Abstract
To raise awareness of high blood pressure (BP) levels and associated risk factors among the Sudanese population. A cross-sectional study was conducted in six Sudanese states during the period May–August 2018. The study area included public indoor and outdoor areas, institutes, and service facilities. A questionnaire for collecting the data was employed including demographic data, along with three consecutive BP measurements. Data were collected by trained volunteers. Hypertension (HTN) was defined as a systolic blood pressure ≥140 mmHg or a diastolic blood pressure ≥90 mmHg based on the mean of the second and third measurements, or in those on antihypertensive medication. The current study indicated a high prevalence of HTN (28.2%) among 40 779 participants and a low level of awareness (20.7%) amongst these participants. Of all, 18.2% of hypertensive participants were on medication and of these, 54.6% were controlled. Of all hypertensives, only 9.9% were controlled. Further action needs to be taken by all stakeholders for raising awareness and increasing screening provision of HTN, which are essential for the development of national health policies for control and management of HTN in Sudan.
Keywords: MMM, Hypertension, Blood pressure, Sudan
Introduction
The worldwide prevalence of hypertension (HTN) was estimated at 26.4% in 2000, and the projected number of adults who will have HTN by 2025 is 1.56 billion.1 Mortality due to HTN accounts for 20%–50% of all deaths.2 The highest prevalence of HTN has been reported in Africa, and approximately 80% of deaths in low-middle income countries are due to cardiovascular disease (CVD), the most common complication of HTN.3,4 High blood pressure (BP) is caused by behavioural risk factors including obesity resulting from unhealthy food intake and insufficient physical activity, and excessive alcohol consumption.5 Sudan has witnessed a rapid rise in the prevalence of HTN during the past few years as a result of behavioural changes and associated risk factors, due to rapid urbanization. It has the second-highest prevalence of HTN in North Africa, with one in four people with a non-communicable disease having HTN.6
The nationwide screening survey ‘May Month Measurement’ (MMM) is conducted worldwide by the International Society of Hypertension (ISH). In Sudan, the Sudanese Society of Hypertension, which falls under the umbrella of ISH, was responsible for conducting the survey in 2017 and 2018. Sudan lacks screening programs. The MMM screening survey provides a good chance to investigate the relationship between specific risk factors and BP levels among the Sudanese population. Large numbers of the Sudanese population can be screened regularly and educated about HTN in order to set preventive measures and control the disease.7 In 2018, the collaborators included the National Health Insurance Fund, Sudan Federal and State Ministries of Health in Sudan, the World Health Organization, Medical and Nursing Faculties, pharmaceutical companies, and Sudanese non-governmental organizations.
Objectives
To raise awareness of raised BP and to determine BP levels and associated risk factors among the Sudanese population.
Methods
This cross-sectional, community-based study was conducted in May–August 2018 in six Sudanese states: Khartoum, Gezira, Blue Nile, Port Sudan, Northern Darfur, and Kurdofan. A total of 850 volunteers trained by experts collected data. Sites included public indoor and outdoor areas, institutes, and service facilities. Volunteers were medical students and graduates, and supervised by medical staff from the participated Sudanese faculties of medicine and nursing sciences. A questionnaire was employed, and electronic BP devices (Omron) were used to measure BP. Ethical clearance was obtained from relevant Committees. Three BP readings were taken for each participant while sitting.8 Hypertension was defined as a systolic blood pressure (SBP) ≥140 mmHg or a diastolic blood pressure (DBP) ≥90 mmHg based on the mean of the second and third measurements, or in those on antihypertensive medication. Multiple imputations based on the global data9 were used to estimate the mean reading where either of the second or third measurement was unrecorded. Data were entered onto spreadsheets, and analysis was performed centrally by the MMM project team.
Results
Of the 40 779 participants enrolled in the survey, 47.3% were females. A total of 53.2% were of unknown ethnicity, 27.5% were of mixed race, and 8.8% were black. The mean age was 31.7 ± 14.4 years, and the overall mean body mass index (BMI) was 24.5 ± 5.0 kg/m2. The age and sex standardized mean for systolic BP was 121 mmHg and for diastolic BP was 80 mmHg. Among all participants, only 27.4% had ever had their BP recorded in the past.
