Abstract
Corona virus disease 2019 (COVID-19) affected medical student clerkships and education around the country. A virtual medical student clerkship was created to integrate didactic education with disease specific lectures for medical students, contouring, and hands on learning with telehealth. Twelve medical students in their 3rd and 4th year were enrolled in this 2 week elective from April 27, 2020 to June 5, 2020. There was significant improvement of overall knowledge about the field of radiation oncology from pre elective to post elective (P < .001). Feedback included enjoying direct exposure to contouring, telehealth, and time with residents. Overall this 2 week rotation was successful in integrating radiation oncology virtually for medical students. This is now being expanded to multiple institutions as an educational resource and future rotations for medical students.
With the advent of corona virus disease 2019 (COVID-19), the landscape of medical-student education has completely transformed, with students no longer permitted on-site for the vast majority of clinical rotations. Elective rotations to further explore specialties at outside institutions are essentially cancelled indefinitely. As hospitals adapt to legal restrictions and public health recommendations, many specialties have learned how to convert in-person patient care to telehealth, and medical educators have quickly and effectively transitioned resident education to virtual platforms.1 Radiation oncology, a technology-forward specialty, is particularly well-positioned to both create and innovate virtual medical student education.2
At Oregon Health & Science University, a virtual 2-week radiation oncology elective for medical students was created that integrated traditional didactic education with hands-on learning and telehealth patient exposure. The elective comprised prerecorded 30-minute lectures on the basics of radiation oncology, palliative radiation, radiation-based management of oncologic emergencies, as well as 8 subsite disease-specific lectures using a mix of both new and established content.3,4 In addition, representatives from dosimetry, radiation therapy, and medical physics developed video-based lectures for these students.
The experience of creating and implementing this type of elective has helped provide novel feedback on educational elements that may augment future rotations. Also, similar to telemedicine in the clinic, the development of robust virtual education platforms may establish a unique niche within medical education in the future.
Hands-On Learning
Hands-on exposure is one of the most critical aspects of learning in the medical school curriculum.5 These live experiences have been proven to be effective in prior simulation-based education studies with medical students.6,7 To provide students in the current environment a hands-on exposure to radiation oncology, students were given access to an institutional contouring platform along with 7 to 9 clinical vignettes and accompanying computed tomography simulation images, as well as instructions to contour both specific target volumes and organs at risk. Students also spent time with dosimetry through lectures and with residents to understand treatment planning aspects. Each day, faculty, residents, and medical students virtually met for contour and case review via chart rounds. Additionally, 4 times a week, residents gave 30-minute case presentations on a particular topic. Students were paired with a resident each week to discuss cases as well as being integrated into telehealth visits. Medical students observed virtual and telephone telehealth visits and were “patched in” to both types of visits with permission of the patient. These telehealth visits were also discussed separately with students prior to and/or after to discuss nuances of the case with the student. Lastly, students gave final 15-minute presentations to the department on a topic of their choice.
Didactics
There is a relative lack of didactic radiation oncology exposure for medical students, with less than one-third of medical students reporting any didactic training geared toward their level of training.8 In this 2-week virtual elective, prerecorded 30-minute lectures that are designed to focus on the basics of a specific cancer or disease site and are targeted for medical students can continue to be used for future medical clerkship rotations. These mini lectures could be used just as the American Society for Radiation Oncology spring refresher education sessions are used for residents and attendings, as overviews and resources on specific topics. These videotaped lectures are accessible to medical students at different institutions as an open learning repository.9 At the end of the course and after watching these didactic lectures, students were asked to complete a 48-question multiple choice examination that included general questions on radiation oncology as well as disease-specific questions, which were reviewed by content experts for content and appropriateness.
