ABSTRACT
Background
Despite increasing research on the double burden of malnutrition (DBM; i.e., coexisting over- and undernutrition), there is no global consensus on DBM definitions.
Objectives
To identify published operational DBM definitions, measure their frequency of use, and discuss implications for future assessment.
Methods
Following a structured search of peer-reviewed articles with terms describing “overnutrition” [e.g., overweight/obesity (OW/OB)] and “undernutrition” (e.g., stunting, micronutrient deficiency), we screened 1920 abstracts, reviewed 500 full texts, and extracted 623 operational definitions from 239 eligible articles.
Results
We organized three identified DBM dimensions (level of assessment, target population, and forms of malnutrition) into a framework for building operational DBM definitions. Frequently occurring definitions included coexisting: 1) OW/OB and thinness, wasting, or underweight (n = 289 occurrences); 2) OW/OB and stunting (n = 161); 3) OW/OB and anemia (n = 74); and 4) OW/OB and micronutrient deficiency (n = 73).
Conclusions
Existing DBM definitions vary widely. Putting structure to possible definitions may facilitate selection of fit-for-purpose indicators to meet public health priorities.
Keywords: literature review, double burden, assessment, malnutrition, noncommunicable disease, obesity, stunting, anemia, micronutrient deficiency
A systematic review identifying operational definitions of the double burden of malnutrition, measuring their frequency of use, and recommending assessment considerations, including a framework for building operational definitions.
Introduction
Globalization and urbanization are creating rapidly changing contexts in which populations can experience multiple forms of malnutrition (1). This concept, termed the “double burden of malnutrition” (DBM) has emerged over the past 3 decades (2–6) and recently has received increased attention as indicated by the series on DBM in The Lancet (1, 7–9). WHO refers to DBM as “characterized by the coexistence of undernutrition along with overweight, obesity or diet-related noncommunicable diseases (NCDs), within individuals, households and populations, and across the life-course” (10). This broad definition soberly confronts the current state of global health where rising rates of overweight and obesity overlap with stagnant or slowly decreasing rates of underweight and stunting (11–13). Yet, it does not provide specific guidance on how to operationalize the measurement of DBM. To address the growing global challenge of DBM, its prevalence must be assessed and monitored, potential interventions tested in research, and effective strategies applied though public health platforms; these activities require clear operational definitions of DBM.
Previous literature has provided comprehensive reviews of the nutrition transition (14, 15), possible etiology of selected forms of DBM (2, 7), and estimates of its prevalence (16–19). Early estimates of DBM prevalence defined it as households containing an overweight or obese mother and a stunted child (4, 20), whereas later work included a range of anthropometric and biochemical outcomes measured in populations, households, and individuals (21). Varela-Silva et al. (22) characterized different types of DBM using a variety of anthropometric indicators, and discussed implications of DBM measurement in prevalence assessments. They emphasized that the indicators used to classify individuals, households, and populations as “double burden” have far-reaching policy and programmatic consequences, such as which target population receives an intervention (22). Their viewpoint is shared by others in the field (23), and highlights an important challenge in interpreting DBM data: that the variation in DBM definitions and indicators of assessment in use in DBM research can result in differing global estimates of DBM prevalence (24). This makes accurate assessment and surveillance of DBM difficult, and could impede progress in the development of effective interventions and policies. Specific definitions, tailored to different programmatic or policy needs, will aid nutrition program planning and policy development and facilitate comparison of DBM data across populations and over time.
To our knowledge there has not been a systematic examination of the operational definitions used to describe DBM. As a first step, this systematic review aimed to identify the definitions used in the literature to assess DBM and to measure their frequency of use. We identify 3 dimensions of DBM definitions (level of assessment, target population assessed, and forms of malnutrition measured) and discuss implications of the selected operational definition of DBM for the interpretation and use of results in research and programmatic settings. In this review, we did not aim to conduct a meta-analysis or report global or regional prevalence of DBM, but we explored the range of DBM prevalence estimates reported in the included articles, as estimated by comparing household-level with dyad-level with individual-level definitions.
Methods
Database search and screening
To identify the variety of DBM definitions in use in the literature, we performed a structured search in PubMed and Scopus of any peer-reviewed articles published before July 12, 2017. The search strategy was developed using keywords related to DBM (double burden, obesity, underweight, malnutrition, etc.), included articles published in any language, and did not include a specific publication start date (Supplemental Methods 1and2). The initial search yielded 1920 titles and abstracts, which were transferred to Covidence (Covidence systematic review software; Veritas Health Innovation) for screening. After removal of duplicates, researchers screened the titles, abstracts, and full texts in duplicate following inclusion and exclusion criteria listed below. Discrepancies were resolved by discussion and consensus.
Inclusion and exclusion criteria
We included cross-sectional studies that aimed to assess the overlap between “overnutrition” and “undernutrition,” that is, studies that presented data on the prevalence of the “double burden of malnutrition,” “dual burden of malnutrition,” or a similar term. Articles examining the nutritional status of obese individuals (e.g., an association between vitamin D or iron deficiency and BMI) were included if the study objectives were framed as related to DBM. Additionally, included articles could be: 1) an analysis of primary or secondary data, 2) baseline data from longitudinal studies or randomized controlled trials, 3) gray literature [e.g., government reports or conference proceedings not published in academic journals (25), such as the Nutrition Papers series from the FAO (26)], and 4) data gathered and/or analyzed at the individual, household, or population level.
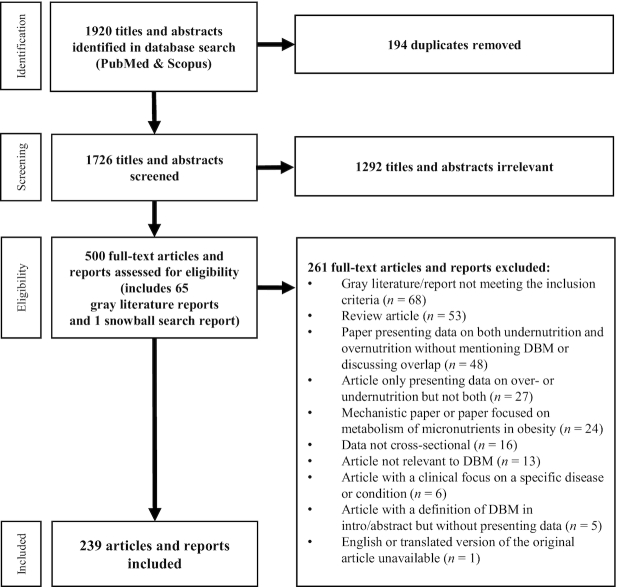
Articles and reports were excluded if they did not present a new analysis of data (such as review articles), or if the article did not present data on both “over-” and “undernutrition.” Additionally, articles with a clinical focus were excluded (i.e., articles focused on patients recovering from bariatric surgery who developed micronutrient deficiencies), as were articles focused on the metabolism of micronutrients in obesity or that examined a “double burden” of infectious disease and chronic disease. See Figure 1 for the complete exclusion criteria.
FIGURE 1.
Flow of identification and eligibility assessment of articles for a systematic review of operational definitions of the double burden of malnutrition (DBM).
Data extraction
A standardized data extraction form was developed in Microsoft Excel (version 2016) and piloted to review eligible articles. Research interns then extracted data in duplicate until discrepancies in data extraction were minimal. Random duplicate extractions continued throughout the data extraction process to assess continued adherence to extraction methodology (n = 78 articles extracted in duplicate, 33%).
