Abstract
Objective:
To provide a broad overview of the state of drug misuse research, particularly focusing on opioid drug use in the U.S.A.
Design:
An overview of published reviews of the literature.
Results:
Prescription opioid use has increased globally from 2008 to 2013, while use of opiates such as heroin and opium have remained stable in many countries, although, decreases have been observed in parts of Europe. Opioid misuse is highest in the United States; approximately 11.8 million Americans misused opioids in 2016. Demographic, genetic, psychosocial and structural/environmental factors all play a role in determining who will become an opioid misuser. Strategies such as increased prescribing of non-opioid derived pain relievers, expansion of medication treatment, distribution of naloxone for overdose reversal and supervised consumption sites are some of the solutions posed to reduce the spread and consequences of opioid misuse.
Conclusion:
Research focused on understanding of opioid neurobiology, as well as empirically based, effective alternatives to pain management and implementation studies on combined prevention and treatment approaches are needed. It will take the combined effort of community members, healthcare professionals, policymakers and researchers in order to prevent and treat opioid misuse.
Keywords: Drug use, opioids, addiction, substance misuse, intervention, treatment
Definitions of drug and opioid misuse
Consumption of substances to alter mood, manage pain and relieve other mental and physical ailments and symptoms is common and can help persons cope with serious illness. However, some substances that are effective at altering mood, mental and physical states can have the potential to be misused. Misuse can include more frequent use than recommended or prescribed (time between doses or multiple doses at the same time), done to produce a desired or recreational effect. Regular patterns of use to achieve recreational effects may result in unintended consequences including severe impairment, physical and psychological dependence and uncontrolled use or use disorder.
Formally, the DSM-V includes criteria to ascertain whether an individual has any substance use disorders. This criterion is further classified it into mild, moderate or severe to indicate the level of severity, in addition to dividing alcohol and other drugs into their own disorders. Important substances included in the DSM-V are: alcohol, cannabis, hallucinogens, inhalants, opioids (including heroin), sedatives, stimulants and tobacco.
Generally, substance use disorder is determined when the use of the substance causes significant impairment, such as health problems, disability and failure to meet major responsibilities at work, school or home. These problems are usually exhibited by the individual by evidence of impaired control, social impairment, risky use, as well as pharmacological criteria. Using too much/too frequently without being able to stop, cravings, problems in relationships and work stemming from drug use, using in dangerous situations and decreased ability to feel effects/needing a higher dose are some of the main criteria used to identify substance use disorder. Endorsing two or more of eleven criteria, due to recurrent use, is used to diagnose substance use disorder (See Table 1) (American Psychiatric Association, 2013).
Table 1.
Eleven criteria for substance use disorder.
|
Certain drugs have more severe consequences of use than others, can be more addictive, harmful to the body or even lethal. However, legality of a drug does not consistently predict severity of consequences. Marijuana is illegal in many locations and yet is considered more innocuous than many other substances (Gable, 2006). Conversely, some of the most harmful drugs, such as opioids, alcohol and tobacco are legal and used widely in many countries, including the U.S.A. Figure 1 displays the most dangerous drugs, based on plotting the dependence potential of the drug versus the active/lethal dose.
Figure 1.
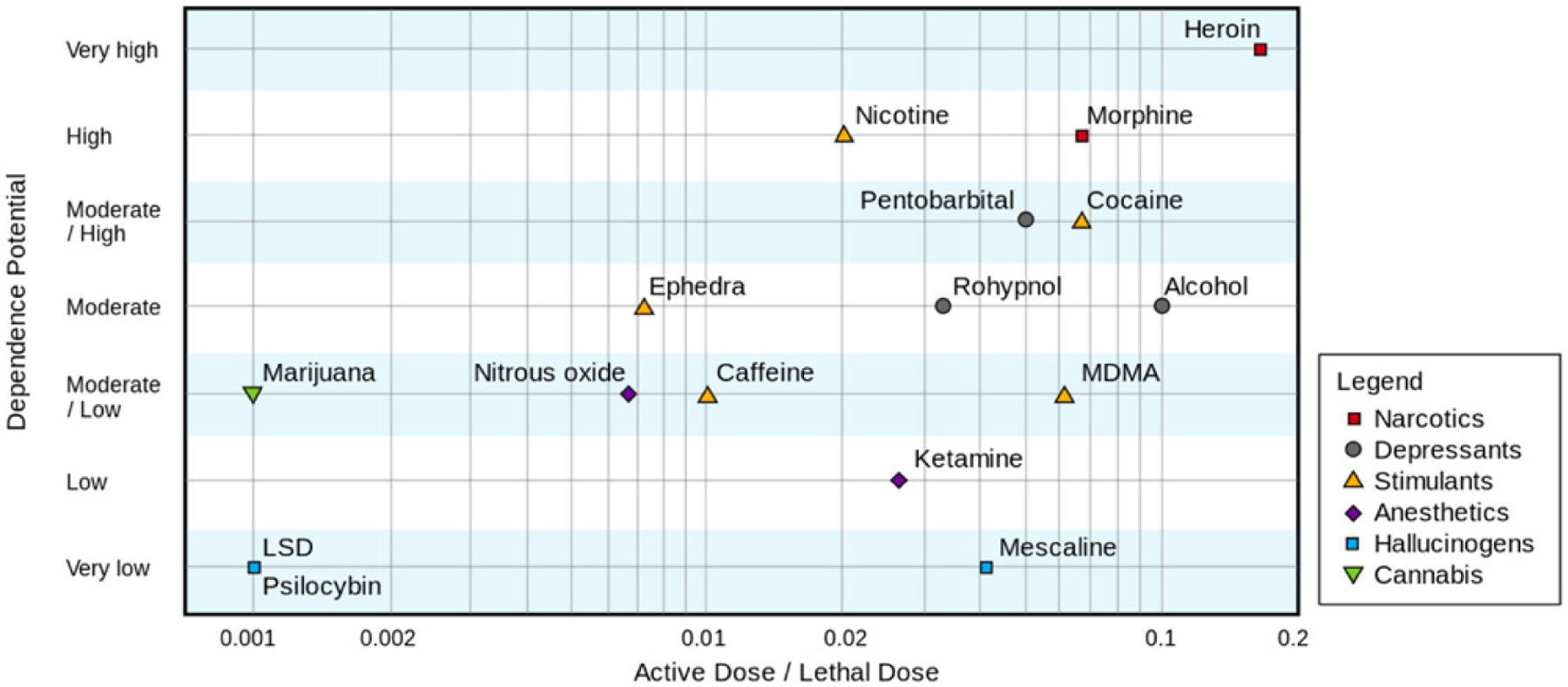
Dependence potential versus active/lethal dose.
Opioid use and the beginning of an epidemic
Prescription opioid use has increased in the U.S.A. and other countries from 2008 to 2013, while use of opiates such as heroin and opium have generally remained stable or even decreased in parts of Europe. Additionally, opioid dependence contributes most of any drugs to the burden of disease, and has increased 74% between 1990 and 2010 globally. In 2014, opioids were responsible for 55% of years of life lost to premature death and 44% of years of life lost through disability (UNODC, 2014). The United States accounts for 99% of the world’s consumption of hydrocodone, 81% of the world’s consumption of oxycodone and 60% of the world’s consumption of hydromorphone (INCB, 2016).
In the United States, the problem with opioids began in the 1990s, when there was increased pressure on doctors to help untreated pain, and to regard pain as the ‘fifth vital sign’ (see: https://www.medpagetoday.com/publichealthpolicy/publichealth/57336; accessed 20 July 2018). Just around that time, Purdue Pharma released a drug named OxyContin (oxycodone) for the treatment of moderate to severe pain, and marketed it heavily to doctors, indicating it was safe and non-addictive (Van Zee, 2009). Sales representatives from the company visited doctors in the U.S.A. and bestowed free gifts upon them, free patient samples, as well as all-expenses paid trips to symposiums for the drug. In 1998, the same company released a video in which a doctor advertised the use of OxyContin for pain, claiming that only 1% of people who take the opioid will become addicted (e.g. being ‘slow release’). The Food and Drug Administration (FDA) has since publicly stated that this claim was unsubstantiated and has cited Purdue for misleading the public.
From 1996 to 2012, sales of OxyContin rose from $48 million to $2.4 billion in the United States (Van Zee, 2009). In addition to unethical and false marketing by pharmaceutical companies, other factors contributed to the rise of opioid over-prescribing. Some of these include a lack of consensus among doctors of appropriate dosing standards and for-profit clinics readily prescribing opioids. Clinicians who are overworked and may want a quick solution to a patient presenting with pain could easily prescribe a pain killer, and have the patient be in and out of the door within minutes. Chronic pain can be hard to definitively diagnose, with no medical test for the general symptom of ‘pain’, with many doctors relying on subjective pain scales and charts to measure a patient’s pain level. Furthermore, prescribing opioids for acute pain, even minor injuries, is common (Delgado et al., 2018). An abundance of unused pills can also lead to drug diversion, which we will discuss further in this review.
This article will examine the antecedents, determinants and consequences of the behaviour of drug use, pivoting this review on one of the most harmful drugs currently affecting the United States and many other countries – opioids. This article aims to: (1) discuss both the positive and negative health impacts of using opioids; (2) discuss the prevalence of opioid use disorder, focusing particularly on rural areas that are hit hardest by prescription pain killers and urban areas where heroin injection is more common; (3) depict a broad description of who uses opioids, and who is likely to be susceptible to misuse, and further harmful trajectories such as injecting behaviour and eventual overdose; (4) examine psychosocial factors that contribute to initiation of opioid use, including personality, social and environmental factors; (5) explore preventive interventions and treatments that have been effective for opioid use disorder, as well as policies and other steps that can be taken to tackle this epidemic on a global level; and (6) consider future directions of research and policy that can be enacted to help curb the development, maintenance and fatality of opioid use.
Classification of and health impact of opioid use
Opiates can be derived from the opium poppy or can be synthesised in a laboratory. Opiates include morphine, codeine, thebaine, heroin, hydrocodone, hydromorphine, oxycodone, meperdine, fentanyl, cairfentanil and pentazocine. Table 2 provides extra details on the chemical classes of opioids. The most common opiates that will be discussed in this review are heroin and prescription opioids. The most common types of prescription opioids are hydrocodone, oxycodone, oxymorphone, morphine, codeine and fentanyl. Effects of opioids usually include euphoria, slurred speech, analgesia, slowed respiration, drowsiness and itching (Julien, 2005). Because of the euphoric response attained by some people through the use of opioids and the strong addictive properties of the drug, the potential for misuse is high.
Table 2.
Chemical classification of opioids.
| Classification and definition | Names/Brand names |
|---|---|
| Natural - Alkaloids contained in the resin of the opium poppy | Morphine |
| Codeine | |
| Thebaine | |
| Semi-Synthetic - Created from natural opiates | Hydrocodone—Vicodin |
| Hydomorphone—Dilaudid | |
| Oxycodone—Oxycontin | |
| Oxymorphone—Opana | |
| Diacetylmorphine—Heroin | |
| Synthetic - Man-made drugs that mimic the effect of opioids | Fentanyl—Duragesic |
| Methadone—Methadose | |
| Meperidine—Demerol | |
| Pentazocine—Talwin |
OxyContin is a very popular brand of oxycodone, marketed by Purdue Pharma in the 1990s. Many studies have investigated OxyContin exclusively, and so any distinct mention of OxyContin in this review can be attributed to a study focusing solely on this brand. OxyContin is designed to provide the delivery of oxycodone over a 12-h period for the treatment of moderate to severe pain. Prior to 2010, it was possible to chew, crush and snort or dissolve in water and inject, leading to rapid release and absorption of the drug. OxyContin is particularly problematic for users as it contains a much larger amount of oxycodone (the active ingredient) than other prescription pain-killers (CSAT, 2001). The abuse deterrent formulation of this product in 2010 reduced manipulations of this product substantially (Cicero & Ellis, 2015).
Side effects and negative consequences
Regarding general use of prescription opioids, common side effects include sedation, dizziness, nausea, vomiting, constipation, respiratory depression, physical dependence and tolerance. Some of the less common side effects are delayed gastric emptying, hyperalgesia (hypersensitivity to pain), immunologic and hormonal dysfunction, muscle rigidity and myoclonus (muscle spasms). Constipation and nausea are the most common side effects of prescribed use of opioids (Ricardo Buenaventura, Rajive Adlaka, & Nalini Sehgal, 2008). Opioid-induced constipation can be especially problematic for users; those reporting this side effect have been found to miss more work, report greater impairment while working or completing activities, and show lower health-related quality of life scores than those not experiencing constipation as a side effect (Bell, Annunziata, & Leslie, 2009). Adults living with children also risk the potential of the child obtaining the drug and ingesting it. Small children who unknowingly ingest the opioids may be at risk for death or other major effects (Bailey, Campagna, & Dart, 2009). Keeping opioids with adolescents in the house may lead to teenagers stealing pills from their parents or other relatives in an attempt to experiment with the drug or sell it to their friends (SAMHSA, 2016).
