | Min | Max | Correlations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||||
| Smoking lapse | 7.73% | – | 0 | 1 | 1 | – | .07* | .05* | .11* | ||||||
| Other smokers | 14.71% | – | 0 | 1 | 2 | .17* | – | .24* | .18* | ||||||
| Smoking allowed | 2.22 | .81 | 1 | 3 | 3 | .27* | .28* | – | .29* | ||||||
| Cigarette availability | 3.11 | 1.65 | 1 | 5 | 4 | .41* | .29* | .43* | – | ||||||
| Income | 3.83 | 2.85 | 1 | 11 | 5 | −.17* | −.24* | −.13* | −.23* | – | |||||
| College | 14.92% | – | 0 | 1 | 6 | −.18* | −.33* | −.11 | −.10 | .49* | – | ||||
| Health insurance | 41.16% | – | 0 | 1 | 7 | −.06 | −.22* | −.15* | −.16* | .66* | .49* | – | |||
| Employed | 57.34% | – | 0 | 1 | 8 | −.25* | −.16* | −.19 * |
−.14* | .46* | .30* | .65* | – | ||
| Age | 41.72 | 11.14 | 21 | 73 | 9 | .02 | .04 | .08 | −.03 | −.04 | .00 | .10 | −.26* | – | |
| Male | 44.38% | – | 0 | 1 | 10 | .00 | .02 | .06 | .03 | .21* | .04 | .07 | .25* | −.02 | – |
| African American | 33.42% | – | 0 | 1 | 11 | .09 | .15* | .18* | .05 | −.27* | −.12 | −.12 | −.20* | .32* | −.09 |
| Latino | 32.60% | – | 0 | 1 | 12 | −.02 | −.09 | −.11 | .05 | .13* | .00 | .09 | .31* | −.40* | .13 |
N = 365 for participants and N = 31,800 for EMAs; within-person correlations are shown above the diagonal and reflect person mean–centered estimates; between-person correlations are shown below the diagonal.
*p < .05.
Table 2 reports within- and between-person estimates from the MSEM. Table 3 reports within- and between-indirect estimates. Within-level estimates from the MSEM reported in Table 2 indicated that momentary increases in exposure to other smokers and exposure to places where smoking was allowed were associated with greater cigarette availability at time j. Increases in each of these factors were associated with a higher likelihood of smoking lapse in the interval j → j + 1 after controlling for smoking lapse in the interval j − 1 → j. Additionally, smoking lapse in the interval j − 1 → j was associated with momentary increases in exposure to other smokers, exposure to places where smoking is allowed, cigarette availability, and the likelihood of subsequent lapse. The within portion of the MSEM explained 36% of the variance in smoking lapse in the interval j → j + 1. Indirect estimates shown in Table 3 showed that both exposure to other smokers and exposure to places where smoking was allowed indirectly increased the likelihood of smoking lapse through increased cigarette availability.
At the between level, lower scores on the latent variable for SES were associated with greater exposure to other smokers, exposure to places where smoking is allowed, and cigarette availability (see Table 2). Exposure to other smokers and exposure to places where smoking was allowed were positively correlated with each other and higher levels on both were associated with greater cigarette availability. Greater exposure to places where smoking was allowed and cigarette availability were significantly associated with a higher likelihood of smoking lapse in the following interval at any given time across the study period. The between-level portion of the MSEM explained 29% of the variance in smoking lapse across the study period. Indirect effects reported in Table 3 indicated that SES was indirectly associated with smoking lapse through cigarette availability and exposure to places where smoking is allowed. Additionally, SES was significantly associated with lapse through exposure to other smokers and cigarette availability in series, as well as through exposure to places where smoking was allowed and cigarette availability in series.
Discussion
Despite broad declines in tobacco use in recent decades, low SES populations have not realized the full benefits of these reductions [6]. As such, tobacco researchers have sought to understand the range of factors contributing to the persistence of cigarette smoking among lower SES populations and the widening gap in SES-related tobacco disparities [29, 30]. The current study employed near real-time data to examine how SES differences in pro-smoking social contexts might hinder a cessation attempt and, ultimately, help drive SES-related tobacco disparities. Estimates from a multilevel structural equation model indicated that lower SES smokers experienced: (a) greater exposure to pro-smoking social contexts (i.e., other smokers and places where smoking was allowed), (b) increased cigarette availability, and (c) a higher likelihood of smoking lapse during a quit attempt. Moreover, pro-smoking social contexts and cigarette availability indirectly connected SES to lapse risk (see Table 3). Importantly, these associations were observed in a relatively low SES sample in which detecting SES-related differences might prove challenging. For example, approximately 15% of participants reported achieving a college degree, which was roughly half of the national average during the study period [31].