Descriptive information extracted from each article included: year of publication, setting [country, world region (27), and urban or rural designation], World Bank income level (27), study design, data source, sex, physiological status and age of the target population, and the DBM term used in the article (double burden, dual burden, triple burden, etc.). DBM definition data extracted from each article included: the article's definition of “overnutrition” and the indicators used [i.e., overweight/obesity (OW/OB) as measured by BMI or BMI z-score], and the article's definition of “undernutrition” and the indicators used (i.e., stunting as measured by height-for-age z-score or anemia as measured by hemoglobin concentration); the population included in the definition of DBM (age groups were defined according to their designation in the original study); the level at which DBM was assessed (individual, dyad, household, or population level where household and dyad levels were defined as in the original study); and reported DBM prevalence. Finally, we recorded whether or not the primary objective of the article was clearly specifically to assess DBM, as opposed to an article presenting data on DBM but with a different primary objective. We then conducted a sensitivity analysis limited to those articles that specifically aimed to assess DBM to explore whether definitions of DBM differed according to the primary objective of the article.
The primary outcome was the frequency of occurrence of operational definitions of DBM, comprising the level of assessment, target population, and forms of malnutrition measured.
Data analysis
Descriptive analyses were performed using SAS statistical software version 9.4 (SAS Institute Inc.) and Microsoft Excel (2016). Frequencies were calculated for all included articles (n = 239), for all reported operational definitions of DBM (n = 623), and for articles whose primary objective was to assess DBM (n = 134). The median and range of reported DBM prevalence are presented for household, dyad, and individual level data, and for the different operational definitions of DBM. We did not include reported DBM prevalence data measured at the population level because each data point consists of multiple prevalence estimates making the data difficult to summarize.
Results
Article characteristics
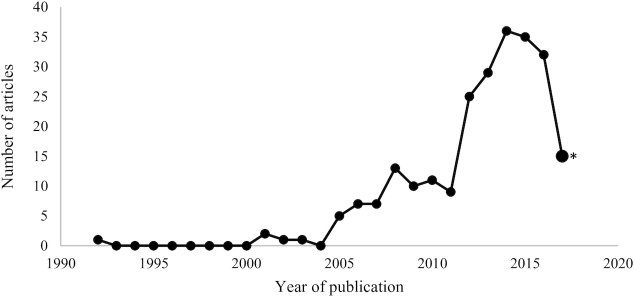
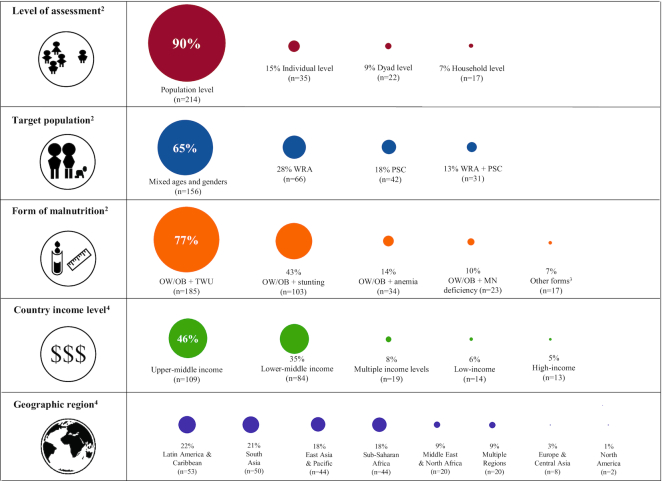
A total of 500 articles, including 66 gray literature reports and articles identified in online or snowball searches (references identified in the reference list of screened articles), proceeded to the full-text review; 239 articles and reports met the criteria for data extraction (Figure 1, Supplemental Table 1). Publication dates ranged from 1992 to 2017, with 72% (n = 172) of the articles published after a distinct increase in 2011 (Figure 2). Included articles were primarily from peer-reviewed journals (97%), and 59% of articles sourced or collected data from population-based national or regional surveys with a health or nutrition focus. More than half (64%) of the articles reported conducting studies in both urban and rural settings. The majority of articles focused on multiple population subgroups, for example, women of reproductive age and young children; no article focused solely on male participants. DBM terminology most frequently used in the literature included “double burden” or “dual burden” (71%), or described the overlap as the “coexistence of” or “simultaneous presence of” varying forms of malnutrition. Three papers assessed a “triple burden” of malnutrition described as coexistence of either 1) obesity, physical inactivity, and undernutrition (28); 2) obesity, undernutrition, and hypertension (29); or 3) adult OW/OB, child stunting, and intestinal parasite infections (30) (Table 1). DBM data from upper-middle-income countries comprised the majority of analyses (n = 109 articles, 46%) and almost half (n = 103 articles, 43%) used data from Latin America and the Caribbean or South Asia (Figure 3). The majority of single-country DBM assessments took place in India (n = 34 articles, data not shown).
FIGURE 2.
Articles published by year (n = 239) included in the systematic review of operational definitions of the double burden of malnutrition. *Data for 2017 include articles published up to July 11, 2017.
TABLE 1.
General characteristics of articles included in the systematic review of operational definitions of the double burden of malnutrition1
| Characteristics | Number (n = 239) | Percentage |
|---|---|---|
| Literature type | ||
| Peer-reviewed journal article | 231 | 97 |
| Gray literature report | 8 | 3 |
| Study design | ||
| Population-based survey, national | 100 | 42 |
| Population-based survey, regional | 41 | 17 |
| Convenience sample survey | 74 | 31 |
| Baseline RCT or cohort study | 3 | 1 |
| Other | 21 | 9 |
| Data source | ||
| Demographic and Health Surveys | 36 | 15 |
| National nutrition survey | 29 | 12 |
| Other survey/study design | 174 | 73 |
| Survey setting | ||
| Both urban and rural | 153 | 64 |
| Urban only | 340 | 14 |
| Rural only | 21 | 9 |
| Unspecified | 31 | 13 |
| Sex of survey participants | ||
| Both | 188 | 79 |
| Female | 51 | 21 |
| Male | 0 | 0 |
| Physiological status of women | ||
| Not pregnant | 124 | 52 |
| Pregnant | 2 | 1 |
| Both | 8 | 3 |
| Unspecified | 105 | 44 |
| Age group2 | ||
| Multiple age groups3 | 142 | 59 |
| Preschool (∼0–5 y) | 19 | 8 |
| School age (∼5–12 y) | 16 | 7 |
| Adolescent (∼13–18 y) | 15 | 6 |
| Adult (∼18+ y) | 45 | 19 |
| Unspecified | 1 | 1 |
| DBM terminology | ||
| Double burden | 114 | 48 |
| Dual burden | 54 | 23 |
| Both double and dual burden | 29 | 12 |
| Coexistence | 21 | 9 |
| Other term4 | 5 | 2 |
| Unspecified | 16 | 7 |
DBM, double burden of malnutrition; RCT, randomized controlled trial.
Age groups of study participants are categorized by approximation according to how the original article defined the study population, i.e., the school-age children group can extend to age 13 or 14 y, and adolescence can begin at age 10 or 11 y.
“Multiple” age groups is defined as combinations of ≥2 of the predefined age groups, such as adults and preschool age children.
Other terms for DBM identified were: “simultaneous,” “concomitant,” “concurrent,” “overlap,” “twin burden,” and “triple burden.”
FIGURE 3.
Major dimensions and research settings of the double burden of malnutrition (DBM) reported in 239 articles assessing DBM1. 1Many articles included multiple definitions of DBM; circle diameter is proportional to the number of articles in which the DBM characteristic was observed. 2Forms of malnutrition, level of assessment, and target population subgroups were classified per the original article's definition, indicator, and/or cutoff value (e.g., overweight/obesity was classified by the specified BMI range, and anemia was classified by the specified hemoglobin concentration). 3“Other” forms of malnutrition included: OW/OB paired with stunting and/or wasting; OW/OB paired with “chronic energy deficiency”; low HDL cholesterol paired with underweight; metabolic syndrome (MetS) paired with anemia; cardiometabolic risk factors (CMRFs; i.e., dyslipidemia, hyperglycemia, hypertension, abdominal obesity, and/or OW/OB) paired with underweight or micronutrient deficiencies; CMRFs or MetS paired with anemia, iron depletion, or vitamin A deficiency; macrosomia paired with low birth weight; OW/OB paired with low upper-arm circumference or low triceps skinfold measurements; and OW/OB paired with food insecurity. 4World Bank classifications (27). DBM; double burden of malnutrition; MN, micronutrient; OW/OB, overweight/obesity; PSC, preschool age children; TWU, thinness/wasting/underweight; WRA, women of reproductive age.