Of 40 779 participants, 2570 (6.3%) reported a history of diabetes, 844 (2.1%) myocardial infarction, and 478 (1.2%) previous stroke. Of all participants, 7701 (18.9%) were overweight or obese, although there were 28.7% with unknown BMI. A total of 4157 (10.2%) respondents reported smoking, and only 55 (0.1%) reported the use of alcohol 1–3 times per month and 40 (0.1%) once or more per week. Among female participants, 405 (2.1%) were pregnant.
Out of 40 779 participants, a total of 11 497 (28.2%) were diagnosed with HTN, of whom 2375 (20.7%) were aware of their condition and 2088 (18.2%) were on medication, of whom, 1139 (54.6%) had controlled BP. Of all hypertensive participants, 9.9% were controlled. Of the 38 691 participants not taking antihypertensive medication, 9409 (24.3%) had a raised BP.
Based on linear regression models after adjustment for age and sex, both SBP and DBP were significantly higher in those receiving antihypertensive treatment, those fasting and those who were overweight or obese (vs. those of a healthy weight). Higher SBP was recorded among those who were smokers, those with a history of stroke and with alcohol use of once or more per week. Higher DBP was recorded among those with diabetes and a history of myocardial infarction (Figure 1). Measurement of BP using the left arm was associated with lower SBP and DBP. Conversely, Higher SBP and DBP were recorded during Fridays and Saturdays (vs. Mondays) and when BP was recorded in public areas (vs. hospitals/clinics).
Figure 1.
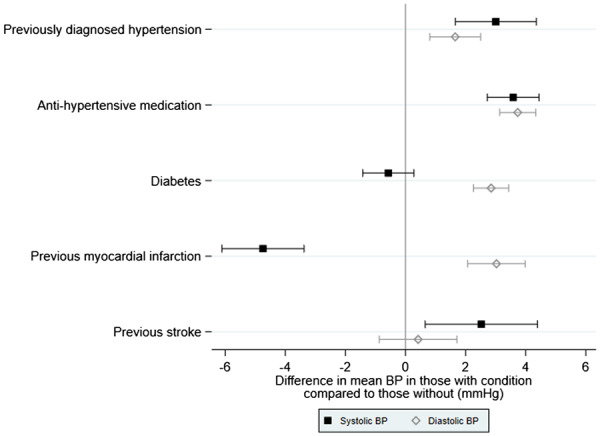
Difference in mean blood pressure in those with each characteristic compared to those without from linear regression models adjusted for age, sex, and antihypertensive medication (antihypertensive medication adjusted for age and sex alone).
Discussion
Sudan has witnessed a rapid rise in the prevalence of HTN during the past few years due to urbanization and changing lifestyles.8,10–13
The current study indicated a high rate of HTN (28.2%) and a low level of awareness about the disease (only a fifth of the hypertensive population), reflected in the low proportion of hypertensive participants receiving treatment (18.2%). In a cohort study conducted between (2011–12), much lower levels of awareness were reported in sub-Saharan African countries (Uganda, South Africa, Tanzania, and Nigeria), where only half of the population was aware of HTN and its consequences.11,12 Awareness is important for the purpose of lifestyle modification and compliance to treatment.14
Among the studied states, normal BP levels were evident only among a small proportion of the population.
Compared to MMM 2017, this study showed higher rates of HTN among participants who were not on treatment (24.3% vs. 15.9%) and slightly higher rates of uncontrolled BP among those who were on treatment (45.4% vs. 41.3%). These groups of the population, with untreated HTN and with poor control, are more likely to proceed to develop complications of HTN and ultimate disability or death.
Everyday life in Sudan is tough for both genders; males may have other additional risk factors that cause them to have higher BP values. At weekends (Fridays and Saturdays), higher levels of BP were noticed. Obesity, smoking, and diabetes were also among the identified risk factors for HTN among the Sudanese screenees. Participants with a history of stroke, elevated BMI, diabetes, or history of previous myocardial infarction had findings consistent with previous epidemiological studies.
This study has highlighted the large proportion of Sudanese people with increased BP levels which are due to several known risk factors; other hidden factors need to be investigated in the near future. Further action should be taken by all stakeholders.
