Abstract
Background
Angioleiomyoma of the pulmonary artery is rare in the literature and few studies have been reported. Here we present a rare case of angioleiomyoma arising from the pulmonary artery in a young patient.
Case presentation
A 27-year-old male patient presented to our clinic due to the incidental finding of a nodule in the right lower lobe of the lung, which was unchanged from the prior year. Preoperative CT scans showed a well-demarcated nodule of soft tissue density penetrated by the basal branch of the right anterior basilar artery (RA8b). Single-port video-assisted RS8 segmentectomy was performed under the guidance of preoperative 3-dimensional reconstruction for histologic confirmation of the tumour. The tumour appeared as a solid tumour of a tube-like structure with vascular endothelium, composed of spindle-shaped smooth muscle cells lacking nuclear atypia and homogenous red-dye substances. The spindle cells were positive for immunostaining for smooth muscle actin (SMA), desmin and Ki-67 and were negative for immunostaining for Dog-1, HMB45, and Melan-A. A pathological diagnosis of primary angioleiomyoma of the pulmonary artery was finally made.
Conclusions
This report is a reminder for thoracic surgeons that angioleiomyoma should be included in the differential diagnosis of lung neoplasms, especially for the mass of soft tissue density penetrated by pulmonary blood vessels shown by CT. Awareness of this rare entity should potentially prevent underdiagnosis and improper surgical treatment.
Keywords: Angioleiomyoma, Lung neoplasm, Differential diagnosis, Case report
Background
Angioleiomyoma is a benign soft tissue tumour comprising mature smooth muscle cells with a prominent vascular component [1]. It typically forms a well-circumscribed, subcutaneous nodule less than 20 mm in adults, especially in the leg [2]. However, this type of tumour rarely occurs in the lung. We herein report an interesting case of angioleiomyoma arising from the pulmonary artery and present a literature review of previously reported cases.
Case presentation
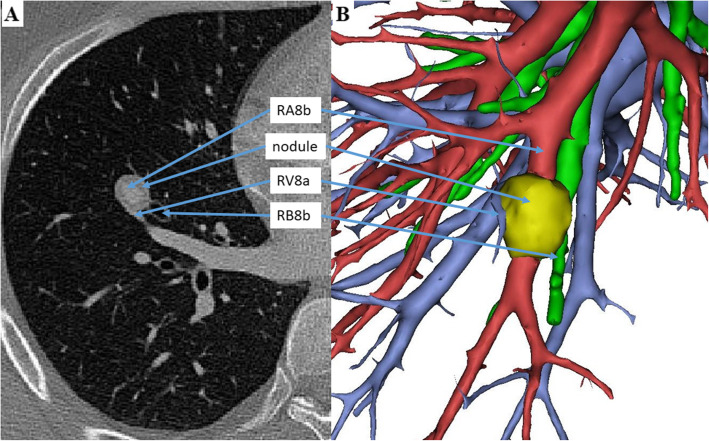
A 27-year-old male patient complained of the incidental finding of a nodule in the right lower lobe of the lung on a routine health examination in October 2019, which was unchanged on repeat examinations from the prior year. No related subjective symptoms were noted and the physical examination showed no abnormalities. The results of routine blood biochemistry, oncological biomarkers and flexible bronchoscopy were normal. Contrast-enhanced computerized tomography of the chest showed a well-demarcated mass with a maximum diameter of 1.7 cm in the right anterior basilar segment of the lung (RS8). The lesion, which displayed a soft tissue density in the periphery, was penetrated by the basal branch of the right anterior basilar artery (RA8b) (Fig. 1).
Fig. 1.