Dimensions of DBM and frequency of use
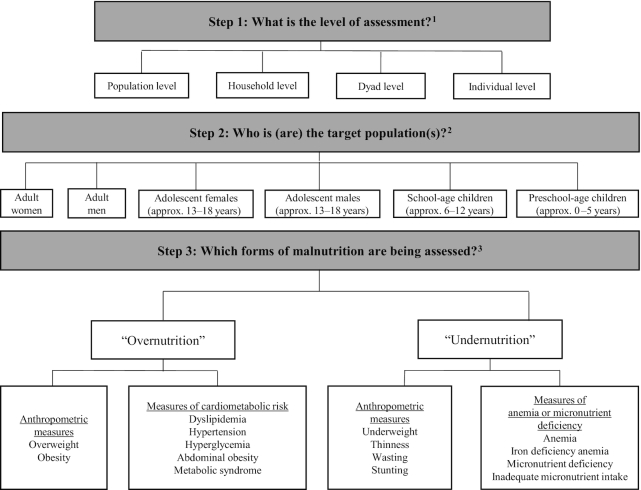
We identified 3 salient dimensions of DBM operational definitions used in the literature: level of assessment, target population, and form of malnutrition. We organized these dimensions into a framework for building operational definitions of DBM that can be used as a starting point in the planning of DBM surveillance and evaluation of interventions (Figure 4). DBM was most frequently assessed at the population level (identified in n = 214 articles, 90%), followed by the individual (n = 35, 15%), dyad (n = 22, 9%), and household levels (n = 17, 7%). Articles varied with regard to the selected target population for assessment; articles assessing DBM in populations of mixed ages, that is, any combination of adults, adolescents, and children, were the most frequently occurring (n = 156, 65%) (Figure 3).
FIGURE 4.
Framework for building operational definitions of the double burden of malnutrition (DBM) based on definitions observed in published literature. The framework for building operational definitions of the DBM can be used by analysts, program planners, and policymakers to determine the specific operational definition of DBM that meets their objective(s). The 3 dimensions of the operational definition (level of assessment, target population, and forms of malnutrition to assess) should be chosen with consideration of the country context and public health priorities, and include the purposeful selection of indicators fit to the purpose of the objective(s). 1Population-level assessment refers to comparisons of national, regional, and subregional populations or smaller populations, such as a population of students within a school or a population of adult women within a community. Household-level assessment refers to comparisons among or across households of all or some specified household members. Dyad-level assessment refers to comparisons among or across mother-child pairs or caregiver-child pairs. Individual-level assessment refers to comparisons of different forms of malnutrition occurring within a single individual. 2Assessment of the target population can include ≥1 age groups. 3Widely used definitions of DBM assess the coexistence of 1 form of “overnutrition” and 1 form of “undernutrition.” This framework can be expanded to assess multiple forms of malnutrition, for example, when assessing a triple burden of malnutrition. Additional forms of “overnutrition” identified in our review included macrosomia. Additional forms of “undernutrition” identified in our review included chronic energy deficiency, low birth weight, low upper-arm circumference, low triceps skinfold measurement, and food insecurity.
The most frequently occurring form of malnutrition was OW/OB paired with assessments of thinness/wasting/underweight (TWU) (identified in n = 185 articles, 77%). Following this, assessments of OW/OB and stunting were frequently reported (n = 103, 43%), as were OW/OB and anemia (n = 34, 14%, with n = 7 assessing iron deficiency anemia), OW/OB and ≥1 micronutrient deficiencies (n = 23, 10%), and “other” coexisting forms of malnutrition (n = 17, 7%) (Figure 3).
Forms of malnutrition were classified as “other” if they appeared in ≤7 articles and included: OW/OB paired with stunting and/or wasting (n = 7) (31–37); OW/OB paired with “chronic energy deficiency” (n = 3) (38–40); low HDL cholesterol paired with underweight (n = 1) (41); metabolic syndrome (MetS) paired with anemia (n = 1) (42); cardiometabolic risk factors (CMRFs; i.e., dyslipidemia, hyperglycemia, hypertension, abdominal obesity, and/or OW/OB) paired with underweight or micronutrient deficiencies (n = 1) (43); CMRFs or MetS paired with anemia, iron depletion, or vitamin A deficiency (n = 1) (44); macrosomia paired with low birth weight (n = 1) (45); OW/OB paired with low upper-arm circumference or low triceps skinfold measurements (n = 1) (46); and OW/OB paired with food insecurity (n = 1) (Figure 3) (47).
Specific forms of malnutrition in DBM by level of assessment
Within the 239 included articles in this review, there were 623 total occurrences of specific operational definitions of DBM (Table 2). At the population level, the most frequently occurring forms of malnutrition included in the definition were coexisting OW/OB and TWU (n = 261 occurrences, 42%) and OW/OB and stunting (n = 110 occurrences, 17%). At the individual level, the combinations of OW/OB and stunting, anemia, or micronutrient deficiency occurred at a similar frequency (4%, 4%, and 3% of occurrences, respectively). DBM assessed at the household or dyad levels was less common; in these cases, women of reproductive age and preschool age children were typically targeted. Supplemental Table 2 details the frequency of occurrence of specific operational definitions of DBM by both level of assessment and target population.
TABLE 2.
Frequency of occurrence (n = 623) of forms of malnutrition characterizing the double burden of malnutrition by level of assessment1
| Level of assessment | |||||
|---|---|---|---|---|---|
| Form of malnutrition | Total | Population | Household | Dyad | Individual |
| Coexisting OW/OB and TWU | 289 (46) | 261 (42) | 7 (1) | 21 (3) | n/a |
| OW/OB and stunting | 161 (26) | 110 (17) | 10 (2) | 17 (3) | 24 (4) |
| OW/OB and anemia | 74 (12) | 48 (8) | 1 (<1) | 0 (0) | 25 (4) |
| OW/OB and MN deficiency | 73 (12) | 55 (9) | 1 (<1) | 0 (0) | 17 (3) |
| Other2 | 26 (4) | 13 (2) | 1 (<1) | 1 (<1) | 11 (2) |
| Total | 623 (100) | 487 (78) | 20 (3) | 39 (6) | 77 (13) |
Total values presented as n (%) where n = 623, or the total number of occurrences of all DBM operational definitions identified within the 239 included articles. DBM, double burden of malnutrition; MN, micronutrient; n/a, not applicable; OW/OB, overweight/obesity; TWU, thinness/wasting/underweight.
“Other” operational DBM definitions included: OW/OB paired with stunting and/or wasting; OW/OB paired with “chronic energy deficiency”; low HDL cholesterol paired with underweight; metabolic syndrome (MetS) paired with anemia; cardiometabolic risk factors (CMRFs; i.e., dyslipidemia, hyperglycemia, hypertension, abdominal obesity, and/or OW/OB) paired with underweight or micronutrient deficiencies; CMRFs or MetS paired with anemia, iron depletion, or vitamin A deficiency; macrosomia paired with low birth weight; OW/OB paired with low upper-arm circumference or low triceps skinfold measurements; and OW/OB paired with food insecurity.
