Abstract
New York City has been described as the epicenter of the COVID-19 pandemic in the United States. While health care workers are notably at increased risk for COVID-19 infection, the impact on resident physicians remains unclear. In this issue of the JCI, Breazzano et al. surveyed resident physicians for their exposure to COVID-19 during the exponential phase of the COVID-19 pandemic. The researchers also assessed how personal protective equipment and COVID-19 testing protected health care workers from infection. This study highlights resident physician experiences of the first COVID-19 wave that can inform and improve preparedness for upcoming COVID-19 surges and other future epidemics.
COVID-19 pandemic in New York City
COVID-19 is the most serious pandemic of this century and has affected nearly every country in the world. As of May 31, 2020, more than 6 million people were infected worldwide, with nearly 1.8 million people infected in the United States. The case fatality rate of COVID-19 is estimated at 2%–7% (1, 2), resulting in shocking numbers of deaths: more than 370,000 globally and more than 100,000 in the United States alone (as of May 31, 2020) (3). New York City has been particularly hard hit with more than 200,000 infected, more than 50,000 hospitalized, and more than 16,000 deaths (4). While the number of infected people in New York and other states is now declining, the epidemic is far from over. Because an effective vaccine is at least 18 months away (5), additional epidemic waves are likely to occur throughout the world. It is therefore imperative that we share experiences of the first COVID-19 wave and begin to implement lessons learned to improve preparedness for upcoming COVID-19 surges and other future epidemics.
Resident physicians’ exposure to COVID-19
In this issue of the JCI, Breazzano et al. reported important survey data on resident physicians’ exposure to COVID-19, and also described how personal protective equipment (PPE) and COVID-19 testing protect health care workers (HCWs) from infection (6). Response to their survey, especially during a time of unprecedented crisis (March 2, 2020, to April 12, 2020) was impressive: 91 of 340 program directors from 24 specialties responded, representing 2306 residents. The authors reported that 4.4% of surveyed residents had confirmed COVID-19, while 7.1% and 3.3% had presumed and suspected COVID-19, respectively. Residency is the critical training period after medical school, lasting 3 to 7 years depending on specialty, with some residents continuing specialized fellowship training after residency that may take another 2 to 4 years. During these years residents receive concentrated and rigorous training in their specialty; for example, internal medicine (IM) residents train primarily at ambulatory care practices, inpatient medicine wards, and medical intensive care units (ICUs). At the time of the COVID-19 epidemic, the Accreditation Council for Graduate Medical Education (ACGME), which oversees all accredited medical training programs in the United States, granted some institutions Pandemic Emergency Status, which allowed many nonmedical subspecialty training programs to suspend training in those fields and deploy their residents and/or fellows to care for COVID-19 patients in inpatient medical units, ICUs, and emergency departments.
While resident physicians are always supervised by senior physicians (attending physicians), resident physicians interact with patients more frequently and thus have more exposure to patients — including COVID-19 patients — than attending physicians. The results of the Breazzano et al. study are therefore surprising, as the frequency of infection among surveyed resident physicians was lower than expected and also substantially lower than what we observed at Montefiore Medical Center. Breazzano and authors reported a confirmed COVID-19 infection rate of 4.4% (6), while at Montefiore Medical Center our 2 large IM residency programs (with a total of 245 resident physicians) had a confirmed COVID-19 infection rate of 17.1% (42 infections confirmed by PCR testing [Benjamin T. Galen, Montefiore Medical Center, personal communication]). The combined infection rate reported by Breazzano et al. (which included confirmed, presumed, and suspected infections) was 14.8% (6), while at Montefiore Medical Center the combined infection rate was 26.9% (Benjamin T. Galen, Montefiore Medical Center, personal communication). The difference between the Breazzano et al. survey rates and the rates we observed suggests that either our Montefiore Medical Center resident physicians were more frequently tested than the study cohort, or that our resident physicians were more exposed, or both. With regard to testing, 32.2% of our residents (79 of 245) were tested but only 11.6% of the residents surveyed in the Breazzano et al. study were tested (6), suggesting that increased frequency of testing may have contributed to the higher rate of confirmed COVID-19 infections we observed (Benjamin T. Galen, Montefiore Medical Center, personal communication).