Student Feedback and Experience
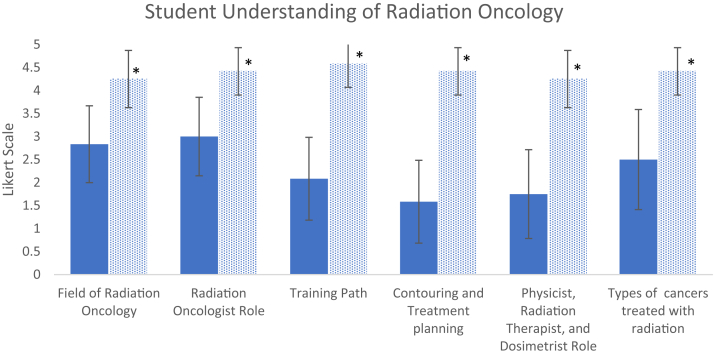
Results from a paired t test for 12 initial participants revealed a significant improvement in overall knowledge about radiation oncology from baseline to postelective (P < .001) from April 27, 2020, to June 5, 2020 (Fig 1). General feedback on the course from learners was positive, with participants reporting excitement to contour and enjoyment of direct feedback and faculty relationships as well as exposure to a field that they would not have typically had the opportunity to experience. Some participants expressed a desire to spend more time with telehealth consult and follow-up patients as well as learning more about treatment planning.
Figure 1.
Medical student understanding of radiation oncology. Including understanding the field of radiation oncology, the radiation oncologist role in cancer care, radiation oncology training path; contouring and treatment planning; understanding the role of a physicist, radiation therapist, and dosimetrist; and types of cancers treated by radiation oncologists (n = 12) by Likert scale from April 27, 2020, to June 5, 2020 (all P values <0.001).
Future of Medical Student Clerkships in Radiation Oncology
There are several strengths to this virtual medical student clerkship approach. First, it provided a formalized set of didactics often missing in medical student training.4 These prerecorded lectures required no additional investment of time from teaching faculty and can be employed to augment future medical student rotations, both in-person and virtual. These lectures have been added to a repository on www.radoncvirtual.com and are able to be accessed from any institution and perhaps internationally.9 Medical students may watch a prerecorded lecture before being paired with a disease-specific attending and use the appropriate contouring case in conjunction with the clinical exposure.
Another strength of the virtual approach is the time and financial convenience. Visiting or away clerkships in radiation oncology were increasingly common and necessary for successful match outcomes before COVID-19. Over one-third of medical students match into an institution in which they visited as an away rotation. Students spend an average of 2 to 3 rotations in radiation oncology outside of their home institution, often in another city and/or state.10,11 This utilization of away rotations as prolonged “sub internships” decreased the opportunity for many students with personal or financial constraints to consider radiation oncology as a specialty. For example, for a medical student to find lodging, travel, and food during a single rotation has been estimated to cost nearly $1000.12 A virtual rotation decreases those barriers and allows for students to “visit” a diverse set of programs. A virtual rotation may also enhance access and exposure to medical students whose medical schools do not have academic radiation oncology programs.
Finally, a strength of this virtual elective is that it lowers barriers for medical student exposure to our small field. As residency applications for radiation oncology decrease and medical student interest appears to be waning,13 this begs the question of inadequate exposure to radiation oncology for medical students in this field.14 Additional innovations in education include the recently launched Radiation Oncology Virtual Education Rotation, a series of virtual educational sessions open to medical students around the world.9 These virtual sessions include case-based discussions on disease-specific topics with faculty from institutions across the country, and like virtual electives, they can also help to fill the gap left by suspended away rotations this summer.
A key aspect of radiation oncology electives is not only educating future radiation oncologists but future physicians entering various specialties that refer to or work with radiation oncology. Virtual medical student radiation oncology electives, although not ideal, may augment and allow for many aspects of the in-person rotation to be improved, as well as offer new areas to be explored post–COVID-19 pandemic.
We also acknowledge limitations to this approach. Our field’s experience with virtual electives is still limited, which warrants further follow-up with more students. Virtual electives may limit in-person patient and attending/resident interactions. The inability to sit next to a patient with cancer and their family is one of the greatest limitations, as students who may consider radiation oncology must have a passion for working with patients with cancer. This virtual approach, while developed out of necessity and lacking the benefit of extensive piloting, attempts to overcome the current limitations in direct patient exposure due to COVID-19 while offering additional educational benefits that might not have been discovered without the crisis.