In conjunction with the sedative effects of opioids, they can also impair cognitive and psychomotor functioning, especially for persons taking the drug for the first time with no history of opioid use disorder (Zacny, 1995). Persons under the influence of opioids may not realise the extent of their impairment and attempt to operate machinery or drive cars, potentially becoming a danger to themselves and others. While chronic opioid users may not experience the same impairments as someone taking them for the first time due to their increased tolerance of the drug and its effects, additional neurocognitive deficits have been reported for persons using opioids for a long period of time. Impairments in verbal working memory, impulsivity and cognitive flexibility (verbal fluency) have been found to be some of the negative neuropsychological consequences of prolonged opioid use (Baldacchino, Balfour, Passetti, Humphris, & Matthews, 2012). In a systematic review conducted by the U.S. Center for Disease Control (CDC), long-term use of opioids was found to be associated with problematic use behaviours, as well as clinically significant impairment and distress (Guy et al., 2017)
Many opiate users begin their use as a result of genuine pain, such as chronic pain and cancer pain patients. Cancer pain can affect persons undergoing treatment, survivors and patients in advanced or terminal stages, and can have a distinct impact on quality of life (Posternak et al., 2016). Overall, 38% of any type of cancer patients reported experiencing moderate to severe pain in a recent meta-analysis. Sixty-six percent of patients in advanced, metastatic care or terminal patients reported pain, as well as 55% of those in anti-cancer treatment and 39% of patients who had concluded their curative treatment (van den Beuken-van, Hochstenbach, Joosten, Tjan-Heijnen, & Janssen, 2016). Cancer survivors often experience a shift from acute pain to a chronic and stable pain which encompasses both cancer and non-cancer pain (Posternak et al., 2016). Opioid use for chronic cancer pain has generally been more acceptable than for chronic non-cancer pain, with little restriction on prescriptions for cancer pain as opposed to non-cancer pain. However, new regulations on opioid prescriptions meant to curb the opioid epidemic may be having a negative effect on cancer patients that need prescription pain killers the most (ACS CAN, 2018).
Pain that cancer survivors experience can come from surgery, radiation and chemo-therapy-induced neuropathies (Wiffen, Wee, Derry, Bell, & Moore, 2017). Even though there is a paucity of literature in managing chronic cancer pain with persistent opioid therapy, extensive literature available for chronic cancer pain based on RCTs shows insufficient evidence to determine long-term benefits of opioid therapy for chronic pain (Manchikanti et al., 2017). Further, there is also an abundance of evidence of serious adverse consequences associated with long-term opioid therapy related to administered dosages, duration and combination of opioids with benzodiazepines (Manchikanti et al., 2017).
Some persons who begin using opioids for legitimate pain may go on to misuse the drugs, which may result in further negative health impacts. Respiratory depression, or slowed breathing, can occur due to the sedative effects of the drug and may result in overdose and death. Some opioids demonstrate among the highest active/lethal dose ratios of any illicit substances, meaning they are some of the most dangerous drugs when it comes to potential for overdose (Gable, 2006). Likelihood of lethality can be exacerbated by combining opioids with alcohol or other depressants. Users may also engage in other risky behaviours such as criminal activities to obtain money or drugs. Persons abusing prescription opioids may go on to use heroin, an opioid which can impact health drastically. Heroin users may experience mental disorders, sexual dysfunction, and women’s menstrual cycles tend to become irregular. Those who snort heroin can damage their mucosal tissues and/or perforate their septum, and intravenous injection users put themselves at risk for scarred and collapsed veins, bacterial infections of the blood vessels and heart valves, abscesses and other soft-tissue infections. Furthermore, heroin may be cut with additives that do not dissolve in blood vessels and may clog vital organs, causing infection or death of small cells in the organs (NIDA, 2018).
Prevalence of opioid use
Past-year use of opioids (including heroin and prescription opioids) is estimated to be between 28.6 and 38 million people globally, with a global average prevalence of 0.7%. Opioid use has increased globally over the past few years, but the main increase has been observed in the United States, where the prevalence rate of past-year opioid use is 4.7% (UNODC, 2014). In Africa, misuse of prescription opioids was reported to be higher than use of heroin (3.6% other opioids, 2.2% heroin). Latin and Central America have generally always had low levels of opioid misuse, and these levels do not appear to have changed in the past few years. Opioid misuse in Asia is low at around 0.35%, however, data is not available for all Asian countries. South-West and Central Asia have higher opioid use rates compared with East and South-East China; the average prevalence for opioid use in Afghanistan, Iran and Pakistan is estimated to be 1.5% and 0.8% in Central Asia. In Western Europe, past-year use of opioids is estimated to be 0.4%; however, Eastern European prevalence rates hover around 1.2%, while South-Eastern European is around 0.8% (UNODC, 2014).
Many who are prescribed opioids for acute or chronic pain take their pills as prescribed, experience pain relief with possibly a few unpleasant side effects and have no further complications associated with the pills. Nevertheless, misusing and/or becoming addicted to opioids is one of its most prevalent negative health impacts. Although, many countries conduct epidemiological surveys to assess prevalence of substance misuse involving alcohol, cannabis, cocaine, etc., a large number of countries do not assess misuse of prescription opioids (Zacny & Lichtor, 2008). Thus, while we have global data on opioid use prevalence, it can be difficult to draw comparisons on prevalence rates of misuse of opioids between countries. For these reasons, much of the information detailed in this section focuses on data acquired from the United States.
In 2016, it was estimated that approximately 11.8 million Americans misused opioids in the last year. Out of those, around 891,000 were children and adolescents aged 12–17. Out of the 11.8 million people misusing opioids, 11.5 million people were estimated to be misusing prescription pain killers. The most popular subtype of misused prescription opioid was hydrocodone, followed by oxycodone, tramadol and codeine. Of those who misused opioids, approximately 2.1 million Americans aged 12 or older were thought to have opioid use disorder, including approximately 152,000 adolescents aged 12–17 years. Heroin and prescription pain killers were the two categories of drugs included in grouping opioid use disorder. Of those 2.1 million people with opioid use disorder, 1.8 million were estimated to have prescription pain killer use disorder, with only a small minority being addicted only to heroin (SAMHSA, 2016).
Standardised mortality ratios in long-term cohort studies in the United States indicate that opioid users are 6 to 20 times more likely to die than the general population. Of all drug overdose deaths in the EU, opioid overdoses accounted for 81% of those deaths (International Narcotics Control Board, 2017). In America, opioids were involved in over 72,000 overdose deaths in 2017 (Ahmad, Rossen, Spencer, Warner, & Sutton, 2018) and opioid overdose deaths were five times higher in 2016 than 1999 (Ahmad et al., 2018). Heroin use disorder has also increased, up by 150% since 2007 (Jones, Logan, Gladden, & Bohm, 2015b). Use of fentanyl, an opioid up to 50 times stronger than heroin, has also had an alarming rise in the last few years. Fentanyl deaths doubled in one year, from 9,580 in 2015 to 19,413 in 2016 (Dowell, Noonan, & Houry, 2017).
Prescription opioids and pain
Although, many of those with opioid use disorder take prescription pills for the intended purpose of relieving subjective pain, they may be taking pills that were not prescribed to them, or at higher doses than needed to effectively manage pain (SAMHSA, 2016). A review of outpatients using opioids in a large healthcare system found that the prevalence of opioid dependence was as high as 26% for those in long-term opioid care (Boscarino et al., 2010). Another systematic review of prevalence of misuse, abuse and addiction among those being treated by opioids for chronic pain revealed average rates of misuse ranging between 21 and 29% and addiction rates ranging from 8 to 12% (Vowles et al., 2015).
A major issue that has yet to be addressed regarding opioid misuse is the source from which people obtain the pain killer. Of the approximate 11.5 million people that misused opioids in the last year, 53% obtained them from a source other than their prescribing physician, such as from relatives or friends, much of the time receiving the opioids free of charge. Only 37.5% of people who indicated having misused pain killers in the last year acquired them from a health care provider (SAMHSA, 2016). This is referred to as drug diversion, which is a significant problem that must be tackled when considering options for opioid prescribing policy. The sheer number of opioids that are available in the U.S.A. because of over-prescribing allows for sharing, gifting and selling of pain killers, creating a danger of opioids getting into the hands of those that do not have any medical use for them.
Often, opioid users have alternate motives to using opioid pain relievers other than getting rid of pain. Other cited reasons for misuse of opioids were to ‘get high’ or feel good, to relax, help with feelings or emotions, help with sleep, experiment with the drug, to prevent withdrawal/they were already ‘hooked’ on it, or even to combine the pain killers with other drugs for additional effects (SAMHSA, 2016). A study of relatives of those who had died of opioid-related overdose in Utah found that the majority (88.6%) reported that the decedent’s experienced some type of pain, although, 29.8% were revealed to be taking the medications for other reasons – such as recreational use and self-medication (Johnson et al., 2013).
Cancer
Despite the insufficient evidence of the benefits over harms of treating long-term cancer pain with opioid therapy, in western countries, a vast majority of cancer patients who experience pain are prescribed an opiate. In the United Kingdom, for example, 13% of all opioid prescriptions are dispensed for cancer pain (Wiffen et al., 2017). Forty-three percent of cancer patients, 10% of cancer survivors and 34% of chronic pain patients in the United States reported using opioids in 2018. The number has decreased significantly for cancer survivors (down from 24%) and chronic pain patients (down from 48%) since 2016, but has remained stable for cancer patients (ACS CAN, 2018). Among cancer patients undergoing curative-intent surgery, such as early-stage breast, melanoma or lung cancer, 10% of patients were still filling opioid prescriptions 3 months and even one-year after surgery at high doses (six tablets per day of 5-mg hydrocodone). This dose is the approximate daily dose consumed for managing early post-operative pain. Typically, surgeons expect patients to finish their medication after about two weeks after completion of surgery. Additionally, undergoing chemotherapy increases risk of chronic opioid use even further, with 15–21% of chemotherapy patients continuing to take opioids past the recommended length (Lee et al., 2017).
Heroin use
The global average prevalence for injection drug use is around 0.27%, but varies widely among countries (UNODC, 2014). In the European Union, heroin is still the most commonly trafficked and used opioid; moreover, the number of opioid drug overdose deaths have increased for the third consecutive year. Heroin use accounts for about 80% of admissions into opioid treatment in the EU (International Narcotics Control Board, 2017). Additionally, Eastern/South-eastern Europe has the highest prevalence of injecting drug use in the region at 1.26% (4.6 times the global average). The Russian Federation had the highest drug-injecting prevalence at 2.29%. In America, the prevalence of lifetime heroin use was around 1.6% among adults in 2013, and prevalence of heroin use disorder was 0.69%, up significantly from 0.33% and 0.03%, respectively, when measured in 2002 (Martins, Sarvet, Santaella-Tenorio, Saha, Grant, & Hasin, 2017).
Differences in drug practices seem to exist between injecting heroin and smoking/inhaling it, also known as ‘chasing the dragon’. Those who inhale heroin tend to have less severe dependence scores and are less likely to be daily users than injectors. Inhalers also tend to be younger, female and have more non-drug using friends than intravenous drug users. Those who inhale heroin are less deeply ingrained in the ‘drug culture’ (Strang, Grifiths, Powis, & Gossop, 1999). Unfortunately, another negative consequence of the rise in prescription opioids is that heroin use has risen among those reporting nonmedical use of prescription pain killers. Persons who misused pain killers more frequently (100þ days in the past year) were at an even greater risk. Frequent pain killer users were at an increased rate of injecting heroin, as well as at increased odds of having heroin dependence compared to those who reported no nonmedical use of prescription pain killers. Additionally, 82.6% of frequent users of prescription pain killers who have also used heroin reported that they misused the prescription opioids prior to initiation of heroin use (Jones, 2013) and in younger cohorts of heroin users, it has been found that the vast majority report initiating opioid misuse with prescription medications (Novak, Bluthenthal, Wenger, Chu, & Kral, 2016).
Adolescents
In the United States, pain killers are the fourth most misused drugs among adolescents, behind cigarettes, alcohol and marijuana (Johnston, O’Malley, Bachman, & Schulenberg, 2009). The annual prevalence of non-medical pain killer use among adolescents has hovered around 9–10% over the last decade or so, with spikes in the recent years (Johnston, O’Malley, Bachman, & Schulenberg, 2011; Johnston et al., 2009; McCabe et al., 2017). Lifetime medical use of prescription opioids among adolescents has, as expected, been higher, around rates of 15% or more beginning in the early 2000s. Medical opioid use prevalence was found to have an estimated linear regression coefficient of 0.552 (p < .01) when predicting lifetime non-medical use of prescription opioids among adolescents, indicating that legitimate medical use is a predictor of future misuse among adolescents (McCabe et al., 2017).
Students enrolled in California continuation high schools (which serve students who have left the regular school system due to problems such as excessive absenteeism, poor academic performance, violence, drug use, etc.) had much higher lifetime rates of prescription opioid use – 36%, and a past-month prevalence of 14%. Among these alternative-high school youth, white ethnicity, living with both parents and increased access to healthcare predicted pain killer medication use a year after baseline. Better healthcare could result in lower out of pocket medication costs for prescription opioids which could in turn increase access to opioids by adolescents who are in an at-risk environment (Sussman et al., 2012).