Another potential reason for the higher infection rate among our resident physicians is that they were more exposed to COVID-19 patients. Indeed, Montefiore Medical Center is located in the Bronx, which has the highest COVID-19 infection rate in New York City (7) and may thus have exposed our resident physicians to a higher number of COVID-19 patients than the hospitals participating in the Breazzano et al. study (6). Moreover, our data included only IM residents, whereas in the Breazzano et al. study only a minority of residents surveyed (5.2%) were IM residents (6). During the surge, our IM residents were deployed only to high exposure areas (inpatient medicine wards, ICUs, and emergency rooms), and we estimate that each resident had 20 to 30 daily interactions with COVID-19 patients; these interactions may have included aerosolizing procedures (e.g., nasopharyngeal swabbing for PCR testing). In addition, our IM resident physicians respond to and lead all cardiac arrests and rapid responses, which were very frequent during the surge (the peak was over 30 per day at Montefiore Medical Center) and exposed residents to aerosolizing procedures, such as intubations. As mentioned, in the reported survey only 5.2% of respondents were IM resident physicians and the authors do not indicate to which units the residents from non-IM specialties were deployed, nor how frequently they were exposed to COVID-19 patients or to aerosolizing procedures (6). Therefore, we cannot compare our resident physicians’ exposure to that of the resident physicians in the study, but it is likely that our resident physicians had more exposure than those surveyed in Breazzano et al. (6).
A second important point raised by the findings of the survey from Breazzano et al. is the importance of timely and accurate COVID-19 diagnosis among resident physicians (6). The ability to test and quarantine residents is essential to having a healthy workforce to meet patient care needs, and was critical during the exponential phase of the pandemic. Knowing resident physicians’ COVID-19 status is key to preventing infections among other HCWs and patients. In addition, having to quarantine residents with equivocal symptoms without confirmatory testing can lead to unnecessary reductions of this vital workforce. Breazzano and colleagues reported estimates for presumed, suspected, and confirmed COVID-19 cases, with presumed cases defined as symptomatic resident physicians who were unable to obtain testing. Figure 3 in Breazzano et al. showed that the number of residents with presumed COVID-19 infection peaked 1 week earlier than confirmed cases (6). Most likely this difference represents increased access to testing as time went on, but also raises the question of whether the presumed cases included uninfected residents who had to be quarantined because testing was unavailable.
Personal protective equipment
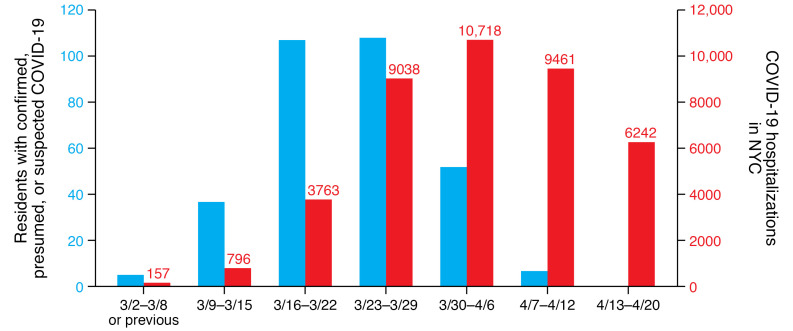
Breazzano and researchers also reported another major finding, that underavailability of PPE during this time period may have put residents at risk of COVID-19 infection. Forty-three of 87 program directors (49.4%) reported that their residents had to work with suboptimal PPE, and 99.2% of residents reported extending the use of or reusing their face masks (6). At the same time as cases of COVID-19 were increasing exponentially in New York City, the CDC revised its recommendations several times (likely because of nationwide PPE shortages). Early in the New York City epidemic the CDC recommended that HCWs wear surgical masks when treating COVID-19 patients (except during aerosolizing procedures), but later (when PPE was no longer in short supply) the CDC recommended using N95 respirators in all COVID-19 patient encounters (8). This change in PPE policy and availability had profound effects: Figure 1 shows that the number of residents infected with COVID-19 as reported by Breazzano et al. peaked 1 to 2 weeks before the peak number of COVID-19 hospitalizations across New York City (6, 9). At the time of peak hospitalizations in New York City, the number of infected residents had decreased, suggesting that adequate PPE was highly effective in preventing HCW exposure and infection.
Figure 1. The number of residents infected with COVID-19 peaked 1 to 2 weeks before the peak number of COVID-19 hospitalizations across New York City.
The blue bars represent the estimated sum of the number of residents with presumed, confirmed, or suspected COVID-19 during each of the weeks described in the paper by Breazzano et al. (left y axis) (6). The total number of COVID-19 hospitalizations per week across all New York City hospitals (red bars, right y axis) peaked during the week of 3/30–4/6 (9). The change in PPE policy and availability may have influenced the COVID-19 cases among resident physicians.