This study is among the first to demonstrate the detrimental effect of pro-smoking social contexts on lapse risk using near real-time data. Although smoking cessation programs have long been aware that exposure to pro-smoking social contexts can increase lapse risk for a smoker trying to quit [15], the current findings indicated that greater exposure to pro-smoking social contexts, and the resulting increase in cigarette availability, are mechanisms connecting SES to smoking lapse. Results of this study provide empirical justification for the inclusion of pro-smoking social contexts in theoretical models seeking to explain SES-related tobacco disparities [11, 19]. Cessation strategies specifically designed to help low-SES smokers navigate greater exposure to pro-smoking social contexts are likely to reduce SES-related tobacco disparities.
Our findings concur with results of a recent study demonstrating that lower SES smokers not engaged in a quit attempt also experienced greater exposure to places where smoking was allowed in daily life [13]. Our results suggest that other social context factors are important to consider beyond location-based smoking restrictions. There are multiple plausible scenarios that might explain these observed associations between SES, exposure to other smokers, exposure to places where smoking is allowed, and cigarette availability. For example, SES-related differences in workplace and home environments might foster these connections. Empirical studies have demonstrated that lower wage and blue collar workers are less likely to be employed in places where there are workplace smoking bans [32], and smokers in these occupations have more difficulty staying quit [32, 33]. Similarly, studies have reported that lower SES households are less likely to have home smoking restrictions or bans in place [34]. As such, lower SES smokers may experience greater exposure to smoking, other smokers, and readily available cigarettes at both work and home. The path from lower SES scores directly to increased cigarette availability (see Fig. 1) may also reflect features of social context unmeasured in the current study such as more frequent exposure to tobacco outlets. Lower SES neighborhoods have been shown to have a higher density of tobacco outlets [35] and living in closer proximity to a tobacco outlet has been linked with reduced success in quitting [36]. Taken together, exposure to pro-smoking social contexts found in workplaces, homes, and neighborhoods likely help normalize tobacco use, reduce perceptions of the substantial health risks emanating from tobacco use, and provide smoking cues that hinder staying quit [30]. Public health approaches directly targeting the normalization of tobacco use in low-SES workplaces and communities, broad application of smoking restrictions in public spaces, and zoning strategies to limit tobacco outlets in residential neighborhoods all have the potential to reduce exposure to mechanisms supporting SES-related tobacco disparities.
Although momentary exposure to other smokers, exposure to places where smoking was allowed, and readily available cigarettes increased risk for lapse even after accounting for recent smoking lapse (see within-person estimates in Table 2), our model identified additional momentary dynamics at play. The significant association of smoking lapse in interval j − 1 → j with subsequent increases in exposure to other smokers, exposure to places where smoking is allowed, and greater cigarette availability at time j suggests that smokers who have recently lapsed may be currently in possession of cigarettes and/or traveling to locations where other smokers have congregated to smoke. This possibility does not negate our primary interpretation given the persistence of significant paths from momentary increases in exposure to pro-smoking social contexts and cigarette availability at time j to subsequent lapse in interval j → j + 1 even after accounting for previous lapse. Not unexpectedly, our model suggests a reciprocal relationship between pro-smoking social contexts and smoking lapse. Secondly, for smokers trying to quit, our model hypothesized that cigarettes become more available as a function of exposure to other smokers or to locations where smoking is allowed. Individual travel patterns should not be thought of as random occurrences and it is possible that awareness of cigarette availability drives a smoker to seek out other smokers and places where smoking is allowed for the express purpose of obtaining cigarettes. In this case, our measure of cigarette availability would represent a characteristic of pro-smoking social contexts that serves to lure a smoker at risk for lapse to specific locations, as opposed to representing a downstream outcome of exposure to pro-smoking social contexts. Of course, exposure to pro-smoking social contexts that increase cigarette availability and cigarette availability serving to lure smokers to pro-smoking social contexts are unlikely to be mutually exclusive. Both interpretations reinforce the importance of our finding that lower SES smokers are, on average, experiencing greater exposure to pro-smoking social contexts, more readily available cigarettes, and, as a result, greater risk of smoking lapse during a quit attempt. Further research should seek to clarify the complex dynamics at work. Detailed location information on the specific places whereby participants report encountering other smokers increased cigarette availability (e.g., tobacco shops or other areas where smokers are known to congregate), and smoking lapse could add important information to aid in designing intervention strategies and policy approaches that facilitate smoking cessation among low SES individuals.