Regional differences
While many high-income countries such as the United States, Canada and Australia have some of the highest reported prevalence of misuse, some lower-middle and lower-income countries also have high levels of opioid misuse, such as Nigeria and Pakistan. Africa and Asia are seeing a rapid expansion of the use of illicitly supplied tramadol, a pharmaceutical opioid that is not under international control, which is posing significant challenges (World Drug Report, 2018). Differences also exist in the European Union. For example, in Estonia, fentanyl is the drug most commonly reported when entering opioid-related treatment, and in Czechia, other opioids other than heroin are reported to be used just over 50% of the time (International Narcotics Control Board, 2017).
In the United States, prescription drug use is heavily concentrated in rural, suburban and small urban areas (Cicero et al., 2007). Rural drug users also seem to be different than those using in urban areas. Comparing an Appalachian county of Kentucky versus a major metropolitan area in the same state, those living in rural Kentucky tended to start using drugs such as oxycodone, hydrocodone, benzodiazepines, cocaine and crack earlier, and also had higher odds of ever using opioids such as methadone, OxyContin and oxycodone than those living in the urban area (Young, Havens, & Leukefeld, 2012). Hospitalisations involving prescription opioid overdoses were more prevalent in the South; however, heroin-related overdoses were more common in the Northeast and were growing rapidly in the Midwest (Unick & Ciccarone, 2017). Southern states, with relatively higher rural representation, such as Alabama, Tennessee and West Virginia had the highest rates of opiate prescriptions per person in 2012 (Guy et al., 2017). States with the highest incidence of overdose deaths included West Virginia, Ohio, New Hampshire, Pennsylvania and Kentucky (Center for Disease Control and Prevention Drug Overdose Death Data).
Doctors in these rural areas may prescribe opioids to treat chronic pain for work that requires heavy labour, such as logging, farming, mining and working in factories. Many of these industries are declining, and thus people are left unemployed and hopeless when there are no more jobs available. Some workplace injuries lead to chronic pain, such as coal miners developing silicosis, a lung disease. Much of the coal mining industry is concentrated in the Appalachian area, which may help explain why opiates caught on so quickly in this particular region. It’s possible that some of these people turn to opioids as a release for their pain, and in turn get addicted (Van Gundy, 2006).
Correlates and determinants of opioid use
Currently, much is still unknown about the long-term outcomes of opioid use among people that initiated opioid use with prescription pain killers. Much of the research that has been conducted on correlates and determinants of opioids and their long-term outcomes such as abstinence and mortality rates has been conducted based on heroin addicts, including what is presented in this section of the article.
Additionally, the majority of studies conducted on opioid misuse have been conducted in the U.S.A. This section will review the literature on how neurobiology, demographics, environmental characteristics, history of dependence and mental illness, and injection drug use culture help to predict opioid misuse.
Neurobiology
There is evidence for heritable vulnerability in opioid dependence. Polymorphisms in genes that code for various receptors such as dopamine, opioid, cannabinoid and serotonin may in part be responsible for individual variation in susceptibility to opioid addiction (Saxon, Oreskovich, & Brkanac, 2005). Across all drugs, approximately 50% of addiction vulnerability has a genetic basis (Wang, Kapoor, & Goate, 2012).
Demographic and psychosocial characteristics
There has been an abundance of studies investigating various demographic, personality, social, environmental and hereditary variables that may be associated with substance misuse. Results from a national U.S. survey found that while women were far less likely to endorse lifetime or past-year non-medical use of opioids than men (15.9% vs. 11.2% – lifetime, 5.9% vs. 4.2%– past year use; p < .0001), they were equally likely to meet criteria for prescription opioid dependence if they had used in the past-year. (Back, Payne, Simpson, & Brady, 2010).
Influences in early life have been identified as potential risk factors for injecting drug use behaviour. In Scotland, a case-control study found that having a two-parent family, as opposed to other family structures, resulted in less likelihood of that child growing up to become an injection drug user, while those who had gone through public care were more likely to become an injection drug user. Early childhood conduct problems, such as problems at school resulting in expulsion and being in the juvenile criminal justice system were associated with injection drug use. Violence and financial problems in the family also increased risk for injection drug use later in life (Macleod et al., 2013). Engaging in risky behaviours such as alcohol and polysubstance use early in life also put adolescents at risk for future injection drug use behaviour (Trenz et al., 2012).
Homelessness and availability of housing is an important structural contributor to initiation of injection drug use. Homelessness has consistently been shown to be a crucial risk factor for initiating injection (Feng et al., 2013; Roy et al., 2003). Drug users who are homeless or lack stable housing may gather in particular drug venues or areas where other users congregate in order to have a safe place to inject (‘safe houses’), thereby potentially increasing chances of sharing needles, as well as bringing injection-naïve persons to areas where injection is common (Roy et al., 2003). Additionally, incarceration, which is often due to involvement in drug-related crimes in the United States, has been found to be negatively related to abstinence from opioids in a long-term follow-up review (Hser, Evans, Grella, Ling, & Anglin, 2015).
First-time heroin injection initiation typically happens within close social networks where illicit drug use is normalised (Draus & Carlson, 2006). Qualitative interviews indicate that much of the time, first-time injecting behaviour is seen as a combination of curiosity and social pressure. One participant told researchers that ‘they (friends) were all doing it, so I was like, “might as well”‘. Reports from a study in rural Ohio also noted that injectors may feel the need to chase the high and use drugs to relieve boredom, as there are not many things to do, as one interviewee expressed (Draus & Carlson, 2006). This may be an important factor in initiation and maintenance of drug use, especially in small-town America where there may be a relative lack of other activities for adolescents and adults to engage in.
In a case-control study comparing prescription opioid users in Utah and those that had died from prescription opioid- related deaths, decedents were more likely to smoke daily, not have graduated high school and have been divorced, separated and/or lived alone. A lack of health care coverage was also more common for the decedents. They also were more likely than the opioid-using comparison group to use the pain medicine more than prescribed and to have obtained the opioids from non-prescription sources (Lanier, Johnson, Rolfs, Friedrichs, & Grey, 2012). The same data were analysed to ascertain characteristics of the decedents as described by their next of kin or best contact. Those who had died from opioid-related overdose in Utah were generally more likely to be middle-aged, Caucasian, not married and resided in more rural areas than the general population of Utah. Of 254 decedents, 76% of their next of kin or best contacts expressed that there had been concern from family or friends about the decedent’s drug use. Only 33% stated that a healthcare provider expressed concern over their drug use. In comparison to the general population, the decedents were also more likely to have financial problems, unemployment, physical disability, mental illness and engaged in alcohol/substance use (Johnson et al., 2013).
Physical and sexual abuse
Childhood sexual abuse has been linked to increased risk for initiating injection drug use (Hadland et al., 2012; Roy et al., 2003). However, when another study matched opioid-dependent persons with those of similar social disadvantages, child maltreatment did not explain the prevalence of opioid-dependence. While opioid abusing females had higher rates of sexual abuse and parental separation, and males reported higher rates of physical and emotional abuse than controls, community participants matched at similar levels of socioeconomic disadvantage had roughly the same incidence rates of child maltreatment and neglect in their past (Conroy, Degenhardt, Mattick, & Nelson, 2009).
Sexual and physical abuse is associated with opioid misuse, with 44.6% of patients in opioid use treatment reporting physical abuse, sexual abuse, or both in their lifetime. Women were more likely to report having experienced both physical and sexual abuse, while men were more likely to report having experienced only physical abuse (Oviedo-Joekes et al., 2011). Even among case-control matched participants of similar social disadvantage, opioid-dependent males had higher prevalence of physical and emotional abuse and females had a higher prevalence of sexual abuse. While opioid misusers who were also victims of physical or sexual abuse were more likely to have poorer psychiatric, family and social functioning, in addition to an increased rate of suicide attempts and previous drug treatments, they still improved over the course of medication-assisted treatment, with approximately the same outcomes as those who had no history of misuse or dependence (Oviedo-Joekes et al., 2011).
Mental health
Of 14 studies reviewed, co-morbid psychiatric disorders were found in 40–80% of opioid- treatment seekers (Strain, 2002). Across multiple long-term outcome studies, rates of depression in opioid users at baseline ranged from approximately 20–30% (Hser et al., 2015). Several other mental health illnesses have been found to be associated with opioid misuse, with one study of methadone treatment patients in Australia citing 41% of participants meeting criteria for PTSD, 71% for antisocial personality disorder and 46% for borderline personality disorder at baseline (Darke, Ross, & Teesson, 2007; Darke, Williamson, Ross, Teesson, & Lynskey, 2004;). A different study found 38.7% of patients in methadone treatment exhibited early signs of conduct disorder or antisocial personality disorder at baseline (Grella & Lovinger, 2011). A history of substance use disorder, younger age, major depression and use of psychotropic medications were all associated with misuse of opioids for outpatients utilising opioid therapy (Boscarino et al., 2010). In a study conducted in Germany, heroin misusers were found to have more fearful-avoidant attachment styles, which the authors proposed could be an indication that heroin might be used as an emotional substitute for lack of coping strategies, based on a self-medication hypothesis (Schindler, Thomasius, Petersen, & Sack, 2009).
There is conflicting evidence about the co-morbidity of mental health illnesses with opioid use disorder, along with the impact of those illnesses on the trajectory of the substance use disorder. This can be attributed to a number of causes – such as under-reporting or misinformation given by the patients, a lack of skill in administering proper clinical questionnaires in treatment facilities, lack of qualified personnel and a lack of empirically driven evidence for treating co-occurring substance use and mental disorders.
Initiation into injecting drug use: from pain relief to injecting behaviour
Heroin is generally stronger than prescription pills and tends to be consumed in ways which can lead to severe negative health outcomes. Pharmaceutical opioid misusers who combined use of more than one opioid in the last year (polyopioid use) had a greater chance of moving on to becoming heroin and/or injecting users. The same was true for those who had been using pharmaceutical opioids (even if it was just the same one), for two years or greater (Grau et al., 2007). Drug dealers often offer heroin as an alternative to prescription pain killers when they are out of opioid pills (Mars, Bourgois, Karandinos, Montero, & Ciccarone, 2014). Hays (2004) gathered data on 187 participants admitted to an adult addictive disease unit for OxyContin abuse, and found that while 83% of patients began their use with oral administration, by the time of admission for treatment, only 14.3% were still swallowing pills, while 62.4% were snorting and 25.6% were injecting opioids.
The typical progression for those who had started with prescription opioid pills was – first regularly taking the pills, then chewing them, then crushing them into powder and sniffing or smoking them. Sniffing or smoking heroin followed, as heroin was often easier to obtain and cheaper than opioid pills, and was able to deliver a stronger high to the already opioid dependent persons. The ‘less extreme’ method of sniffing or smoking made it easier to transition into injecting heroin, as the jump was not direct from oral ingestion of pills to injecting (Mars et al., 2014). By the time opioid users inject, they are usually already dependent on some sort of opioid and may experience withdrawals if they do not maintain their drug use. This, combined with the money they can save by injecting rather than swallowing pills or snorting, also contributes to opioid users initiating injection behaviour (Draus & Carlson, 2006).
In the larger-sociocultural context, drug use is generally seen as a negative behaviour, with injecting drug use in particular viewed as extremely dangerous. The drug user who is considering initiating their first injection has to put aside their worries about the public perception of them as ‘hard-drug users’ or ‘junkies’, which is often seen as a distinct turning point in the person’s drug use and their perception of themselves (Hassin, 1994; Rosenbaum, 1979). Concurrently, the first injection provides a ‘rush’ unlike any other of the drug – while they may have used opioids before through various other methods of administration, the immediate and euphoric feeling of the drug has been described as unexplainable and uncontrollable (Fitzgerald, Louie, Rosenthal, & Crofts, 1999; Martin, 2010).
Users often indicated that they thought they would ‘never do such a thing’, and yet all of those ‘nevers’ came true. They explained that the gradual transitions from swallowing prescription pain killers, to sniffing/smoking pills, to sniffing/smoking heroin, to injecting heroin was a response to their increased tolerance and dependence. Avoidance of withdrawal and changing contexts in which norms that were once taboo became normalised through friends and others in their social network of other drug users (Mars et al., 2014).
Estimates of injecting users who facilitate the initiation into injection of others range from 17 to 47% (Bryant, & Treloar, 2008; Crofts, Louie, Rosenthal, & Jolley, 1996). The person administering the injection (usually a friend, partner or family member) was reported to be intoxicated at the time of injection by 80% of respondents, and 10% of first-time injectors in rural Kentucky reported that the syringe had previously been used (Young, Larian, & Havens, 2014). Because injecting behaviour is a complex social process involving interpersonal relationships as well as the larger community of drug users, a focus should also be placed on reducing facilitation of injecting (Strike et al., 2014; Wenger, Lopez, Kral & Bluthenthal, 2016; Werb et al., 2018). This approach is promising, in part, because people who inject drugs often express reluctance to assist with injecting someone for the first time (Guise, Horyniak, Melo, McNeil, & Werb, 2017; Guise et al., 2018; Wenger et al., 2016).
Age differences in initiation of injection drug use
Studies on trajectories to injection drug use have found that most people who will inject do so by their mid-twenties, although, about 1 in 7 will initiate injection at the ages of 30 or older (Arreola et al., 2014). Age cohort differences in pathways to injection drug use have been observed, with people who were born in the 1960s and 1970s and came of age when cocaine and crack cocaine where the most popular illicit drugs, reporting longer time to first injection. Cohorts of people born since then have been exposed to opioids during vulnerable ages (teens to early twenties) and report both injecting sooner and being more likely to initiate injection with heroin as compared to those born in the 1970s (Bluthenthal, Wenger, Chu, Bourgois, & Kral, 2017).