Findings of CT and 3D reconstruction in a patient with angioleiomyoma of the pulmonary artery. Contrast-enhanced computed tomography (CT) of the chest showed a well-demarcated mass with a maximum diameter of 1.7 cm in the right anterior basilar segment of the lung (RS8), adjacent to the basal branch of the right anterior basilar bronchus (RB8b). The lesion, displaying soft tissue density in the periphery, was penetrated by the basal branch of the right anterior basilar artery (RA8b) and bypassed by the lateral branch of the right anterior basilar vein (RV8a). Preoperative 3-dimensional (3D) reconstruction of the pulmonary vessels and bronchial trees of the right lower lobe from CT images was performed, and single-port RS8 segmentectomy was performed for histologic confirmation of the mass
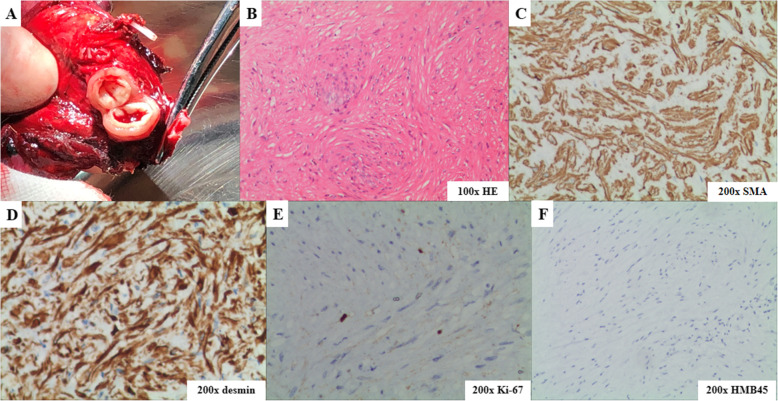
Preoperative 3-dimensional reconstruction of the pulmonary vessels and bronchial trees of the right lower lobe from CT images was performed for surgical guidance (Fig. 1) and surgical resection was performed for histologic confirmation of the tumour. In view of its centrally-located site and suspicion of a benign lesion, single-port video-assisted RS8 segmentectomy was performed. The well-bounded nodule was resected with clear margins. After dividing the lesion, it appeared as a solid tumour of a tube-like structure with vascular endothelium (Fig. 2), composed of spindle-shaped smooth muscle cells lacking nuclear atypia and homogenous red-dye substances. Focal calcification was noted and no malignant evidence was detected. The spindle cells exhibited positive immunostaining for smooth muscle actin (SMA), desmin and Ki-67 (labelling 3%) and negative immunostaining for Dog-1, HMB45, and Melan-A (Fig. 2). The patient experienced an uneventful postoperative course. Immediate postoperative radiographs on postoperative day 3 showed complete reexpansion of the lung without obvious pneumothorax or hydrothorax. At his 6-month follow-up, the patient was well without complications or evidence of recurrence.
Fig. 2.
Gross appearance and microscopic pathology of the tumour. a, After dividing the mass, it appeared as a solid tumour exhibiting a tube-like structure with vascular endothelium; b, Histologically, the mass was displayed as proliferating spindle-shaped smooth muscle cells lacking nuclear atypia and homogenous red-dye substances; c, the spindle cells showed positive immunostaining for smooth muscle actin (SMA); d, the spindle cells showed positive immunostaining for desmin; e, the spindle cells showed positive immunostaining for Ki-67 (labelling 3%); f, the spindle cells showed negative immunostaining for HMB45
Discussion
Angioleiomyoma, also known as angiomyoma or vascular leiomyoma, is a benign soft tissue tumour comprising mature smooth muscle cells with a prominent vascular component. It was previously classified under ‘smooth muscle tumours’ by the World Health Organization (WHO) in 2002, but reclassified under ‘pericytic tumours’ in the updated classification because of morphological features shared with myopericytoma, that is, showing a perivascular concentric arrangement of smooth muscle cells [3]. Additionally, Morimoto et al. proposed a classification system, that divided angioleiomyoma into solid, cavernous, and venous types and reported that these pathologic subtypes were associated with clinical manifestations [4].