Anthropometric indicators used to asses DBM
Because assessment of DBM was most frequently carried out through anthropometric measurements of OW/OB or underweight, wasting, thinness, and stunting, we examined the specific indicators and cutoffs used for these measures (Tables 3 and 4). WHO growth standards and cutoffs were the primary source cited to classify the anthropometric measurements (48), with exceptions for National Center for Health Statistics/CDC reference values for overweight BMI-for-age percentiles (n = 12 articles), and the International Obesity Task Force (IOTF) BMI classifications for thinness (n = 7) (49, 50). Just under one-quarter of adult BMI classifications for OW/OB were based on IOTF cutoffs. BMI standards for Asian populations were referenced in 36 of 54 total articles assessing BMI in Asian populations. Only 3 articles used indicators other than anthropometrics to assess the “overnutrition” component of DBM. One examined anemia in the presence of MetS (42), and 2 examined micronutrient deficiencies and the presence of ≥1 CMRFs and/or MetS (43, 44).
TABLE 3.
Anthropometric indicators and sources of reference values for assessing overweight/obesity or noncommunicable disease risk from 239 articles assessing the double burden of malnutrition in adults and children1
| Anthropometric | Source | Number of articles |
|---|---|---|
| indicator | (refs 48–50) | n (%) |
| BMI | 162 (68) | |
| WHO | 103 | |
| NCHS/CDC | 2 | |
| IOTF | 23 | |
| Other2 or unspecified | 34 | |
| BMI-for-age z-score | 86 (36) | |
| WHO | 73 | |
| NCHS/CDC | 2 | |
| IOTF | 4 | |
| Other or unspecified | 7 | |
| BMI-for-age percentile | 29 (13) | |
| WHO | 10 | |
| NCHS/CDC | 12 | |
| IOTF | 2 | |
| Other or unspecified | 5 | |
| Waist circumference | 8 (3) | |
| WHO | 3 | |
| Other or unspecified | 5 | |
| Waist-to-hip ratio | 6 (3) | |
| WHO | 1 | |
| Other or unspecified | 5 |
Some articles presented multiple indicators of overweight/obesity so percentage total is greater than 100. IOTF, International Obesity Task Force; NCHS/CDC, National Center for Health Statistics/CDC.
Sources were classified as “other” if they were sourced from uncommon literature sources, such as citing a single article for country-specific cutoff values for BMI.
TABLE 4.
Common anthropometric indicators of underweight, stunting, thinness, and wasting, and sources of reference values from 239 articles assessing the double burden of malnutrition in adults and children1
| Anthropometric category | Source | Number of articles |
|---|---|---|
| and indicator | (refs 48–50) | n (%) |
| Underweight | 181 (76) | |
| BMI | 93 | |
| WHO | 65 | |
| IOTF | 9 | |
| Other2 or unspecified | 19 | |
| BMI-for-age z-score | 65 | |
| WHO | 54 | |
| NCHS/CDC | 3 | |
| Other or unspecified | 8 | |
| BMI-for-age percentile | 16 | |
| WHO | 6 | |
| NCHS/CDC | 4 | |
| Other or unspecified | 6 | |
| Other or unspecified3 | 7 | |
| Stunting | 111 (46) | |
| Length/height-for-age z-score | 102 | |
| WHO | 85 | |
| NCHS/CDC | 4 | |
| Other or unspecified | 13 | |
| Length/height-for-age percentiles | 4 | |
| NCHS/CDC | 2 | |
| Other or unspecified | 2 | |
| Short stature (cm) | 4 | |
| Other or unspecified | 3 | |
| Multiple (z-score and percentile) | 1 | |
| WHO and NCHS/CDC | 1 | |
| Wasting | 37 (15) | |
| Weight-for-height z-score | 33 | |
| WHO | 26 | |
| NCHS/CDC | 2 | |
| Other or unspecified | 5 | |
| Other or unspecified4 | 4 | |
| Thinness | 30 (13) | |
| BMI | 11 | |
| WHO | 2 | |
| IOTF | 7 | |
| Other or unspecified | 2 | |
| BMI-for-age z-score | 15 | |
| WHO | 12 | |
| IOTF | 1 | |
| Other or unspecified | 2 | |
| BMI-for-age percentile | 2 | |
| WHO | 1 | |
| Other or unspecified | 1 | |
| Multiple (z-score and percentile) | 2 |
Some articles presented multiple “undernutrition” indicators so percentage total is greater than 100. IOTF, International Obesity Task Force; NCHS/CDC, National Center for Health Statistics/CDC.
Sources were classified as “other” if they were sourced from uncommon literature sources, such as citing an individual article for country-specific cutoff values for underweight.
3Underweight indicators classified as “other” included measurements of low birthweight or combinations of multiple indicators.
Wasting indicators classified as “other” included measurements of body fat or muscle mass, or combinations of multiple indicators.
Anemia and micronutrient indicators used to assess DBM
A total of 34 of the 239 included articles (14%) assessed DBM as OW/OB paired with anemia, with 7 of the articles assessing iron deficiency anemia specifically. One additional article (42) defined DBM as coexisting MetS and anemia. Most articles (n = 27) cited WHO anemia cutoff values based on age, sex, and physiological status. OW/OB paired with ≥1 micronutrient deficiencies was assessed in 23 articles (10%), and 2 additional articles (43, 44) defined DBM as the presence of ≥1 CMRFs and ≥1 micronutrient deficiencies. Iron status was assessed in 23 of the articles, 13 of which measured iron status with serum ferritin, with the remaining articles measuring iron status using transferrin saturation, soluble transferrin receptor concentration, serum iron, or combinations of these indicators. WHO cutoff values for iron deficiency were referenced in 12 articles. Other reported micronutrient deficiencies included vitamin A (n = 14, 5% of articles), zinc (n = 7, 3%), vitamin D (n = 6, 3%), vitamin B-12 (n = 3, 1%), folate (n = 2, 1%), copper (n = 1, 0.5%), and selenium (n = 1, 0.5%), with most articles relying on biomarker cutoffs to define deficiency, but 1 article presenting inadequate dietary intake of the micronutrient (51) (Supplemental Table 3).
Reported DBM prevalence at the household, dyad, and individual levels
We noted a wide variation in reported DBM prevalence at the household, dyad, and individual levels (Table 5). At the individual level, median prevalence for OW/OB and stunting was 5.2% (n = 25 articles) and 28.4% (n = 28) for OW/OB and micronutrient deficiency, whereas reported prevalence for both these forms of malnutrition within single articles ranged from 1% to >60%. Particularly wide ranges in prevalence were reported for coexisting OW/OB and stunting at the dyad and individual levels (0.4–79.8%, n = 17, and 0.1–68.4%, n = 25, respectively), and OW/OB and micronutrient deficiency at the individual level (1.0–94.0%, n = 21).
TABLE 5.
Median (range) reported prevalence of the double burden of malnutrition by form of malnutrition and level of assessment1
| Level of assessment | ||||||
|---|---|---|---|---|---|---|
| Form of malnutrition | Household | n | Dyad | n | Individual | n |
| Coexisting OW/OB and TWU | 15.2 (6.2–24.7) | 10 | 15.6 (0.2–38.6) | 16 | n/a | |
| OW/OB and stunting | 11.8 (2.6–30.6) | 9 | 6.3 (0.4–79.8) | 17 | 5.2 (0.1–68.4) | 25 |
| OW/OB and anemia | 12.6 | 1 | — | 0 | 9.7 (0.7–67.0) | 25 |
| OW/OB and MN deficiency | 14.0 | 1 | — | 0 | 28.4 (1.0–94.0) | 21 |
| Other2 | 16.2 | 1 | 20.0 | 1 | 5.6 (1.2–76.4) | 14 |
Values presented as median (range) of prevalence estimates; n = number of articles. Population-level data are not presented because each data point consists of multiple prevalence estimates making the data difficult to summarize. MN, micronutrient; OW/OB, overweight/obesity; TWU, thinness/wasting/underweight.
“Other” operational double burden of malnutrition definitions included: OW/OB paired with stunting and/or wasting; cardiometabolic risk factors paired with underweight, anemia, or micronutrient deficiencies; and OW/OB paired with food insecurity.