Gender differences in initiation of injection drug use
Many sociocultural and psychological factors contribute to first-time injection behaviour, and it appears that for women, social factors and interpersonal relationships play a bigger role in the first-time injection experience than for men. For example, women were more likely to be initiated into injection by their partner, inject at a partner’s house, receive the drugs and syringes as gifts from their partner and depend on them for further injections. They were also more likely to have a partner that was also an intravenous drug user (Draus & Carlson, 2006; Young et al., 2014). Women were also more likely to inject for the first time due to social pressure (i.e. ‘feeling pressured into it’ or ‘wanting to be cool’). There’s also some qualitative evidence for the idea that some women may try injecting for the first time as a way to get closer with their partner; to bond and strengthen their relationship through mutual trust, as well as protect their relationship from failing. Thus, it seems that especially for women, the first initiation into injecting drugs should be viewed from the sociocultural and interpersonal relationships that surround their individual experiences (Martin, 2010).
Strategies to decrease prevalence of opioid misuse
Global organisations have acknowledged the rise in opioid misuse across the world, including the World Health Organization, the International Narcotics Control Board and the United Nations. The increase in synthetic opioid usage may put additional pressure on national health care systems, particularly those that are fragile and are not able to provide coverage and services for substance use disorders (World Drug Report, 2018). The United States Food and Drug Administration (FDA) has instituted many regulations on prescribing such as strengthening warning labels and requiring authorisation from prescribers to refill medications instead of simply allowing them to refill automatically (FDA, 2018). The CDC has also implemented many guidelines for prescribers to ensure as safe of prescribing as possible (CDC, 2017).
Still, much is left to be done to prevent those at risk for developing opioid use disorder, and to help those that are already affected. Unfortunately, sometimes legislative action that aims to reduce pain killer prescribing may actually lead to increased heroin use (Kolodny et al., 2015). In 2010, Purdue Pharma was approved by the FDA to make a tamper-resistant OxyContin formula (Food and Drug Administration, 2009), which was meant to stop users from crushing up pills to sniff or smoke them to circumvent their time-release action. This shift resulted in some users transitioning to heroin, as it was the easier, faster and cheaper option. The U.S. Drug Enforcement Agency (DEA) sent out a notice to healthcare organisations, noting that the reformulation of the drug may lead to some users transitioning to heroin (Office of Diversion Control Liaison and Policy Section Liaison Unit, Drug Enforcement Administration, 2010). This warning was largely ignored (Mars et al., 2014).
Prevention
Types of prevention
Universal prevention refers to programming that targets all individuals and attempts to prevent society at large from abusing opioids. Selective prevention targets elevated risk groups, such as those who are being treated with opioids for chronic pain (or relatives of opiate misusers). Finally, indicated prevention targets high risk subgroups such as those who are misusing prescription opioids to prevent them from escalating their drug use into injecting behaviour.
Universal prevention that emphasises instilling fear of drug use, or informational interventions that educate individuals on the negative consequences of drug use have not been found to be particularly effective (Sussman & Ames, 2008). Comprehensive social-influence orientated approaches that counteract social influences and impart life skills may be more effective. These approaches use techniques such as refusal skill instruction, media literacy and correction of social informational inaccuracies (Sussman & Ames, 2008). Additional cognitive-behavioral therapy (CBT) techniques include self-monitoring and instruction on how to cope with stressful situations such as seeking out social support, relaxation strategies such as meditating, self-management, behavioural regulation and problem-solving strategies (Sussman, 2017). Selective and indicated prevention programming may rely on a motivation-skills-decision-making model (Sussman, 2017).
Prevention programming for adolescents should primarily focus on (a) redirecting or reducing problem antecedent behaviours (violence, impulsivity, sensation-seeking), (b) strengthening resiliency traits (self-regulation, coping, cognitive control) and (c) reducing exposure to conditions in which drug use may occur (peer pressure, stress, adversity). Older teens or those at relatively high risk for opiate misuse can enhance their motivation not to use (e.g. explore health as a value, confront their general self-image as a moderate against their more immoderate behaviour, rebel against negative stereotyping), learn self-control skills and engage in decision making (for more details see Sussman, 2017). While universal and selective prevention programme strategies have not targeted opiate misuse specifically (prevalence is too low), effects on gateway or other hard drugs have been promising (Sussman, 2017; Sussman & Ames, 2008). In addition, one study evaluating the longitudinal effects of a brief universal prevention intervention for middle schoolers found significant relative rate reductions of prescription opioid misuse in the participant’s later adolescent and young adult years (Spoth et al., 2013).
Studies have shown that regulatory prevention, which aims to limit availability of drugs through laws or taxes is especially effective for reducing levels of harm for young people, at least when it comes to readily available substances such as alcohol and tobacco (Mohler-Kuo, Rehm, Heeb, & Gmel, 2004; Tauras, Markowitz, & Cawley, 2005). This becomes more complicated with prescription opioids, however, as they are generally obtained from a doctor (generally for free or at a reduced cost with insurance), or from family and friends who were prescribed the medication. A brief script-safety intervention was implemented for 62 patients who were being prescribed opioids, which showed post-intervention improvements in knowledge about safe prescription storage and misuse behaviours. The intervention lasted 15 minutes and educated patients about proper storage techniques, as well as the dangers of sharing prescription pills with others (McCauley, Back, & Brady, 2013). Quick interventions such as these may be practical and efficient to use in doctor’s offices to help reduce drug diversion.
Project TND, a 12-session school-based prevention programme that targets at-risk youth (such as those attending alternative high schools) with the goal of deterring them from using alcohol or other substances, has shown to be effective at reducing hard drug use (including pain killers) in seven randomised controlled trials (See Sussman, 2017 for a summary of trials). The model the programme is based on incorporates prosocial motivation enhancement, life and social skills and decision-making strategies as cognitive-behavioural processes that decrease vulnerability to a wide range of deviant outcomes. Some of the motivation enhancement techniques – which are critical to this programme – include correcting drug myths through cognitive elaboration strategies, counteracting stereotypes, valuing health and clarification of attitudinal perspectives. Social skills such as self-control, communication and acquisition are also taught. Finally, decision-making strategies are given in four steps – brainstorming, weighing pros and cons, selecting the best option and following through. After multiple RCTs, it’s been hypothesised that the key ingredient to the success of Project TND is the classroom context which facilitates facilitator–youth and youth–youth interactions as they engage in programme activities (Sussman, 2015).
A meta-analysis of the research on 120 school-based drug prevention programmes further found significant superiority of interactive versus non-interactive prevention programmes for adolescent illicit drug use (Tobler & Stratton, 1997). A separate meta-analysis identified factors related to efficacy of school-based interventions. Gottfredson and Wilson (2003) concluded that prevention programmes do not need to be very lengthy (programmes under 4.5 months were generally as effective as longer ones that extended throughout the entire school year). They also found that targeting middle schoolers and designing programmes that can be delivered by peer leaders could increase the effectiveness of school-based substance use prevention programmes. Middle schoolers (over older adolescents and younger children) were also slightly more likely to achieve a significant effect on alcohol or other drug use than programming for elementary or senior high school youth (Gottfredson & Wilson, 2003). Additionally, programmes that incorporated social competency skills had stronger effects when targeting higher-risk youth rather than the general population.
Alternatives to pain relief
The CDC guidelines recommend nonpharmacological and non-opioid pharmacological therapy as the first-line of treatment for pain, except in more severe cases such as palliative, active cancer or end-of-life care (Dowell, Haegerich, & Chou, 2016). To help prevent individuals from abusing prescription opioids in the first place, it is important to ensure that pain relief opioids are only being prescribed when deemed absolutely necessary, and that usage is monitored strictly thereafter. The benefits of pain relief should be weighed against the risks posed by opioids. There has been little to no evidence of opioids exhibiting long-term benefits in either pain or function for patients with chronic pain when outcomes were examined at least one year later. In contrast, there is clear and distinct evidence of the risks and harms related to opioid usage such as dependence, overdose and motor vehicle injury. When opioids are deemed necessary, it is still important to consider combining opioids with other treatment modalities in order to increase rates of success as well as possibly reduce dosage of opioids required to manage the pain (Dowell et al., 2016).
Alternative pharmacological treatments to opioids include nonsteroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, anticonvulsants, duloxetine, topical agents, muscle relaxants and interventional procedures such as steroid injections (Ling, Mooney, & Hillhouse, 2011). A number of studies have investigated the efficacy of anti-depressants for the treatment of pain such as chronic lower back pain and neuropathic pain with some evidence of pain relief among patients using tricyclic or tetracyclic antidepressants that inhibit norephreninereine reuptake (Saarto & Wiffen, 2010; Salerno, Browning, & Jackson, 2002; Staiger, Gaster, Sullivan, & Deyo, 2003). In fact, a randomised clinical trial with a sample of 240 patients suffering from moderate to severe chronic back pain, or hip or knee osteoarthritis demonstrated that non-opioid (acetaminophen or a nonsteroidal anti-inflammatory drug) and opioid treatment did not differ significantly in their reduction of pain-related function. Furthermore, the non-opioid group had less pain-intensity, as well as less adverse medication-related side effects than those in the opioid group (Krebs et al., 2018).
In states in the U.S.A. where medical marijuana is legal, prescribing cannabis instead of or alongside opioids may facilitate reductions in opioid use. Use of medical marijuana has been shown to decrease opioid use, reduce side effects of medications such as opioids, and improve quality of life of chronic pain patients (Boehnke, Litinas, & Clauw, 2016). A study of injecting drug users in Los Angeles and San Francisco found that opioid users who used cannabis in the last 30 days used opioids less frequently (Kral et al., 2015). Cannabis may also help to reduce cravings and withdrawal symptoms as well as prevent users from developing a strong tolerance for opioids (Cichewicz & Welch, 2003). When taken together, cannabis can augment the analgesic effects of opioids (Abrams, Couey, Shade, Kelly, & Benowitz, 2011).
Non-pharmacological options include exercise, physical therapy and psychological therapy. Different types of exercise treatment have shown to have varying level of improvement in pain and function for patients with fibromyalgia and osteoarthritis of the knee (Busch, Barber, Overend, Peloso, & Schachter, 2007; Fransen et al., 2015). Cognitive-behavioural therapy (CBT) has been found to have some positive effects on improving disability, catastrophic thinking and altering mood in chronic pain patients (Williams, Eccleston, & Morley, 2012). CBT could be utilised by chronic pain patients in order to offset some of the psychological symptoms and effects that dealing with chronic pain may produce, which may in turn help to mitigate the need to use opioids as a way of dealing with pain that’s not only physical.
Monitoring prescription opioid use and mitigating harmful consequences
Starting patients with immediate release, rather than extended release/long-acting opioids is recommended, along with starting off the patient with the lowest effective dosage. Often, opioid misuse starts with the prescription of opioids for an acute disorder. Roughly one-quarter of patients going into the emergency department for the treatment of a minor injury (ankle sprain) were prescribed opioids, with the number ranging from 2.8 to 40% in different states in the U.S.A. (Delgado et al., 2018). The CDC distributed guidelines in 2016 for safer opioid prescribing. The CDC recommends enough pills for three days or less of pain relief, asserting that more than seven days of opioids will rarely be needed for acute pain. Clinicians should assess patients for certain risk factors such as history of substance misuse, depression and prior use of psychotropic medication. If there are symptoms of opioid use disorder, relevant to indicated prevention, clinicians should assess the patient more thoroughly or refer them to the proper mental health source for treatment that includes pharmacological-assisted therapy. When increasing opioid dosage, the CDC recommends that clinicians give patients the option of also being prescribed naltrexone in order to reduce the risk of overdose (Dowell et al., 2016).
Clinicians are also recommended to establish treatment goals and expectancies with their patients when prescribing opioids. For first-time chronic pain opioid prescriptions, a follow-up within 1–4 weeks is important to evaluate benefits and harms, with further monitoring recommended at least every 3 months, re-evaluating if an opioid prescription is still necessary. Only when there is clinically meaningful improvement in pain and function that outweighs the risks of opioid misuse should the clinician continue prescribing opioids to their patient. It is also important for clinicians to discuss the risks and side effects associated with using opioids with their patients and potentially patient’s family members before issuing a prescription. It may also be pertinent to educate family members and loved ones of the signs and symptoms of opioid use disorder, as well as proper storage and discarding methods of the pills. For older adults and/or those with cognitive impairments, it may be necessary for clinicians to determine if a caregiver is needed in order to assist the patient with their medication administration (Dowell et al., 2016). Although, prescribing practices were already decreasing since 2012, the time of the CDC guidelines release (March 2016) was associated with a greater decline in overall opioid prescriptions, as well as high dosage prescriptions, which indicates that national guidelines may be effective in reducing availability of prescription opioids (Bohnert, Guy, & Losby, 2018).
Preventing non-medical use of prescription opioids
It is hard to control the situation of friends and relatives passing off their drugs to someone else. That is, pain killers may be obtained through a legal prescription but then go on to be sold or gifted to partner’s, friends, or family members for illicit consumption or misuse (Alexander, Kruszewski, & Webster, 2012). This problem could potentially be addressed by increased education, and encouraging physicians and pharmacists to assert to their patients the importance of refraining from drug gifting.