Clinically, angioleiomyoma usually occurs in the lower extremities and appears as a solitary, slow-growing, mobile, firm and occasionally painful cutaneous mass [1]. The pain can often be paroxysmal and provoked by exposure to cold and wind, which is thought to be due to active contraction of smooth muscle that results in local ischaemia [5]. Angioleiomyoma rarely occurs in the lung. Whether patients with angioleiomyoma in the lung have symptoms may depend on the tumour size and location. Symptoms may range from an asymptomatic presentation to recurrent cough when the tumour grows large enough in the lung parenchyma [6, 7].
Preoperative diagnosis of angioleiomyoma is difficult before histopathology [8]. Complete surgical resection is the only way to guarantee curative outcomes [5]. Angioleiomyoma can be correctly diagnosed by microscopy with conventional H&E staining. Special staining for smooth muscle cells, such as actin, desmin, or myosin, and for vascular endothelium, such as factor VIII or CD31 can aid in differentiating angioleiomyoma from haemangioma, angiofibroma, fibroma, angiomyolipoma, and angiomyosarcoma [9]. Attention should also be paid to the possibility of benign metastasizing leiomyoma (BML) when encountering female patients because of BML’s metastatic traits of invading the pulmonary artery [10]. Despite the vascular nature of these tumours, significant bleeding during surgical excision is seldom seen [8]. Recurrence after complete removal is extremely rare, regardless of the pathological subtype [8].
To the best of our knowledge, only two cases of angioleiomyoma of the pulmonary artery have been reported so far [6, 7]. The clinicopathological features of the previously reported cases and our case are summarized in Table 1. Klotz et al. reported a case of angioleiomyoma infiltrated into the left pulmonary artery of a 54-year-old patient who underwent tangential resection of the infringed artery followed by a direct suture of the vessel wall [6]. Terada described a 62-year-old female patient receiving lobectomy for a small mass in the right upper lobe of the lung, in which this mass turned out to be an angioleiomyoma arising from the pulmonary artery [7]. Herein, we report a rare case of angioleiomyoma arising from the RA8b artery in a young male patient who received single-port video-assisted RS8 segmentectomy and we review the literature on angioleiomyoma of the pulmonary artery.
Table 1.
Clinical and pathological features of angioleiomyomas of the pulmonary artery
| Klotz et al | Terada | Present case | |
|---|---|---|---|
| Age/gender | 54/female | 62/female | 27/male |
| Symptoms | Recurrent cough | None | None |
| Smoking status | Non-smoker | Non-smoker | Non-smoker |
| Location | Left upper lobe | Right upper lobe | Right lower lobe |
| Tumour size (cm) | 3.5 | 1 | 1.7 |
| Gross view | Tumour mass with the lumen of an artery vessel | Continuous to a pulmonary artery and small pulmonary arteries scattered within the tumour | Tube-like structure with vascular endothelium |
| Histology | Consisted of spindle cells, arranged in nested bundles | Consisted of mature smooth muscle with acidophilic cytoplasm | Consisted of spindle-shaped smooth muscle cells |
| Immunostains | Actin, desmin | Actin, vimentin, Ki-67 (2%) | SMA, desmin, Ki-67 (3%) |
| Treatment | Resection of the whole tumour and pulmonary arterioplasty | Lobectomy | Segmentectomy |
| Clinical outcomes | Free of disease for 12 months | Free of disease for 10 years | Free of disease for 6 months |
Conclusion
We believe this report emphasizes the necessary awareness of thoracic surgeons that angioleiomyoma should be included in the differential diagnosis of lung neoplasms, Although an accurate preoperative diagnosis can be challenging, in our opinion, CT imaging findings presenting as a soft-tissue density nodule penetrated by the pulmonary blood vessel may indicate the possibility of angioleiomyoma. Due to the benign nature of this tumour, sublobar resection is appropriate for the treatment of angioleiomyoma of the pulmonary artery.