Acknowledgements
A special thanks is given to all collaborators and volunteers. Investigators who organized and led field work: Ibrahim Draig, Abdelfatah I. Karar, Mona A. Eltaib, Khalid M, Eisa, Jalal Abdelrasoul, Mosab A. Osman, Abeer O Hussein, Awaab Gadour, Khalida H. Saeed, Awatif A Alhassan, Amna M. Elasha, Nadia M. Amin, Ibtisam Alfadil.
Funding
The funding institutes are: (1) International Society of Hypertension: 150 Electronic Devices and $ 4,400. (2) National Sudan Health Insurance Fund: 25,000 Sudanese Ginahs for each of six states campaigns; total of 150,000 Sudanese Ginahs and final 10,000 Sudanese Ginahs making total 160,000 Sudanese Ginahs. (3) Astrazenica Pharmaceutical Company: 70,000 Sudanese Ginahs. (4) Alwali Pharmaceutical Company: 25,000 Sudanese Ginahs. (5) Al Hikma Pharmaceutical Company: 25,000 Sudanese Ginahs. 6. Fast Company: 10,000 Sudanese Ginahs. 7. International University of Africa: Logistics in transportation, Media.
Conflict of interest: none declared.
References
- 1. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J.. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:H217–H223. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Hypertension Control: Report of a WHO Expert Committee. WHO Technical Report Series, Vol. 862. Geneva: WHO; 1996. pH1–H83. https://apps.who.int/iris/handle/10665/38276 (21 March 2020). [PubMed] [Google Scholar]
- 3. World Health Organization. Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization; 2011.http://www.who.int/nmh/publications/ncd_report2010/en/ (21 March 2020).
- 4. World Health Organization. A global brief on hypertension: silent killer, global public health crisis. 2013. World Health Organization. http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/ (21 March 2020).
- 5.World Health Organization. Global status report on noncommunicable diseases, 2010. Geneva, Switzerland: World Health organization; 2011. https://www.who.int/nmh/publications/ncd_report2010/en/ (21 March 2020).
- 6. Elfaki BA, Mustafa HE, Elnimeiri MK.. Prevalence and awareness of hypertension among Sudanese rural population, Sinnar state, Sudan, 2016. J Nurs Educ Pract 2017;7:H1. [Google Scholar]
- 7. Ali I, Behairy H, Abugroun A, Beaney T, Kobeissi E, Abdalla A, Mohamed A, Wagialla N, Medani SS, Ismail EM, Hassan DA, Altahir FM, Gdoor A, Mohamed I, Elnour S, Poulter . May Measurement Month 2017: an analysis of blood pressure screening in Sudan—Northern Africa and Middle East. Eur Heart J Suppl 2019;21(Supplement_D):HD111–HD114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Sudan Steps Survey report; 2005. https://www.who.int/ncds/surveillance/steps/STEPS_Report_Sudan2005.pdf (21 March 2020).
- 9. Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, . May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J 2019;40:H2006–H2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Sudan STEPS Survey Report, Fact sheet; 2016. https://www.who.int/ncds/surveillance/steps/Sudan-2016-STEPSfactsheet.pdf?ua=1 (21 March 2020) .
- 11. Eckert S, Kohler S, Urbanization and health in developing countries: a systematic review. World Health Popul 2014;15:H7–H20. [DOI] [PubMed] [Google Scholar]
- 12. Mishra SR, Ghimire S, Shrestha N, Shrestha A, Virani SS.. Socio-economic inequalities in hypertension burden and cascade of services: nationwide cross-sectional study in Nepal. J Hum Hypertens 2019;33:H613–H625. [DOI] [PubMed] [Google Scholar]
- 13. Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, BajunirweS. F, Njelekela M, Chiwanga FS, Reid T, Volmink J, Adami H-O, Holmes MD, Dalal . The burden of hypertension in sub-Saharan Africa: a four-country cross sectional study. BMC Public Health 2015;15:H1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Singh S, Shankar R, Singh GP.. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int J Hypertens 2017.H–H.https://www.hindawi.com/journals/ijhy/2017/5491838/ (21 March 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]