Additional education on the risks of opioids is needed. While there are various anti-drug programmes already instituted in many public-school districts, it appears that there has been a lack of emphasis placed on the high-risk of addiction when using opioids. Adolescents generally know that heroin is dangerous, with 73% of eighth-graders perceiving use of it without a needle as high risk. However, only 26% perceived occasional use of Vicodin as high risk. Additionally, occasional Vicodin use was thought to be less risky than occasional marijuana use, smoking 1–5 cigarettes a day and moderate alcohol use by the same group of adolescents (Johnston, O’Malley, Bachman, & Schulenberg, 2013). Thus, educating adolescents on the high risks and negative consequences of using opioids is a priority.
Treatment
Admission and completion
Admissions into opioid treatment in the U.S.A. increased 400% from 1998 to 2008, from 52,480 admissions to 120,877 (TEDS, 2010). Unfortunately, there are many users that may not get the treatment they need due to financial barriers, stigma, inadequate local capacity for care and other barriers (Hser et al., 2015). Like some other alcohol/substance use treatments, detoxification is required often as a precursor to more formal treatment, with the patient then moving onto outpatient or residential treatment programmes. Like other drugs, opioid misusers generally go through multiple cycles of treatment and relapse which may occur over a long period of time. Abstinence rates for those in remission of opioid misuse hover around 30% or lower in studies where a 10-year or more follow-up has been tracked, and are mostly stable thereafter (Hser et al., 2015). This echoes that of other drugs. Even with abstinence from opioids, however, many still go on to use or have increased use of alcohol or other drugs, perhaps in place of the opioids (Grella & Lovinger, 2011).
Demographic characteristics of patients that successfully completed treatment included older age, higher education, full-time employment and private insurance. Interestingly, patients referred through the criminal justice system also had higher treatment completion rates. Unfortunately, the odds of success as determined by completing treatment decreased slightly with every prior additional treatment attempt (Pan, Gao, Grant, Novicoff, & Kang, 2018). Healthcare providers make up only a small minority of referrals of opioid misusers to substance use treatment facilities (less than 10%). There is also evidence that referral from a healthcare source tends to result in lower treatment completion (Marie, Sahker, & Arndt, 2015). It is still important for healthcare providers to recognise signs of opioid dependence and refer patients to the correct sources, aiding in closing the gap of those with opioid use disorder that are not being treated. Addicts who wish to recover with the help of support groups can also turn to 12-step programmes such as Narcotics Anonymous (NA) and Heroin Anonymous (HA), both of which help opioid users get and stay clean. Though there has been no literature regarding efficacy of 12-step programmes specific to opioid misuse, the available evidence is that abstinence rates among participants in any 12-step programme is about as high as cognitive-behavioural treatment and motivational interviewing (Project MATCH) (Connors, 1998). The literature regarding AA (Alcoholics Anonymous) indicates that about 10% of people will remain active for several years, and of those who remain active, 50% maintain sobriety, especially if they are helping others in recovery (Galaif & Sussman, 1995; Pagano, Friend, Tonigan & Stout, 2004).
Treatment completion rates for opioid misuse are lower than those that are referred for other drugs (Marie et al., 2015). In a study of outpatient and rehabilitation/residential treatment programmes that receive public funding in the U.S.A., treatment completion of patients admitted for opioid use disorder was found to vary widely by state and was more successful in states that had a greater per population availability of treatment facilities that accepted state health insurance, and/or centres that had the option of sliding scale fees. States with a greater proportion of its residents living in rural areas tended to have lower treatment completion rates, and residential treatment was found to be four times greater at getting patients to complete treatment than outpatient treatment (Pan et al., 2018). Patients who had to wait longer for treatment (versus waiting zero days) were less likely to complete treatment (Pan et al., 2018).
Medication-assisted treatment
Medication-assisted treatment offers patients various long-acting opioids such as methadone, buprenorphine or naltrexone in order to control their drug use long-term. Methadone is a full agonist, buprenorphine a partial agonist and naltrexone an antagonist. Methadone maintenance treatment is generally funded by the public sector in the United States, and buprenorphine treatment is generally only offered in private clinics and offices. Buprenorphine has been shown to have no ceiling effect for pain relief (analgesia), while at the same time limiting the respiratory depression effects it has on the body, mitigating some of the potentially fatal consequences of the drug (Pergolizzi et al., 2010). Additionally, unlike some other opioids which have been shown to produce hyperalgesia (increased sensitivity to pain; Fishbain, Cole, Lewis, Gao, & Rosomoff) buprenorphine produces significant anti-hyperalgesia effects (Pergolizzi et al., 2010). These approaches are effective in approximately 50% of opiate addicts (Sussman & Ames, 2008). Methadone has been identified as the first-line medication assisted treatment for opioid use, however, there are mixed results of which is better – methadone, buprenorphine or heroin-assisted treatment. While treatment dropout and relapse may still occur at high rates even following medication-assisted treatment, one systematic review found that incorporating broader outcome measures such as HIV risk behaviours showed reductions following entrance into any maintenance programme (Gowing, Farrell, Borneman, Sullivan, & Ali, 2008). Other variables such as polydrug use, physical and mental health and criminal activity have been mentioned as important outcomes that should be measured in the opioid treatment research.
Treatment of opioid use disorder can be enhanced by using methadone or buprenorphine in conjunction with psychological intervention and therapy (Connock et al., 2007). Combining both pharmacological interventions with psychosocial treatment helps with treatment completion, reduced opioid use and remaining abstinent in patients going through opioid detoxification (Amato, Minozzi, Davoli, & Vecchi, 2011). Buprenorphine combined with naloxone or even buprenorphine alone significantly decreased opioid use and cravings for opioids in addicted individuals when administrated in an private-practice office setting (Fudala et al., 2003). In fact, administering buprenorphine to opioid-dependent patients in emergency departments increased engagement in subsequent addiction treatment and reduced self-reported opioid use (D’onofrio et al., 2015). Administration of buprenorphine during an emergency room visit can help alleviate withdrawal symptoms and may serve as a portal for the patients to further go on to addiction treatment. Additionally, Buprenorphine prescribing capacity was found to be positively associated with higher patient treatment completion rates by state (Pan et al., 2018).
Barriers to utilising buprenorphine exist on a global level. The World Drug Report (2018) reported that only 79 countries have both needle/syringe programmes and opioid substitution therapy as part of their substance use treatment services; out of those, only four countries were classified as having ‘high levels’ of coverage for both of these types of interventions. Unfortunately, some countries such as Russia forbid opioid substitution therapy such as buprenorphine and methadone. However, evidence of efficacy and safety of long-acting, slow release formulations of naltrexone for relapse prevention and former opioid addicts in St. Petersburg has shown promise (Krupitsky, Zvartau, & Woody, 2010). One review of national and state treatment capacity found that 96% of states in the U.S.A. had opioid misuse or dependence rates that exceeded their buprenorphine treatment capacity rates (Jones, Campopiano, Baldwin, & McCance-Katz, 2015a). Forty-seven percent of U.S. counties have no physicians that can prescribe buprenorphine, with the number increasing to 72% in the most rural counties.
In Germany, a trial of a 2-year heroin-assisted treatment (HAT) for severely addicted opioid users was associated with improvements in mental and physical health, as well as decreased street heroin use. (Verthein et al., 2008). For persons who are unable to quit intravenous drug use, HAT has been shown to be more effective than methadone maintenance, including higher retention rates and improvement of physical and/or mental health (Haasen et al., 2007). Furthermore, additional studies have found HAT to be more cost-effective than methadone treatment (Dijkgraaf et al., 2005). While the idea of giving people with opioid or heroin use disorders access to heroin can be controversial, it may be a viable solution for severely addicted individuals to keep functioning in their daily lives.
While marijuana is not considered one of the ‘medication-assisted therapies’ for opioid misuse, it is still pertinent to consider medical marijuana as a supplement to treatment of opioid addiction. An Australian household study on drugs indicated that heroin and non-medical prescription opioid users tend to substitute cannabis for opioids if the opioid of choice is not available 32–57% of the time (Australian Institute of Health and Welfare ((AIHW, 2002). A study of 350 medical marijuana patients from Berkley, California – where medical cannabis has been legal since 1996, found that patients report using cannabis as a substitute for more harmful drugs. Specifically, 40% of patients reported using cannabis as a substitute for alcohol, 26% for illicit drugs and 66% used marijuana as a substitute for prescription drugs (Reiman, 2009). No other illicit drugs such as cocaine, methamphethamine or alcohol were associated with frequency of opioid use (Kral et al., 2015). However, most of the research completed on marijuana substitution has involved weak research designs, and its use has its own negative consequences.
Improving treatment
Addiction is a complex disease to treat, and many healthcare providers feel that they do not have the necessary training and/or time in order to treat their opioid-addicted patients. Getting to understand someone’s addiction requires time – to build trust between the physician and patient, time to get a history of the addiction and time to figure out a treatment plan and possible referrals for the patient to follow up on. In rural areas, this problem tends to be even worse as there is already a lack of health-care providers, including those specialising in addiction. One solution posed to this issue is to recruit young new doctors to work with patients suffering from opioid use disorders in rural areas in exchange for some sort of loan-pay off programme. Another example is the organisation known as Project ECHO – which uses teleconferencing tools to address gaps in healthcare, especially in underserved areas such as rural communities. Healthcare practitioners from all around the world can receive guidance from other physicians on what they can do to treat complex issues, including opioid addiction (See: https://www.vox.com/science-and-health/2018/7/31/17398914/opioid-epidemic-project-echo-new-mexico-addiction).
Chronic care strategies have been employed in numerous diseases such as diabetes and hypertension, with frequent monitoring and check-ins with clinicians and other healthcare personnel. This type of care is pro-active, enables clinicians to see risk factors and warning signs before problems escalate, and integrates many different approaches to treatment, as well as networking a number of different healthcare professionals. Using the Chronic Care Model (CCM) has led to improved patient care and better health outcomes (Coleman, Austin, Brach, & Wagner, 2009). It is interesting to note that patients suffering from chronic disease do not do much better in complying with taking their medication and lifestyle changes than individuals with substance use disorders do in maintaining sobriety. McLellan (2002) argues for a continued care approach in substance abuse rehabilitation, just as with chronic diseases, rather than treating these disorders as ones that can be fixed in one single treatment programme. He argues for monitoring of patients; continuously checking in to see how they are doing with their ongoing and lifetime susceptibility to relapse, and utilising different sources such as physicians, case workers and counsellors to ensure the best chance at maintaining sobriety.
Policy
There is a need for development of quality improvement measures assessing pain and function, as well as more research on alternative treatments for pain. Insurance companies may also help to eliminate opioid misuse by increasing initiatives for doctors to have safe prescribing habits, along with increased coverage for alternative treatments. Increasing availability and accessibility of prescription drug monitoring data (PDMP) in places that lack this kind of online information can also help to curb doctor shopping in dependent patients. The International Commission on Narcotic Drugs has acknowledged the importance of proper disposal and safe return of medication, and some jurisdictions have even implemented prescription drug take back days (International Narcotics Control Board, 2017).
The United States has implemented a prescription drug monitoring programme (PDMP), which is a state-based system of data that allows clinicians to check whether or not their patients have been prescribed opioids from other healthcare sources. Usage of PDMP has found to be effective in reduction of obtaining excess opioids by going to multiple healthcare providers, otherwise known as ‘doctor shopping’ (Reifler et al., 2012). New York and Tennessee both instituted drug monitoring laws in 2012 which required prescribers to check a patient’s drug prescribing record through a database before prescribing them additional opioids. New York saw a 75% drop in patients obtaining pills from multiple prescribers, and Tennessee saw a 36% drop one year later (PDMP, 2014). Drug monitoring programmes can be especially effective if the data is made available in real-time, is used by all prescribers for all controlled substances, and is actively managed, sending alerts to physicians when problems are identified (Guy et al., 2017).
Unfortunately, while drug monitoring programmes can be effective in reducing instances of ‘doctor shopping’ or obtaining prescriptions from multiple providers, many of these programmes are underutilised by prescribers. One study found that in a survey of 420 responding physicians, 72% of them were aware that their state had a drug monitoring system, and only 53% used these programmes. Barriers to using the PDMPs included the length of time often necessary to retrieve information, as well as non-friendly formats for engaging with the programmes (Rutkow, Turner, Lucas, Hwang, & Alexander, 2015). These issues need to be addressed on a state-level in order to ensure that doctors have easy access to their patient’s information. Additionally, because these programmes are instituted on a country by country, and further, a state-by-state basis, it is possible that a patient could just go to another state to ‘doctor shop’. It may be worth considering putting federal and national databases into place.