Sensitivity analysis by article primary objective
We identified articles in which the primary objective was specifically to assess DBM (n = 134 articles, 56%) and those with a different primary objective (n = 87, 36%); in an additional 8% of articles (n = 18), the distinction was unclear. In our sensitivity analysis to explore if definitions of DBM differed according to the primary objective of the article, we found that the distributions of the forms of malnutrition by level of assessment and target population were similar when compared with the full set of articles. Of note, all articles assessing OW/OB and anemia or micronutrient deficiencies at the individual level were articles in which the main objective was to assess DBM. Supplemental Tables 4 and 5 detail the frequency of occurrence of DBM operational definitions in the 134 articles whose primary objective was to assess DBM, by level of assessment and by target population, respectively.
Discussion
Rapid changes to global food systems and increasing urbanization have created a world where multiple forms of malnutrition, ranging from wasting and micronutrient deficiencies to obesity and diet-related NCDs, coexist in populations, households, and individuals. Efforts to characterize the resulting nutrition situation have employed various definitions of DBM. In this systematic review, we have summarized the frequency of occurrence of different operational definitions of DBM in articles reporting DBM prevalence, and identified 3 dimensions of DBM definitions: 1) the level of assessment (i.e., population, dyad, household, or individual); 2) the target population assessed; and 3) the forms of malnutrition measured (i.e., OW/OB, TWU, stunting, anemia, and micronutrient deficiencies). Together, these 3 dimensions form a framework for building operational definitions of DBM that can be applied in nutrition assessment and surveillance, and for the planning and evaluation of nutrition policies and programs, including double dutyinterventions [interventions that aim simultaneously to address multiple forms of malnutrition (52)]. This framework could be further adapted to capture exposure of an individual to multiple forms of malnutrition across the life course, an additional dimension of DBM not covered in this review.
In the studies reviewed, we observed that DBM was most commonly assessed at the population level using anthropometric indicators of OW/OB and TWU. A much smaller proportion of articles assessed the overlap of OW/OB with stunting, anemia, or micronutrient deficiencies. Only 4 articles specifically assessed biochemical indicators of cardiometabolic risk, despite the growing global prevalence of NCDs (53). We found great heterogeneity among age groups and target populations assessed; most articles focused on populations of mixed ages and sexes, and whereas several focused on just women or just children, no articles focused solely on men. The implications of these gaps in DBM assessment are discussed below.
The varied definitions of DBM uncovered in our review point to a need for more comprehensive terminology to describe the global nutrition situation. Although there is general consensus that the nutrition transition has resulted in coexisting under- and overnutrition in low- and middle-income countries (LMIC) (1), we suggest that the term double burden of malnutrition is problematic because it evokes a linear continuum of undernutrition to overnutrition, implying that malnutrition can be reduced to “too little” or “too much.” This narrow conceptualization is inadequate to reflect the complex and evolving ways in which homeostasis can be perturbed by nutritional exposures, or how these exposures are expressed phenotypically as malnutrition. In the 2013 Sight and Life report, Provo (54) suggested “dropping the double” from DBM to allow for better coordination of interventions addressing all forms of malnutrition, and Delisle (55) proposed the term “double burden of dysnutrition” to emphasize a synergistic and cumulative relation. A need for more inclusive terminology is further exemplified by usage of the term “triple burden of malnutrition,” though using this term might contribute to confusion if the 3 burdens are not clearly defined. For example, the “triple burden” previously described coexisting communicable disease, NCD, and underweight (6); however, recent literature defines it as coexisting OW/OB, underweight or stunting, and micronutrient deficiencies (56,57). Although we retained the term DBM for this review due to its common usage, including by WHO and the recent DBM series in The Lancet (1, 7–10), we share this perspective on the need for updated terminology that reflects malnutrition's multiple possible phenotypes. Our proposed framework for building operational DBM definitions could assist in advancing the conceptualization of DBM; this framework can be further adapted to enhance our measurement and understanding of the evolving global nutrition situation.
Given the many possible phenotypes of malnutrition, the intentional selection of indicators specifically fit to the purpose of the measurement is of critical importance. In our review, the majority of articles leveraged existing data from representative surveys assessing DBM with standard anthropometric indicators. Although this approach has its advantages, available data might not always be best suited to address specific programmatic or research needs. As discussed by Habicht and Pelletier (58) and Habicht and Stoltzfus (59), nutrition indicators should be chosen based on prespecified criteria that unambiguously reflect the objectives. In the context of DBM, when selecting an indicator, analysts should consider if the objective is to establish the prevalence of DBM, monitor DBM trends over time, test an intervention, or evaluate a program or policy's effectiveness. For example, data to estimate the prevalence of overweight (elevated BMI) and anemia are widely available and useful for monitoring trends over time and comparing across countries, but more specific measures, such as blood pressure, glycated hemoglobin, or micronutrient biomarkers, can be more appropriate for assessing the impact of novel interventions on individual and population health outcomes. Additionally, it might be necessary to consider if the selected indicators measure DBM components that can be impacted by nutrition interventions alone, or if their multifactorial etiology requires additional inputs. For example, both anemia and stunting are considered global nutrition targets, but are unlikely to be resolved solely by nutrition-specific interventions (23, 60, 61). In both programmatic and research settings, a suite of fit-for-purpose indicators might need to be employed in DBM assessment.
For the purpose of guiding formulation of policies and programs to address DBM, efforts are needed to monitor its prevalence and trends. As global monitoring reports provide estimates of DBM prevalence useful for assessing progress on meeting global health targets (13, 62, 63), how these reports define and report DBM can subsequently shape where and how DBM is then addressed through programming and interventions. Importantly, the reported prevalence of DBM will vary depending on the definition used (24, 64, 65). In this review, the estimates of DBM prevalence are difficult to interpret because the data come from different studies and varying target populations; however, other studies have reported differences in DBM prevalence with different operational definitions using the same study population (66, 67). For example, recent analyses of population-level survey data from multiple countries found that median individual-level DBM prevalence was 8.6% compared with 21.9% when anemia compared with micronutrient deficiency was applied as the undernutrition component of DBM (66). Thus, the selection of a particular DBM definition can determine whether DBM is perceived to be a problem in a given population, and tracking the prevalence of DBM using several definitions can give a more complete picture of the nutrition situation. Additionally, the forms of malnutrition selected to represent DBM will drive decisions about which interventions to pursue. Although there is some overlap, the list of commonly available interventions likely differs if the goal is to reduce wasting compared with stunting, or to address obesity in children compared with adults. The coordination of DBM definition selection with the priorities expressed in national nutrition strategies can facilitate the linkages between DBM surveillance, effective interventions, and optimal use of resources.
Shrimpton et al. (68) highlighted the research implications of selecting a suite of fit-for-purpose indicators in a study assessing the prevalence of NCDs in Chinese adults. In this population, increased waist circumference tends to be a better measure of diabetes risk whereas risk of hypertension is associated with higher BMI; thus, a combination of the 2 indicators can best capture a true picture of NCD risk in Chinese adults (68). Also, women tend to have higher prevalence of OW/OB when compared with men; however, men tend to have higher prevalence of elevated fasting plasma glucose and hypertension (69). If both groups are included in an assessment of NCD risk, including both biochemical and anthropometric indicators can provide the most insight into population risk. These examples illustrate that the construction of DBM operational definitions and the selection of indicators for subsequent DBM assessment should be informed by the context of the research and should be clearly linked to the research objectives (58, 59). Use of the proposed framework for building DBM operational definitions can assist in clarifying this process.