Some limitations to the current study should be noted. First, SES did not maintain a significant direct association with smoking lapse after accounting for demographic factors, social contexts, and cigarette availability. Although this was not unsurprising given that the total effect of SES on lapse risk was decomposed into the indirect effects displayed in Table 3 [25], it is important to note that additional risk factors may connect lower SES to smoking lapse. Previous research has suggested that stress or psychological distress may help explain challenges to quitting among low SES smokers [19]. These factors are likely to be intimately connected with pro-smoking social contexts (e.g., elevated stress resulting from attempts to maintain abstinence in the face of exposure to other smokers) and future research could help flesh out these relationships. Additionally, studies have found that individuals living in low SES neighborhoods are often targeted directly by tobacco company marketing [4]. It is likely that multiple features of living and working in low SES communities, stress and other psychological factors, and social contexts each contribute to reduced success in quitting among low SES smokers. Future studies should disentangle how these multiple factors are associated in the daily lives of low SES smokers trying to quit. Second, the smokers participating in the study all resided in Houston, TX, and smokers in rural areas or other urban areas may be systematically exposed to different levels of pro-smoking social contexts. For instance, smokers in rural areas regardless of SES may encounter fewer individuals who are currently smoking simply because they encounter fewer individuals. They may also experience fewer location-based smoking restrictions.
The results of this study contribute near real-time evidence to the growing consensus that low SES smokers experience more difficulty staying quit and have both conceptual and public health implications [4, 5]. A better understanding of the lived experiences and social contexts for low SES smokers is essential to improving cessation programs, developing strategies to target low SES smokers, and addressing the growing SES-related inequities in cigarette smoking. Most importantly, continued progress in understanding the reasons that low SES populations have not realized the full benefits of tobacco control successes is essential to eliminating SES-related tobacco disparities [29, 30].
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award numbers F32CA232796, R01DA014818, P30CA042014, and P30CA016672. Additional support was provided by the Huntsman Cancer Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Huntsman Cancer Foundation.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Christopher Cambron, Cho Y. Lam, Paul Cinciripini, Liang Li, and David W. Wetter declare that they have no conflict of interest.
Authors’ Contributions CC formulated the research question, designed the study, analyzed the data, and wrote the article. CYL contributed to the design of the study and reviewed the article. PC is a co-investigator on R01DA014818 that produced the data for this study. LL reviewed the article. DWW contributed to the design of the study, reviewed the article, and is the principal investigator on R01DA014818 that produced the data for this study.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the University of Texas MD Anderson Cancer Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. [DOI] [PubMed] [Google Scholar]
- 2. USDHHS. The Health Consequences of Smoking-50 Years of Progress. A Report of the Surgeon General. Atlanta, CA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 3. Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: an update. Am J Prev Med. 2015;48:326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107–123. [DOI] [PubMed] [Google Scholar]
- 5. Haskins J. Smoking rates still high among low-income Americans. Am J Public Health. 2017;107:1847–1847. [Google Scholar]
- 6. Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M; ITC Collaboration Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2010;12 Suppl:S20–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32:399–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gilpin EA, Pierce JP. Demographic differences in patterns in the incidence of smoking cessation: United States 1950-1990. Ann Epidemiol. 2002;12:141–150. [DOI] [PubMed] [Google Scholar]
- 9. Poland B, Frohlich K, Haines RJ, Mykhalovskiy E, Rock M, Sparks R. The social context of smoking: the next frontier in tobacco control? Tob Control. 2006;15:59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Cur Dir Psychol Sci. 2003;12:119–123. [Google Scholar]