While remaining controversial, needle-exchange programmes have been shown to reduce associated harms of injection drug use such as transmission of diseases. Furthermore, the use of naloxone, which is an opioid overdose antidote, has been found to be effective when persons are provided with training (Seal et al., 2005). Indeed, lay person’s use of naloxone to reverse overdoses is now occurring regularly throughout the U.S.A. (CDC, 2012; Wheeler, Jones, Gilbert, Davidson, Centers for Disease Control and Prevention, 2015), and the World Health Organization has recommended the use of naloxone. Syringe exchange programmes often offer naloxone so that injection drug users can save the lives of their peers, and there is increased pressure to provide nonparamedic first responders such as police and firefighters with naloxone, as it has been an effective strategy for reviving overdose victims (Williams, Marsden, & Strang, 2014). Family and friends of opioid users could also benefit from acquiring training on the administration of naloxone. Some local health departments and community programmes offer naloxone for free, but the availability and legality of obtaining naloxone without a prescription varies by state. Supervised consumptions rooms are worthy of consideration, and evaluations of these programmes have consistently found that individuals who use opiates in these settings do not die when overdose occurs (Potier, Laprévote, Dubois-Arber, Cottencin, & Rolland, 2014).
Conclusions
Some of the proposed options for reducing opioid use and misuse include prevention education, improved surveillance and monitoring of prescriptions, encouraging cautious prescribing and increasing timely treatment programming. There are a number of future avenues to be pursued regarding opioids, drug use and how to prevent and treat these problems. For example, Peltz and Südhof (2018) believe that a general opiate-induced maladaptation occurs in the brain circuits of many addicts. In order to study this, they suggest going beyond examining these mechanisms at a neural circuit level to characterising molecular signalling in the opioid-induced changes. If some of these pathways are better understood, new therapeutic approaches could be developed to help target the early stages of opioid addiction. Pharmaceutical research has also shown promise in pre-clinical trials in the development of an ‘opioid vaccine’, which would prevent the drug from entering the brain, thus, inhibiting it from producing any sort of psychoactive effects such as a high (Olson & Janda, 2017).
One major issue that must be addressed when considering opioid use reduction in the form of policies and initiatives is the treatment of those who do have legitimate, chronic or acute pain. It is estimated that 1 in 5 people worldwide suffer from chronic pain (Sullivan & Eagel, 2005), so getting rid of opioids altogether is clearly not a solution. Recent reports demonstrate that cancer patients have experienced difficulties in obtaining their prescription opioids. Barriers such as not having the drug in stock at the pharmacy, pharmacists questioning the need for a prescription and reduction of refills or number of pills were all cited by cancer patients (ACS CAN, 2018). It is unclear how many of these patients are abusing opioids, yet, it is hard to justify denying them opioids to manage their current cancer pain. A balance must be struck between limiting access to opioids for potential misusers and ensuring that those who truly benefit from prescription opioids are not experiencing barriers to their pain management.
Instead, more research is needed on pain management and alternative therapies that can be used for pain patients. Cannabis has been used for the relief of chronic non-cancer pain, can improve appetite, reduce muscle pain, alleviate anxiety and help with sleep (Abrams, Jay, Shade, Vizoso, & Reda, 2007; Ware et al., 2010). It can also help with nausea, neuropathic and non-neuropathic pain, spasticity, Tourette syndrome, seizures and glaucoma (Ben Amar, 2006; Grotenhermen & Muller-Vahl, 2012; Robson, 2001), and there are numerous ongoing research studies investigating its efficacy for other ailments and symptoms. A detailed 2017 report that considered over 10,000 research articles published on marijuana since 1999 found conclusive or substantial evidence that chronic pain patients being treated with cannabis or cannabinoids were likely to experience reductions in pain symptoms. Oral cannabinoids were effective in reducing chemotherapy-induced nausea and vomiting, as well as improving patient-reported multiple sclerosis spasticity symptoms (National Academies of Sciences, Engineering, and Medicine, 2017).
Rhodes (1997) postulates that drug users who may be experiencing difficult circumstances and a chaotic life attach a great amount of meaning to their intimate relationships, also deriving a sense of security from their partners or drug-using friends. Because of this intense attachment to other drug users in their social network, drug users may weigh the risks of drug behaviours such as injecting against the risks of losing those intimate relationships, and much of the time, the drug users will choose the risks of the drug. While individual choices and cognition must definitely be considered when analysing drug use behaviour and associated public health strategies to prevent it, there is evidence that for some drug users, particularly women, intimate relationships and social bonds play crucial roles in initiation and maintenance of drug use. This is a further topic of research that should be investigated, and public health outreach and intervention strategies should aim to incorporate solutions that tackle and untie the social networks and bonds of the drug user, or apply group-level strategies to change use among members of the social circle.
Healthcare organisations, clinicians, policymakers, researchers, local law enforcement, educators and lay people can all contribute to efforts to prevent and treat opioid misuse. Healthcare organisations, clinicians and law enforcement officials can increase access to and distribution of potentially life-saving resources such as Naloxone. There has been a push to administer buprenorphine to individuals in the emergency room who have come in for opioid withdrawal or overdose, an issue that hospitals, clinics and doctors can all have a voice in. Researchers must continue to conduct empirical studies on prevention and treatment of opioid abuse, which can help to inform policies developed at national levels. Public health officials must educate individuals on harm-reduction techniques, as well as the rising prevalence of overdoses, especially due to highly potent opioids such as fentanyl. In some regions, lay persons are able to acquire Naloxone to prevent opioid overdose if they ever come into contact with someone in an emergency situation. Lay people should also be informed of the signs of addiction and thus may be able to get their loved ones to seek help if they notice the symptoms in someone they know. Finally, it is important to understand the plight of individuals going through this difficult disorder, and not stigmatise opioid users any further.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Abrams DI, Couey P, Shade SB, Kelly ME, & Benowitz NL (2011). Cannabinoid–opioid interaction in chronic pain. Clinical Pharmacology & Therapeutics, 90, 844–851. doi: 10.1038/clpt.2011.188 [DOI] [PubMed] [Google Scholar]
- Abrams DI, Jay CA, Shade SB, Vizoso H, & Reda H (2007). Cannabis in painful HIV-associated sensory neuropathy—A randomized placebo-controlled trial. Neurology, 68, 515–521. doi: 10.1212/01.wnl.0000253187.66183.9c [DOI] [PubMed] [Google Scholar]
- Ahmad FB, Rossen LM, Spencer MR, Warner M, & Sutton P (2018). Provisional drug overdose death counts. National Center for Health Statistics. Retrived from: https://www.cdc.gov/nchs/nvss/vsrr/drugoverdose-data.htm
- Alexander GC, Kruszewski SP, & Webster DW (2012). Rethinking opioid prescribing to protect patient safety and public health. JAMA, 308, 1865–1866. doi: 10.1001/jama.2012.14282 [DOI] [PubMed] [Google Scholar]
- Amato L, Minozzi S, Davoli M, & Vecchi S (2011). Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. The Cochrane Database of Systematic Reviews, 9. [DOI] [PubMed] [Google Scholar]
- American Cancer Society Cancer Action Network (ACS CAN). (2018). Retrieved from https://www.acscan.org/sites/default/files/ACS%20CAN%20PQLC%20Opioid%20Research%20Project%20Key%20Findings%20Summary%20Memo%20FINAL.pdf
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-V- TR (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Arreola S, Bluthenthal RN, Wenger L, Chu D, Thing J, & Kral AH (2014). Characteristics of people who initiate injection drug use later in life. Drug Alcohol Depend, 138, 244–250. doi: 10.1016/j.drugalcdep.2014.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (AIHW). (2002). 2001 National drug strategy household survey: First RESULTS (AIHW cat. no. PHE 35. Drug Statistics Series No. 9) Canberra: AIHW; Retrieved from http://www.aihw.gov.au/publication-detail/?id= 6442467340 [Google Scholar]
- Back SE, Payne RL, Simpson AN, & Brady KT (2010). Gender and prescription opioids: Findings from the National Survey on Drug Use and Health. Addictive Behaviours, 35, 1001–1007. doi: 10.1016/j.addbeh.2010.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey JE, Campagna E, & Dart RC (2009). The underrecognized toll of prescription opioid abuse on young children. Annals of Emergency Medicine, 53, 419–424. doi: 10.1016/j.annemergmed.2008.07.015 [DOI] [PubMed] [Google Scholar]
- Baldacchino A, Balfour DJK, Passetti F, Humphris G, & Matthews K (2012). Neuropsychological consequences of chronic opioid use: A quantitative review and meta-analysis. Neuroscience & Biobehavioral Reviews, 36, 2056–2068. doi: 10.1016/j.neubiorev.2012.06.006 [DOI] [PubMed] [Google Scholar]
- Bell T, Annunziata K, & Leslie JB (2009). Opioid-induced constipation negatively impacts pain management, productivity, and health-related quality of life: Findings from the National Health and Wellness Survey. Journal of Opioid Management, 5, 137–144. [DOI] [PubMed] [Google Scholar]
- Ben Amar M (2006). Cannabinoids in medicine: A review of their therapeutic potential. Journal of Ethnopharmacology, 105, 1–25. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Wenger L, Chu D, Bourgois P, & Kral AH (2017). Drug use generations and patterns of injection drug use: Birth cohort differences among people who inject drugs in Los Angeles and San Francisco, California. Drug and Alcohol Dependence, 175, 210–218. doi: 10.1016/j.drugalcdep.2017.04.001 doi:10.1016/j.drugalcdep.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehnke KF, Litinas E, & Clauw DJ (2016). Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. The Journal of Pain, 17, 739–744. doi: 10.1016/j.jpain.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Bohnert AS, Guy GP Jr., & Losby JL (2018). Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention’s 2016 opioid guideline. Annals of Internal Medicine, 169, 367–375. doi: 10.7326/M18-1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, Gerhard GS, & Stewart WF (2010). Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction, 105, 1776–1782. doi: 10.1111/j.1360-0443.2010.03052.x [DOI] [PubMed] [Google Scholar]
- Bryant J, & Treloar C (2006). Risk practices and other characteristics of injecting drug users who obtain injecting equipment from pharmacies and personal networks. International Journal of Drug Policy, 17, 418–424. doi: 10.1016/j.drugpo.2006.07.004 [DOI] [Google Scholar]
- Busch AJ, Barber KA, Overend TJ, Peloso PMJ, & Schachter CL (2007). Exercise for treating fibromyalgia syndrome. The Cochrane Database of Systematic Reviews (4). [DOI] [PubMed] [Google Scholar]
- CDC. (2012). Community-based opioid overdose prevention programs providing Naloxone – United States, 2010. MMWR: Morbidity and Mortality Weekly Report, 61, 101–105. [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Dart RC, Inciardi JA, Woody GE, Schnoll S, & Muñoz A (2007). The development of a comprehensive risk-management program for prescription opioid analgesics: Researched Abuse, Diversion and Addiction-Related Surveillance (RADARSV®). Pain Medicine, 8, 157–170. doi: 10.1111/j.1526-4637.2006.00259.x [DOI] [PubMed] [Google Scholar]
- Cicero TJ, & Ellis MS (2015). Abuse-deterrent formulations and the prescription opioid abuse epidemic in the united states: Lessons learned from oxycontin. JAMA Psychiatry, 72, 424–430. doi: 10.1001/jamapsychiatry.2014.3043 [DOI] [PubMed] [Google Scholar]
- Cichewicz DL, & Welch SP (2003). Modulation of oral morphine antinociceptive tolerance and naloxone-precipitated withdrawal signs by oral Delta 9-tetrahydrocannabinol. Journal of Pharmacology and Experimental Therapeutics, 305, 812–817. doi: 10.1124/jpet.102.046870 [DOI] [PubMed] [Google Scholar]
- Coleman K, Austin BT, Brach C, & Wagner EH (2009). Evidence on the chronic care model in the new millennium. Health Aff (Millwood), 28, 75–85. doi: 10.1377/hlthaff.28.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- INCB. (2016). Comments on the reported statistics on narcotic drugs International Narcotics Control Board; Retrieved from https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2017/7_Part_2_comments_E.pdf [Google Scholar]
- Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, … Burls A (2007). Methadone and buprenorphine for the management of opioid dependence: A systematic review and economic evaluation In NIHR Health Technology Assessment programme: Executive Summaries NIHR Journals Library. [DOI] [PubMed] [Google Scholar]
- Connors GJ (1998). Overview of Project MATCH. The Addictions Newsletter, 5, 4–5. [Google Scholar]
- Conroy E, Degenhardt L, Mattick RP, & Nelson EC (2009). Child maltreatment as a risk factor for opioid dependence: Comparison of family characteristics and type and severity of child maltreatment with a matched control group. Child Abuse & Neglect, 33, 343–352. doi: 10.1016/j.chiabu.2008.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crofts N, Louie R, Rosenthal D, & Jolley D (1996). The first hit: Circumstances surrounding initiation into injecting. Addiction, 91, 1187–1196. doi: 10.1046/j.1360-0443.1996.918118710.x [DOI] [PubMed] [Google Scholar]