Guidance in devising new policies on epidemic preparedness
Pandemics and large epidemics, like severe weather events, earthquakes, and nuclear disasters, are inevitable and warrant preparation. After nuclear reactor disasters (mainly Chernobyl) the United States implemented policies to stockpile and predistribute potassium iodide (KI) for future events (10). Specifically, national legislation mandated that KI be available at key locations for distribution to protect local populations in the event of nuclear fallout. While the COVID-19 pandemic is not completely analogous to nuclear disasters, there are similarities: inability to predict timing, location, or number of people affected, and the extraordinary number of resources that need to be mobilized. Government agencies should prepare for all disasters, including large epidemics and pandemics. Such preparedness must include stockpiling and distribution plans for PPE, rapid deployment of resources to develop new testing kits and vaccines (in the case of an emerging pathogen, such as SARS-CoV-2), and maintaining adequate supply and a plan for distribution of existing test kits and vaccines (in the case of a known pathogen). Regardless of pathogen, PPE is critical for HCWs and other essential workers to perform their jobs safely. Government agencies must study the successes and failures of our health care system’s COVID-19 response to ensure adequate preparedness for the next large epidemic. The data in the study by Breazzano et al. should serve as important guidance in devising new policies on epidemic preparedness. Only careful planning and preparedness will ensure that the confusion and exposure we witnessed in March and April in New York City will not happen again.
Acknowledgments
We thank Ross Merkin, Ariel Kruger, Gaurav Bhardwaj, and Benjamin Galen for sharing with us their data of COVID-19 infection rates among IM residents at Montefiore Medical Center. We also thank Andrew Racine for helpful discussions and suggestions.
Version 1. 06/23/2020
In-Press Preview
Version 2. 08/04/2020
Electronic publication
Version 3. 09/01/2020
Print issue publication
Footnotes
Conflict of interest: YT was the primary investigator on a basic research project jointly funded by the Juvenile Diabetes Research Foundation and Pfizer. YT has 2 patent applications (PCT/US2016/067775 and US provisional 61/883,062).
Copyright: © 2020, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2020;130(9):4543–4545. https://doi.org/10.1172/JCI140296.
See the related article at New York City COVID-19 resident physician exposure during exponential phase of pandemic.
Contributor Information
Lauren I. Shapiro, Email: LSHAPIRO@montefiore.org.
Grace R. Kajita, Email: gkajita@montefiore.org.
Yaron Tomer, Email: ytomer@montefiore.org.
References
- 1.Omer SB, Malani P, Del Rio C. The COVID-19 pandemic in the US: A clinical update. JAMA. doi: 10.1001/jama.2020.5788. doi: 10.1001/jama.2020.5788. [published online April 6, 2020]. [DOI] [PubMed] [Google Scholar]
- 2.Barthel W, Markwardt F. Aggregation of blood platelets by adrenaline and its uptake. Biochem Pharmacol. 1975;24(20):1903–1904. doi: 10.1016/0006-2952(75)90415-3. [DOI] [PubMed] [Google Scholar]
- 3. Johns Hopkins University. Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html Updated June 24, 2020. Accessed June 24, 2020.
- 4. NYC Health. COVID-19: Data. Summary. https://www1.nyc.gov/site/doh/covid/covid-19-data.page#download Updated June 24, 2020. Accessed June 24, 2020.
- 5.Amanat F, Krammer F. SARS-CoV-2 vaccines: status report. Immunity. 2020;52(4):583–589. doi: 10.1016/j.immuni.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breazzano MP, et al. New York City COVID-19 resident physician exposure during exponential phase of pandemic. J Clin Invest. 2020;130(9):4726–4733. doi: 10.1172/JCI139587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. NYC Health. COVID-19: Data. By borough. https://www1.nyc.gov/site/doh/covid/covid-19-data-boroughs.page Updated June 24, 2020. Accessed June 24, 2020.
- 8. CDC. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html Updated July 15, 2020. Accessed May 25, 2020.
- 9. NYC Health. COVID-19: Data. Summary. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Updated July 22, 2020. Accessed May 27, 2020.
- 10.Leung AM, et al. American Thyroid Association scientific statement on the use of potassium iodide ingestion in a nuclear emergency. Thyroid. 2017;27(7):865–877. doi: 10.1089/thy.2017.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]