COVID-19 necessitated many changes in our clinical and operational environment, but it also provided an opportunity for ingenuity in medical student education. We are now working to expand this virtual elective to multiple institutions across the country to continue to improve educational resources and future rotations for medical students.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
References
- 1.Pollom E.S., Frank J., Miller J. Continuing medical student education during the COVID19 pandemic: Development of a virtual radiation oncology clerkship. Adv Radiat Oncol. 2020;5:732–736. doi: 10.1016/j.adro.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahn JM, Wairiri L, Jimenez RB, et al. Virtual medical student elective in radiation oncology in the era of Covid-19. Radiation Oncology Education Collaborative Study Group Annual Symposium. May 15, 2020.
- 3.Jimenez R.B., Johnson A., Padilla L. The impact of an introductory radiation oncology curriculum (IROC) for radiation oncology trainees across the United States and Canada. Int J Radiat Oncol Biol Phys. 2020 doi: 10.1016/j.ijrobp.2020.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Golden D.W., Spektor A., Rudra S. Radiation oncology medical student clerkship: Implementation and evaluation of a bi-institutional pilot curriculum. Int J Radiat Oncol Biol Phys. 2014;88:45–50. doi: 10.1016/j.ijrobp.2013.10.041. [DOI] [PubMed] [Google Scholar]
- 5.Gordon J.A., Wilkerson W.M., Shaffer D.W., Armstrong E.G. "Practicing" medicine without risk: Students' and educators' responses to high-fidelity patient simulation. Acad Med. 2001;76:469–472. doi: 10.1097/00001888-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Rooney M.K., Zhu F., Gillespie E.F. Simulation as more than a treatment-planning tool: A systematic review of the literature on radiation oncology simulation-based medical education. Int J Radiat Oncol Biol Phys. 2018;102:257–283. doi: 10.1016/j.ijrobp.2018.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radiation Oncology Education Collaborative Study Group ROECSGWC. Golden D.W., Braunstein S. Multi-institutional implementation and evaluation of a curriculum for the medical student clerkship in radiation oncology. J Am Coll Radiol. 2016;13:203–209. doi: 10.1016/j.jacr.2015.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jagadeesan V.S., Raleigh D.R., Koshy M., Howard A.R., Chmura S.J., Golden D.W. A national radiation oncology medical student clerkship survey: didactic curricular components increase confidence in clinical competency. Int J Radiat Oncol Biol Phys. 2014;88:51–56. doi: 10.1016/j.ijrobp.2013.11.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Virtual Radiation Oncology For Medical Students. www.radoncvirtual.com Available at: Accessed July 5, 2020.
- 10.Jang S., Rosenberg S.A., Hullet C., Bradley K.A., Kimple R.J. Value of elective radiation oncology rotations: How many is too many? Int J Radiat Oncol Biol Phys. 2018;100:558–559. doi: 10.1016/j.ijrobp.2017.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sidiqi B.U., Gillespie E.F., Lapen K., Tsai C.J., Dawson M., Wu A.J. Patterns and perceptions of "away" rotations among radiation oncology residency applicants. Int J Radiat Oncol Biol Phys. 2020 doi: 10.1016/j.ijrobp.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winterton M., Ahn J., Bernstein J. The prevalence and cost of medical student visiting rotations. BMC Med Educ. 2016;16:291. doi: 10.1186/s12909-016-0805-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bates J.E., Amdur R.J., Lee W.R. Unfilled positions in the 2020 radiation oncology residency match: No longer an isolated event. Pract Radiat Oncol. 2020 doi: 10.1016/j.prro.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Zaorsky N.G., Shaikh T., Handorf E. What are medical students in the united states learning about radiation oncology? Results of a multi-institutional survey. Int J Radiat Oncol Biol Phys. 2016;94:235–242. doi: 10.1016/j.ijrobp.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]