- D’onofrio G, O’connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, … Fiellin DA (2015). Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA, 313, 1636–1644. doi: 10.1001/jama.2015.3474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Ross J, & Teesson M (2007). The Australian Treatment Outcome Study (ATOS): What have we learnt about treatment for heroin dependence? Drug and Alcohol Review, 26(1), 49–54. doi: 10.1080/09595230601036986 [DOI] [PubMed] [Google Scholar]
- Darke S, Williamson A, Ross J, Teesson M, & Lynskey M (2004). Borderline personality disorder, antisocial personality disorder and risk-taking among heroin users: Findings from the Australian Treatment Outcome Study (ATOS). Drug & Alcohol Dependence, 74(1), 77–83. doi: 10.1016/j.drugalcdep.2003.12.002 [DOI] [PubMed] [Google Scholar]
- Delgado MK, Huang Y, Meisel Z, Hennessy S, Yokell M, Polsky D, & Perrone J (2018). National variation in opioid prescribing and risk of prolonged use for opioid-naive patients treated in the emergency department for ankle sprains. Annals of Emergency Medicine, 72(4), 389–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkgraaf MG, van der Zanden BP, de Borgie CA, Blanken P, van Ree JM, & van den Brink W (2005). Cost utility analysis of co-prescribed heroin compared with methadone maintenance treatment in heroin addicts in two randomised trials. BMJ, 330, 1297. doi: 10.1136/bmj.330.7503.1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D, Haegerich TM, & Chou R (2016). CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA, 315, 1624–1645. doi: 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D, Noonan RK, & Houry D (2017). Underlying factors in drug overdose deaths. JAMA, 318, 2295–2296. doi: 10.1001/jama.2017.15971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draus PJ, & Carlson RG (2006). Needles in the haystacks: The social context of initiation to heroin injection in rural Ohio. Substance Use & Misuse, 41, 1111–1124. doi: 10.1080/10826080500411577 [DOI] [PubMed] [Google Scholar]
- FDA. (2018). Timeline of selected FDA activities and significant events addressing opioid misuse and abuse US Food and Drug Administration; Retrieved from https://fas.org/sgp/crs/misc/R45218.pdf [Google Scholar]
- Feng C, DeBeck K, Kerr T, Mathias S, Montaner J, & Wood E (2013). Homelessness independently predicts injection drug use initiation among street-involved youth in a Canadian setting. Journal of Adolescent Health, 52, 499–501. doi: 10.1016/j.jadohealth.2012.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbain DA, Cole B, Lewis J, Rosomoff HL, & Rosomoff RS (2007). What percentage of chronic nonmalignant pain patients exposed to chronic opioid analgesic therapy develop abuse/addiction and/or aberrant drug-related behaviors? A structured evidence-based review. Pain Medicine, 9, 444–459. doi: 10.1111/j.1526-4637.2007.00370.x [DOI] [PubMed] [Google Scholar]
- Fitzgerald JL, Louie R, Rosenthal D, & Crofts N (1999). The meaning of the rush for initiates to injecting drug use. Contemporary Drug Problems, 26, 481–504. doi: 10.1177/009145099902600307 [DOI] [Google Scholar]
- Food and Drug Administration. (2009). Summary minutes. Joint Meeting of the Anesthetic Life Support Drugs Advisory Committee and Drug Safety & Risk Management Advisory Committee. Accessed October 20, 2018.https://www.federalregister.gov/documents/2009/04/24/E9-9380/joint-meeting-of-the-drug-safety-and-risk-management-advisory-committee-nonprescriptiondrugshttps://www.federalregister.gov/d/E9-9380
- Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, & Bennell KL (2015). Exercise for osteoarthritis of the knee: A Cochrane systematic review. British Journal of Sports Medicine, 49, 1554–1557. [DOI] [PubMed] [Google Scholar]
- Fudala PJ, Bridge TP, Herbert S, Williford WO, Chiang CN, Jones K, … Ling W (2003). Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. New England Journal of Medicine, 349, 949–958. doi: 10.1056/NEJMoa022164 [DOI] [PubMed] [Google Scholar]
- Gable RS (2006). Acute toxicity of drugs versus regulatory status In Fish JM (Ed.), Drugs and society: U.S. public policy (pp. 149–162). Lanham, MD: Rowman & Littlefield Publishers. [Google Scholar]
- Galaif ER, & Sussman S (1995). For whom does alcoholics anonymous work? International Journal of the Addictions, 30, 161–184. [DOI] [PubMed] [Google Scholar]
- Gottfredson DC, & Wilson DB (2003). Characteristics of effective school-based substance abuse prevention. Prevention Science, 4(1), 27–38. doi: 10.1023/A:1021782710278 [DOI] [PubMed] [Google Scholar]
- Gowing L, Farrell M, Borneman R, Sullivan LE, & Ali R (2008). Substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database of Systematic Reviews, 2, CD004145. [DOI] [PubMed] [Google Scholar]
- Grau LE, Dasgupta N, Grau LE, Dasgupta N, Harvey AP, Grau LE, … Grau LE (2007). Illicit use of opioids: Is OxyContin a “gateway drug”? The American Journal on Addictions, 16, 166–173. doi: 10.1080/10550490701375293 [DOI] [PubMed] [Google Scholar]
- Grella CE, & Lovinger K (2011). 30-year trajectories of heroin and other drug use among men and women sampled from methadone treatment in California. Drug Alcohol Depend, 118(2–3), 251–258. doi: 10.1016/j.drugalcdep.2011.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grotenhermen F, & Muller-Vahl K (2012). The therapeutic potential of cannabis and cannabinoids. Deutsches Ärzteblatt international, 109, 495–501. doi: 10.3238/arztebl.2012.0495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guise A, Horyniak D, Melo J, McNeil R, & Werb D (2017). The experience of initiating injection drug use and its social context: A qualitative systematic review and thematic synthesis. Addiction, 112, 2098–2111. doi: 10.1111/add.13957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guise A, Melo J, Mittal ML, Rafful C, Cuevas-Mota J, Davidson P, … Werb D (2018). A fragmented code: The moral and structural context for providing assistance with injection drug use initiation in San Diego, USA. International Journal of Drug Policy, 55, 51–60. doi: 10.1016/j.drugpo.2018.02.009 doi:10.1016/j.drugpo.2018.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy GP Jr, Zhang K, Bohm MK, Losby J, Lewis B, Young R, … Dowell D (2017). Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR. Morbidity and mortality weekly report, 66(26), 697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, & Naber D (2007). Heroin-assisted treatment for opioid dependence: Randomised controlled trial. The British Journal of Psychiatry, 191(1), 55–62. doi: 10.1192/bjp.bp.106.026112 [DOI] [PubMed] [Google Scholar]
- Hadland SE, Werb D, Kerr T, Fu E, Wang H, Montaner JS, & Wood E (2012). Childhood sexual abuse and risk for initiating injection drug use: A prospective cohort study. Preventive Medicine, 55, 500–504. doi: 10.1016/j.ypmed.2012.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassin J (1994). Living a responsible life: The impact of AIDS on the social identity of intravenous drug users. Social Science & Medicine, 39, 391–400. [DOI] [PubMed] [Google Scholar]
- Hays LR (2004). A profile of oxycontin addiction. Journal of Addictive Diseases, 23, 1–9, doi: 10.1300/J069v23n04_01 [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Grella C, Ling W, & Anglin D (2015). Long-term course of opioid addiction Harvard Review of Psychiatry, 23, 76–89. doi: 10.1097/HRP.0000000000000052 [DOI] [PubMed] [Google Scholar]
- International Narcotics Control Board: Report of the International Narcotics Control Board for 2017. 2017. New York: United Nations, 2018; Retrieved from https://www.incb.org/documents/Publications/AnnualReports/AR2017/Annual_Report_chapters/Chapter_2_2017.pdf [Google Scholar]
- Johnson EM, Lanier WA, Merrill RM, Crook J, Porucznik CA, Rolfs RT, & Sauer B (2013). Unintentional prescription opioid-related overdose deaths: Description of decedents by next of kin or best contact, Utah, 2008–2009. Journal of General Internal Medicine, 28, 522–529. doi: 10.1007/s11606-012-2225-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2009). Monitoring the Future national survey results on drug use, 1975–2008 Volume I: Secondary school students (NIH Publication No. 09–7402; 721 pp.). Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2011). Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010 Bethesda, MD: National Institute on Drug Abuse; Retrieved from http://monitoringthefuture.org/pubs/monographs/mtf-overview2010.pdf [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2013). Monitoring the Future national results on adolescent drug use: Overview of key findings, 2012 Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Jones CM (2013). Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers–United States, 2002–2004 and 2008–2010. Drug & Alcohol Dependence, 132(1), 95–100. doi: 10.1016/j.drugalcdep.2013.01.007 [DOI] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, & McCance-Katz E (2015a). National and state treatment need and capacity for opioid agonist medication-assisted treatment. American Journal of Public Health, 105, e55–e63. doi: 10.2105/AJPH.2015.302664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, & Bohm MK (2015b). Vital Signs: Demographic and Substance Use Trends Among Heroin Users - United States, 2002–2013. MMWR Morbidity and Mortality Weekly Report, 64, 719–725. [PMC free article] [PubMed] [Google Scholar]
- Julien RM (2005). A primer of drug action (9th ed.). New York, NY: W.H. Freeman and Company. [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, & Alexander GC (2015). The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annual Review of Public Health, 36, 559–574. doi: 10.1146/annurev-publ-health-031914-122957 [DOI] [PubMed] [Google Scholar]
- Kral AH, Wenger L, Novak SP, Chu D, Corsi KF, Coffa D, … Bluthenthal RN (2015). Is cannabis use associated with less opioid use among people who inject drugs? Drug Alcohol Depend, 153, 236–241. doi: 10.1016/j.drugalcdep.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, … Noorbaloochi S (2018). Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. JAMA, 319, 872–882. doi: 10.1001/jama.2018.0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupitsky E, Zvartau E, & Woody G (2010). Use of naltrexone to treat opioid addiction in a country in which methadone and buprenorphine are not available. Current Psychiatry Reports, 12, 448–453. doi: 10.1007/s11920-010-0135-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier WA, Johnson EM, Rolfs RT, Friedrichs MD, & Grey TC (2012). Risk factors for prescription opioid-related death, Utah, 2008–2009. Pain Medicine, 13, 1580–1589. doi: 10.1111/j.1526-4637.2012.01518.x [DOI] [PubMed] [Google Scholar]
- Lee JSJ, Hu HM, Edelman AL, Brummett CM, Englesbe MJ, Waljee JF, … Dossett LA (2017). New persistent opioid use among patients with cancer after curative-intent surgery. Journal of Clinical Oncology, 35, 4042–4049. doi: 10.1200/JCO.2017.74.1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Mooney L, & Hillhouse M (2011). Prescription opioid abuse, pain and addiction: Clinical issues and implications. Drug and Alcohol Review, 30, 300–305. doi: 10.1111/j.1465-3362.2010.00271.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macleod J, Hickman M, Jones HE, Copeland L, McKenzie J, De Angelis D, … Robertson JR (2013). Early life influences on the risk of injecting drug use: Case control study based on the Edinburgh Addiction Cohort. Addiction, 108, 743–750. doi: 10.1111/add.12056 [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, & Hirsch J (2017). Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician, 20, S3–S92. [PubMed] [Google Scholar]
- Marie BS, Sahker E, & Arndt S (2015). Referrals and treatment completion for prescription opioid admissions: Five years of national data. Journal of Substance Abuse Treatment, 59, 109–114. doi: 10.1016/j.jsat.2015.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, & Ciccarone D (2014). “Every ‘never’I ever said came true”: Transitions from opioid pills to heroin injecting. International Journal of Drug Policy, 25, 257–266. doi: 10.1016/j.drugpo.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin FS (2010). Becoming vulnerable: Young women’s accounts of initiation to injecting drug use. Addiction Research & Theory, 18, 511–527. doi: 10.3109/16066351003611653 [DOI] [Google Scholar]
- Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, & Hasin DS (2017). Changes in US lifetime heroin use and heroin use disorder: Prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74, 445–455. doi: 10.1001/jamapsychiatry.2017.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, & Boyd CJ (2017). Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics, 139, e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley JL, Back SE, & Brady KT (2013). Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addictive Behaviors, 38, 2230–2235. doi: 10.1016/j.addbeh.2013.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT (2002). Have we evaluated addiction treatment correctly? Implications from a chronic care perspective. Addiction, 97(3), 249–252. [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M, Rehm J, Heeb JL, & Gmel G (2004). Decreased taxation, spirits consumption and alcohol-related problems in Switzerland. Journal of Studies on Alcohol, 65, 266–273. doi: 10.15288/jsa.2004.65.266 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. Washington, DC: The National Academies Press. doi: 10.17226/24625 [DOI] [PubMed] [Google Scholar]
- NIDA. (2018). Heroin. Retrieved from https://www.drugabuse.gov/publications/research-reports/heroin
- Novak SP, Bluthenthal R, Wenger L, Chu D, & Kral AH (2016). Initiation of heroin and prescription opioid pain relievers by birth cohort. American Journal of Public Health, 106, 298–300. doi: 10.2105/AJPH.2015.302972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noyes R, Brunk SF, Avery DH, & Canter A (1975a). The analgesic properties of delta-9-tetrahydrocannabinol and codeine. Clinical Pharmacology and Therapeutics, 18(1), 84–89. doi: 10.1002/cpt197518184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Diversion Control Liaison and Policy Section Liaison Unit (ODLL), Drug Enforcement Administration. (2010). Information bulletin regarding a change in formulation for OxyContin tablets.