With these considerations in mind, we identified 3 important gaps in DBM assessment: research using specific measures of NCD risk; inclusion of micronutrient deficiencies and anemia as forms of undernutrition; and expansion of the target groups assessed. First, in the literature reviewed, “overnutrition” was overwhelmingly measured with BMI, despite the limitations of BMI as an indicator of metabolic health (23, 61). Whereas many articles discussed the growing prevalence of NCDs alongside persistent undernutrition, only 4 articles explicitly assessed biochemical indicators of cardiometabolic risk in their assessments of DBM. Anthropometric indicators, such as BMI and waist circumference, can be sufficient for establishing a population's risk of NCDs, such as risk of diabetes (70). However, if the objective of the research is to decrease morbidity or mortality in a population suffering from NCDs, it is important to measure the indicator directly when feasible, such as measuring arterial blood pressure, fasting plasma glucose, or cholesterol concentrations, along with anthropometric indicators, to assess morbidity due to MetS (71). Inclusion of these measures in Demographic and Health Surveys (72) and WHO NCD risk factor surveillance surveys (73) is an encouraging sign of the feasibility of this approach.
A second important gap in DBM research, which was also largely excluded from the recent Lancet series (1,7), is the coexistence of micronutrient deficiencies and/or anemias with OW/OB or NCDs. Only one-quarter of the articles included in our review assessed anemia or biochemical indicators of micronutrient deficiency in the context of DBM; of these, most focused on anemia. This might be in part because of limited data on micronutrient deficiency prevalence (74), particularly in LMIC, despite being considered a public health priority due to the critical role of micronutrients in health (75, 76). Such data are needed to understand the relations of coexisting micronutrient deficiencies and anemias with OW/OB and other NCDs. Some studies report that overweight and obese individuals can be at higher risk of developing micronutrient deficiencies or anemia (77–80); other studies have found negative relations, indicating that different individuals are affected (66, 67). Further research is required to clarify whether specific micronutrient deficiencies are more prevalent in those with NCDs, which in turn requires addressing new questions around measurement of DBM: Do we need to construct a separate operational definition of DBM for each micronutrient, or can deficiencies be combined into a satisfactory index? Should we weight certain deficiencies as more important, for example, based on greater prevalence or severity of deficiency consequences? To answer these questions more data on micronutrient deficiencies and anemias in countries are urgently needed, as is more research to understand the etiology of coexisting micronutrient deficiencies, anemias, and OW/OB.
Third, no articles in our review specifically targeted men in DBM assessments, and few articles specifically targeted adolescents (n = 15). The lack of representation of these groups in DBM data could bias conclusions regarding DBM prevalence. Although women and young children are more vulnerable to many forms of malnutrition and have therefore been the primary targets of nutrition programs in LMIC, adolescence is a critical life stage to impact lifelong health and the health of future generations, and others have called for more emphasis on DBM research in this age group (81). Additionally, whereas undernutrition research in LMIC has traditionally focused on women and young children, men should not be ignored in efforts to address obesity and NCDs globally. NCDs are the largest contributor to the global premature mortality rate (82). Because men make up approximately half of the world's adult population, data on their DBM status is important for interventions and policies aimed at DBM prevention. Finally, in many contexts men have greater household decision-making power than women, which can impact nutritional status among other household members (83). Including men in DBM assessment is therefore important for the success of DBM interventions overall, and including those aimed at children, women of reproductive age, and adolescents.
Limitations of this analysis are that the original literature search was limited to 2 databases (PubMed and Scopus) and was conducted in July 2017, thus excluding articles published after that time or in other databases. However, a qualitative examination of articles published since that date and identified by applying the same search terms suggested that inclusion of more recent studies was unlikely to result in major shifts in characterization of the most common DBM operational definitions. Additionally, although there could be some subjectivity involved in interpreting the inclusion criteria, we limited the influence of potential subjectivity by screening articles in duplicate and holding weekly discussions among the research team to standardize screening and data extraction. We also conducted a sensitivity analysis limited to articles in which the assessment of DBM was clearly reported as the primary study aim, and confirmed that general trends in how DBM is defined in the literature still remained. Finally, the protocol for this review focused on identifying studies that assessed DBM in cross-sectional analyses, that is, coexisting “undernutrition” and “overnutrition” at the same point in time. Our review does not address the concept of “intraindividual DBM,” that is, exposure of an individual to multiple forms of malnutrition over the life course (7). However, because global monitoring reports and many research activities focus on cross-sectional data, our objective was to clarify the use of operational definitions of “concurrent DBM” for assessment, surveillance, and evaluation of the effects of interventions and programs. Despite these limitations, we believe this review offers a reasonable depiction of how concurrent DBM is conceptualized in the literature. A similar examination of prospective cohort studies could help characterize specific indicators of “life course DBM.”
In conclusion, there is growing global consensus that the presence of coexisting multiple forms of malnutrition deserves urgent attention and will require novel approaches to nutrition policy and programming. In this systematic review, we identified 3 dimensions of DBM operational definitions (level of assessment, target population, and form of malnutrition), and proposed a framework for building operational definitions of DBM. We found that studies of DBM prevalence most commonly reported coexistence of anthropometric measures of undernutrition and overnutrition at the population level in mixed population groups. Other forms of malnutrition, such as diet-related NCDs and micronutrient deficiencies, and coexistence of multiple forms of malnutrition at the individual or household level, have received relatively little attention as components of DBM. Efforts to address DBM will require consideration of which forms of malnutrition and which population groups constitute the greatest context-specific public health priorities, and will require operational definitions that capture the desired purpose of the assessment. Characterization of DBM with clear and specific operational definitions will allow for better comparability of DBM data across populations and over time, and will improve future surveillance efforts, intervention implementation and evaluation, and program and policy development.
Supplementary Material
ACKNOWLEDGEMENTS
We gratefully acknowledge the time and effort contributed by our research interns who performed abstract and full-text screening and/or data extraction: Callie Austin, Jordan Balletto, Emily Becher, Katie Lei, Kezia Monoarfa Tan, Celina Morales, and Anran Shao. Statistician Charles Arnold provided technical support.
The authors’ responsibilities were as follows—JND, BMO, and RE-S: designed and conducted the research; JND: analyzed the data and wrote the first draft of the manuscript; RE-S: had primary responsibility for final content; and all authors: critically reviewed, edited, read, and approved the final manuscript.
Notes
This research was supported by the USDA National Institute of Food and Agriculture Hatch Project 1013897.
Author disclosures: The authors report no conflicts of interest.
Supplemental Methods and Supplemental Tables 1–5 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Abbreviations used: CMRF, cardiometabolic risk factor; DBM, double burden of malnutrition; IOTF, International Obesity Task Force; LMIC, low- and middle-income countries; MetS, metabolic syndrome; MN, micronutrient; NCD, noncommunicable disease; NCHS, National Center for Health Statistics; OW/OB, overweight/obesity; TWU, thinness/wasting/underweight.
Contributor Information
Jennie N Davis, Institute for Global Nutrition, Department of Nutrition, University of California, Davis, Davis, CA, USA.
Brietta M Oaks, Department of Nutrition and Food Sciences, University of Rhode Island, Kingston, RI, USA.
Reina Engle-Stone, Email: renglestone@ucdavis.edu, Institute for Global Nutrition, Department of Nutrition, University of California, Davis, Davis, CA, USA.