Additional file 1. Video 1 Legend. Single-port RS8 segmentectomy was performed through the fifth intercostal space between anterior axillary line and midaxillary line. Insufflation technique was utilized to establish intersegmental border (Asian Cardiovasc Thorac Ann 2019 Nov; 27 [9]). RA8, right anterior basilar artery, RB8, right anterior basilar bronchus, RV8a, lateral branch of right anterior basilar vein.
Acknowledgements
Not applicable.
Abbreviations
- RA8b
The basal branch of the right anterior basilar artery
- RS8
The right anterior basilar segment of the lung
- SMA
Smooth muscle actin
- WHO
World Health Organization
- BML
Benign metastasizing leiomyoma
Authors’ contributions
YH drafted and edited this manuscript, assisted in the surgery, and analysed the patient data. SYR edited this manuscript and analysed the patient data. ST, XW and FY analysed the patient data. QL prepared and assessed the histopathological images. WL performed the surgery, edited this manuscript, and analysed the patient data. The author(s) read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81700070 to Siying Ren), the Hunan Province Natural Science Foundation of China (2019JJ30038 to Siying Ren) and the Hunan Province Health Department Research Fund (B2018–0541 to Siying Ren).
Availability of data and materials
As this paper is a case report, all data generated or analysed are included in this article.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Second Xiangya Hospital of Central South University, Changsha, China. Written informed consent was obtained from the patient reported in this study.
Consent for publication
Written informed consent for publication of the clinical details and/or clinical images was provided by the patient.
Competing interests
The authors have no conflicts of interest to declare in this work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13019-020-01275-z.
References
- 1.Dalainas I. Vascular smooth muscle tumors: review of the literature. Int J Surg. 2008;6(2):157–163. doi: 10.1016/j.ijsu.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Ramesh P, Annapureddy SR, Khan F, Sutaria PD. Angioleiomyoma: a clinical, pathological and radiological review. Int J Clin Pract. 2004;58(6):587–591. doi: 10.1111/j.1368-5031.2004.00085.x. [DOI] [PubMed] [Google Scholar]
- 3.Jo VY, Fletcher CD. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46(2):95–104. doi: 10.1097/PAT.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 4.Morimoto N. Angioleiomyoma. A clinicopathologic study. Med J Kagoshina Univ. 1973;24:663–683. [Google Scholar]
- 5.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer. 1984;54(1):126–130. doi: 10.1002/1097-0142(19840701)54:1<126::AID-CNCR2820540125>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 6.Klotz LV, Morresi-Hauf A, Hatz RA, Lindner M. Vascular leiomyoma of the pulmonary artery. Ann Thorac Surg. 2016;101(1):342–344. doi: 10.1016/j.athoracsur.2015.02.113. [DOI] [PubMed] [Google Scholar]
- 7.Terada T. Vascular leiomyoma of the lung arising from pulmonary artery. Int J Clin Exp Pathol. 2013;6(1):97–99. [PMC free article] [PubMed] [Google Scholar]
- 8.Wang CP, Chang YL, Sheen TS. Vascular leiomyoma of the head and neck. Laryngoscope. 2004;114(4):661–665. doi: 10.1097/00005537-200404000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Maeda Y, Hirota J, Osaki T, Hayashi K, Sonobe H, Otsuki Y. Angiomyoma of the upper lip: report of a case with electron microscopic and immunohistochemical observation. Br J Oral Maxillofac Surg. 1989;27(3):236–242. doi: 10.1016/0266-4356(89)90151-4. [DOI] [PubMed] [Google Scholar]
- 10.Poujade O, Genin AS, Dhouha M, Luton D. A benign metastasizing leiomyoma involving a nodule in the pulmonary artery: case and literature review. Eur J Gynaecol Oncol. 2010;31(3):329–332. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As this paper is a case report, all data generated or analysed are included in this article.