- Olson ME, & Janda KD (2017). Vaccines to combat the opioid crisis: Vaccines that prevent opioids and other substances of abuse from entering the brain could effectively treat addiction and abuse. EMBO Reports, e201745322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oviedo-Joekes E, Marchand K, Guh D, Marsh DC, Brissette S, Krausz M, … Schechter MT (2011). History of reported sexual or physical abuse among long-term heroin users and their response to substitution treatment. Addictive Behaviors, 36(1–2), 55–60. doi: 10.1016/j.addbeh.2010.08.020 [DOI] [PubMed] [Google Scholar]
- Pagano ME, Friend KB, Tonigan JS, & Stout RL (2004). Helping other alcoholics in alcoholics anonymous and drinking outcomes: Findings from project MATCH. Journal of Studies on Alcohol, 65, 766–773. doi: 10.15288/jsa.2004.65.766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan H, Gao S, Grant K, Novicoff W, & Kang H (2018, April). Analyzing national and state opioid abuse treatment completion with multilevel modeling Paper presented at the Systems and Information Engineering Design Symposium (SIEDS) (pp. 123–128). IEEE. [Google Scholar]
- PDMP Center of Excellence at Brandeis University. (2014). FL: Vital Signs Morbidity and Mortality Weekly Report, July 1, 2014.
- Peltz G, & Südhof TC (2018). The neurobiology of opioid addiction and the potential for prevention strategies. JAMA, 319, 2071–2072. doi: 10.1001/jama.2018.3394 [DOI] [PubMed] [Google Scholar]
- Pergolizzi J, Aloisi AM, Dahan A, Filitz J, Langford R, Likar R, … Sacerdote P (2010). Current knowledge of buprenorphine and its unique pharmacological profile. Pain Practice, 10, 428–450. doi: 10.1111/j.1533-2500.2010.00378.x [DOI] [PubMed] [Google Scholar]
- Posternak V, Dunn LB, Dhruva A, Paul SM, Luce J, Mastick J, … Miaskowski C (2016). Differences in demographic, clinical, and symptom characteristics and quality of life outcomes among oncology patients with different types of pain. Pain, 157, 892. doi: 10.1097/j.pain.0000000000000456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potier C, Laprévote V, Dubois-Arber F, Cottencin O, & Rolland B (2014). Supervised injection services: What has been demonstrated? A systematic literature review. Drug & Alcohol Dependence, 145, 48–68. doi: 10.1016/j.drugalcdep.2014.10.012 [DOI] [PubMed] [Google Scholar]
- Reifler LM, Droz D, Bailey JE, Schnoll SH, Fant R, Dart RC, & Bucher Bartelson B (2012). Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Medicine, 13, 434–442. doi: 10.1111/j.1526-4637.2012.01327.x [DOI] [PubMed] [Google Scholar]
- Reiman A (2009). Cannabis as a substitute for alcohol and other drugs. Harm Reduction Journal 6, 35. doi: 10.1186/1477-7517-6-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T (1997). Risk theory in epidemic times: Sex, drugs and the social organisation of ‘risk behaviour’. Sociology of Health & Illness, 19, 208–227. doi: 10.1111/1467-9566.ep10934410 [DOI] [Google Scholar]
- Ricardo Buenaventura M, Rajive Adlaka M, & Nalini Sehgal M (2008). Opioid complications and side effects. Pain physician, 11, S105–S120. [PubMed] [Google Scholar]
- Robson P (2001). Therapeutic aspects of cannabis and cannabinoids. The British Journal of Psychiatry, 178, 107–115. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M (1979). Becoming addicted: The woman addict. Contemporary Drug Problems, 8, 141. [Google Scholar]
- Roy É, Haley N, Leclerc P, C edras L, Blais L, & Boivin JF (2003). Drug injection among street youths in Montreal: Predictors of initiation. Journal of Urban Health, 80(1), 92–105. doi: 10.1093/jurban/jtg092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutkow L, Turner L, Lucas E, Hwang C, & Alexander GC (2015). Most primary care physicians are aware of prescription drug monitoring programs, but many find the data difficult to access. Health Affairs (Millwood), 34, 484–492. doi: 10.1377/hlthaff.2014.1085 [DOI] [PubMed] [Google Scholar]
- Saarto T, & Wiffen PJ (2010). Antidepressants for neuropathic pain: A Cochrane review. Journal of Neurology, Neurosurgery & Psychiatry, 81(12), 1372–1373. [DOI] [PubMed] [Google Scholar]
- Salerno SM, Browning R, & Jackson JL (2002). The effect of antidepressant treatment on chronic back pain: A meta-analysis. Archives of Internal Medicine, 162(1), 19–24. [DOI] [PubMed] [Google Scholar]
- Saxon AJ, Oreskovich MR, & Brkanac Z (2005). Genetic determinants of addiction to opioids and cocaine. Harvard Review of Psychiatry, 13, 218–232. doi: 10.1080/10673220500243364 [DOI] [PubMed] [Google Scholar]
- Schindler A, Thomasius R, Petersen K, & Sack PM (2009). Heroin as an attachment substitute? Differences in attachment representations between opioid, ecstasy and cannabis abusers. Attachment & Human Development, 11, 307–330. doi: 10.1080/14616730902815009 [DOI] [PubMed] [Google Scholar]
- Seal KH, Thawley R, Gee L, Bamberger J, Kral AH, Ciccarone D, … Edlin BR (2005). Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: A pilot intervention study. Journal of Urban Health, 82, 303–311. doi: 10.1093/jurban/jti053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Shin C, Ralston E, Redmond C, Greenberg M, & Feinberg M (2013). Longitudinal effects of universal preventive intervention on prescription drug misuse: Three randomized controlled trials with late adolescents and young adults. American Journal of Public Health, 103, 665–672. doi: 10.2105/AJPH.2012.301209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staiger TO, Gaster B, Sullivan MD, & Deyo RA (2003). Systematic review of antidepressants in the treatment of chronic low back pain. Spine, 28, 2540–2545. doi: 10.1097/01.BRS.0000092372.73527.BA [DOI] [PubMed] [Google Scholar]
- Strain EC (2002). Assessment and treatment of comorbid psychiatric disorders in opioid-dependent patients. Clinical Journal of Pain, 18, 514–527. [DOI] [PubMed] [Google Scholar]
- Strang J, Grifiths P, Powis B, & Gossop M (1999). Heroin chasers and heroin injectors: Differences observed in a community sample in London, UK. The American Journal on Addictions, 8, 148–160. [DOI] [PubMed] [Google Scholar]
- Strike C, Rotondi M, Kolla G, Roy E, Rotondi NK, Rudzinski K, … Hunt N (2014). Interrupting the social processes linked with initiation of injection drug use: Results from a pilot study. Drug Alcohol Depend, 137, 48–54. doi: 10.1016/j.drugalcdep.2014.01.004 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2016). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17–5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2010). Office of Applied Studies, Substance Abuse and Mental Health Services Administration, Treatment Episode Data Set (TEDS). Based on administrative data reported by States to TEDS through July 1, 2010. 2010. Available at: http://wwwdasis.samhsa.gov/webt/quicklink/US08.htm [Google Scholar]
- Sullivan LW, & Eagel BA (2005). Leveling the playing field: Recognizing and rectifying disparities in management of pain. Pain Medicine, 6(1), 5–10. doi: 10.1111/j.1526-4637.2005.05016.x [DOI] [PubMed] [Google Scholar]
- Sussman SY (2015). Evaluating the efficacy of Project TND: Evidence from seven research trials In Scheier LM (Ed.), Handbook of adolescent drug use prevention: Research, intervention strategies, and practice (pp. 159–176). Washington, DC, US: American Psychological Association. [Google Scholar]
- Sussman S (2017). Substance and behavioral addictions: Concepts, causes, and cures Cambridge University Press. [Google Scholar]
- Sussman S, & Ames SL (2008). Drug abuse: Concepts, prevention, and cessation. Cambridge University Press. [Google Scholar]
- Sussman S, Rohrbach LA, Spruijt-Metz D, Barnett E, Lisha N, & Sun P (2012). One-year prediction of pain killer use among at-risk older teens and emerging adults. Journal of Drug Education, 42, 195–210. doi: 10.2190/DE.42.2.e [DOI] [PubMed] [Google Scholar]
- Tauras JA, Markowitz S, & Cawley J (2005). Tobacco control policies and youth smoking: Evidence from a new era In Substance use: Individual behaviour, social interactions, markets and politics (pp. 277–291). Emerald Group Publishing Limited. [PubMed] [Google Scholar]
- Tobler NS, & Stratton HH (1997). Effectiveness of school-based drug prevention programs: A meta-analysis of the research. Journal of Primary Prevention, 18(1), 71–128. doi: 10.1023/A:1024630205999 [DOI] [Google Scholar]
- Trenz RC, Scherer M, Harrell P, Zur J, Sinha A, & Latimer W (2012). Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addictive Behaviors, 37, 367–372. doi: 10.1016/j.addbeh.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unick GJ, & Ciccarone D (2017). US regional and demographic differences inprescription opioid and heroin-related overdose hospitalizations. International Journal of Drug Policy, 46, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime, World Drug Report (UNODC). (2014). United Nations publication, Sales No. E.14.XI.7.
- U.S. Department of Health and Human Services, Center for Substance Abuse Treatment (CSAT). (2001). OxyContin: Prescription Drug Abuse. DHHS Publication No. (SMA)02–3636 NCADI Publication No. MS726. Washington, DC: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- van den Beuken-van MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, & Janssen DJ (2016). Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. Journal of Pain and Symptom Management, 51, 1070–1090. doi: 10.1016/j.jpainsymman.2015.12.340 [DOI] [PubMed] [Google Scholar]
- Van Gundy KT (2006). “Substance abuse in rural and small town America”. The Carsey School of Public Policy at the Scholars’ Repository. 7 https://scholars.unh.edu/carsey/7 [Google Scholar]
- Van Zee A (2009). The promotion and marketing of oxycontin: Commercial triumph, public health tragedy. American Journal of Public Health, 99, 221–227. doi: 10.2105/AJPH.2007.131714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verthein U, Bonorden-Kleij K, Degkwitz P, Dilg C, Köhler WK, Passie T, … Haasen C (2008). Long-term effects of heroin-assisted treatment in Germany. Addiction, 103, 960–966. doi: 10.1111/j.1360-0443.2008.02185.x [DOI] [PubMed] [Google Scholar]
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, & van der Goes DN (2015). Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain, 156, 569–576. doi: 10.1097/01.j.pain.0000460357.01998.f1 [DOI] [PubMed] [Google Scholar]
- Wang JC, Kapoor M, & Goate AM (2012). The genetics of substance dependence. Annual Review of Genomics and Human Genetics, 13, 241–261. doi: 10.1146/annurev-genom-090711-163844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware MA; Wang T; Shapiro S; Robinson A; Ducruet T; Huynh T, … Collet J-P (2010). Smoked cannabis for chronic neuropathic pain: A randomized controlled trial. Canadian Medical Association Journal, 182, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger LD, Lopez AM, Kral AH, & Bluthenthal RN (2016). Moral ambivalence and the decision to initiate others into injection drug use: A qualitative study in two California cities. International Journal of Drug Policy, 37, 42–51. doi: 10.1016/j.drugpo.2016.07.008 [DOI] [PubMed] [Google Scholar]
- Werb D, Bluthenthal RN, Kolla G, Strike C, Kral AH, Uuskula A, & Des Jarlais D (2018). Preventing injection drug use initiation: State of the evidence and opportunities for the future. Journal of Urban Health, 95(1), 91–98. doi: 10.1007/s11524-017-0192-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler E, Jones TS, Gilbert MK, Davidson PJ, Centers for Disease Control and Prevention (CDC). (2015). Opioid overdose prevention programs providing naloxone to layper-sons—United States, 2014. MMWR Morbidity and Mortality Weekly Report, 64, 631–635. [PMC free article] [PubMed] [Google Scholar]
- Wiffen PJ, Wee B, Derry S, Bell RF, & Moore RA (2017). Opioids for cancer pain-an overview of Cochrane reviews Cochrane Database of Systematic Reviews Chichester. UK: Wiley. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams ACDC, Eccleston C, & Morley S (2012). Psychological therapies for the management of chronic pain (excluding headache) in adults. The Cochrane Database of Systematic Reviews (11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AV, Marsden J, & Strang J (2014). Training family members to manage heroin overdose and administer naloxone: Randomized trial of effects on knowledge and attitudes. Addiction, 109, 250–259. doi: 10.1111/add.12360 [DOI] [PubMed] [Google Scholar]
- World Drug Report. (2018). United Nations publication, Sales No. E.18.XI.9.
- Young AM, Havens JR, & Leukefeld CG (2012). A comparison of rural and urban nonmedical prescription opioid users’ lifetime and recent drug use. The American Journal of Drug and Alcohol Abuse, 38, 220–227. doi: 10.3109/00952990.2011.643971 [DOI] [PubMed] [Google Scholar]
- Young AM, Larian N, & Havens JR (2014). Gender differences in circumstances surrounding first injection experience of rural injection drug users in the United States. Drug & Alcohol Dependence, 134, 401–405. doi: 10.1016/j.drugalcdep.2013.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacny JP (1995). A review of the effects of opioids on psychomotor and cognitive functioning in humans. Experimental and Clinical Psychopharmacology, 3, 432–466. doi: 10.1037/1064-1297.3.4.432 [DOI] [Google Scholar]
- Zacny JP, & Lichtor SA (2008). Nonmedical use of prescription opioids: Motive and ubiquity issues. The Journal of Pain, 9, 473–486. doi: 10.1016/j.jpain.2007.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]