References
- 1. Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2019;395(10217):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shrimpton R, Rokx C. The double burden of malnutrition: a review of global evidence. Washington (DC): The World Bank; 2012.. pp. 1–74.. Health Nutrition and Population Discussion Paper. Report no. 79525. [Google Scholar]
- 3. Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: a critical review. Food Nutr Bull. 2014;35(2):230–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr. 2000;130(12):2965–71. [DOI] [PubMed] [Google Scholar]
- 5. Garrett JL, Ruel MT. Stunted child–overweight mother pairs: prevalence and association with economic development and urbanization. Food Nutr Bull. 2005;26(2):209–21. [DOI] [PubMed] [Google Scholar]
- 6. Gillespie S, Haddad L. Attacking the double burden of malnutrition in Asia and the Pacific. Manila (Philippines): Asian Development Bank; 2001. ADB Nutrition and Development Series No. 4. [Google Scholar]
- 7. Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2019;395(10217):75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2019;395(10218):142–55. [DOI] [PubMed] [Google Scholar]
- 9. Nugent R, Levin C, Hale J, Hutchinson B. Economic effects of the double burden of malnutrition. Lancet. 2019;395(10218):156–64. [DOI] [PubMed] [Google Scholar]
- 10. World Health Organization The double burden of malnutrition: policy brief. [Internet] Geneva: World Health Organization; 2017.; [cited 2019 July 21]. Available from: http://www.who.int/nutrition/publications/doubleburdenmalnutrition-policybrief/en/. [Google Scholar]
- 11. NCD Risk Factor Collaboration (NCD RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prentice AM. The double burden of malnutrition in countries passing through the economic transition. Ann Nutr Metab. 2018;72(3):47–54. [DOI] [PubMed] [Google Scholar]
- 13. FAO, IFAD, UNICEF, WFP and WHO The state of food security and nutrition in the world 2019. Safeguarding against economic slowdowns and downturns. [Internet] Rome: FAO; 2019. [cited 2019 July 19]. Available from: https://data.unicef.org/resources/sofi-2019/. [Google Scholar]
- 14. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Popkin BM. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr Rev. 2017;75(2):73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jaacks LM, Slining MM, Popkin BP. Recent underweight and overweight trends by rural-urban residence among women in low- and middle-income countries. J Nutr. 2015;145(2):352–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jaacks LM, Slining MM, Popkin BM. Recent trends in the prevalence of under- and overweight among adolescent girls in low- and middle-income countries. Pediatr Obes. 2015;10(6):428–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Min J, Zhao Y, Slivka L, Wang Y. Double burden of diseases worldwide: coexistence of undernutrition and overnutrition-related non-communicable chronic diseases. Obes Rev. 2018;19(1):49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abdullah A. The double burden of undernutrition and overnutrition in developing countries: an update. Curr Obes Rep. 2015;4(3):337–49. [DOI] [PubMed] [Google Scholar]
- 20. Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes. 2005;29(1):129–36. [DOI] [PubMed] [Google Scholar]
- 21. Rivera JA, Pedraza LS, Martorell R, Gil A. Introduction to the double burden of undernutrition and excess weight in Latin America. Am J Clin Nutr. 2014;100(6):1613S–6S. [DOI] [PubMed] [Google Scholar]
- 22. Varela-Silva MI, Dickinson F, Wilson HJ, Azcorra H, Griffiths P, Bogin B. The nutritional dual-burden in developing countries – how is it assessed and what are the health implications?. Coll Antropol. 2012;36(1):39–45. [PubMed] [Google Scholar]
- 23. Leroy JL, Frongillo EA. Perspective: what does stunting really mean? A critical review of the evidence. Adv Nutr. 2019;10(2):196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bates K, Gjonca A, Leone T. Double burden or double counting of child malnutrition? The methodological and theoretical implications of stuntingoverweight in low and middle income countries. J Epidemiol Community Health. 2017;71(8):779–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch VA. Cochrane handbook for systematic reviews of interventions; version 6.0. [Internet] Cochrane Training; 2019 (updated July 2019). Available from: www.training.cochrane.org/handbook. [Google Scholar]
- 26. Food and Agriculture Organization of the United Nations The double burden of malnutrition: case studies from six developing countries. [Internet] Rome: FAO; 2006.; [cited 2020 June 8]. Nutrition Paper. Report no. 84. Available from: http://www.fao.org/3/a0442e/a0442e00.htm. [PubMed] [Google Scholar]
- 27. The World Bank World development indicators – the world by income and region. [Internet]. [cited 2019 July 15]. Available from: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html. [Google Scholar]
- 28. Singh RB, Pella D, Mechirova V, Kartikey K, Demeester F, Tomar RS, Beegom R, Mehta AS, Gupta SB, De AK et al. Prevalence of obesity, physical inactivity and undernutrition, a triple burden of diseases during transition in a developing economy. The five city study group. Acta Cardiol. 2007;62(2):119–27. [DOI] [PubMed] [Google Scholar]
- 29. Kshatriya GK, Acharyae SK. Triple burden of obesity, undernutrition, and cardiovascular disease risk among Indian tribes. PLoS One. 2016;11(1):e0147934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ponce MC, Incani RN, Pinelli E, Kulve N, Ramak R, Polmana K, Doaka CM. Are intestinal parasites fuelling the rise in dual burden households in Venezuela?. Trans R Soc Trop Med Hyg. 2013;107(2):119–23. [DOI] [PubMed] [Google Scholar]
- 31. Armstrong MEG, Lambert MI, Lambert EV. Relationships between different nutritional anthropometric statuses and health-related fitness of South African primary school children. Ann Hum Biol. 2017;44(3):208–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bouzitou GDN, Fayomi B, Delisle H. Child malnutrition and maternal overweight in same households in poor urban areas of Benin. Cah Sante. 2005;15(4):263–70. [PubMed] [Google Scholar]
- 33. Murcia-Moreno NP, Cortés-Osorio V. Double burden of malnutrition in Caldas and an approach to its social determinants. Rev Fac Med. 2016;64(2):239–47. [Google Scholar]
- 34. Wong CY, Zalilah MS, Chua EY, Norhasmah S, Chin YS, Siti Nur'Asyura A. Double-burden of malnutrition among the indigenous peoples (Orang Asli) of Peninsular Malaysia. BMC Public Health. 2015;15:680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang N, Becares L, Chandola T. Patterns and determinants of double-burden of malnutrition among rural children: evidence from China. PLoS One. 2016;11(7):e0158119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. dos Santos FK, Maia JA, Gomes TN, Daca T, Madeira A, Katzmarzyk PT, Prista A. Secular trends in growth and nutritional status of Mozambican school-aged children and adolescents. PLoS One. 2014;9(12):e114068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Khor GL, Sharif ZM. Dual forms of malnutrition in the same households in Malaysia – a case study among Malay rural households. Asia Pac J Clin Nutr. 2003;12(4):427–37. [PubMed] [Google Scholar]
- 38. Pei L, Ren L, Wang D, Yan H. The evaluation of maternal health in rural western China. Ethn Health. 2014;19(3):297–310. [DOI] [PubMed] [Google Scholar]
- 39. Rai RK. Factors associated with nutritional status among adult women in urban India, 1998–2006. Asia Pac J Public Health. 2015;27(2):NP1241–52. [DOI] [PubMed] [Google Scholar]
- 40. Santa Jiménez Acosta C, María Elena Díaz Sánchez C, García Roche RG, Gorbea MB, Ordóñez IW. Changes in the nutritional status of adult Cuban population from different regions of Cuba. Rev Cuba Hig Epidemiol. 2012;50(1):4–13. [Google Scholar]