- 11. Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007;102 Suppl 2:5–29. [DOI] [PubMed] [Google Scholar]
- 12. Fisher EB. The importance of context in understanding behavior and promoting health. Ann Behav Med. 2008;35:3–18. [DOI] [PubMed] [Google Scholar]
- 13. Jahnel T, Ferguson SG, Shiffman S, Thrul J, Schüz B. Momentary smoking context as a mediator of the relationship between SES and smoking. Addict Behav. 2018;83:136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shiffman S, Gwaltney CJ, Balabanis MH, et al. Immediate antecedents of cigarette smoking: an analysis from ecological momentary assessment. J Abnorm Psychol. 2002;111:531–545. [DOI] [PubMed] [Google Scholar]
- 15. Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. J Consult Clin Psychol. 1996;64:366–379. [DOI] [PubMed] [Google Scholar]
- 16. Paul CL, Ross S, Bryant J, Hill W, Bonevski B, Keevy N. The social context of smoking: A qualitative study comparing smokers of high versus low socioeconomic position. BMC Public Health. 2010;10:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychol Assess. 2009;21:486–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. [DOI] [PubMed] [Google Scholar]
- 19. Businelle MS, Kendzor DE, Reitzel LR, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychol. 2010;29:262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fiore M, Jaen C, Baker T.. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guidelines. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. [Google Scholar]
- 21. Shiffman S, Waters AJ. Negative affect and smoking lapses: a prospective analysis. J Consult Clin Psychol. 2004;72:192–201. [DOI] [PubMed] [Google Scholar]
- 22. Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol. 2011;62:583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation in multilevel data: The advantages of multilevel SEM. Struct Equ Modeling. 2011;18:161–182. [Google Scholar]
- 24. Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods. 2010;15:209–233. [DOI] [PubMed] [Google Scholar]
- 25. MacKinnon DP, Pirlott AG. Statistical approaches for enhancing causal interpretation of the M to Y relation in mediation analysis. Pers Soc Psychol Rev. 2015;19:30–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Muthen L, Muthen B.. Mplus. Los Angeles: Muthen & Muthen; 2017. [Google Scholar]
- 27. Muthén B, Asparouhov T. Bayesian structural equation modeling: a more flexible representation of substantive theory. Psychol Methods. 2012;17:313–335. [DOI] [PubMed] [Google Scholar]
- 28. Montoya AK, Hayes AF. Two-condition within-participant statistical mediation analysis: A path-analytic framework. Psychol Methods. 2017;22:6–27. [DOI] [PubMed] [Google Scholar]
- 29. Drope J, Liber AC, Cahn Z, et al. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68:106–115. [DOI] [PubMed] [Google Scholar]
- 30. Link BG, Phelan J. The social shaping of health and smoking. Drug Alcohol Depend. 2009;104 Suppl 1:S6–10. [DOI] [PubMed] [Google Scholar]
- 31. National Center for Education Statistics. Table 104.10: Rates of high school completion and bachelor’s degree attainment among persons age 25 and over, by race/ethnicity and sex. In U.S. Department of Education (ed.), Digest of Education Statistics; 2018. [Google Scholar]
- 32. Ham DC, Przybeck T, Strickland JR, Luke DA, Bierut LJ, Evanoff BA. Occupation and workplace policies predict smoking behaviors: analysis of national data from the current population survey. J Occup Environ Med. 2011;53:1337–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fagan P, Shavers VL, Lawrence D, Gibson JT, O’Connell ME. Employment characteristics and socioeconomic factors associated with disparities in smoking abstinence and former smoking among U.S. workers. J Health Care Poor Underserved. 2007;18:52–72. [DOI] [PubMed] [Google Scholar]
- 34. Zhang X, Martinez-Donate AP, Kuo D, Jones NR, Palmersheim KA. Trends in home smoking bans in the U.S.A., 1995-2007: prevalence, discrepancies and disparities. Tob Control. 2012;21:330–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rodriguez D, Carlos HA, Adachi-Mejia AM, Berke EM, Sargent JD. Predictors of tobacco outlet density nationwide: a geographic analysis. Tob Control. 2013;22:349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Reitzel LR, Cromley EK, Li Y, et al. The effect of tobacco outlet density and proximity on smoking cessation. Am J Public Health. 2011;101:315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]