- 41. Delisle H, Ntandou G, Sodjinou R, Couillard C, Despres JP. At-risk serum cholesterol profile at both ends of the nutrition spectrum in West African adults? The Benin study. Nutrients. 2013;5(4):1366–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jones AD, Hayter AKM, Baker CP, Prabhakaran P, Gupta V, Kulkarni B, Smith GD, Ben-Shlomo Y, Krishna KVR, Kinra S. The co-occurrence of anemia and cardiometabolic disease risk demonstrates sex-specific sociodemographic patterning in an urbanizing rural region of southern India. Eur J Clin Nutr. 2016;70(3):364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zeba AN, Delisle HF, Renier G. Dietary patterns and physical inactivity, two contributing factors to the double burden of malnutrition among adults in Burkina Faso, West Africa. J Nutr Sci. 2014;3:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zeba AN, Delisle HF, Renier G, Savadogo B, Baya B. The double burden of malnutrition and cardiometabolic risk widens the gender and socio-economic health gap: a study among adults in Burkina Faso (West Africa). Public Health Nutr. 2012;15(12):2210–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abubakari A, Kynast-Wolf G, Jahn A. Prevalence of abnormal birth weight and related factors in Northern region, Ghana. BMC Pregnancy Childbirth. 2015;15:335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Houck K, Sorensen MV, Lu F, Alban D, Alvarez K, Hidobro D, Doljanin C, Ona AI. The effects of market integration on childhood growth and nutritional status: the dual burden of under- and over-nutrition in the northern Ecuadorian Amazon. Am J Hum Biol. 2013;25(4):524–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jomaa L, Naja F, Cheaib R, Hwalla N. Household food insecurity is associated with a higher burden of obesity and risk of dietary inadequacies among mothers in Beirut, Lebanon. BMC Public Health. 2017;17(1):567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. World Health Organization Multicentre Growth Reference Study Group WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006.. pp. 1–312. [Google Scholar]
- 49. Kuczmarski R, Ogden C, Guo S. 2000 CDC growth charts for the United States: methods and development. Hyattsville (MD): National Center for Health Statistics; 2002. Vital and Health Statistics. Report no. 11(246). [PubMed] [Google Scholar]
- 50. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Atalah E, Amigo H, Bustos P. Does Chile's nutritional situation constitute a double burden?. Am J Clin Nutr. 2014;100(6):1623S–7S. [DOI] [PubMed] [Google Scholar]
- 52. World Health Organization Double-duty actions for nutrition: policy brief. [Internet] Geneva: World Health Organization; 2017.; [cited 2019 July 21]. Available from: http://www.who.int/nutrition/publications/double-duty-actions-nutrition-policybrief/en/. [Google Scholar]
- 53. Barquera S, Pedroza-Tobias A, Medina C. Cardiovascular diseases in mega-countries: the challenges of the nutrition, physical activity and epidemiologic transitions, and the double burden of disease. Curr Opin Lipidol. 2016;27(4):329–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Provo AM. Towards sustainable nutrition for all: tackling the double burden of malnutrition in Africa. Sight Life. 2013;27(3):40–8. [Google Scholar]
- 55. Delisle HF. Poverty. Ann N Y Acad Sci. 2008;1136(1):172–84. [DOI] [PubMed] [Google Scholar]
- 56. Meenakshi JV. Trends and patterns in the triple burden of malnutrition in India. Agric Econ. 2016;47:S115–34. [Google Scholar]
- 57. Sunuwar DR, Singh DR, Pradhan PMS.Prevalence and factors associated with double and triple burden of malnutrition among mothers and children in Nepal: evidence from 2016 Nepal Demographic and Health Survey. BMC Public Health 2020;20:405. 10.1186/s12889-020-8356-y32223749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Habicht J-P, Pelletier DL. The importance of context in choosing nutritional indicators. J Nutr. 1990;120(S11):1519–24. [DOI] [PubMed] [Google Scholar]
- 59. Habicht JP, Stoltzfus RJ. What do indicators indicate? Am J Clin Nutr. 1997;66(1):190–1. [DOI] [PubMed] [Google Scholar]
- 60. Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann N Y Acad Sci. 2019;1450(1):15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Perumal N, Bassani DG, Roth DE. Use and misuse of stunting as a measure of child health. J Nutr. 2018;148(3):311–5. [DOI] [PubMed] [Google Scholar]
- 62. Shekar M, Popkin B.. Obesity: health and economic consequences of an impending global challenge. Washington (DC): World Bank Group; 2020. [Google Scholar]
- 63. 2020 Global Nutrition Report: action on equity to end malnutrition. Bristol (UK): Development Initiatives; 2020. [Google Scholar]
- 64. Rachmi CN, Agho KE, Li M, Baur LA. Stunting, underweight and overweight in children aged 2.0–4.9 years in Indonesia: prevalence trends and associated risk factors. PLoS One. 2016;11(5):e0154756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kosaka S, Umezaki M. A systematic review of the prevalence and predictors of the double burden of malnutrition within households. Br J Nutr. 2017;117(8):1118–27. [DOI] [PubMed] [Google Scholar]
- 66. Williams AM, Addo OY, Guo J, Ismaily S, Namaste SM, Oaks BM, Rohner F, Suchdev PS, Young MF, Flores-Ayala R et al. Intra-individual double burden of overweight or obesity and micronutrient deficiencies or anemia among women of reproductive age in 17 population-based surveys. Am J Clin Nutr. 2019;112:(Supplement_1):468S–77S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Engle-Stone R, Guo J, Ismaily S, Addo OY, Ahmed T, Oaks BM, Suchdev PS, Flores-Ayala R, Williams AM. Intra-individual double burden of overweight and micronutrient deficiencies or anemia among preschool children. Am J Clin Nutr. 2019;112:(Supplement_1):478S–87S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shrimpton R, Mbuya NV, Provo AM. The double burden of malnutrition in East Asia and the Pacific: evidence and lessons for a multisectoral response. [Internet] Washington (DC): World Bank; 2016.. pp. 1–94.. Health Nutrition and Population Discussion Paper. Available from: http://hdl.handle.net/10986/26102. [Google Scholar]
- 69. GBD 2015 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diab Rep. 2015;15(9):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. International Diabetes Federation The IDF consensus worldwide definition of the metabolic syndrome. [Internet] IDF Communications; 2006. [cited 2019 Nov 8]. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html. [Google Scholar]
- 72. Mitsuaki H, Grover N, Huang C. The measurement of non-communicable diseases in 25 countries with demographic and health surveys. [Internet] Rockville (MD): ICF International; 2015. DHS Occasional Papers no. 10. Available from: https://dhsprogram.com/pubs/pdf/OP10/OP10.pdf. [Google Scholar]
- 73. World Health Organization Noncommunicable diseases country profiles 2018. [Internet] World Health Organization; 2018.; [cited 2020 Feb 1]. Available from: https://www.who.int/publications/i/item/9789241514620. [Google Scholar]
- 74. OpeN-Global: open access knowledge hub of nutritional biomarkers for global health [Internet]. [cited 2020 July 9]. Available from: https://open-global.kcl.ac.uk/.
- 75. Engle-Stone R, Perkins A, Clermont A, Walker N, Haskell MJ, Vosti SA, Haskell MJ, Vosti SA, Brown KH. Estimating lives saved by achieving dietary micronutrient adequacy, with a focus on vitamin A intervention programs in Cameroon. J Nutr. 2017;147(11):2194S–203S. [DOI] [PubMed] [Google Scholar]
- 76. Allen LH, Peerson JM, Olney DK. Provision of multiple rather than two or fewer micronutrients more effectively improves growth and other outcomes in micronutrient-deficient children and adults. J Nutr. 2009;139(5):1022–30. [DOI] [PubMed] [Google Scholar]
- 77. Ganz T, Nemeth E. Hepcidin and iron homeostasis. Biochim Biophys Acta Mol Cell Res. 2012;1823(9):1434–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhao L, Zhang X, Shen Y, Fang X, Wang Y, Wang F. Obesity and iron deficiency: a quantitative meta-analysis. Obes Rev. 2015;16(12):1081–93. [DOI] [PubMed] [Google Scholar]
- 79. García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutr Rev. 2009;67(10):559–72. [DOI] [PubMed] [Google Scholar]
- 80. Zimmermann MB, Zeder C, Muthayya S, Winichagoon P, Chaouki N, Aeberli I, Hurrell RF. Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification. Int J Obes. 2008;32(7):1098–104. [DOI] [PubMed] [Google Scholar]
- 81. Akseer N, Al‐Gashm S, Mehta S, Mokdad A, Bhutta ZA. Global and regional trends in the nutritional status of young people: a critical and neglected age group. Ann N Y Acad Sci. 2017;1393(1):3–20. [DOI] [PubMed] [Google Scholar]
- 82. World Health Organization WHO fact sheet: noncommunicable diseases. [Internet] WHO; 2018.; [cited 2019 Dec 22]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. [Google Scholar]
- 83. Carlson GJ, Kordas K, Murray‐Kolb LE. Associations between women's autonomy and child nutritional status: a review of the literature. Matern Child Nutr. 2015;11(4):452–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.